Abstract
Objectives
To characterize physical and mental diseases and utilization of healthcare services and identify factors associated with mortality among oldest-old patients using the Veterans Health Administration (VHA).
Design
Retrospective study with 5-year survival follow-up.
Setting
VHA system-wide.
Participants
A total of 721,588 veterans using the VHA aged 80 years or older as of October 2008: 80–89 years old (n = 665,249), 90–99 years old (n = 56,118), and 100–115 years old (n = 221).
Measurements
Patient demographics, physical and mental diseases, healthcare services, and 5-year survival were included.
Results
Accelerated failure time models identified protective and risk factors associated with mortality by age group. During a 5-year follow-up period, 44% of patients died with survival rates of 59% for 80’s, 32% for 90’s and 15% for 100’s. In the multivariable model, protective effects for veterans 80–99 were being female, minority race/ethnicity, married, having certain physical and mental diagnoses (hypertension, cataract, dyslipidemia, posttraumatic stress disorder, bipolar disorder), urgent care visits, invasive surgery, and few (1–3) prescriptions. Risk factors were lower VHA priority status, physical and mental conditions (diabetes, anemia, congestive heart failure, dementia, anxiety, depression, smoking, substance abuse disorder), hospital admission, and nursing home care. For those in their 100s, married status, smoking, hospital admission, nursing home care, invasive surgery, and prescription use were significant risk factors; only ED use was protective.
Conclusion
Although the data are limited only to VHA care (thus missing Medicare services), this study shows many veterans served by VHA live to advanced old age despite multiple chronic conditions. Further study is needed to determine whether a comprehensive, coordinated care system like VHA is associated with greater longevity for very old persons.
Keywords: Health services, Oldest-old, Survival, Veterans
INTRODUCTION
According to the 2010 census, over 22.6 million veterans live in the U.S. of whom almost two million are over the age of 80 (1). With increased life expectancy and demographic shifts in our population, the proportion of oldest-old adults, aged over 80 years, continues to increase (2, 3). The publicly funded Veterans Health Administration (VHA) must care efficiently and effectively for its increasing population of veterans, who are older, sicker, and socioeconomically disadvantaged relative to civilians (4). The number of oldest-old veterans who received VHA benefits or services nearly doubled from approximately 880,000 in 2002 to 1.6 million in 2013 (5) with significant ramifications for demand for healthcare, especially in the area of long-term or domiciliary care (6).
A large body of literature has investigated the health consequences of military service, which represents a unique experience that often impacts future health status and medical needs. Many veterans encountered life-threatening environments during their military service (6), leading to higher incidence of physical and mental diseases and contributing to higher mortality compared to non-veterans (7, 8). Dobkin and Shabani reported that functioning and health status among Vietnam veterans deteriorated more rapidly than non-veterans (9). The association between mortality and chronic disease in veterans has been well-documented across numerous conditions such as chronic obstructive pulmonary disease, cancer, mental disorders, and type-2 diabetes (10–13). Moreover, many studies have shown that mental illness such as post-traumatic stress disorder (PTSD) is significantly associated with a high rate of mortality among old veterans (14, 15). These studies, nevertheless, did not differentiate between older adults aged 80 years and over and treated them as a homogeneous group with those 65 and over (i.e., 65+), although great differences in health conditions and healthcare services utilization exist between younger (64–80 years) and older (80 years and older) groups of old people (16,17).
Given the large number of veterans over age 80 and the increasing emphasis on managing the aging process, it is important to identify associations between healthcare utilization and survival for the VHA’s oldest patients. Further, understanding how complex health conditions impact survival adds to our knowledge of key pathways connecting military service to health status and longevity. The purpose of this study was to: 1) examine the utilization of VHA health services and comorbidity among patients aged over 80 years; and 2) explore the demographic, clinical and health services correlates of mortality among these veterans.
METHODS
Data Source and Sample
The retrospective study relied on administrative extracts from the VHA’s electronic medical records system collected for the Surgical Treatment Outcomes for Patients with Psychiatric Disorders study (18). Among the 5.5 million patients treated in fiscal year 2009, 721,588 veterans aged over 80 years as of October 1, 2008 with diagnosis-generating care encounters were identified. Data were derived from the VHA's all-electronic medical record systems, major portions of which are copied nightly into the Corporate Data Warehouse (CDW) at the Austin Information Technology Center. Data in the CDW include all encounters (inpatient; outpatient including emergency department visits), prescription fills, lab tests and their results, other procedures, diagnoses, and demographic and enrollment data. The study was approved by the institutional review boards at South Texas and Central Texas Veterans Health Care Systems.
Measures
October 2008 to September 2009 served as the baseline fiscal year (FY2009) from which demographics, diagnoses, and healthcare utilization measures were obtained. Patient demographics included age, gender, race, Hispanic ethnicity, and marital status. Patients were categorized as aged 80–89 years, 90–99 years, or 100 and older as of October 1, 2008. Race was recoded as white, African American, Asian, and missing. VHA priority status captures why the veteran is eligible for VHA care; it is related to severity of illness and socioeconomic status (19, 20). Priority 1 identifies veterans who have been 50–100% disabled by a condition related to their military service (service-connected disability); these veterans incur no copays for care or pharmacy benefits. Priority 2 and 3 denote veterans with 10% to 40% service-connected disability; Priority 4 veterans are catastrophically disabled or homebound; Priority 5 are eligible based on low income; Priority 6 comprise various groups of military experiences such as Purple Heart award; Priority 2–6 veterans incur copays for pharmacy benefits. Priority 7 and 8 identify veterans who do not meet the above criteria and have agreed to copays for care and prescription medications. To simplify interpretation, we combined patients into Priority 1 vs Priority 2–6 vs Priority 7–8.
Medical comorbidity was indexed by the Charlson-Deyo score which includes weighted indicators of 19 comorbid conditions associated with one-year post-discharge mortality (i.e., myocardial infarct, chronic heart failure, peripheral vascular disease, stroke, dementia, chronic pulmonary disease, rheumatologic disease, peptic ulcer disease, liver disease, liver failure, diabetes, diabetes with complication, hemiplegia or paraplegia, chronic kidney disease, solid tumor, leukemia/myeloma, metastatic solid tumors, HIV, and AIDS) (21). Additional chronic conditions were defined by ICD9 codes (Appendix A) (22–24).
Healthcare service measures included any occurrence of emergency department (ED) visits, urgent care visits, non-urgent outpatient services, hospital admission, intensive care unit admission, use of nursing home care, and receipt of major surgery. Number of medication classes, excluding “as needed” prescriptions and prescriptions for less than 30 days, was counted as a general measure of chronic comorbidity burden, classified as none, 1–3, or 4 or more (25). The number of antibiotic prescriptions and cancer-related medications were tallied to allow for severity adjustment of these conditions.
Follow-up mortality data through FY2013 was obtained from the mini-vitals file. Mini-vitals file provides best date of death based on four sources of information: inpatient VA records for stays terminating in death; the Beneficiary Identification Records Locator Subsystem (BIRLS) file of veterans for whom a death benefit claim has been filed; the U.S. government's Social Security Administration records; and Centers for Medicare and Medicaid Services records for health care coverage of elderly, disabled, or impoverished persons. The algorithm showed approximately 98% sensitivity relative to the National Death Index, the gold standard for death data in the United States (26). Survival in days from October 1, 2008 was measured to date of death or censored at five years (September 30, 2013). A dichotomous variable was created for Cox proportional hazards models denoting death during the follow-up period (1 = died; 0 = survived), with the survived value signaling censored follow-up.
Analysis
Descriptive analyses included frequencies (percentages) and means (standard deviations, ranges) of demographic, clinical, and healthcare service measures, overall and by age group. Kaplan-Meier product-limit survival curves graphically summarized 5-year survival. While typically a Cox proportional hazards model would assess correlates of survival, the proportional hazards assumption was not met in this study. Therefore, accelerated failure time (AFT) models assuming a gamma distribution were used to examine demographic, clinical and healthcare services factors associated with survival for each age group separately, reporting the adjusted estimated ratios of the expected survival time and their 95% confidence intervals (CI). These models included demographic characteristics, physical and mental illness measures, healthcare services indicators, and medication measures. Sensitivity of effects to covariates was assessed; effects were robust in bivariate and reduced models. A reduced model was used with the 100’s group to conserve power. A criterion alpha level of less than .05 was used throughout. All analyses were conducted in SAS 9.2 (SAS Institute, Inc., Cary, NC) using PROC LIFEREG for AFT models and PROC LIFETEST to plot the Kaplan-Meier estimates.
RESULTS
Sample Characteristics
The study population consisted of 721,588 VHA patients; 665,249 in their 80’s, 56,118 in their 90’s, and 221 aged 100–115 (Table 1). The average age was 84 (sd = 3.3) years. Average days to death from the first day of FY2009 was 1,446 (sd = 542) days, approximately four years, with those over age 100 surviving an average of 848 (sd = 602) days. The majority were male (98%), white (90%) and non-Hispanic (97%). Two thirds of patients (67%) were married. With respect to VHA priority status, more than a third (38%) were priority 7 or 8 while 12% were priority 1; 6% qualified for VHA care because they were catastrophically disabled and 27% were impoverished. Women comprised an increasing proportion of each successive age group, such that 8% of those surpassing 100 years were women.
Table 1.
Characteristics of Veterans Health Administration Patients aged 80–115 in FY2009
| All Vets (n=721,588) |
80’s (n=665,249) |
90’s (n=56,118) |
100’s (n=221) |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Age in years (range: 80–115; M, sd)*** | 84.3 | 3.3 | 83.7 | 2.6 | 91.5 | 1.8 | 101.3 | 2.3 |
| Survival in days (M, sd)*** | 1,446 | 541.7 | 1,468 | 531.1 | 1,188 | 595.2 | 847.7 | 602.0 |
| Charlson Comorbidity Score (range: 0–34; M, sd)*** | 1.5 | 1.7 | 1.5 | 1.7 | 1.4 | 1.7 | 1.2 | 1.5 |
| Female*** | 16,581 | 2.3 | 14,784 | 2.2 | 1,779 | 3.2 | 18 | 8.1 |
| Race (missing/unknown=140,610)*** | ||||||||
| White | 525,070 | 90.4 | 484,494 | 90.5 | 40,443 | 89.0 | 133 | 75.1 |
| African American | 44,074 | 7.6 | 40,166 | 7.5 | 3,881 | 8.5 | 27 | 15.3 |
| Other | 11,834 | 2.0 | 10,708 | 2.0 | 1,109 | 2.4 | 17 | 9.6 |
| Hispanic*** | 19,981 | 2.8 | 18,294 | 2.8 | 1,676 | 3.0 | 11 | 5.0 |
| Married*** | 482,933 | 66.9 | 452,406 | 68.0 | 30,466 | 54.3 | 61 | 27.6 |
| Census Region*** | ||||||||
| Northeast | 150,671 | 20.9 | 138,617 | 20.8 | 12,009 | 21.4 | 45 | 20.4 |
| Midwest | 176,044 | 24.4 | 163,405 | 24.6 | 12,596 | 22.5 | 43 | 19.5 |
| South | 266,909 | 37.0 | 246,553 | 37.1 | 20,281 | 36.1 | 75 | 33.9 |
| West | 118,387 | 16.4 | 108,079 | 16.3 | 10,259 | 18.3 | 49 | 22.2 |
| Puerto Rico and Virgin Islands | 9,577 | 1.3 | 8,595 | 1.3 | 973 | 1.7 | 9 | 4.1 |
| Veterans Health Administration Priority Status*** | ||||||||
| Priority 1 | 89,038 | 12.3 | 80,353 | 12.1 | 8,651 | 15.4 | 34 | 15.4 |
| Priority 2–6 | 356,940 | 49.5 | 326,758 | 49.1 | 30,047 | 53.5 | 135 | 61.1 |
| Priority 7–8 | 275,610 | 38.2 | 258,138 | 38.8 | 17,420 | 31.0 | 52 | 23.5 |
p<.001
Clinical Factors and Healthcare Service Utilization
Charlson Comorbidity scores averaged 1.5 (sd = 1.7) indicating chronic disease was quite prevalent (72% had hypertension, 57% lipid disorders, 26% diabetes; see Table 2). Hypertension was decreasingly common with advancing age: 72% of octogenarians, 68% of nonagenarians, and 50% of centenarians. Dyslipidemia followed a similar pattern: 59% for 80’s, 43% for 90’s, and 16% for 100’s. Dementia (2–5%), anemia (15–21%), and congestive heart failure (CHF; 9–14%) affected higher proportions of centenarians.
Table 2.
Clinical and Healthcare Service Factors of Veterans Health Administration Patients Aged 80–115 in FY2009
| All Vets (n=721,588) |
80’s (n=665,249) |
90’s (n=56,118) |
100’s (n=221) |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Physical Illness | ||||||||
| Diabetes*** | 186,620 | 25.9 | 176,162 | 26.5 | 10,439 | 18.6 | 19 | 8.6 |
| Hypertension*** | 515,954 | 71.5 | 477,536 | 71.8 | 38,308 | 68.3 | 110 | 49.8 |
| Dementia*** | 16,469 | 2.3 | 14,632 | 2.2 | 1,827 | 3.3 | 10 | 4.5 |
| Dyslipidemia*** | 414,310 | 57.4 | 390,199 | 58.7 | 24,076 | 42.9 | 35 | 15.8 |
| Anemia*** | 107,442 | 14.9 | 96,696 | 14.5 | 10,699 | 19.1 | 47 | 21.3 |
| CHF*** | 66,011 | 9.2 | 59,053 | 8.9 | 6,927 | 12.3 | 31 | 14.0 |
| Cataract*** | 96,931 | 13.4 | 91,062 | 13.7 | 5,845 | 10.4 | 24 | 10.9 |
| Mental Illness | ||||||||
| Anxiety*** | 17,157 | 2.4 | 15,383 | 2.3 | 1,770 | 3.2 | 4 | 1.8 |
| Major Depressive Disorder*** | 4,393 | 0.6 | 4,183 | 0.6 | 210 | 0.4 | - | - |
| Any depression*** | 36,253 | 5.0 | 32,523 | 4.9 | 3,717 | 6.6 | 13 | 5.9 |
| Nicotine Dependence*** | 16,030 | 2.2 | 15,071 | 2.3 | 956 | 1.7 | 3 | 1.4 |
| Schizophrenia | 2,278 | 0.3 | 2,118 | 0.3 | 159 | 0.3 | 1 | 0.5 |
| Bipolar Disorder*** | 1,616 | 0.2 | 1,552 | 0.2 | 64 | 0.1 | - | - |
| Post-traumatic Stress Disorder*** | 12,578 | 1.7 | 11,799 | 1.8 | 779 | 1.4 | - | - |
| Substance Abuse Disorder*** | 14,911 | 2.1 | 14,122 | 2.1 | 787 | 1.4 | 2 | 0.9 |
| Healthcare Services (Any) | ||||||||
| ED visits*** | 173,627 | 24.1 | 159,326 | 24.0 | 14,231 | 25.4 | 70 | 31.7 |
| Urgent Care Visits*** | 46,614 | 6.5 | 43,236 | 6.5 | 3,369 | 6.0 | 9 | 4.1 |
| Non-Urgent Outpatient Services*** | 720,677 | 99.9 | 664,493 | 99.9 | 55,967 | 99.7 | 217 | 98.2 |
| Hospital Admission*** | 150,018 | 20.8 | 136,194 | 20.5 | 13,745 | 24.5 | 79 | 35.8 |
| Intensive Care Unit Admission | 35,394 | 4.9 | 32,732 | 4.9 | 2,649 | 4.7 | 13 | 5.9 |
| Nursing Home Care*** | 41,343 | 5.7 | 36,482 | 5.5 | 4,829 | 8.6 | 32 | 14.5 |
| Invasive Surgery*** | 27,209 | 3.8 | 25,646 | 3.9 | 1,557 | 2.8 | 6 | 2.7 |
| Healthcare Services (FY2009) | ||||||||
| ED visits*** | 85,830 | 11.9 | 77,790 | 11.7 | 7,993 | 14.2 | 47 | 21.3 |
| Urgent Care Visits*** | 20,609 | 2.9 | 18,824 | 2.8 | 1,781 | 3.2 | 4 | 1.8 |
| Non-Urgent Outpatient Services*** | 720,522 | 99.9 | 664,348 | 99.9 | 55,957 | 99.7 | 217 | 98.2 |
| Hospital Admission*** | 61,177 | 8.5 | 54,523 | 8.2 | 6,611 | 11.8 | 43 | 19.5 |
| Intensive Care Unit Admission*** | 11,481 | 1.6 | 10,430 | 1.6 | 1,046 | 1.9 | 5 | 2.3 |
| Nursing Home Care | 11,557 | 1.6 | 9,892 | 1.5 | 1,648 | 2.9 | 17 | 7.7 |
| Invasive Surgery*** | 8,626 | 1.2 | 8,062 | 1.2 | 563 | 1.0 | 1 | 0.5 |
| Medication Class Count*** | ||||||||
| 0 prescription | 82,331 | 11.4 | 74,453 | 11.2 | 7,821 | 13.9 | 57 | 25.8 |
| 1–3 prescriptions | 154,494 | 21.4 | 142,212 | 21.4 | 12,234 | 21.8 | 48 | 21.7 |
| 4+ prescriptions | 484,763 | 67.2 | 448,584 | 67.4 | 36,063 | 64.3 | 116 | 52.5 |
| Died from FY2009–FY2013*** | 314,190 | 43.5 | 275,926 | 41.5 | 38,076 | 67.9 | 188 | 85.1 |
p<.001
Diagnosis of mental illness was uncommon. Whereas many younger veterans have mental illnesses such as post-traumatic stress disorder (27), 5% of our patients had depression and only 2% were diagnosed with anxiety. Age group differences in healthcare utilization rates were observed. The centenarian group showed higher rates of ED visits (21% vs. 14% for 90s vs 12% for 80s) and hospital admissions (20% vs. 12% for 90s vs. 8% for 80s). The eldest veterans used fewer medications on average: proportion taking no medications was 26% for 100’s vs. 14% for 90s vs. 11% for 80s.
Protective and Risk Factors for 5-year Survival
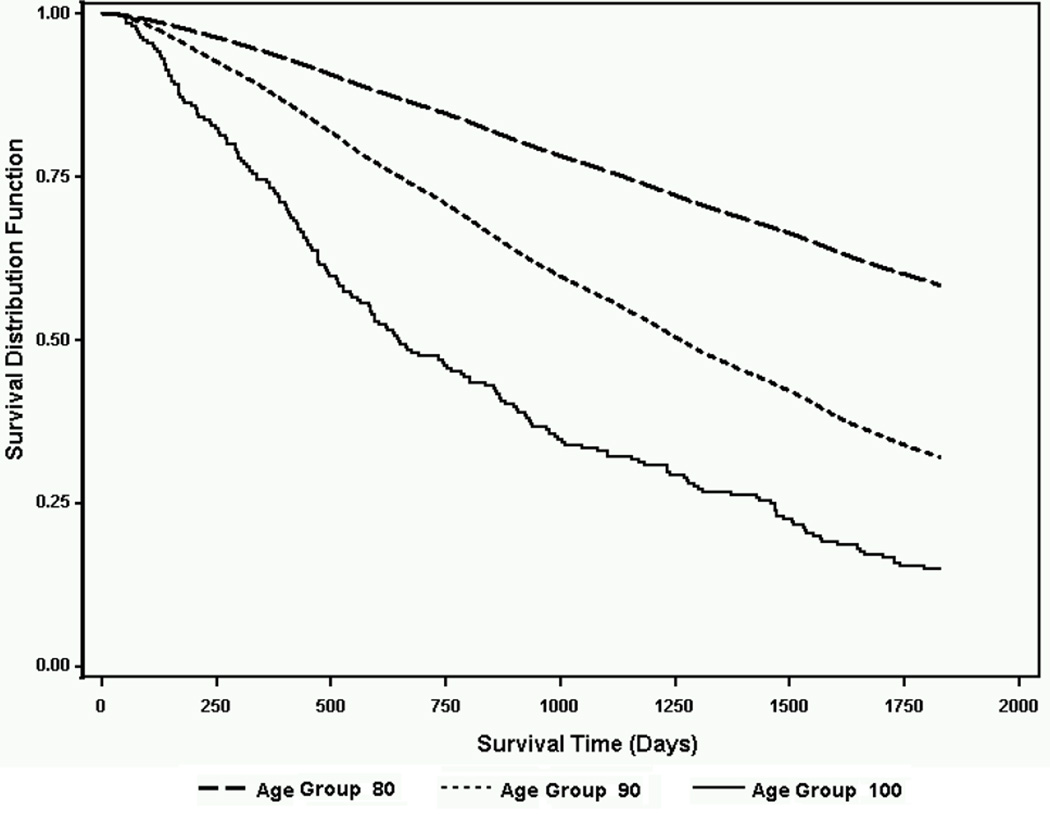
Overall, 56% of patients survived five years. Kaplan-Meier survival curves for the three age groups are displayed in Figure 1. As expected, octogenarians had a significantly higher survival rate (58%), followed by those in their 90s (32%) and centenarians (15%).
Figure 1.
Kaplan-Meier Survival Curves by Age Group
Adjusted models of survival over five years showed slightly different risk and protective factors among the three age groups (Table 3). For the 80’s group, all risk and protective factors were significant. Being female (survival ratio 1.22), minority race/ethnicity (1.06 to 1.14), and married (1.07) were associated with longer survival. Many types of healthcare utilization including ED visits, urgent care visits, having invasive surgery, and taking 1–3 medications (vs. 0) were protective while hospital admission (0.68) and use of nursing home care (0.64) were significant risk factors for survival. Lower VHA priority status (0.89 to 0.9), diagnosis with some chronic conditions (e.g., diabetes, dementia, depression), and taking 4 or more medications (4+) were also a risk factor for veterans aged 80–89 years (0.50 to 0.97), although cataract, dyslipidemia, and hypertension were protective (1.15 to 1.3).
Table 3.
Characteristics Associated with 5- Year Survival by Age Group among Veterans Health Administration Patients Aged 80–115
| 80’s (n=665,249) |
90’s (n=56,118) |
100’s (n=221) |
||||
|---|---|---|---|---|---|---|
| Survival Ratio (95% CI) |
p | Survival Ratio (95% CI) |
p | Survival Ratio (95% CI) |
p | |
| Female | 1.22 (1.20,1.24) | <0.01 | 1.25 (1.19,1.30) | <0.01 | 1.53 (0.99,2.37) | 0.06 |
| White race (reference) | ||||||
| African American | 1.07 (1.06,1.08) | <0.01 | 1.11 (1.07,1.14) | <0.01 | 1.30 (0.89,1.90) | 0.18 |
| Asian | 1.06 (1.03,1.08) | <0.01 | 1.18 (1.12,1.25) | <0.01 | 0.98 (0.63,1.52) | 0.93 |
| Hispanic | 1.14 (1.12,1.16) | <0.01 | 1.08 (1.03,1.13) | <0.01 | 1.09 (0.63,1.88) | 0.76 |
| Missing Race | 1.01 (1.00,1.01) | 0.17 | 0.99 (0.97,1.01) | 0.33 | 1.49 (1.07,2.08) | 0.02 |
| Married | 1.07 (1.07,1.08) | <0.01 | 1.03 (1.01,1.05) | <0.01 | 0.63 (0.49,0.81) | <0.01 |
| Veterans Health Administration Priority 7–8 (reference) | ||||||
| Priority 1 | 0.9 (0.89,0.91) | <0.01 | 0.97 (0.95,1.00) | 0.04 | 0.73 (0.49,1.07) | 0.11 |
| Priority 2–6 | 0.89 (0.89,0.90) | <0.01 | 0.94 (0.92,0.96) | <0.01 | 0.83 (0.62,1.11) | 0.21 |
| Diabetes | 0.88 (0.88,0.89) | <0.01 | 0.90 (0.88,0.92) | <0.01 | 1.31 (0.85,2.02) | 0.22 |
| Hypertension | 1.15 (1.14,1.16) | <0.01 | 1.15 (1.13,1.17) | <0.01 | 1.18 (0.92,1.51) | 0.19 |
| Anemia | 0.85 (0.84,0.85) | <0.01 | 0.90 (0.88,0.92) | <0.01 | 1.14 (0.84,1.55) | 0.39 |
| CHF | 0.65 (0.64,0.66) | <0.01 | 0.70 (0.68,0.71) | <0.01 | 0.88 (0.61,1.26) | 0.49 |
| Cataract | 1.28 (1.27,1.29) | <0.01 | 1.25 (1.22,1.28) | <0.01 | 1.09 (0.73,1.61) | 0.68 |
| Dementia | 0.72 (0.71,0.73) | <0.01 | 0.82 (0.79,0.85) | <0.01 | 0.69 (0.38,1.25) | 0.22 |
| Dyslipidemia | 1.3 (1.29,1.31) | <0.01 | 1.23 (1.21,1.25) | <0.01 | 1.39 (1.00,1.93) | 0.05 |
| Anxiety | 0.68 (0.67,0.69) | <0.01 | 0.79 (0.76,0.82) | <0.01 | 1.36 (0.59,3.12) | 0.47 |
| Depression | 0.50 (0.49,0.50) | <0.01 | 0.68 (0.66,0.7) | <0.01 | 0.81 (0.50,1.33) | 0.41 |
| Nicotine Dependence | 0.6 (0.59,0.61) | <0.01 | 0.78 (0.73,0.84) | <0.01 | 0.14 (0.02,0.78) | 0.03 |
| Post-traumatic Stress Disorder | 1.37 (1.34,1.4) | <0.01 | 1.33 (1.25,1.43) | <0.01 | ^ | ------- |
| Bipolar Disorder | 1.12 (1.07,1.18) | <0.01 | 1.34 (1.07,1.68) | 0.01 | ^ | ------- |
| Schizophrenia | 1.08 (1.03,1.12) | <0.01 | 0.97 (0.85,1.11) | 0.68 | ^ | ------- |
| Substance Abuse Disorder | 0.77 (0.75,0.79) | <0.01 | 0.88 (0.82,0.96) | <0.01 | 7.22 (0.89,58.74) | 0.06 |
| ED visits | 1.03 (1.02,1.04) | <0.01 | 1.02 (0.99,1.05) | 0.22 | 1.5 (1.02,2.20) | 0.04 |
| Urgent Care Visits | 1.13 (1.11,1.15) | <0.01 | 1.13 (1.08,1.18) | <0.01 | 1.56 (0.61,4.01) | 0.35 |
| Hospital Admission | 0.68 (0.68,0.69) | <0.01 | 0.67 (0.65,0.69) | <0.01 | 0.48 (0.29,0.77) | <0.01 |
| Nursing Home Care | 0.64 (0.63,0.65) | <0.01 | 0.67 (0.64,0.71) | <0.01 | 0.52 (0.30,0.90) | 0.02 |
| Invasive Surgery | 1.14 (1.11,1.16) | <0.01 | 1.05 (0.98,1.13) | 0.17 | 0.07 (0.01,0.35) | <0.01 |
| Medication Class Count: 0 prescriptions (reference) | ||||||
| Medication Class Count: 1–3 prescriptions | 1.13 (1.12,1.14) | <0.01 | 1.11 (1.08,1.14) | <0.01 | 0.67 (0.47,0.96) | 0.03 |
| Medication Class Count: 4+ prescriptions | 0.97 (0.96,0.98) | <0.01 | 1.04 (1.02,1.07) | <0.01 | 0.69 (0.51,0.95) | 0.02 |
Insufficient cases of the variables produced non-positive definite convergence in the 100’s model and were excluded in the final model.
For the nonagenarians, the patterns of risk and protective factors were similar to the octogenarians' except that two factors were uncorrelated (schizophrenia, ED use) and prescription of 4 or more medication was protective. Being female (1.25), minority race/ethnicity (1.08 to 1.18), and married status (1.03) had favorable survival ratios. Urgent care visits and taking medications (vs. 0) were also protective factors (1.04 to 1.13). Interestingly, selected physical and mental illnesses were associated with a reduced likelihood of death for the 90’s group as well: hypertension (1.15), cataracts (1.25), dyslipidemia (1.23), post-traumatic stress disorder (1.33), and bipolar disorder (1.34). Diagnosis with other chronic conditions was a risk factor (diabetes, anemia, CHF, dementia, etc., 0.70 to 0.90). Priority status 1, Priority status 2–6, hospital admission, and use of nursing home care were significant risk factors for survival (0.67 to 0.97). In spite of showing protective effects among the 80-year-old group, being diagnosed with schizophrenia, having ED visits, or having invasive surgery were not significantly associated with mortality in the 90-year-olds.
After excluding rare and inestimable factors (schizophrenia, bipolar disorder, post-traumatic stress disorder), the model within centenarian veterans found that ED use (1.5) was protective while being married, nicotine dependence, taking medications, hospitalization, invasive surgery, and nursing home care (0.07 to 0.63) increased risk of death. In summary, there were no common protective factor against mortality across age groups, medication burden and marital status had discordant effects, and shared risk factors were nicotine dependence, hospitalization and nursing home use.
DISCUSSION
Findings from this study suggest that healthcare utilization patterns correlate with survival among oldest-old veterans. Although previous studies have examined the association between chronic diseases and mortality (10–15, 28), this study is among the first to examine correlates of the incident rate of death among the oldest-old veterans, aged 80–115 years. As such, the findings of this study are noteworthy for several reasons. First, a surprising number of oldest-old veterans, three-quarters of a million persons in a single year, utilize the VHA. Existing studies about military service and health outcomes in late life have addressed veterans’ experience of greater age-related changes in health and more rapid health declines over time compared to non-veterans (29). Findings from Wilmoth and her colleagues showed steeper health declines and higher mortality as veterans age (29). The patients in this study, however, appeared to have overcome any presumed health disadvantage of being veterans and survived past the age of 80. Moreover, a few chronic physical illnesses (hypertension, cataracts, dyslipidemia) and mental illnesses (bipolar disorder and post-traumatic stress disorder) did not correlate with mortality among veterans in the 80’s and 90’s groups. Possibly it is because ongoing care, as evidenced by these diagnoses, was effective, that engagement was the essential factor (30), or because the mental illnesses were late-onset or only recently disclosed (31). It would be informative to determine in future work when these veterans first developed their diagnosed conditions and whether their care differed from that of decedents.
Second, several variables were found to be risk factors (hospital admission, nursing home care, smoking) for death across three age groups. Not surprisingly, with regards for veterans who survived to very old age, the greatest risk to death was related to hospitalization, staying in nursing home, and smoking, which is in line with previous research (32–34). Using nursing home after hospitalization has been one of the most prevalent risk factors for mortality regardless of the aging process (35). Interestingly, visiting the ED was protective against death in the oldest old group. The Behavioral Model of Health Service Use developed by Andersen and colleagues (36, 37) may be considered relevant. This model assumes that mortality is a function of healthcare utilization behavior influenced by three factors: predisposing factors, enabling factors, and need (35, 36, 38, 39). Therefore, enrollment in the VHA system (i.e., available resources as a predisposing factor) and medical need (i.e., comorbidity as a need factor) might lead patients to visit the ED, which, in turn, may reduce the incident rate of death among oldest-old veterans (40). Future research should explore whether frequency of outpatient care is important. Surprisingly, diagnoses of hypertension, dyslipidemia, schizophrenia and bipolar disorder were negatively related to mortality. Treatment in controlling blood pressure and cholesterol has been effective in preventing stroke, other cardiovascular diseases, or total mortality among older adults (41). Studies, however, have shown conflicting results in the benefit of treatment among patients age 80 and older (42–44). The Hypertension in the Very Elderly Trial (HYVET) can be supportive for this result (45). Studies have shown that serious mental illness can reduce the lifespan among the general population (46) and among veterans (40). Why, then, do those illnesses appear to be protective factors for oldest-old veterans? One explanation is that the mental illnesses were late-onset or recently diagnosed (31). Another reason might be early treatment in the VHA system. That is, their physicians might be able to detect early signs of mental illness, provide effective treatment, and monitor follow-up, suggesting that engagement is strongly associated to survival, even when serious conditions are present or diagnosed. Or, the treatment may have focused on psychotherapy, foregoing antipsychotic medications associated with metabolic disorder. This might reduce the risk effects of serious mental illness in this study.
It is important to acknowledge the study's limitations. First, severity of diagnosed conditions could not be captured. Patients in this study might have mild levels of mental health illness or dementia. Closer investigation of levels of mental illness or dementia would be a good topic for future research. Second, the sample of this study was derived from veterans who enrolled in VHA, a system that has traditionally catered to the most disadvantaged veterans of military service (47). Medicare data were not included although many VHA patients also benefit from Medicare. Results may not generalize to non-veterans, women, or persons who are healthier or wealthier than VHA patients. Furthermore, patients are generally eligible for VHA care because they are impoverished, disabled, multi-morbid or have specific military service experiences. Therefore, findings here may not generalize to patients covered by private health insurance or Medicare. Third, the survivorship effect was not considered. A few studies suggest that survival bias should be considered when focusing on very old age (48,49). For example, survivors into very late life could be assumed to have better status in domains such as physical health, behavioral health, and psychological aspects compared to their counterparts who were close to death or died prematurely (49). Patients included in this study could have been functioning better on physical and mental health indicators than those who had died earlier. In other words, the sickest had already died and the survivors were able to cope either without dangerous medications (e.g., psychotherapy alone) or had milder cases. A longitudinal design can differentiate selective survivorship effects related to longevity and enhance our understanding of trajectories in the relationship between healthcare utilization and mortality.
Despite these limitations, this study has multiple strengths: especially focusing on a very large cohort of male participants aged 80 years and older. Furthermore, the VHA serves a large population of veterans representing a more disadvantaged population who would otherwise face difficulty accessing healthcare. One possible avenue towards improving the quality of life and longevity is a deeper understanding of healthcare utilization patterns among oldest-old persons. Currently the VHA is the only U.S. system designed to provide longitudinal coordinated care through the end of life. This may be an optimal model for patient longevity.
Acknowledgments
Laurel Copeland: Employed by (a) Baylor Scott & White Health, and (b) Department of Veterans Affairs; unpaid Governing Board member representing Baylor Scott & White in the Health Care Systems Research Network (formerly “HMO Research Network”); Grant funding from Veterans Health Administration including HX-09-335, National Institute of Mental Health, Scott & White Research, VA Office of Rural Health, the Henry M. Jackson Foundation for the Advancement of Military Medicine (with Wounded Warrior Project, Walmart Foundation, May & Stanley Smith Charitable Trust, Robert R. McCormick Foundation, Onward Veterans and Schultz Family Foundation, Bob Woodruff Foundation, Phil & Marge Odeen, and the Rumsfeld Foundation). John Zeber: employment: Baylor Scott & White and the Department of Veterans Affairs; grant: NA HSRD merit grant on infectious disease (PI), Mental Health Research Network (co-I), Astra-Zeneca drug safety study (PI, pending); board (unpaid): Academy health behavioral interest group advisory board, World Journal of Psychiatry editorial board. Marcia Ory: Have personnel relationship with lead author; was faculty mentor. Marcos Restrepo: Employed by Department of Veterans Affairs and University of Texas Health Science Center at San Antonio. Dr. Restrepo’s time is partially protected by Award Number K23HL096054 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the Department of Veterans Affairs. The funding agencies had no role in the preparation, review, or approval of the manuscript. Paul Smith: Employed by Baylor Scott & White Health; Stocks: Vanguard target date retirement funds.
This work was completed with support from the Veterans Health Administration. The views are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Sponsor’s Role:
Cho, Copeland, Stock, MacCarthy, Zeber, Ory, Smith, Stevens: NA
Restrepo: The sponsor had no role in the conceptualization, analysis, interpretation, development or writing of this paper.
Appendix A
ICD 9 codes for additional chronic conditions
| Chronic conditions | ICD 9 codes |
|---|---|
| Dyslipidemia | 272 |
| Hypertension | 401–405 |
| Substance use disorders (SUD) | 291–292, 303–305 excluding 305.1 |
| Schizophrenia | 295 |
| Bipolar disorder | 296.0–296.1, 296.4–296.8 |
| Post-traumatic stress disorder | 309.81 |
| Major depressive disorder | 296.2–296.3, 311 |
| Any depressive disorder | 296.82, 298.0, 300.4, 301.12, 307.44, 309.0–309.1, 309.28, 311 |
| Nicotine dependence | 305.1 or V15.82 |
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
- Cho, Copeland: conceptual development, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript, and critical review of manuscript
- Stock, MacCarthy: acquisition of subjects and/or data, analysis of data
- Zeber, Restrepo, Ory, Stevens: study design, manuscript preparation, and critical review of manuscript
- Smith: Critical review of manuscript as a geriatrician
REFERENCES
- 1.U.S. Bureau of the Census. Veterans living by period of service, age, sex. [Accessed October 31, 2014];2010 Available at: http://www.census.gov/compendia/statab/2012/tables/12s0521.pdf.
- 2.Ailshire JA, Crimmins E. Psychosocial factors associated with longevity in the United States: Age differences between the old and oldest-old in the Health and Retirement Study. Gerontologist. 2011;2011:530534. doi: 10.4061/2011/530534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell FC, Miller ML. Life tables for the United States Social Security area 1900–2100: Actuarial study. Washington, DC: U.S.: Social Security Administration, Office of the Chief Actuary; 2002. p. 120. [Google Scholar]
- 4.Kizer K, Demakis J, Feussner J. Reinventing VA health care: Systematizing quality improvement and quality innovation. Med Care. 2000;38:S7–S16. [PubMed] [Google Scholar]
- 5.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Government Printing Office; 2012. [Google Scholar]
- 6.Liu X, Engel C, Kang H, et al. The effect of veteran status on mortality among older Americans and its pathways. Popul Res Policy Rev. 2005;24:573–592. [Google Scholar]
- 7.London A, Wilmoth J. Military service and, (Dis)Continuity in the life-course: Evidence on disadvantage and mortality from the Health and Retirement Study and the Study of Assets and Health Dynamics Among the Oldest-Old. Res Aging. 2006;28:135–159. [Google Scholar]
- 8.Wimmer LT, Fogel RW. Aging of Union Army men: A longitudinal study, 1830–1940. J Am Stat Assoc. Proceedings of the Government Statistical Section. 1991:56–61.
- 9.Dobkin C, Shabani R. The health effects of military service: Evidence from the Vietnam draft. Econ Inq. 2009;47:69–80. [Google Scholar]
- 10.Darnell K, Dwivedi AK, Weng Z, et al. Disproportionate utilization of healthcare resources among veterans with COPD: A retrospective analysis of factors associated with COPD healthcare cost. Cost Eff Resour Alloc. 2013;11:1–10. doi: 10.1186/1478-7547-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watanabe KK, Kang HK. Military service in Vietnam and the risk of death from trauma and selected cancers. Ann Epidemiol. 1995;5:407–412. doi: 10.1016/1047-2797(95)00039-a. [DOI] [PubMed] [Google Scholar]
- 12.Bullamn TA, Kang HK. Posttraumatic-stress-disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Ment Dis. 1994;182:604–610. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Hunt KJ, Gebregziabher M, Lynch CP, et al. Impact of diabetes control on mortality by race in a national cohort of veterans. Ann Epidemiol. 2013;23:74–79. doi: 10.1016/j.annepidem.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Boscarino J. Posttraumatic-stress-disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16:248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 15.Drescher K, Rosen C, Burling T, et al. Causes of death among male veterans who received residential treatment for PTSD. J Trauma Stress. 2003;16:535–543. doi: 10.1023/B:JOTS.0000004076.62793.79. [DOI] [PubMed] [Google Scholar]
- 16.Nie JX, Wang L, Tracy CS, et al. Health care service utilization among the elderly: Findings from the Study to Understand the Chronic Condition Experience of the Elderly and the Disabled (SUCCEED project) J Eval Clin Pract. 2008;14:1044–1049. doi: 10.1111/j.1365-2753.2008.00952.x. [DOI] [PubMed] [Google Scholar]
- 17.Vegda K, Nie JX, Wang L, et al. Trends in health services utilization, medication use, and health conditions among older adults: A 2-year retrospective chart review in a primary care practice. BMC Health Serv Res. 2009;9:217–223. doi: 10.1186/1472-6963-9-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Copeland LA, Sako EY, Zeber JE, et al. Mortality after cardiac or vascular operations by preexisting serious mental illness status in the Veterans Health Administration. Gen Hosp Psychiatry. 2014;36:502–508. doi: 10.1016/j.genhosppsych.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Kazis L, Miller D, Clark J, et al. Health-related quality of life in patients served by the department of veterans affairs: Results from the Veterans Health Study. Arch Intern Med. 1998;158:626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 20.Pugh M, Copeland L, Zeber JE, et al. The impact of epilepsy on health status among younger and older adults. Epilepsia. 2005;46:1820–1827. doi: 10.1111/j.1528-1167.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 21.Charson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic co-morbidity in longitudinal-Studies - Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Veterans Affairs. Re-engaging veterans with serious mental illness in treatment. [Accessed October 27, 2014]; Available at: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2476.
- 23.Blow FC, McCarthy JF, Valenstein M, et al. Care for veterans with psychosis in the VHA, FY 04. Ann Arbor, MI: VA National Serious Mental Illness Treatment Research and Evaluation Center; Annual National Psychosis Registry Report; 2005. [Google Scholar]
- 24.Copeland LA, Mortensen EM, Zeber JE, et al. Pulmonary disease among inpatient decedents: Impact of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:720–726. doi: 10.1016/j.pnpbp.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 25.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 26.Sohn MW, Arnold N, Maynard C, et al. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:1–8. doi: 10.1186/1478-7954-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: Mental health disorders among 103,788 U.S. veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 28.Shephard B. A War of Nerves: Soldiers and psychiatrists in the twentieth century. Boston, MA: Harvard University Press; 2003. [Google Scholar]
- 29.Wilmoth JM, London AS, Parker WM. Military service and men's health trajectories in later life. J Gerontol B Psychol Sci Soc Sci. 2010;65:744–755. doi: 10.1093/geronb/gbq072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsan JY, Stock EM, Gonzalez JM, et al. Mortality and guideline-concordant care for older patients with schizophrenia: A retrospective longitudinal study. BMC Med. 2012;10:147. doi: 10.1186/1741-7015-10-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leibowitz RQ, Jeffreys MD, Copeland LA, et al. Veterans' disclosure of trauma to healthcare providers. Gen Hosp Psychiatry. 2008;30:100–103. doi: 10.1016/j.genhosppsych.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 33.Wood KA, Ely EW. What does it mean to be critically ill and elderly? Curr Opin Crit Care. 2003;9:316–320. doi: 10.1097/00075198-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Roch A, Wiramus S, Pauly V, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care. 2011;15:R36. doi: 10.1186/cc9984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Banta JE, Andersen RM, Young AS, et al. Psychiatric comorbidity and mortality among veterans hospitalized for congestive heart failure. Mil Med. 2010;175:732–741. doi: 10.7205/milmed-d-10-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walter L, Brand R, Counsell S, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–2994. doi: 10.1001/jama.285.23.2987. [DOI] [PubMed] [Google Scholar]
- 37.Andersen RM, Davidson PL. In: Improving access to care in America: Individual and contextual indicators. Andersen RM, Rice TH, Kominski EF, editors. San Francisco, CA: Jossey-Bass; 2001. pp. 3–30. [Google Scholar]
- 38.Andersen RM. Revisiting the behavioral-model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 39.Fan L, Shah MN, Veazie PJ, et al. Factors associated with emergency department use among the rural elderly. J Rural Health. 2011;27:39–49. doi: 10.1111/j.1748-0361.2010.00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolinsky FD, Liu L, Miller TR, et al. Emergency department utilization patterns among older adults. J Gerontol A Biol Sci Med Sci. 2008;63:204–209. doi: 10.1093/gerona/63.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lawers CM, Bennett DA, Feigin VL, et al. Blood pressure and stroke: An overview of published reviews. Stroke. 2004;35:1024–1033. [PubMed] [Google Scholar]
- 42.Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, et al. Total cholesterol and risk of mortality in the oldest old. Lancet. 1997;350:1119–1123. doi: 10.1016/s0140-6736(97)04430-9. [DOI] [PubMed] [Google Scholar]
- 43.Satish S, Freeman DH, Jr, Ray L, et al. The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc. 2001;49:367–374. doi: 10.1046/j.1532-5415.2001.49078.x. [DOI] [PubMed] [Google Scholar]
- 44.Rastas S, Pirttila T, Viramo P, et al. Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc. 2006;54:912–918. doi: 10.1111/j.1532-5415.2006.00742.x. [DOI] [PubMed] [Google Scholar]
- 45.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 46.Thorp SR, Sones HM, Glorioso D, et al. Older patients with schizophrenia: Does military veteran status matter? Am J Geriatr Psychiatry. 2012;20:248–256. doi: 10.1097/JGP.0b013e3182096ae5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morgan RO, Teal CR, Reddy SG, et al. Measurement in Veterans Affairs Health Services Research: Veterans as a special population. Health Serv Res. 2005;40:1573–1583. doi: 10.1111/j.1475-6773.2005.00448.x. PMID:16178996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baltes P, Smith J. A systemic-wholistic view of psychological functioning in very old age: Introduction to a collection of articles from the Berlin Aging Study. Psychol Aging. 1997;12:395–409. doi: 10.1037//0882-7974.12.3.395. [DOI] [PubMed] [Google Scholar]
- 49.Baltes PB, Reese HW, Nesselroade JR. Life-Span developmental psychology: Introduction to Research Methods. Hillsdale: Erlbaum; 1998. [Google Scholar]