Abstract
Gastrointestinal stromal tumour (GIST) involving rectum is rare. No definite method of treatment has been established because of a small number of cases being reported. It is usually managed with invasive or ablative surgery, such as abdominoperineal resection (APR). The acceptance of minimally invasive (laparoscopic) surgery in colorectal disease plays a pivotal role in improving the postoperative quality of life. We report a case of a large lower rectal GIST who underwent laparoscopic excision of tumour through a subserosal approach whilst preserving the anal sphincter and without any rectal resection.
Keywords: Laparoscopy, rectal GIST, subserosal excision
INTRODUCTION
The acceptance of minimally invasive laparoscopic surgery in colorectal disease plays a pivotal role in improving the postoperative quality of life for those undergoing colorectal surgery. The incidence of rectal gastrointestinal stromal tumour (GIST) is 0.1%. Definitive treatment of rectal GIST is not well-established. GIST of lower rectum is usually managed with invasive or ablative surgery such as abdominoperineal resection (APR). We report a case of a large lower rectal GIST who underwent laparoscopic excision of tumour through a subserosal approach whilst preserving the anal sphincter and without any rectal resection.
CASE REPORT
A 66-year-old male patient, diabetic and hypertensive, presented with a history of (h/o) constipation since 6 months and retention of urine. No other symptoms were present. The patient had a past h/o open appendicectomy in childhood. After initial assessment, indwelling urinary catheter was introduced for the chronic retention of urine. Per abdominal examination was unremarkable, except for an infraumbilical right paramedian surgical scar. Per rectal examination revealed a firm, immobile, non-tender mass with a smooth surface (extramural) in the right posterolateral region, 3 cm from the anal verge with significant luminal narrowing. Routine blood tests were normal. Magnetic resonance imaging (MRI) abdomen and pelvis showed large well-circumscribed nodular mass measuring 6.3 cm × 5.4 cm × 6.7 cm in the right lateral intramural segment of the rectal wall [Figure 1]. The lesion was 3 cm from the anal verge. Sigmoidoscopy revealed an indentation in the right lateral wall with normal mucosa and a small sigmoid diverticula.
Figure 1.

MRI pelvis
The patient was diagnosed to have large leiomyoma of the lower rectum and was advised surgery. Various surgical options were discussed, but the patient firmly refused any ablative procedure needing a permanent stoma, such as APR. After thorough preoperative evaluation and counselling, the patient underwent laparoscopic excision of the tumour. Four ports (two 10 mm and 5 mm ports) were placed [Figure 2a]. Rectal mobilization was done with a harmonic scalpel and revealed smooth surfaced tumour in the right posterolateral wall below the peritoneal reflection. It was well-encapsulated without any infiltration of seminal vesicles or the prostate [Figure 2b]. After dissecting the rectal serosa with harmonic scalpel, the tumour was delivered through the serosal opening by maneuvering per rectally by an assistant. Tumour was excised with capsule intact and was placed in an endobag and removed piecemeal through a 10-mm umbilical port. There was no breach in the rectal lumen as confirmed by a leak test (gas insufflation). Serosa was not sutured, as there was a wide gap between the edges. Covering loop ileostomy was done. Total operative time was 2 h. Intraoperative blood loss was approximately 100mL. Postoperative stay was uneventful and patient was discharged on the 4th postoperative day in a stable condition. Histopathological findings revealed spindle-shaped cells with elongated fusiform nuclei consistent with leiomyoma, with 4-5 mitoses/10 high-power fields (HPF), with no necrosis and no mucosal lining [Figure 3]. Immunohistochemistry (IHC) revealed cluster of differentiation (CD) 117 positive, Ki 67 15-20% and desmin-negative, hence diagnosed as GIST postoperatively. A medical oncologist's opinion was sought and was advised for adjuvant imatinib therapy. Neoadjuvant imatinib therapy was not considered as the diagnosis of GIST was confirmed only postoperatively, after the IHC report.
Figure 2.
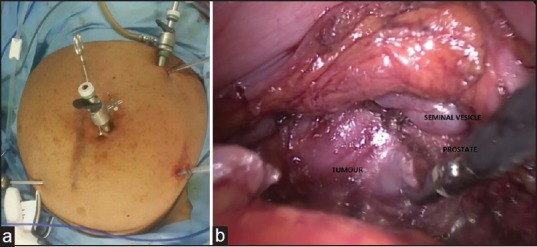
(a) Port placement (b) Laparoscopic view of the tumour
Figure 3.
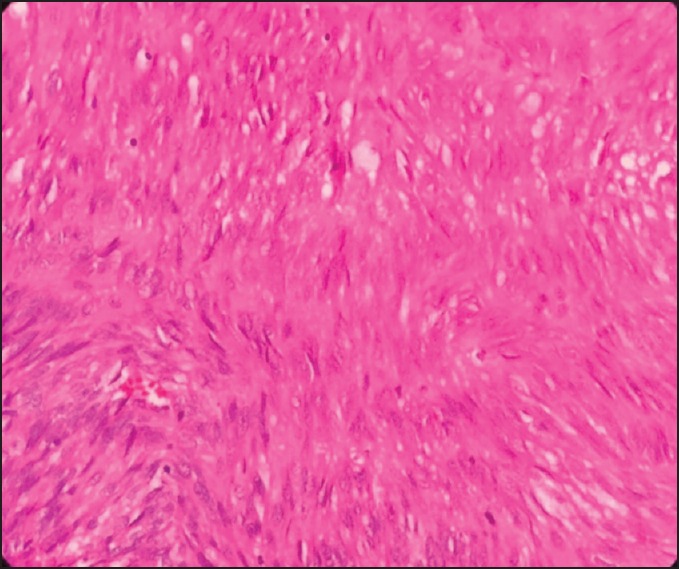
Tumour histopathology
DISCUSSION
GIST is an uncommon tumour of gastrointestinal tract, very rarely involves the rectum (5%).[1] Rectal GIST makes up 0.1% of all the rectal tumours.[1] They have poor outcome when compared to gastric or small intestinal GISTs. Surgical resection is the main modality of treatment for localized GISTs. Complete resection of rectal GISTs can be difficult if they are of a large size, adheres to surrounding structures or the pelvic floor or its anatomical location and is in close proximity with sphincter muscles. Prior treatment with imatinib, followed by surgical resection, has been reported for GISTs where en bloc resection was difficult.[2]
Laparoscopic colorectal surgery is beneficial because of the minimized access trauma and in addition, magnification provides more precise image of the area of dissection and improves the accuracy of surgery. Adequate visualization between the tumour and the seminal vesicles/prostate is difficult in laparotomy and can be achieved in laparoscopy. Few cases of lower rectal GISTs resected by laparoscopic surgery with sphincter-saving procedures have been described. Fujimoto et al. described five laparoscopic intersphincteric resections of rectal GISTs following imatinib treatment for 4-12 months.[3] They mentioned that laparoscopic surgery was found to be safe and feasible for downsized GISTs. Miettinen et al. reported 122 patients with rectal GIST. A number of 15 (12%) patients underwent anterior resection and 24 (20%) patients underwent local resection for tumours >5 cm.[4] No definite method of treatment of rectal GIST has been established because of the small number of such cases.[5] In our patient, laparoscopic approach facilitated magnified visualization of the tumour on the posterolateral wall of rectum. A laparoscopic approach for such a large GIST in the lower rectum as seen in our patient was considered ideal to enable sphincter preservation and continence. An open approach, due to space constraints in an android pelvis, would have led to either an APR or partial ablation of the sphincter and possible subsequent incontinence; as per our knowledge, we believe the present patient represents the first case of a lower rectal large GIST treated by laparoscopic excision of GIST without compromising on sphincter activity and need for rectal resection. While the primary objectives of complete tumour excision and preservation of sphincter integrity were met by the laparoscopic approach, the patient will need adjuvant chemotherapy and long-term follow-up is mandatory for optimal results.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank Dr. Veena, Department of Pathology, Fortis Hospitals, Bannerghatta Road, Bengaluru, Karnataka, India, for her guidance in preparing this manuscript.
REFERENCES
- 1.Miettinen M, Lasota J. Gastrointestinal stromal tumors — Definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1–12. doi: 10.1007/s004280000338. [DOI] [PubMed] [Google Scholar]
- 2.Nozawa H, Kanazawa T, Tanaka T, Takahashi M, Ishihara S, Sunami E, et al. Laparoscopic resection of a gastrointestinal stromal tumor of the lower rectum in a patient with coronary artery disease following long-term neoadjuvant imatinib treatment and anticoagulation therapy. World J Surg Oncol. 2014;12:211. doi: 10.1186/1477-7819-12-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fujimoto Y, Akiyoshi T, Konishi T, Nagayama S, Fukunaga Y, Ueno M. Laparoscopic sphincter-preserving surgery (intersphincteric resection) after neoadjuvant imatinib treatment for gastrointestinal stromal tumor (GIST) of the rectum. Int J Colorectal Dis. 2014;29:111–6. doi: 10.1007/s00384-013-1769-7. [DOI] [PubMed] [Google Scholar]
- 4.Miettinen M, Virolainen M, Maarit-Sarlomo-Rikala Gastrointestinal stromal tumors — Value of CD34 antigen in their identification and separation from true leiomyomas and schwannomas. Am J Surg Pathol. 1995;19:207–16. doi: 10.1097/00000478-199502000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Nakamura T, Ihara A, Mitomi H, Kokuba Y, Sato T, Ozawa H, et al. Gastrointestinal stromal tumor of the rectum resected by laparoscopic surgery: Report of a case. Surg Today. 2007;37:1004–8. doi: 10.1007/s00595-007-3509-5. [DOI] [PubMed] [Google Scholar]


