Abstract
BACKGROUND:
Patients with small bowel tumours frequently require surgical intervention. Minimally invasive techniques require advanced skills and may not be offered to many patients. We present a laparoscopic single-incision technique that is minimally invasive without requiring intracorporeal anastomosis.
MATERIALS AND METHODS:
The cases of all patients with laparoscopic small bowel resections performed by one surgeon from 2008 to 2012 were reviewed. A single-port technique was introduced after it became available at our institution in 2009. Before that, conventional laparoscopy (LAP) was performed with extension of the periumbilical incision to allow externalisation of the bowel.
RESULTS:
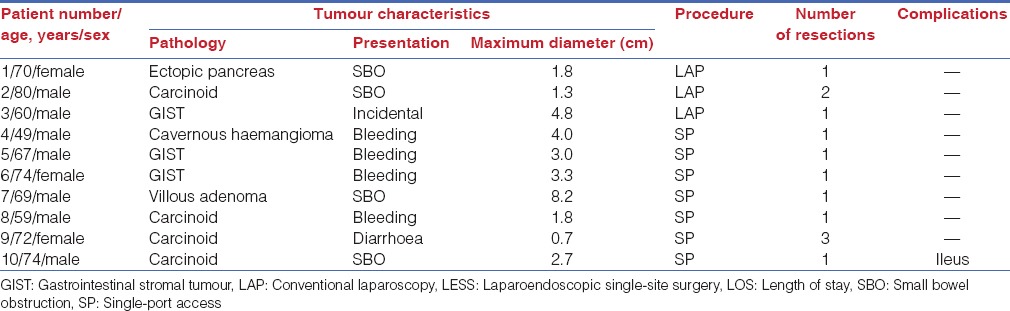
Totally, 10 patients were identified who underwent laparoscopic resection of small bowel tumours: 9 in the small bowel and 1 in the terminal ileum near the cecum. Three tumours were resected before 2009 using LAP, and 7 were resected using the single-port technique. Median length of stay was 3 days, median follow-up was 16.5 months, and no patients had a recurrence. Operative time, post-operative complications, hospital length of stay, and narcotic utilisation were similar between the single-port and traditional laparoscopic groups.
CONCLUSION:
Laparoscopic removal of small bowel tumours with a small, periumbilical trocar incision is both effective and feasible without advanced technical skill.
Keywords: Carcinoid, gastrointestinal stromal tumour, laparoendoscopic single-site surgery, single-incision small bowel resection, single-incision surgery, small bowel tumours
INTRODUCTION
Tumours of the small bowel are rare, accounting for only 1% of all gastrointestinal tract neoplasms. The most common presentations of small bowel tumours include obstruction and occult gastrointestinal haemorrhage, although the clinical presentation is often vague. Small bowel neoplasms are associated with several disease states, including Peutz–Jeghers syndrome, familial polyposis syndromes, Crohn's disease, celiac disease, and immunodeficiency states. The incidence of small bowel tumours varies in the literature from series to series because of the relative rarity of these tumours, but the more common tumours include adenomas, lipomas, haemangiomas, gastrointestinal stromal tumours (GISTs), carcinoid tumours, lymphomas, and adenocarcinomas.[1,2] The current best treatment for most of these small bowel tumours is surgical resection when feasible, especially in symptomatic disease.
Options for resection of small bowel tumours include both open and laparoscopic techniques. Open surgical small bowel procedures require a large incision for resection, and multiple trials have suggested improved post-operative pain control, shorter duration of hospital stay, and fewer wound infections with laparoscopic surgery, without increasing complication rates.[3,4,5,6] Furthermore, multiple studies have confirmed the oncologic safety of laparoscopic tumour resections when feasible,[3,4,7] including adequate resection of mesenteric lymph node basins.
Laparoscopic procedures for small bowel resection require enlarging an incision to allow for specimen removal and/or intracorporeal anastomosis. Minimally invasive GIST resection, when used in selected patients, has shown to result in shorter length of stay, improved post-operative pain, and slightly fewer complications compared with open procedures,[7,8] without negative effects on oncologic outcomes. Resections of GISTs using single-port access techniques have been described for relatively small gastric GISTs.[9] No current data exist for single-port resections of small bowel GISTs or carcinoid tumours, but single-site surgery is being increasingly used for various gastrointestinal operations, ranging from basic procedures such as appendectomy, cholecystectomy, and ventral hernia repair, to more advanced procedures including minor hepatectomies, gastrectomies, and small bowel and colon resections.
We sought to describe our experience with resection of primary small bowel tumours, including small GISTs, neuroendocrine carcinomas, and other rare small bowel tumours, using a single-port access technique. We hypothesised that single-site resections of small bowel tumours would be comparable to laparoscopic resections in terms of oncologic resection and safety and would be feasible without requiring advanced laparoscopic skills, thus making it easier for both the patient and the surgeon.
MATERIALS AND METHODS
One surgeon at our centre routinely performs single-incision laparoscopic surgery. We reviewed the experience of this surgeon (J.B.) with laparoscopic small bowel resections. We searched for the records of the surgeon's patients who underwent laparoscopic small bowel resection for small bowel tumours, including GISTs, carcinoid tumours, and other rare small bowel tumours, from May 2008 to June 2012. Approval was obtained from our Institutional Review Board.
Patients identified were grouped according to type of procedure: Conventional laparoscopy (LAP) or single-port access. Patient characteristics reviewed included age, sex, body mass index, hospital length of stay, and post-operative narcotic utilisation. Operative reports were identified to define the process of single-port access small bowel resection. Pathology reports were reviewed to evaluate tumour type and oncologic resection margin status.
Statistical analysis was performed using the χ2 test for univariate analysis and non-parametric rank sum tests using the Wilcoxon model. Results were reported as number of patients or median (interquartile range), as appropriate. P < 0.05 was considered significant.
Surgical Technique
Anaesthesia preparation was the same as for any bowel operation. Our institution practices the enhanced recovery pathway, with pre-operative acetaminophen and ketorolac, and lack of bowel preparation.
Both laparoscopic and single-incision port sites were injected with a 1:1 mixture of 0.25% bupivacaine and 1% lidocaine. Post-operatively, patients receive scheduled acetaminophen and ketorolac, with narcotic medications available for breakthrough pain.
For standard laparoscopic procedures (i.e., LAP), the abdomen was entered under direct visualisation using either the Hasson technique, with insertion of a 10-mm camera port or the Veress needle and a 5-mm optical-viewer trocar. Two additional 5-mm working ports were inserted under direct visualisation. The small bowel was freed from any adhesions and fully mobilised. The periumbilical 10-mm trocar incision was extended to an average length of 3 cm, and the wound edges were protected with a wound protector. The small bowel was externalised and examined in its entirety, and tumours could be resected, with primary anastomosis performed extracorporeally. Anastomoses were performed with the GIA stapler (Ethicon), with imbricating sutures to oversew the staple lines.
For the single-port procedure, the periumbilical incision was made 3 cm long to allow placement of the GelPOINT Advanced Access Platform (Applied Medical Resources) [Figure 1]. This platform allows for three instruments to be used. The fasciotomy was extended to the length needed for specimen removal, without extending the skin incision. The surgical videoscope was the Stryker 30° 5-mm camera. We used the same straight instruments as in traditional laparoscopic procedures in all cases. For the single-port procedure, the small bowel was mobilised and freed from adhesions in a similar fashion to LAP. The bowel was then externalised through the GelPOINT incision, which already has a wound protector in place. Care was taken not to externalise a large portion of small bowel at a time to avoid venous congestion [Figure 2]. The remainder of the procedure was the same as for LAP procedures.
Figure 1.

Photograph of single-port incision device (Applied Medical Resources)
Figure 2.

Intraoperative photographs of initial exploration of small bowel tumour and mobilization of attachments
RESULTS
Totally, 10 patients were identified who underwent laparoscopic resection of small bowel tumours and consented to be in the study [Table 1]; 9 tumours were in the small bowel [Figure 3], and 1 was in the terminal ileum near the cecum. Three tumours were resected using LAP (LAP group), with extension of the periumbilical incision to allow externalisation of the bowel. The other 7 tumours were resected using the single-incision technique (single-port access group), with a 3 cm periumbilical incision made for placement of the GelPOINT platform. The bowel was then externalised through this incision. There were no significant differences in age, sex, body mass index, operative time, post-operative complications, size of tumour, hospital length of stay or post-operative narcotic use between the single-port and LAP groups [Table 2]. Median length of stay was 3 days, median follow-up was 16.5 months, and no patients had recurrence of tumour. A complication developed in only 1 patient — a post-operative ileus requiring nasogastric tube decompression and hospitalisation for 9 days. One patient in the single-port group was given a diagnosis of metastatic gastric cancer from linitis plastica, despite normal upper endoscopy results, and underwent additional work-up, which led to a prolonged hospital stay.
Table 1.
Patient characteristics
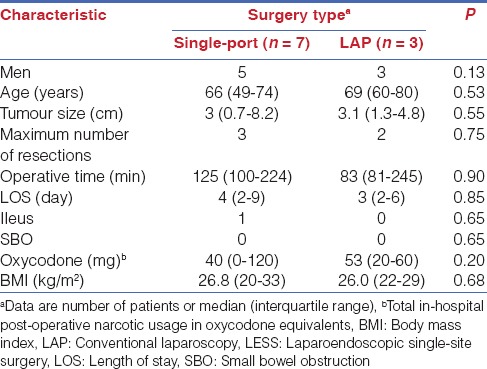
Figure 3.

Computed tomography with intravenous contrast demonstrating tumour emanating from a loop of small bowel
Table 2.
Tumour and procedure characteristics
DISCUSSION
For GISTs, surgical resection has been described using both open and laparoscopic techniques,[10] although the literature regarding GISTs overwhelmingly involves tumours located in the stomach. Current National Comprehensive Cancer Network guidelines for the management of GISTs recommend:
Resection if the tumour is larger than 2 cm; laparoscopic resection of gastric GISTs is feasible as long as standard surgical oncologic procedures are observed;
Minimising tumour manipulation and avoidance of tumour capsule rupture to prevent intraperitoneal tumour seeding; and
Removing the tumour in a plastic bag to minimise laparoscopic port site recurrence.
Given the rarity of lymphatic metastasis with GISTs, surgical treatment involves segmental resection without lymphadenectomy.[11] Some authors believe that relatively small tumours (2-5 cm) should be treated solely with laparoscopy.[8]
Similarly, surgical resection of carcinoid tumours is recommended to improve symptoms and survival,[12,13] even in the presence of metastatic disease, to prevent future obstructive complications.[14] All carcinoid tumours deemed operable should be resected surgically. Given the propensity of carcinoid tumours for lymphatic metastasis, formal resection of all draining lymph node basins should be performed at the time of primary excision. In addition, any obvious mesenteric nodules should be excised at the time of operation.[15] Surgical management of carcinoid tumours classically uses an open method to allow palpation of the entire length of bowel, which aids in the detection of small tumours and mesenteric nodules. In our study, the small bowel could still be eviscerated and therefore palpated using the single-port technique, thus keeping this tenet intact. We have not yet found body mass index to be a limiting factor in the selection of patients for a single-site operation. However, a larger body mass index sometimes does necessitate changing the operative site to be nearer the suspected tumour site to allow for ease of triangulation of the instruments.
Our study showed that in selected patients, laparoscopic removal of small bowel tumours is both safe and feasible. Single-port access remains a good option for removal of these tumours, as long as the entire small bowel can be externalised and visualised. No data until date suggest increases in local recurrence, port site recurrences or inadequacy of resections with laparoscopic removal of such tumours. GIST tumours have a propensity to spread haematogenously, and avoiding capsule rupture seems to be important in the oncologic safety of the operation. Carcinoid tumours, with a propensity for lymphatic metastases, can be resected in a similar fashion to bowel adenocarcinoma, provided the entire small bowel is externalised, inspected, and palpated for occult disease. In our small series, we were able to safely perform multiple small bowel resections through a single, small, periumbilical incision [Figure 4]. This demonstrates a key advantage of single-port surgery over LAP — in traditional LAP this would require enlargement of 1 of the incisions. Once the bowel is externalised, multiple bowel resections can be performed without added difficulty; the surgeon simply performs additional anastomoses on externalised bowel.
Figure 4.

Post-operative photograph. 6-week follow-up image demonstrating the cosmetically pleasing result of the single-port incision
An additional benefit of single-port surgery using the GelPOINT access platform is the wound protection device already incorporated into the access port. Previous studies have shown a significant decrease in surgical site infections with the use of plastic wound retractors.[16] At our institution, the cost of one of these devices is equivalent to that of three traditional laparoscopic trocars. In contrast, although operative times were not significantly different, the duration was slightly longer in the single-port access group, which may lead to the increased cost.
We readily acknowledge the limitations of such a small study size. Given the relative rarity of these tumours, our numbers did not demonstrate statistically significant differences in length of stay, narcotic utilisation or post-operative complications between the single-port and LAP groups. Nonetheless, this procedure is technically easier than standard laparoscopy with intracorporeal anastomosis and results in fewer incisions than standard laparoscopy with extracorporeal anastomosis. The patient benefits from the laparoscopic approach with a single, small incision.
Footnotes
Source of Support: This study was supported in part by the NIH (grant number 1K23 DK093553-01A).
Conflict of Interest: None declared.
REFERENCES
- 1.Hodin RA, Matthews JB. Small intestine. In: Norton JA, Barie PS, Bollinger RR, Chang AE, Lowry SF, Mulfihill SJ, et al., editors. Surgery: Basic Science and Clinical Evidence. 2nd ed. New York: Springer; 2008. pp. 963–90. [Google Scholar]
- 2.Coco C, Rizzo G, Manno A, Mattana C, Verbo A. Surgical treatment of small bowel neoplasms. Eur Rev Med Pharmacol Sci. 2010;14:327–33. [PubMed] [Google Scholar]
- 3.Pitiakoudis M, Zezos P, Courcoutsakis N, Papanas N, Giatromanolaki A, Sivridis E, et al. Is laparoscopic resection the appropriate management of a jejunal gastrointestinal stromal tumor (GIST).Report of a case? Surg Laparosc Endosc Percutan Tech. 2010;20:e160–3. doi: 10.1097/SLE.0b013e3181f334ca. [DOI] [PubMed] [Google Scholar]
- 4.Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, et al. Laparoscopically assisted vs open colectomy for colon cancer: A meta-analysis. Arch Surg. 2007;142:298–303. doi: 10.1001/archsurg.142.3.298. [DOI] [PubMed] [Google Scholar]
- 5.Dasari BV, McKay D, Gardiner K. Laparoscopic versus Open surgery for small bowel Crohn's disease. Cochrane Database Syst Rev. 2011;1:CD006956. doi: 10.1002/14651858.CD006956.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Liu Z, Zhang P, Ma Y, Chen H, Zhou Y, Zhang M, et al. Laparoscopy or not: A meta-analysis of the surgical effects of laparoscopic versus open appendicectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:362–70. doi: 10.1097/SLE.0b013e3182006f40. [DOI] [PubMed] [Google Scholar]
- 7.Karakousis GC, Singer S, Zheng J, Gonen M, Coit D, DeMatteo RP, et al. Laparoscopic versus open gastric resections for primary gastrointestinal stromal tumors (GISTs): A size-matched comparison. Ann Surg Oncol. 2011;18:1599–605. doi: 10.1245/s10434-010-1517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006;139:484–92. doi: 10.1016/j.surg.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Wu SD, Kong J, Su Y, Fan Y. Safety and application of transumbilical single-incision laparoscopic gastrectomy for GIST: SILS in benign gastric disease. Surg Innov. 2013;20:365–9. doi: 10.1177/1553350612455224. [DOI] [PubMed] [Google Scholar]
- 10.Grover S, Ashley SW, Raut CP. Small intestine gastrointestinal stromal tumors. Curr Opin Gastroenterol. 2012;28:113–23. doi: 10.1097/MOG.0b013e32834ec154. [DOI] [PubMed] [Google Scholar]
- 11.Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, et al. NCCN Task Force report: Update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010;8(Suppl 2):S1–41. doi: 10.6004/jnccn.2010.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hellman P, Lundström T, Ohrvall U, Eriksson B, Skogseid B, Oberg K, et al. Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastases. World J Surg. 2002;26:991–7. doi: 10.1007/s00268-002-6630-z. [DOI] [PubMed] [Google Scholar]
- 13.Givi B, Pommier SJ, Thompson AK, Diggs BS, Pommier RF. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery. 2006;140:891–7. doi: 10.1016/j.surg.2006.07.033. [DOI] [PubMed] [Google Scholar]
- 14.Boudreaux JP, Putty B, Frey DJ, Woltering E, Anthony L, Daly I, et al. Surgical treatment of advanced-stage carcinoid tumors: Lessons learned. Ann Surg. 2005;241:839–45. doi: 10.1097/01.sla.0000164073.08093.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pasieka JL. Carcinoid tumors. Surg Clin North Am. 2009;89:1123–37. doi: 10.1016/j.suc.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Edwards JP, Ho AL, Tee MC, Dixon E, Ball CG. Wound protectors reduce surgical site infection: A meta-analysis of randomized controlled trials. Ann Surg. 2012;256:53–9. doi: 10.1097/SLA.0b013e3182570372. [DOI] [PubMed] [Google Scholar]


