Abstract
Osteoma is a slow growing benign tumor result from either cancellous or compact bone proliferation. Osteoma of the jaws may arise from the surface of the bone as a sessile mass located either peripherally or endosteally. This paper presents a rare case report of peripheral cancellous osteoma, involving the buccal cortical plate and alveolar process of the right maxilla of a 37-year-old female patient.
Keywords: Cancellous, maxilla, osteoma, periodontal flap
INTRODUCTION
Osteomas are benign osteogenic lesions of bone.[1,2,3] Histopathologically, osteoma is categorized as compact osteoma and cancellous osteoma, and depending on the location, it can be categorized as peripheral (periosteal) osteoma, central (endosteal) osteoma, and extraskeletal growth. Osteoma cutis is an example of extraskeletal lesion typically located within muscle or the dermis of the skin. Osteoma involves more frontal sinus in comparison to ethmoid and maxillary sinus. In regard to the osteoma of the jaws, mandibular involvement is more in comparison to maxilla. The lingual aspect of the mandibular body and inferior border of the angle of mandible are the most common affected sites in mandible.[4] Here, we are presenting intraoral peripheral cancellous osteoma affecting the maxilla of a 37-year-old female patient. To the best of our knowledge, this is the latest report of peripheral osteoma (PO) involving maxilla (posterior buccal cortical plate and alveolar process of right side of maxilla), and its cancellous variety make this case more rare.
CASE REPORT
A 37-year-old female patient presented with complaints of swelling over the face at the right side. Swelling was not remarkable extraorally and was present just below the line drawn from the corner of the lip to the ala of the nose [Figure 1]; an intraoral firm mass on the posterior right buccal surface of maxilla since past 2 years was also noted [Figure 2]. The swelling started with a size of a peanut and gradually and steadily increased in size. No previous history of any trauma, pain, or paresthesia at the site of the swelling was reported. There was no history of diabetes and hypertension. Submental and submandibular lymph nodes were not palpable. On intraoral examination, there was presence of solitary, elliptical growth over the buccal cortical plate and alveolar process of the right side of the maxilla in relation with 15, 16, 17 region. The overlying mucosa was normal but appeared stretched. The swelling was smooth, immobile, nontender, and hard in consistency. The overlying mucosa was firmly adhered to the swelling. The swelling was extending from the cervical margin of 15, 16, 17 apically to the mucogingival junction [Figure 2]. The pulp vitality of maxillary right molars was positive.
Figure 1.

Extraoral presentation of peripheral cancellous osteoma
Figure 2.

Intraoral exophytic mass located on the right maxillary buccal cortical plate
On the basis of history, sex of the patient, site of the lesion (posterior maxillary buccal cortical and alveolar process), and clinical finding of unilaterally expansile mass, a provisional diagnosis of fibrous dysplasia was given with a differential diagnosis of exostoses, peripheral osteoma, osteoid osteoma, and osteoblastoma. On radiographic examination, Intraoral periapical (IOPA) view revealed a less dense radiopaque shadow, superimposing the occlusal surface of 15, 16, 17, extending occlusally. Right lateral cross-sectional occlusal view of maxilla [Figure 3] revealed well-defined, solitary, elliptical shape approximately 3 × 1.5 cm in area seen in relation to the buccal cortical plate of 15, 16, 17. The overall internal structure of the lesion appeared to be more homogenously radiopaque in the posterior two-third of the lesion with an increased number of uniformly arranged trabeculae, whereas anteriorly less homogenous with fewer trabeculae.
Figure 3.

Right lateral cross-sectional occlusal view of the maxilla showing well defined, solitary elliptical radio-opaque mass in relation to the buccal cortical plate of 15,16,17 with varying density
Under local anesthesia [(lignocaine 2% with adrenaline; 1 in 800,000 concentration), posterior and middle superior alveolar nerve block and local infiltrations were given] via an intraoral approach, the mucoperiosteal flap was raised and the lesion was totally excised, from distal to14 up to mesial of 18 region, using a chisel–mallet and rotary instrument. Postoperatively, the patient was advised to take soft and cold food and follow proper course of antibiotic and anti-inflammatory drugs. Patient was followed-up after 7 days. She recovered without any complications.
The surgical excised tissue was sent to the histopathology lab. On macroscopic examination, the excised tissue was bony hard, elliptical shaped, and measured approximately 3 × 1.5 cm [Figure 4]. The microscopic examination of hematoxylin and eosin stained section at high-power magnification showed numerous bony trabeculae of cancellous bone with abundant fibrofatty tissue. Few areas showed bony trabeculae with osteoblastic rimming. Overall, clinicopathological features were suggestive of cancellous osteoma [Figure 5].
Figure 4.
Surgically excised lesion of peripheral osteoma
Figure 5.
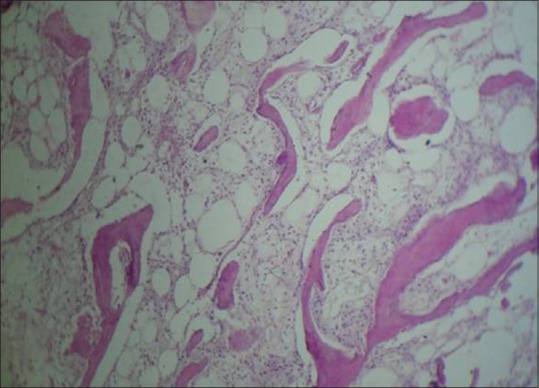
Photomicrograph showing mature bony trabeculae with variable amount of fibrofatty bone marrow (H and E stain, ×40)
DISCUSSION
Osteoma is slow growing bony lesion composed of either mature compact and cancellous bone.[5] Most of the jaw osteomas are seen in young adult but can arise at any age. The osteoma lesions in general are solitary and asymptomatic without sex predilection.[4] Kaplan et al., in their case series, found a male-to-female ratio of 2:1.[6] Maxillary osteoma involvement is lesser than the mandibular osteoma.[7,8,9,10] Thus, in our case report, maxillary osteoma with its peripheral cancellous variety makes it a rarer entity. The rare occurrence of osteoma in maxilla can be explained because only very few cases of maxillary osteoma specially with its cancellous variant have been reported till now.[3,5,11] In our case, intraoral examination revealed a well-defined, solitary, elliptical mass over the buccal cortical plate and alveolar process of the right-side of maxilla in relation with 15, 16, 17 region.
Clinically, PO is smaller (10–40 mm) in size, however, if left untreated, they can grow to larger size and can be described as gigantiform or huge osteoma.[8,12] With larger lesions, patient may present with complaints of facial deformity and occlusal dysfunction.[3,6] In our case, though asymptomatic in nature, swelling extended up to the occlusal level, creating discomfort during mastication. Regarding pathogenesis of PO, various theories have been suggested such as reactive condition triggered by trauma, developmental or embryological, and inflammatory. In many of the cases, patients are unable to recall the past history of trauma. In addition, it has been suggested that chronic infection involving paranasal sinuses is responsible for the proliferation of osteogenic cells. According to the embryological theory, it has been suggested that osteomas could originate from the sutures present between bones with various embryological derivation (endrochondral/membranous), however, it is very rare because osteoma mostly occurs in adults and not in children. It has been also suggested that, because PO is located near to the muscle attachment area, muscle traction could be the possible cause of PO. Thus, muscle traction in combination with trauma was also suggested as a one of the cause of pathogenesis of PO.[5,9,13]
Conventional radiographic images are generally adequate in diagnosing an osteoma, which shows the well-circumscribed radio-opaque mass affected cortical bone. In addition to panoramic radiograph, Waters view or tomograms usually helps to reveal the lesion. The computerized tomography (CT) scan also shows the details of the osteoma location in a better manner, especially with three-dimensional reconstruction.[9,14,15,16] In the present case, right lateral cross-sectional occlusal view of maxilla radiograph revealed the bony mass.
Because of the negative history of trauma, etiopathogenesis of osteoma was correlated with development at that site. Peripheral maxillary cancellous osteoma is a different entity from other bony lesions such as exostoses, monostotic fibrous dysplasia, osteoid osteoma, and osteoblastoma. Exostoses are bony overgrowth such as mandibular tori. Typical histological features of fibrous dysplasia is helpful to differentiate it from PO; osteoblastoma and ostoid osteoma grow more rapidly and are more painful than PO.[16,17] The patients with peripheral osteoma should be examined to rule out Gardner's syndrome (GS) which is an autosomal dominant syndrome that shows the presence of polyps in the gastrointestinal area, several osteomas, soft tissue tumors, skin tumors, and supernumerary multiple impacted teeth.[17,18,19] Our patient did not report any such findings, and there were neither intestinal problems nor impacted or supernumerary teeth.
Treatment of choice is surgical removal from the base of the lesion. Till now, malignant transformation of osteoma has not been reported.[17] The recurrence rate of osteoma is very rare.[20] Osteoma are believed to be relatively uncommon and most of them are compact variety[6,7,8,9,12,14,17,18,19,20,21,22] and cancellous type of osteoma is very rare.[2,3,5,11,23] Our patient of peripheral cancellous osteoma recovered without any complication after surgery, and there was no evidence of recurrence during 2 years of follow-up.
CONCLUSION
PO of the maxilla is relatively rare and its cancellous type of proliferation is extremely rare case. They present as slow growing, well-circumscribed, and lobulated masses. Simple X-ray is sufficient to provide diagnostic information, and its histopathologic features are the main diagnostic tool. Simple excision of the lesion in its entirety is the treatment of choice; the recurrence is very rare. The association of osteoma with Gardner's syndrome must always be kept in mind before deciding the treatment plan.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shafer WG, Hine MK, Levy BM. Shafer's Textbook of oral pathology. 7th edition. Elsevier; 2012. pp. 154–6. [Google Scholar]
- 2.Batra N, Batra R, Gaur A. Peripheral osteoma of maxilla: A case report. Natl J Maxillofac Surg. 2014;5:240–2. doi: 10.4103/0975-5950.154848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sah K, Kale A, Seema H, Kotrashetti V, Pramod BJ. Peripheral osteoma of the maxilla: A rare case report. Contemp Clin Dent. 2011;2:49–52. doi: 10.4103/0976-237X.79299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neville W, Damm D, Allen C, Bouquot JE. Oral & maxillofacial pathology. 3rd edition. Elsevier; 2011. pp. 650–1. [Google Scholar]
- 5.Durighetto AF, Jr, de Moraes Ramos FM, da Rocha MA, da Cruz Perez DE. Peripheral osteoma of the maxilla: Report of a case. Dentomaxillofac Radiol. 2007;36:308–10. doi: 10.1259/dmfr/52795470. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan I, DMD, Nicolaou Z, Hatuel D, Calderon Solitary central osteoma of the jaws: A diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e22–9. doi: 10.1016/j.tripleo.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Shakya H. Peripheral Osteoma of the Mandible. J Clin Imaging Sci. 2011;1:56. doi: 10.4103/2156-7514.90483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogbureke KU, Nashed MN, Ayoub AF. Huge peripheral osteoma of the mandible: A case report and review of the literature. Pathol Res Pract. 2007;203:185–8. doi: 10.1016/j.prp.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Dalambiras S, Boutsioukis C, Tilaveridis I. Peripheral osteoma of the maxilla: Report of an unusual case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:e19–24. doi: 10.1016/j.tripleo.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. Diagnosis and management: A study of 14 cases. Med Oral Patol Oral Cir Bucal. 2005;10(Suppl 2):E139–42. [PubMed] [Google Scholar]
- 11.Chaudhry J, Rawal SY, Anderson KM, Rawal YB. Cancellous osteoma of the maxillary tuberosity: Case report. Gen Dent. 2009;57:427–9. [PubMed] [Google Scholar]
- 12.Kaya GS, Omezli MM, Sipal S, Ertas U. Oral myiasis: Gigantic peripheral osteoma of the mandible: A Case report. J Clin Exp Dent. 2010;2:e160–2. [Google Scholar]
- 13.Regezi JA, Sciubba JJ, Jordan RCK. Patologia bucal: Correlações clínico-patológicas. 5th ed. Rio de Janeiro: Guanabara Koogan; 2008. pp. 452–3. [Google Scholar]
- 14.Agrawal R, Agrawal S, Bhargava S, Motlani M, Agrawal R. An Uncommon Case of Solitary Peripheral Osteoma in the Mandible. Case Rep Dent 2015. 2015:319738. doi: 10.1155/2015/319738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White SC, Pharoah MJ. Oral Radiology, Principles & Interpretation. 5th edition. Elsevier, Mosby Inc; 2004. p. 443. [Google Scholar]
- 16.de Franca TR, Gueiros LA, de Castro JF, Catunda I, Leao JC, da Cruz Perez DE. Solitary peripheral osteomas of the jaws. Imaging Sci Dent. 2012;42:99–103. doi: 10.5624/isd.2012.42.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prabhuji ML, Kishore HC, Sethna G, Moghe AG. Peripheral osteoma of the hard palate. J Indian Soc Periodontol. 2012;16:134–7. doi: 10.4103/0972-124X.94623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ragupathy K, Priyadharsini I, Sanjay P, Yuvaraj V, Balaji TS. Peripheral osteoma of the body of mandible: A case report. J Maxillofac Oral Surg. 2015;14:1004–8. doi: 10.1007/s12663-014-0710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kshirsagar K, Bhate K, Pawar V, SanthoshKumar SN, Kheur S, Dusane S. Solitary peripheral osteoma of the angle of the mandible. Case Rep Dent 2015. 2015:430619. doi: 10.1155/2015/430619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shetty SK, Biddappa L. Recurrence of a giant peripheral osteoma of mandible. J Maxillofac Oral Surg. 2015;14((Suppl 1)):452–6. doi: 10.1007/s12663-014-0674-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim DY, Oh KS. A rare case of peripheral osteoma of the zygoma. Arch Plast Surg. 2015;42:103–5. doi: 10.5999/aps.2015.42.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rao S, Rao S, Pramod DS. Transoral removal of peripheral osteoma at sigmoid notch of the mandible. J Maxillofac Oral Surg. 2015;14((Suppl 1)):255–7. doi: 10.1007/s12663-013-0472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weihsin HU, Thadani S, Agrawal M, Sharma N, Tailor S. Peripheral osteoma of the palate: Report of a case and review of literature. J Clin Diagn Res. 2014;8:ZD29–31. doi: 10.7860/JCDR/2014/7888.5351. [DOI] [PMC free article] [PubMed] [Google Scholar]


