Abstract
CONTEXT:
Laparoscopic surgery is commonly used for the treatment of many pediatric surgical diseases at our department. Single-incision laparoscopic surgery (SILS) is well-known for its cosmetic benefit. We, hereby, present our experience of SILS and evaluate its efficacy.
MATERIALS AND METHODS:
From July 2012 to June 2014, 78 patients aged less than 18 years who underwent SILS were retrospectively evaluated. There were 44 males and 34 females, with a mean age of 10.3 years. The procedures included appendectomy (n = 64), reduction of intussusception (n = 8), removal of an intestinal foreign body (n = 3), and Meckel's diverticulectomy (n = 3). We compared the patients who underwent SILS with those who underwent conventional laparoscopic surgery (CLS), regarding these procedures. The parameters for analysis included the patient's demographic data, surgical indication, complications, operative time, and length of hospital stay.
CONCLUSION:
SILS is comparable to CLS regarding two major procedures, namely, appendectomy and reduction of intussusception. There were no significant differences between the two groups regarding the patients' demographic data, complications, and length of hospital stay. According to our experience of SILS, it could be a feasible and safe procedure for the treatment of various pediatric surgical diseases. However, large prospective randomized studies are needed to identify the differences between SIL and CLS.
Keywords: Conventional laparoscopic surgery (CLS), Single incision laparoscopic surgery (SILS), Appendectomy
INTRODUCTION
Laparoscopic surgery has been widely used for the treatment of many pediatric surgical diseases, and it has benefits that include a shorter hospital stay, reduced postoperative pain, and a reduced time for recovery as compared with conventional laparotomy. Single-incision laparoscopic surgery (SILS) has been attempted in many surgical fields to further improve the cosmetic and clinical outcomes. We, hereby, present our experience of SILS in children and compare the procedure with conventional laparoscopy in terms of its efficacy and feasibility.
MATERIALS AND METHODS
With the approval of our Institutional Review Board, the medical records of children who underwent SILS between July 2012 and June 2014 and CLS between January 2010 and June 2014 were retrospectively reviewed. Their demographic data, surgical details, and clinical outcomes were recorded.
SILS was performed as a modified procedure using a wound retractor, traditional surgical glove, and conventional laparoscopy equipment.[12] It was not associated with a marked increase in the medical cost.
Complicated cases, in which the addition of another trocar was necessary, were excluded. The differences between the two groups (SILS and CLS) were analyzed using IBM® SPSS® Statistics Version 20.0. The mean differences (MDs) with 95% confidence intervals (CIs) were calculated to assess the demographic data, operative time, and length of hospital stay. Pooled odds ratios (ORs) with 95% CIs were calculated for postoperative complications. A P value <0.05 was considered to indicate statistical significance.
RESULTS
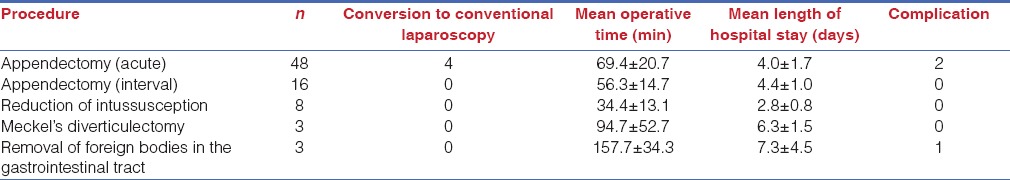
Seventy eight SILS procedures were performed during the 2-year period at our department. These comprised appendectomy (n = 64), reduction of intussusception (n = 8), removal of an intestinal foreign body (n = 3), and Meckel's diverticulectomy (n = 3). The surgical outcomes are shown in Table 1. Two complications in patients with acute appendicitis were a residual abscess and the need for a longer duration of antibiotic treatment. The abscess was identified by abdominal echo imaging. The three cases involving the removal of foreign bodies from the gastrointestinal tract included one patient with gastric trichobezoar and two with multiple magnets in the intestine. One associated complication was wound infection with ventral hernia in a patient with intestinal perforation due to magnets; however, this complication had subsided without surgery at the follow-up.
Table 1.
SILS outcome
In the CLS group, the procedures included simple appendectomy without drainage (n = 246) and reduction of intussusception (n = 15). Complications associated with the cases of acute appendicitis included wound infection (n = 7) and abscess (n = 12).
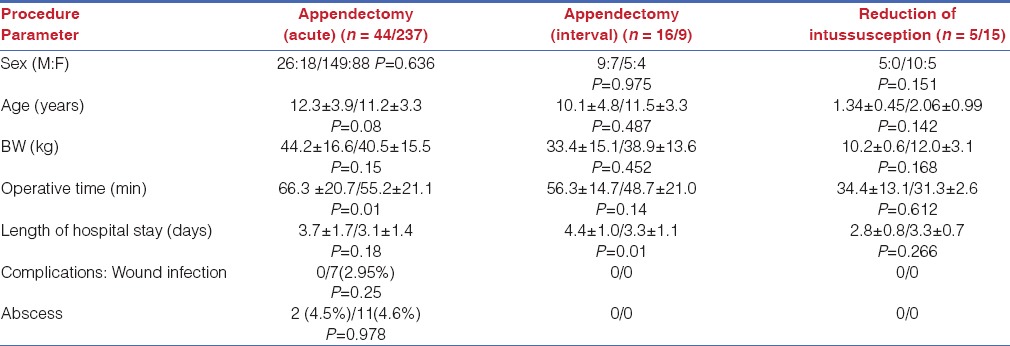
Among the patients who underwent appendectomy, four who underwent SILS and required placement of another trocar were excluded. Among the cases of intussusception in the SILS group, three were excluded for conversion to the assisted method by extension of umbilical wound for 1~2 cm to manage the leading point. Two of them were Meckel's diverticulum and the other one was intestinal lymphoma. In addition, we separated the appendectomy cases into two subgroups, namely, acute appendicitis and interval appendectomy due to their markedly different compositions. The cases of interval appendectomy accounted for 26.7% (16/60) of the SILS group and 3.66% (9/246) of the CLS group. There was no significant difference in gender, age, or body weight (BW) between SILS and CLS in the three groups [Table 2]. No patient was converted to the open method in these groups. In the acute appendicitis group, a longer operative time was noted with SILS but the length of hospital stay and complication rate in SILS showed no significant difference. However, in the interval appendectomy group, a greater length of hospital stay was noted with SILS but the operative time of SILS did not differ significantly compared to that of CLS. In the intussusception cases, no significant difference was noted in the operative time and length of hospital stay between SILS and CLS [Table 2].
Table 2.
Comparison between SILS/CLS
DISCUSSION
SILS has been used in several procedures, e.g., appendectomy,[1] ileostomy, colostomy,[2] colectomy,[3] intestinal anastomosis,[4] cholecystectomy,[5] adrenalectomy,[6] gastrectomy,[7] splenectomy,[8] and urologic surgery.[9] Both the public and patients favor SILS over CLS.[10,11]
In the SILS group, the clinical outcomes indicated no significant side effects and acceptable results. Removal of the intestinal foreign bodies was performed in two cases with multiple magnets and one case with gastric trichobezoar. Among the four cases of conversion to CLS in appendectomy, three required the placement of another trocar for the insertion of drainage and the other case required trocar for severe adhesion in interval appendectomy. Although some studies have reported a method involving the placement of a drainage tube via the umbilical wound directly instead of placing another trocar,[12] we did not adopt this method in the present study.
A recent meta-analysis reported similar postoperative morbidity and wound infection rates for single-incision laparoscopic appendectomy and conventional laparoscopy, but single-incision surgery required a longer operative time.[13] In our study, the same result was noted in the cases of acute appendicitis but not interval appendectomy. The benefit of single-incision laparoscopic appendectomy is cosmetic satisfaction, while its disadvantages are a longer operative time and a higher conversion rate.[14] In addition, single-incision laparoscopic appendectomy was reported in a randomized prospective study to lead to early recovery.[12] The conversion rate for single-incision laparoscopic appendectomy in published studies ranged 0-41%; the conversion rate in this study was 6.25%.
CONCLUSION
SILS is comparable to CLS for treatment of selected cases of acute appendicitis, interval appendectomy, and intussusception. There was no significant difference between the two groups in terms of complication rates and the clinical outcomes were acceptable. Our experience of SILS suggests it to be a feasible and safe procedure for the treatment of various pediatric surgical diseases. However, large, prospective, randomized studies are needed to evaluate the differences between SILS and CLS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Raakow R, Jacob DA. Initial experience in laparoscopic single-port appendectomy: A pilot study. Dig Surg. 2011;28:74–9. doi: 10.1159/000322921. [DOI] [PubMed] [Google Scholar]
- 2.Shah A, Moftah M, Hadi Nahar Al-Furaji H, Cahill RA. Standardized technique for single port laparoscopic ileostomy and colostomy. Colorectal Dis. 2014;16:O248–52. doi: 10.1111/codi.12601. [DOI] [PubMed] [Google Scholar]
- 3.Costedio MM, Remzi FH. Single-port laparoscopic colectomy. Tech Coloproctol. 2013;17(Suppl 1):S29–34. doi: 10.1007/s10151-012-0935-1. [DOI] [PubMed] [Google Scholar]
- 4.Naqi SA, Smyth J, Mortensen N, Hompes R, Cahill R. Single-incision laparoscopic ileorectal anastomosis. Colorectal Dis. 2014;16:O297–9. doi: 10.1111/codi.12584. [DOI] [PubMed] [Google Scholar]
- 5.Vilallonga R, Barbaros U, Sümer A, Demirel T, Fort JM, González O, et al. Single-port transumbilical laparoscopic cholecystectomy: A prospective randomised comparison of clinical results of 140 cases. J Minim Access Surg. 2012;8:74–8. doi: 10.4103/0972-9941.97586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vidal O, Astudillo E, Valentini M, Ginestá C, Espert JJ, Gracía-Valdecasas JC, et al. Single-port laparoscopic left adrenalectomy (SILS): 3 years' experience of a single institution. Surg Laparosc Endosc Percutan Tech. 2014;24:440–3. doi: 10.1097/SLE.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 7.Mittermair R, Pratschke J, Sucher R. Single-incision laparoscopic sleeve gastrectomy. Am Surg. 2013;79:393–7. [PubMed] [Google Scholar]
- 8.Gkegkes ID, Mourtarakos S, Iavazzo C. Single-incision laparoscopic splenectomy. JSLS. 2014;18:pii: e201400350. doi: 10.4293/JSLS.2014.00350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherif H, El-Tabey M, Abo-Taleb A, Abdelbaky A. Single-incision laparoscopic surgery in urology. Curr Urol. 2012;6:8–14. doi: 10.1159/000338862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fransen SA, Broeders E, Stassen L, Bouvy N. The voice of Holland: Dutch public and patient's opinion favours single-port laparoscopy. J Minim Access Surg. 2014;10:119–25. doi: 10.4103/0972-9941.134874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dauser B, Görgei A, Stopfer J, Herbst F. Conventional laparoscopy vs. single port surgery from a patient's point of view: Influence of demographics and body mass index. Wien Klin Wochenschr. 2012;124:834–41. doi: 10.1007/s00508-012-0299-6. [DOI] [PubMed] [Google Scholar]
- 12.Liang HH, Hung CS, Wang W, Tam KW, Chang CC, Liu HH, et al. Single-incision versus conventional laparoscopic appendectomy in 686 cases: A retrospective comparative analysis. Can J Surg. 2014;57:E89–97. doi: 10.1503/cjs.023812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antoniou SA, Koch OO, Antoniou GA, Lasithiotakis K, Chalkiadakis GE, Pointner R, et al. Meta-analysis of randomized trials on single-incision laparoscopic versus conventional laparoscopic appendectomy. Am J Surg. 2014;207:613–22. doi: 10.1016/j.amjsurg.2013.07.045. [DOI] [PubMed] [Google Scholar]
- 14.Cai YL, Xiong XZ, Wu SJ, Cheng Y, Lu J, Zhang J, et al. Single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy: Systematic review and meta-analysis. World J Gastroenterol. 2013;19:5165–73. doi: 10.3748/wjg.v19.i31.5165. [DOI] [PMC free article] [PubMed] [Google Scholar]


