Abstract
Background:
The correct position of the endotracheal tube is confirmed by various modalities, most of which are not entirely reliable. Ultrasound is now increasingly available to anesthesiologists in the operating theater and is an attractive alternative. To investigate the usefulness of sonography in identifying the correct tracheal tube position in human cadavers.
Materials and Methods:
Endotracheal tubes placed randomly into trachea or esophagus was identified with a linear ultrasound probe placed transversely just above the suprasternal notch by a single anesthesiologist.
Results:
Of the 100 intubations performed at random, 99 were correctly identified to give a sensitivity of 100% and a specificity of 97.9%.
Conclusion:
Sonography is a useful technique to identify correct position of the tracheal tube.
Keywords: Esophageal intubation, sonography, tracheal intubation
Introduction
Endotracheal intubation is a standard procedure performed to manage the airway during general anesthesia. Confirmation of correct position of the tracheal tube is vital, as unrecognized esophageal intubation (EI) can lead to irreversible hypoxic brain damage or death.
The correct position of the tracheal tube is routinely confirmed by various modalities, most of which are not entirely reliable. Direct visualization of the endotracheal tube passing through the glottis and detection of exhaled carbon-dioxide by capnography is routinely applied in operating theaters for confirmation of correct tracheal tube position.[1] Direct visualization of the tube passing into glottis is not always possible, especially if the intubation is difficult.[1] Capnography can be false-positive when the tube is in the esophagus after exhaled gases are forced into stomach during bag-mask ventilation or ingestion of carbonated beverages and can be false-negative in severe bronchospasm, kinked tracheal tube, and cardiac arrest.[1]
Ultrasound machines are now increasingly available for anesthesiologists in the operating rooms for vascular access and regional anesthesia. Sonography is noninvasive and superficial structures of the neck are easily identified with minimal training, making ultrasound a potential tool to detect correct tracheal tube placement. Das et al.[2] and Chou et al.[3] in a recent meta-analysis have found ultrasonography to be highly sensitive and specific in detecting endotracheal tube position. The aim of this study was to investigate the effectiveness of sonography in identifying tracheal tube position in human cadavers.
Materials and Methods
The study was conducted on fresh frozen unembalmed cadavers in the legal custody of cadaver lab at advanced learning center of our Institution. Two adult cadavers, a male and a female cadaver were chosen for the study. Of the six anesthesiologists who participated in the study, five of them performed intubations and a single anesthesiologist identified all tracheal and EIs by ultrasound. The anesthesiologist performing the ultrasound had very minimal training by the institutional radiology department in identifying trachea and esophagus sonographically. The anesthesiologists were allowed to perform 10 intubations on each of the cadavers. They were allowed to randomly choose at their own discretion the number of tracheal or EIs as well as the order of tracheal or EIs. Tracheal tube sizes 7.5 and 8.5 were used for female and male cadavers respectively. The anesthesiologist who was blinded to the random order of intubation identified all intubations with a linear high-frequency probe (Venue 40, GE) placed transversely just superior to the suprasternal notch. The transducer was applied to the cadaver only immediately before and during the actual intubation. The anesthesiologists independently recorded each intubation on separate data collection sheet for later analysis. When the endotracheal tube entered the trachea, a brief flutter or snowstorm or a hyperechoic shadow was seen in the trachea[4,5,6] [Figure 1]. When the esophagus was intubated it was seen to be opened by the tracheal tube[6] [Figure 2].
Figure 1.
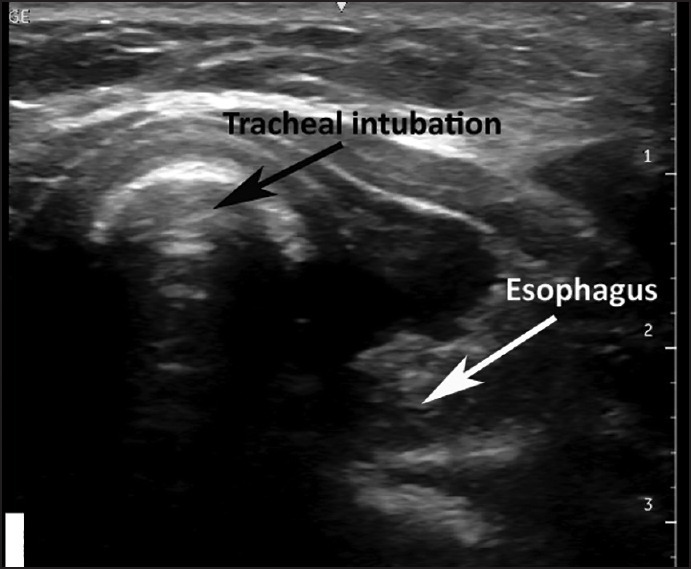
Tracheal intubation as seen on sonography
Figure 2.
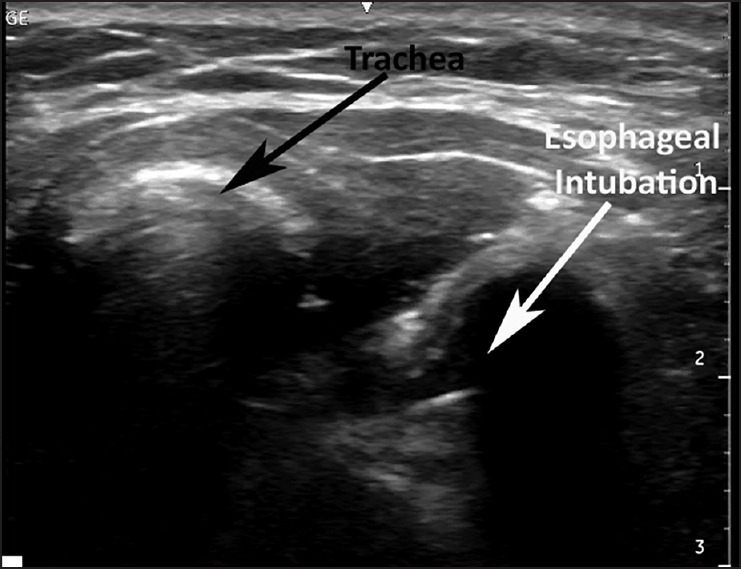
Oesophageal intubation as seen on sonography
Sensitivity, specificity, and positive and negative predictive values and their 95% confidence intervals (CIs) were calculated for determination of tube placement.
Results
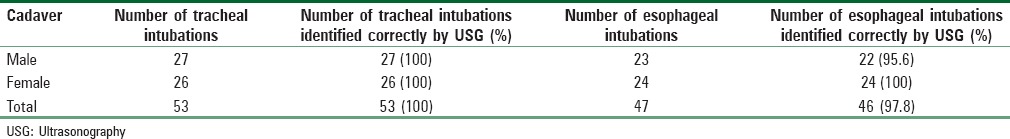
A total of 100 intubations were performed on the two cadavers by the five anesthesiologists of which 53 were tracheal and 47 were esophageal. Ninety-nine of these intubations were correctly identified as tracheal or esophageal by sonography. One EI done on the male cadaver was wrongly identified as tracheal. The accuracy of identification of tracheal intubation was 100% and that of EI was 97.8% [Table 1], resulting in sensitivity of 100% (95% CI: 93.3-100%), specificity of 97.9% (95% CI: 88.7-99.6%), a positive predictive value of 98.1% (95% CI: 90.1-99.9%), and a negative predictive value of 100% (95% CI: 92.3-100%). In both cadavers chosen for the study, the esophagus was seen to the left of the trachea.
Table 1.
Data on tracheal and oesophageal intubations
Discussion
Endotracheal intubation is a vital skill required for airway management and is routinely performed in anesthesia. Direct visualization of endotracheal tube passing through the glottis is considered the gold standard for correct tube placement. However, in patients with unfavorable upper airway anatomy, airway trauma, or secretions, it may not always be possible to visualize the vocal cords.[6] Various indirect methods have been described to verify tracheal tube position.[1] Auscultation of the lungs is the commonly employed first step, and capnography are routinely used in the operating theater for confirmation of tube position.
Sonography is increasingly available to anesthesiologists in operating room for vascular access and regional anesthesia. Sonography is an attractive alternative to confirm tracheal tube position as it is simple, easy to learn, and noninvasive method for assessing tube position. Sonography can detect correct tube position by direct visualization of the tube in the trachea or esophagus[6] and indirectly by visualizing ventilation, either by detecting sliding of the pleura or movement of diaphragm before and after intubation.[7,8] Hsieh et al.[8] confirmed correct tracheal tube position in pediatric patients by sonographic identification of diaphragmatic motion in subxiphoid view and Weaver et al.[7] Used the lung sliding sign in adult cadavers to confirm tracheal intubation. Indirect sonographic identification of tracheal intubation by diaphragmatic motion or lung sliding requires ventilation of lungs and hence, may increase the risk of aspiration if the tube is inadvertently placed in the esophagus and ventilated for confirmation. The trachea and esophagus may be visualized on sonography in both long axis and transverse views. Drescher et al., Employed the long axis sagittal view in cadavers and found sonography to be 100% sensitive and 98% specific for detection of EI.[4] Park et al., Confirmed endotracheal intubation with a sensitivity and specificity of 100% by a combination of transcricothyroid ultrasound and identification of lung sliding in an Emergency Department setting.[5]
Muslu et al.[6] reported a sensitivity and specificity of 100% for identifying correct tracheal tube position in adult surgical patients with the ultrasound probe placed transversely at suprasternal notch. The position of the tube was identified within 3 sec of tube placement.[6] In our study, the sensitivity was 100%, and specificity was 97.9% for correct identification of tracheal intubation. Out of the 100 intubations performed, one EI was wrongly identified as tracheal. In both the cadavers in our study, the esophagus was found to the left of the trachea. Other studies[6] have similarly found esophagus to the left in most of their patients.
Limitation of this study was that it has been carried out in only two cadavers and needs to be evaluated further in clinical scenarios. Furthermore, all intubations were identified by a single person who had received prior training and his performance may not reflect that of the average untrained user.
Conclusion
Although this study has the limitation of having been done in cadavers rather than live subjects and with a single ultrasound operator, it shows that sonography can accurately detect endotracheal tube position and is an attractive alternative to identify correct tube position.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Cadaver lab, Advanced Learning Centre, GEF, Bengaluru.
References
- 1.Salem MR, Baraka A. Confirmation of tracheal intubation. In: Hagberg CA, editor. Benumof's Airway Management. 2nd ed. Philadelphia, USA: Mosby Elsevier; 2007. pp. 697–727. [Google Scholar]
- 2.Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: A systematic review and meta-analysis. Can J Anaesth. 2015;62:413–23. doi: 10.1007/s12630-014-0301-z. [DOI] [PubMed] [Google Scholar]
- 3.Chou EH, Dickman E, Tsou PY, Tessaro M, Tsai YM, Ma MH, et al. Ultrasonography for confirmation of endotracheal tube placement: A systematic review and meta-analysis. Resuscitation. 2015;90:97–103. doi: 10.1016/j.resuscitation.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Drescher MJ, Conard FU, Schamban NE. Identification and description of esophageal intubation using ultrasound. Acad Emerg Med. 2000;7:722–5. doi: 10.1111/j.1553-2712.2000.tb02055.x. [DOI] [PubMed] [Google Scholar]
- 5.Park SC, Ryu JH, Yeom SR, Jeong JW, Cho SJ. Confirmation of endotracheal intubation by combined ultrasonographic methods in the Emergency Department. Emerg Med Australas. 2009;21:293–7. doi: 10.1111/j.1742-6723.2009.01199.x. [DOI] [PubMed] [Google Scholar]
- 6.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 7.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13:239–44. doi: 10.1197/j.aem.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh KS, Lee CL, Lin CC, Huang TC, Weng KP, Lu WH. Secondary confirmation of endotracheal tube position by ultrasound image. Crit Care Med. 2004;32:S374–7. doi: 10.1097/01.ccm.0000134354.20449.b2. [DOI] [PubMed] [Google Scholar]


