Abstract
Background:
Radiologic data remains the gold standard for the diagnosis of pneumothorax (PTX). The use of ultrasonography (US) has recently emerged as the method of choice with physicians who can perform bedside US.
Purpose:
To compare the diagnostic accuracy of lung US against bedside chest radiography (CR) for the detection of PTX using thoracic computed tomography (CT) as the gold standard.
Materials and Methods:
We conducted a prospective, single-blind study on 192 critically ill patients; each patient received lung US examination, bedside CR, followed by thoracic CT scan searching for PTX.
Results:
Of the studied patients, CT of the chest confirmed the diagnosis of PTX in 36 (18.75%) patients of which 31 were diagnosed by thoracic US while CR detected only 19 cases. Overall lung US showed a considerable higher sensitivity than bedside CR (86.1% vs. 52.7%), lung US also showed higher, negative predictive values, and diagnostic accuracy against CR (96.8% vs. 90.1%), and (95.3% vs. 90.6%), respectively. CR had a slightly higher specificity than lung US (99.4% vs. 97.4%), and higher positive predictive values (95.0% vs. 88.6%).
Conclusion:
Lung US is an accurate modality more than anteroposterior bedside CR in comparison with CT scanning when evaluating critically ill mechanically ventilated patients, patients underwent thoracocentesis, central venous catheter insertion, or patients with polytrauma.
Keywords: Intensive Care Unit, lung ultrasound, mechanical ventilation, pneumothorax
Introduction
Pneumothorax (PTX) is defined as the presence of air within the pleural space and is a common problem in the Intensive Care Units (ICU). Pneumothoraces can occur spontaneously, as a result of trauma, or from iatrogenic causes such as central venous catheter insertion, mechanical ventilation, thoracocentesis, and lung biopsy.
The prevalence of PTX in mechanically ventilated patients is high ranging from 4% to 15%[1,2] and it is considered as one of the most serious complications of positive pressure ventilation. Traumatic PTX is also commonly seen in the ICU. It is the second most common sign of chest trauma following rib fracture, and its incidence is up to 50% of patients with chest trauma.[3]
Chest radiographs have traditionally been the first test ordered to both make and rule out the diagnosis of PTX in the setting of trauma or after invasive procedures.[4] In the critically ill, the supine or semi-recumbent anterior-posterior film is frequently obtained making the reliability of chest radiographs to be limited.[5,6] If there is doubt regarding the findings on a chest radiograph and the patient is stable, it is advised to conduct further imaging with ultrasonography (US) or chest computed tomography (CT) scan[7] [Figure 1]. Thoracic CT scan is considered the gold standard test for both diagnosing and determining the size of PTX.[8] However, it is expensive and cannot be performed on a routine basis. In addition, the transportation of critically ill patients and exposure to radiation carries a measurable risk [Figure 2].
Figure 1.
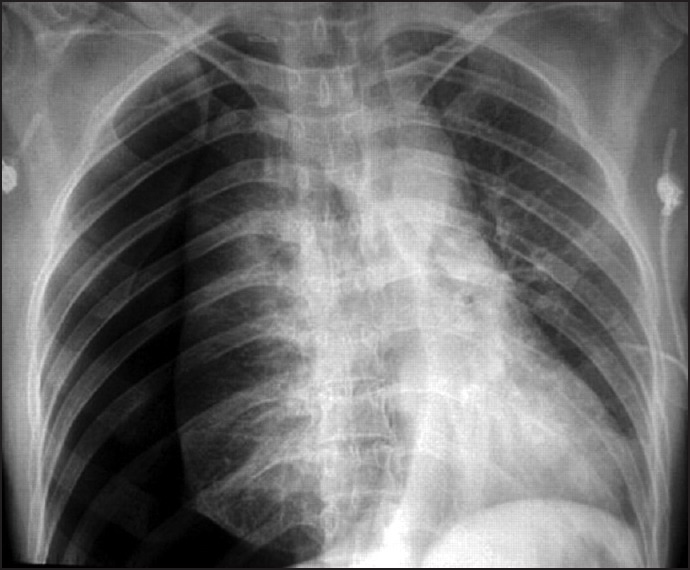
Chest radiograph showing right side pneumothorax
Figure 2.
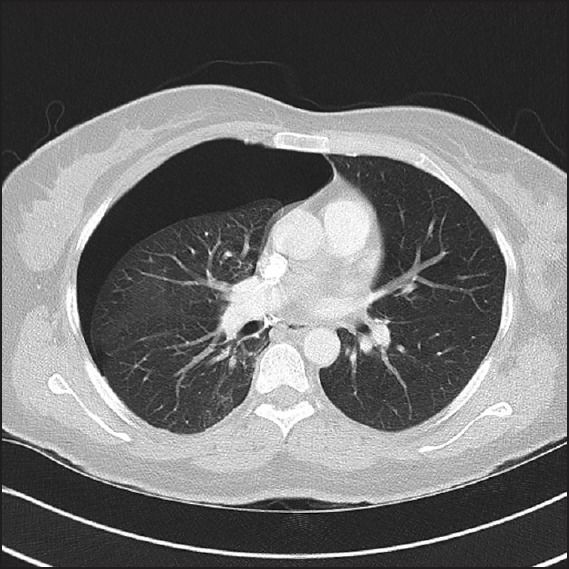
Thoracic computed tomography showing right side pneumothorax
The use of lung US for diagnosis of PTX has recently emerged as the method of choice with physicians who can perform bedside US.[9,10] There are many advantages of US over the standard chest radiography (CR) and CT scanning, including the absence of radiation, being portable, real-time imaging, and the ability to easily repeat evaluations. US has been used to rule out PTX after central line placement, as well as after transbronchial biopsy.[11,12] Though there is a learning curve associated with the use of chest US, it is relatively short.[13]
The aim of this study was to compare the sensitivity and specificity of bedside lung US with those for supine portable AP, CR, and thoracic CT scan (gold standard) for the detection of a PTX in critically ill patients.
Materials and Methods
After obtaining approval by Ain Shams University Hospital Ethics Committee, newly admitted critically ill patients at two ICU units; a medical-surgical ICU and a trauma ICU were enrolled in a prospective, single-blind study.
The study was conducted from March 2013 to July 2014. Enrollment criteria included adult patients admitted to the ICU and were at risk to develop PTX:
Mechanically ventilated patients with hypoxemia and/or elevated airway pressure.
Patients who underwent invasive procedures; thoracocentesis (pleural tapping) or central venous catheter insertion.
Polytraumatized patients who admitted to the ICU before imaging.
The final number of enrolled patients according to former criteria was 276 from which 13 patients were transferred died, before full radiological assessment by the used protocol, 69 patients could not perform CT scans due to hemodynamic instability, and two patients excluded from analysis ending by 192 patients completing the whole study [Flow Chart 1].
Flow Chart 1.
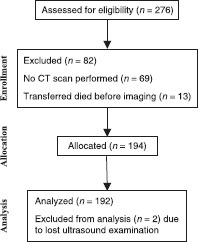
The consort E-flow chart
Study protocol
All the studied patients were evaluated by performing bedside US examinations of the chest using a 38 mm, 8-12 MHz broadband linear US probe GE Healthcare, LOGIQ C3 Premium® (Wauwatosa, Wisconsin, USA).
Images were obtained in a longitudinal scanning plane with the transducer indicator in a cephalad position along the mid-clavicular (2nd intercostal space), anterior axillary (4th intercostal space), mid-axillary (6th intercostal space), and posterior axillary (6th intercostal space) lines. Each line was scanned for 15-20 s, allowing a complete examination of each hemithorax to be performed in 60-80 s.
After selecting the B-mode, the intensivist who performed the examination placed the US probe perpendicular to the ribs on the anterior part of the chest, the bat sign was obtained showing 2 ribs in short axis, and the pleural line was identified as a hyperechoic line between the two rib shadows, lung sliding, and comet tail artifacts were checked during respiration. When lung sliding and comet tail artifacts were not seen, PTX was suspected and US was switched to M-mode seeking for the seashore sign [Figure 3]. When the seashore sign could not be seen, and instead a barcode sign [Figure 4] was viewed in the same location as the absence of both lung sliding, and comet tail artifacts, PTX was provisionally diagnosed.
Figure 3.
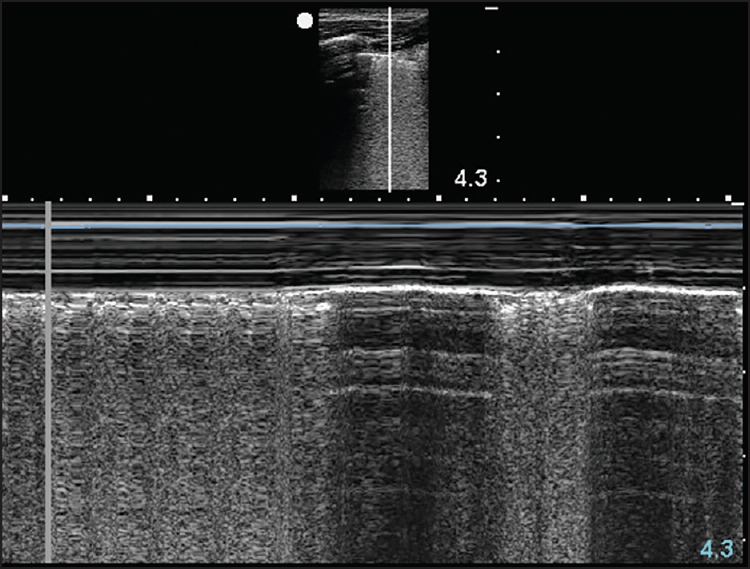
Lung ultrasound showing Seashore sign in a patient without pneumothorax
Figure 4.

Lung ultrasound showing barcode sign in a patient with pneumothorax
Portable, AP chest radiographs were obtained immediately after US evaluation. CT examination was obtained for the studied patients within 2 h. All examinations (lung US, thoracic CT, and CR) were performed while the patients were in the supine position.
Measurements
The intensivist who performed the US examination filled out a data form asking for his determination of the absence or presence of PTX in all examined lung fields, CR, and CT results were interpreted in the radiology department. The US performing physician was blinded to the CR and CT results until data collection was complete. Recorded US results were compared against both the reading of the CR and that of the CT. Radiologists were blinded to US results.
Statistical analysis
Variables were expressed as frequency, percentage, and mean ± standard deviation. Each lung region was evaluated and characterized as positive or negative for PTX. Each hemithorax was considered as positive or negative for PTX by the presence or absence of a single positive region, respectively. The results of thoracic US and chest X-ray were compared with the results of CT scan (considered to be the gold standard). Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy were calculated using standard formulas.
Results
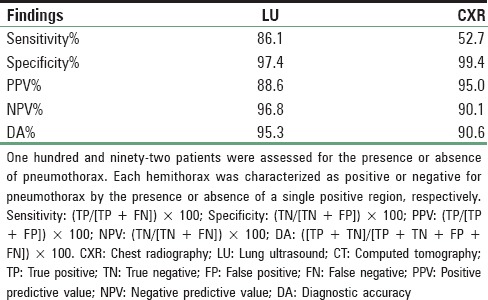
Characteristics of the patients enrolled in the study are shown in Table 1. A total of 192 patients were evaluated using the three image modalities; thoracic CT, lung US, and CR. Of the 192 patients, there were 89 mechanically ventilated patients with hypoxemia and/or elevated airway pressure, 44 polytraumatized patients, and 59 patients who underwent invasive procedures in the form of thoracocentesis or insertion of central venous catheters CT of the chest (considered the gold standard) confirmed the diagnosis of PTX in 36 (18.75%) patients of which 31 were diagnosed by thoracic US while only 19 patients detected by supine AP chest X-ray. Four of the five missed pneumothoraces by lung US were small, and did not require any intervention and one case necessitated chest tube insertion; in that case, there was 3-h delay between thoracic US and CT scan which might account for development of large PTX. There were four false positive cases; in all of them the pneumothoraces were considered to be small in size. Analysis of these cases revealed that three cases occurred in mechanically ventilated patients with severe chronic obstructive pulmonary disease and overinflation, and one patient had subcutaneous emphysema following blunt chest trauma. Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of lung US and CR are shown in Table 2. Overall lung US showed a considerable higher sensitivity than bedside CR (86.1% vs. 52.7%), it also showed higher, negative predictive values (96.8% vs. 90.1%), and diagnostic accuracy (95.3% vs. 90.6%). CR had a slightly higher specificity than lung US (99.4% vs. 97.4%), and higher positive predictive values (95.0% vs. 88.6%).
Table 1.
Patient's characteristics
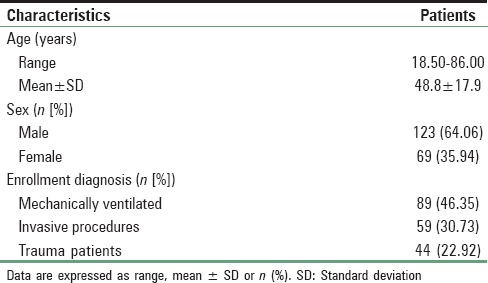
Table 2.
Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of CXR and LU as compared to CT scan
Discussion
The incidence of PTX among mechanically ventilated patients is high and is considered as one of the most serious complications of positive pressure ventilation. Thoracocentesis and central venous catheter insertion, both may induce PTX that might necessitate chest tube insertion for drainage. Traumatic PTX also is common in the ICU and it occurs, especially with chest trauma.
This study showed that thoracic US is more accurate than CR in detecting PTX both in critically ill mechanically ventilated and in polytraumatized patients. To make accurate diagnosis using US, we examined four points in each hemithorax and all intensivists involved in the study had passed both training program and sufficient supervised clinical practice before starting the study (100 examinations at least). We also used the high frequency linear US probe for better imaging quality and easy detection of presence or absence of lung sliding and comet tail signs. Switching to M-mode made the diagnosis easier, especially in difficult cases such as obese patients or patients with surgical emphysema.
In a study on 176 blunt trauma patients, attending emergency physicians performed bedside trauma US examinations using a microconvex US transducer to determine the presence of a sliding lung sign to rule out PTX, their results were higher as compared to ours as regard sensitivity of US for the detection of PTX.[14]
In another study by Garofalo et al., on a series of 184 patients who underwent chest US after percutaneous needle biopsy. US findings were compared with CT and to X-rays. Their results showed that PTX was identified in 46 patients by CT, in 44 by US, with no false positives, and in 19 by X-rays. US sensitivity, specificity, and diagnostic effectiveness were all higher than our results in spite of using the low frequency curved US probe.[15]
Chung and coworkers published a study comparing the detectability of high-resolution ultrasound (HRUS) and bedside CR for a PTX on 97 patients who underwent a transthoracic needle aspiration and biopsy (TNAB) of the lung. From 97 patients, 35 PTX cases were found on CT after the TNAB. The sensitivities in detecting the PTX were 80% and 47% in HRUS and CR, respectively. The specificities were 94% and 94%, respectively, and the diagnostic accuracies were 89% and 77%, respectively. In this study, the operator was a radiologist, and the probe used was the linear probe as the one utilized in our study and their results as regard US and CR use for the detection of PTX was comparable to our results in spite of different type of patients.[16]
Another group of radiologists compared the accuracy of US with that of supine CR in the detection of traumatic pneumothoraces, with CT as the reference standard using linear probe for diagnosis of PTX on 27 blunt thoracic trauma. Results showed that sensitivities of US as compared to CR were 100% and 36.4%, respectively. One false-positive US case, while at CR no false-positive case was detected with a resultant specificity of 93.8 % for US and 100% for CR.[17]
A study by Zhang et al. aimed to detect and assess the size of the PTX in polytraumatized patients using bedside US using low frequency curved probe. The diagnostic efficacy of US and CR for the detection of PTX, were compared to results of CT and chest drain as the gold standard. Results showed that the diagnostic sensitivity, specificity, positive and negative predictive values, and accuracy for US were 86.2%, 97.2%, 89.3% and 96.3%, and 94.8%, respectively.[18]
Soldati et al. studied two series of patients with polytrauma and blunt chest trauma for the diagnosis of pneumothoraces using transthoracic US utilizing the low frequency curved probe. Results were compared to CR and spiral CT, and they concluded that US study may detect occult PTX undiagnosed by standard plain radiography and its extension with an accuracy that is almost as high as CT scanning (the reference standard).[19,20]
Limitations of the study
This study has several limitations. A large number of patients were excluded due to inability to transfer hemodynamically unstable patients to the CT. Patients who were clinically diagnosed as having tension PTX were managed by inserting chest tube for drainage before CT scanning and were also excluded from the study. The CT scans were often performed with time lag after initial US and CR, thus giving time for the PTX to enlarge in some cases. Patients were enrolled on a researcher-availability basis; however, this is unlikely to have led to any selection bias, because the researchers worked all shifts and all days in the ICU during the study course.
Conclusion
Chest US is an accurate modality more than anteroposterior bedside CR with CT scanning as a reference when evaluating critically ill mechanically ventilated patients, patients underwent invasive procedures (thoracocentesis and central venous catheter insertion), or patients with polytrauma.
We recommend the routine use of chest US in evaluating critically ill mechanically ventilated patients, the same as in initial evaluation of polytrauma patients in the emergency setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Strange C. Pleural complications in the Intensive Care Unit. Clin Chest Med. 1999;20:317–27. doi: 10.1016/s0272-5231(05)70144-1. [DOI] [PubMed] [Google Scholar]
- 2.de Latorre FJ, Tomasa A, Klamburg J, Leon C, Soler M, Rius J. Incidence of pneumothorax and pneumomediastinum in patients with aspiration pneumonia requiring ventilatory support. Chest. 1977;72:141–4. doi: 10.1378/chest.72.2.141. [DOI] [PubMed] [Google Scholar]
- 3.Wilson H, Ellsmere J, Tallon J, Kirkpatrick A. Occult pneumothorax in the blunt trauma patient: Tube thoracostomy or observation? Injury. 2009;40:928–31. doi: 10.1016/j.injury.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Chiles C, Ravin CE. Radiographic recognition of pneumothorax in the Intensive Care Unit. Crit Care Med. 1986;14:677–80. doi: 10.1097/00003246-198608000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Tocino IM, Miller MH, Fairfax WR. Distribution of pneumothorax in the supine and semirecumbent critically ill adult. AJR Am J Roentgenol. 1985;144:901–5. doi: 10.2214/ajr.144.5.901. [DOI] [PubMed] [Google Scholar]
- 6.Ball CG, Kirkpatrick AW, Laupland KB, Fox DL, Litvinchuk S, Dyer DM, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. Am J Surg. 2005;189:541–6. doi: 10.1016/j.amjsurg.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 7.Mowery NT, Gunter OL, Collier BR, Diaz JJ, Jr, Haut E, Hildreth A, et al. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011;70:510–8. doi: 10.1097/TA.0b013e31820b5c31. [DOI] [PubMed] [Google Scholar]
- 8.Kelly AM, Weldon D, Tsang AY, Graham CA. Comparison between two methods for estimating pneumothorax size from chest X-rays. Respir Med. 2006;100:1356–9. doi: 10.1016/j.rmed.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: A meta-analysis. Chest. 2011;140:859–66. doi: 10.1378/chest.10-2946. [DOI] [PubMed] [Google Scholar]
- 10.Brook OR, Beck-Razi N, Abadi S, Filatov J, Ilivitzki A, Litmanovich D, et al. Sonographic detection of pneumothorax by radiology residents as part of extended focused assessment with sonography for trauma. J Ultrasound Med. 2009;28:749–55. doi: 10.7863/jum.2009.28.6.749. [DOI] [PubMed] [Google Scholar]
- 11.Reissig A, Kroegel C. Accuracy of transthoracic sonography in excluding post-interventional pneumothorax and hydropneumothorax. Comparison to chest radiography. Eur J Radiol. 2005;53:463–70. doi: 10.1016/j.ejrad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, Corradi F. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: An alternative to chest radiography. Crit Care Med. 2010;38:533–8. doi: 10.1097/CCM.0b013e3181c0328f. [DOI] [PubMed] [Google Scholar]
- 13.Mayo PH, Goltz HR, Tafreshi M, Doelken P. Safety of ultrasound-guided thoracentesis in patients receiving mechanical ventilation. Chest. 2004;125:1059–62. doi: 10.1378/chest.125.3.1059. [DOI] [PubMed] [Google Scholar]
- 14.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Garofalo G, Busso M, Perotto F, De Pascale A, Fava C. Ultrasound diagnosis of pneumothorax. Radiol Med. 2006;111:516–25. doi: 10.1007/s11547-006-0047-y. [DOI] [PubMed] [Google Scholar]
- 16.Chung MJ, Goo JM, Im JG, Cho JM, Cho SB, Kim SJ. Value of high-resolution ultrasound in detecting a pneumothorax. Eur Radiol. 2005;15:930–5. doi: 10.1007/s00330-004-2518-7. [DOI] [PubMed] [Google Scholar]
- 17.Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT – Initial experience. Radiology. 2002;225:210–4. doi: 10.1148/radiol.2251011102. [DOI] [PubMed] [Google Scholar]
- 18.Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, et al. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10:R112. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soldati G, Testa A, Pignataro G, Portale G, Biasucci DG, Leone A, et al. The ultrasonographic deep sulcus sign in traumatic pneumothorax. Ultrasound Med Biol. 2006;32:1157–63. doi: 10.1016/j.ultrasmedbio.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Occult traumatic pneumothorax: Diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008;133:204–11. doi: 10.1378/chest.07-1595. [DOI] [PubMed] [Google Scholar]


