Summary
Allergic asthma is less prevalent in countries with parasitic helminth infections, and mice infected with parasites such as Heligmosomoides polygyrus are protected from allergic airway inflammation. To establish whether suppression of allergy could be mediated by soluble products of this helminth, we tested H. polygyrus excretory-secretory (HES) material for its ability to impair allergic inflammation. When HES was added to sensitising doses of ovalbumin, the subsequent allergic airway response was suppressed, with ablated cell infiltration, a lower ratio of effector (CD4+CD25+Foxp3−) to regulatory (CD4+Foxp3+) T (Treg) cells, and reduced Th1, Th2 and Th17 cytokine production. HES exposure reduced IL-5 responses and eosinophilia, abolished IgE production, and inhibited the type 2 innate molecules arginase-1 and RELM-α. Although HES contains a TGF-β-like activity, similar effects in modulating allergy were not observed when administering mammalian TGF-β alone. HES also protected previously sensitised mice, suppressing recruitment of eosinophils to the airways when given at challenge, but no change in Th or Treg cell populations was apparent. Because heat-treatment of HES did not impair suppression at sensitisation, but compromised its ability to suppress at challenge, we propose that HES contains distinct heat-stable and heat-labile immunomodulatory molecules which modulate pro-allergic adaptive and innate cell populations.
Keywords: allergy, eosinophils, IgE, infection, macrophages
1. Introduction
Allergic asthma has dramatically increased in prevalence in developing countries, exceeding 5% of the Western European and North American populations [1]. This contrasts with much lower asthma incidence in tropical countries which have significant levels of parasite infections, and these observations have stimulated research into the effects of parasitic organisms on human allergy [2–4]. From these studies, it has emerged that allergic diseases are least common in parts of the world with high helminth endemicity, and that within endemic populations the prevalence of atopy is significantly lower in individuals with chronic worm infections [5–10].
While a causal link between human helminth infections and reduced allergy has yet to be proven [2], chemotherapeutic clearance of intestinal helminths can result in accentuated atopic responsiveness [11–13], and helminth infection blocks overt allergy in a number of animal models [14–17] The degree to which helminths may influence allergy, however, is clearly variable between different parasite species [18], and is probably dependent upon the duration and intensity of infection [2,19], each factors that need to be taken into account in assessing this interaction.
The concept that helminths may act in a beneficial way for therapy of immunological disorders is one that has been gaining interest in recent years, especially since reports that the majority of inflammatory bowel disease (IBD) patients infected with Trichuris suis, the pig whipworm, went into remission [20,21]. Subsequent trials in allergic rhinitis have tested both T. suis therapy [22] and the effects of the human hookworm Necator americanus [23], and the latter parasite has also been trialled for coeliac disease [24,25]. While these later studies did not find any clinical improvement, significant suppression of inflammatory gut immune responses occurred with N. americanus [25,26]. Beyond clinical trials, there have also been remarkable reports of remission of multiple sclerosis in patients serendipitously acquiring intestinal helminth infections [27–29] and a case history of an IBD patient self-medicated with the human species T. trichiura resulting in both remission of symptoms and a switch in mucosal immune reactivity towards IL-22 [30].
Prompted by reports from human helminth-infected populations, we previously studied the effects of a model intestinal nematode parasite, Heligmosomoides polygyrus, on the expression of allergic airway inflammation in an experimental system using ovalbumin and house dust mite allergy [31]. We found that mice carrying a chronic infection with this helminth showed profound suppression of lung eosinophilia, airway tissue inflammation and type 2 cytokine production in response to airway challenge. Moreover, mice that had been sensitised to allergen were protected from airway allergy if they subsequently became infected; hence, this parasite may confer a therapeutic effect in reversing the allergic state in vivo. This protective effect could also be adoptively transferred with either regulatory T (Treg) cell [31], or B-cell transfer [32], in both cases in an IL-10 independent manner. Together with a number of other studies on H. polygyrus infection in allergy [33,34], colitis [35–37] and diabetes [38,39], it is clear that this helminth down-regulates multiple effector pathways of the adaptive immune response [40].
Therapy of human immune pathologies with live helminth parasites continues to be evaluated, but will remain an empirical process. Moreover, permitted doses of live parasites are minimal due to ethical and logistical constraints [41], such that exposure levels and duration do not approach those seen in endemic populations. Future therapeutic applications of live helminths will inevitably be limited by the same factors, arguing the case for developing non-living molecular derivatives based on helminth immunomodulatory products; such molecules should also permit a more mechanistic understanding of interactions with the host immune system [42]. Indeed, a number of parasite-derived products have shown some protective ability in immunopathology models [16,17]. Products of Ancylostoma caninum [43,44], Hymenolepis diminuta [45], Schistosoma mansoni [44] and Trichinella spiralis [46] all contain immunomodulators which can suppress pathology in mouse models of colitis, while somatic constitutents of Ascaris suum can inhibit allergic inflammation [47,48], as can secretions of Nippostrongylus brasiliensis [49]. Physiologically, active immunomodulators are most likely to be secreted from live parasites into their host environment [50], and in this report we focus on the H. polygyrus Excretory-Secretory (HES) products as potential modulators of airway allergy in a mouse model.
HES is a complex mixture of proteins, carbohydrates and lipids, many of which have been defined by proteomics [51] and monoclonal antibody analysis [52]. HES is known to down-modulate dendritic cell responses [53] and includes a molecule that binds to and signals through the mammalian TGF-β receptor [54]. Similarly to mammalian TGF-β, HES induces Foxp3 expression in stimulated CD4+ T cells in vitro, which are functionally suppressive and able to suppress airway allergic pathology. Like other nematode organisms, the H. polygyrus genome includes TGF-β family members [55], however it is as yet unclear if these are responsible for the TGF-β signal.
We have now tested HES for its effects in a mouse allergy model, and show that it replicates the suppression of pathology seen in the same model with live H. polygyrus infection [31]. We report below that co-administration of HES with sensitising allergen inhibits both innate and adaptive arms of the immune response, including eosinophilia, type 2 innate response markers, antibody generation and effector T-cell reactivity. Moreover, airway eosinophilia could be suppressed to a significant extent even when HES was administered at airway challenge to mice previously sensitised to allergen in the absence of the helminth products, opening the door to future research into therapeutic application to alleviate immunopathological conditions.
2. Results
2.1. Inhibition of airway allergy in mice co-sensitised with HES
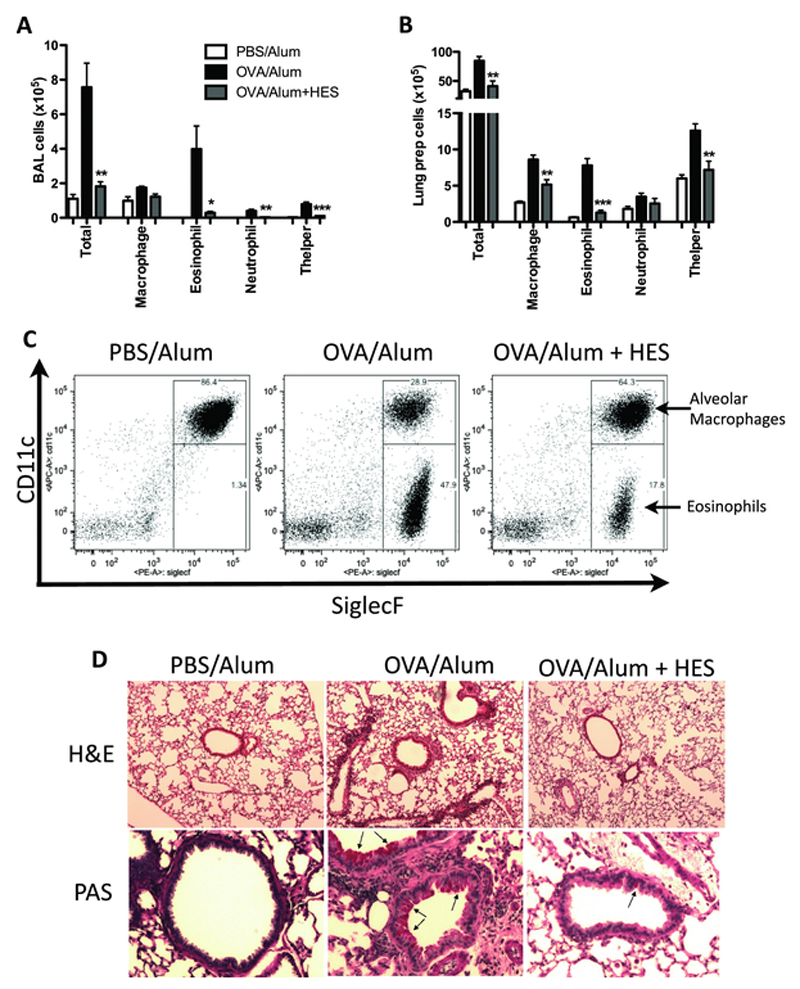
We first tested the ability of H. polygyrus excretory-secretory products (HES) to alter the outcome of an airway allergy model which has previously been shown to be suppressed during live infection with this parasite [31]. Mice were sensitised with two injections of alum-precipitated ovalbumin (OVA) in PBS on days 0 and 14; we added soluble HES to the suspension to avoid any functional denaturation that might occur through alum precipitation. All animals received an airway challenge of OVA on days 28, 29 and 30. As shown in Fig. 1, addition of HES at sensitisation resulted in profound suppression of the airway allergic inflammation measured by total cell numbers as well as inflitrates of eosinophils and CD4+ T helper cells in the bronchoalveolar lavage (Fig. 1 A) and lung tissue Fig 1 B). As well as absolute cell numbers, proportions of BAL SiglecF+CD11c− eosinophils were also sharply reduced with HES administration (Fig. 1 C). Haemotoxylin and Eosin (H&E) and Periodic Acid-Schiff (PAS) staining of formalin-fixed lung sections also showed reduced inflammatory infiltrate and mucus production with HES administration (Figure 1 D).
Figure 1. HES suppresses airway allergy.
20 μg HES was coadministered with each sensitisation injection of OVA-Alum on d0 and d14, and challenges of 30 min of 1% OVA aerosol were given at days 28-30. Bronchioalveolar lavage (BAL) fluid and lung tissue for cell preparation were collected at day 31. Shown are: (A) the numbers of total BAL cells and cell types, (B) the numbers of total lung preparation cells and cell types, (C) a representative flow cytometry plot of SiglecF vs. CD11c expression on BAL cells and (D) representative haematoxylin and eosin (H&E, 20× magnification) and periodic acid-Schiff (PAS, 200× magnification) staining of formalin-fixed lung sections. (A-D) Results are representative of at least 2 repeat experiments each with 4-6 mice per group. (D) Arrows indicate mucus-producing cells. Significant differences shown compare OVA/Alum to OVA/Alum + HES. Error bars are SEM. *p<0.05, **p<0.01, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
2.2. Inhibition is not due to antigenic competition
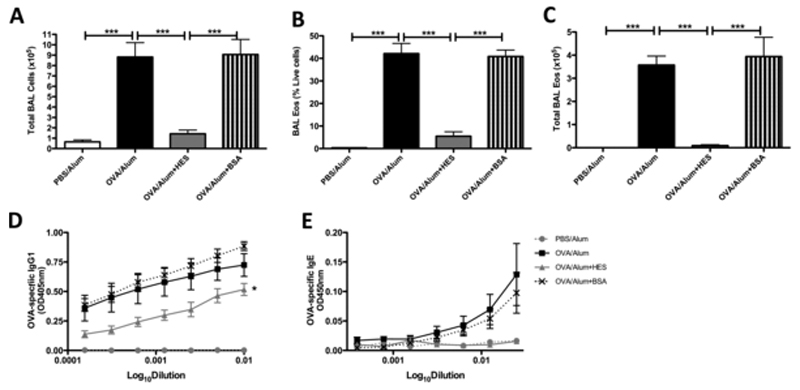
To address whether the suppression of OVA-specific responsiveness by HES was due to a simple antigen competition effect by the additional proteins, we repeated these experiments using bovine serum albumin (BSA) admixed with OVA-alum (Fig 2). BSA co-administration could not replicate the potent suppression of BAL total and eosinophil cell numbers seen with HES administration (Fig 2 A-C). We also found that when OVA-alum was co-administered with HES, but not with BSA, anti-OVA IgG1 titres were diminished more than tenfold (Fig 2 D) and IgE almost completely ablated (Fig. 2 E). Anti-OVA IgG2a titres were also reduced (data not shown), indicating that a shift to Th1 responsiveness had not occurred.
Figure 2. The suppressive effects of HES are not due to antigen competition.
20 μg HES or Bovine Serum Albumin (BSA) were coadministered with each sensitisation injection of OVA-Alum on d0 and d14, and following challenge at days 28-30, bronchoalveolar lavage (BAL) fluid and serum were collected at day 31. Shown are: (A) the total BAL cell numbers, (B) the SiglecF+CD11c- (eosinophil) proportion of total BAL cells, (C) the SiglecF+CD11c- (eosinophil) BAL cell numbers, (D) OVA-specific IgG1 measured by ELISA and (E) the OVA-specific IgE measured by ELISA. Results are representative of 2 repeat experiments each with 4-6 mice per group. Error bars are SEM. ***p<0.001, one-way ANOVA, with a Tukey’s post test.
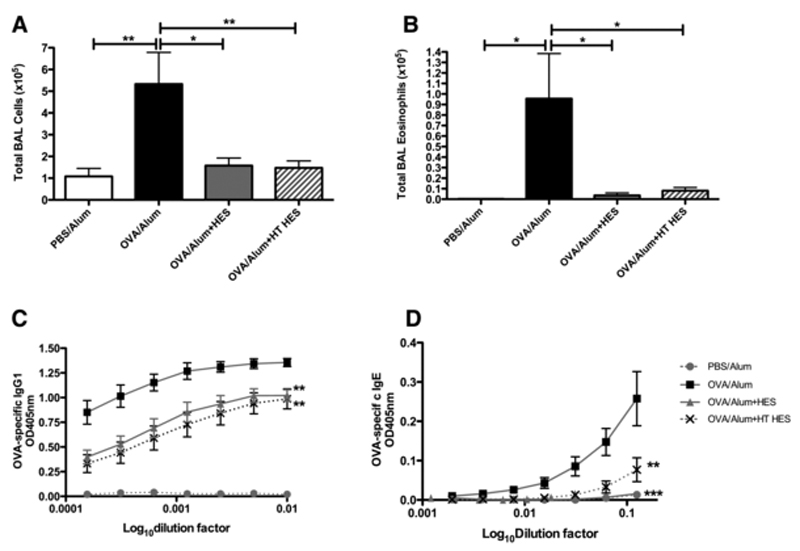
2.3. Inhibition by HES is mediated by heat-stable components
Because HES is a complex mixture of multiple proteins and glycoconjugates [51] we next determined whether the functional effect of HES was mediated by a heat-stable component. HES was pre-incubated at 100°C, and compared with untreated HES for its ability to suppress airway inflammation. As shown in Fig. 3, heat-treated HES is as potent as HES at suppressing total numbers (Fig. 3 A) and eosinophilic infiltrate into the BAL (Fig. 3 B). Heat-treated HES was similar to untreated HES in reduction of OVA-specific IgG1 (Fig. 3 C) and IgE (Fig. 3 D).
Figure 3. The suppressive effects of HES are heat stable.
20 μg HES or heat-treated HES (HT-HES) were coadministered with each sensitisation injection of OVA-Alum on d0 and d14, and following challenge at days 28-30, BAL fluid and serum were collected at day 31. Shown are: (A) the total BAL cell numbers, (B) SiglecF+CD11c− eosinophil numbers, (C) OVA-specific IgG1 measured by ELISA and (D) OVA-specific IgE measured by ELISA. Results are representative of 4 repeat experiments each with 4-6 mice per group. Error bars are SEM. *p<0.05, **p<0.01, one-way ANOVA, with a Tukey’s post test.
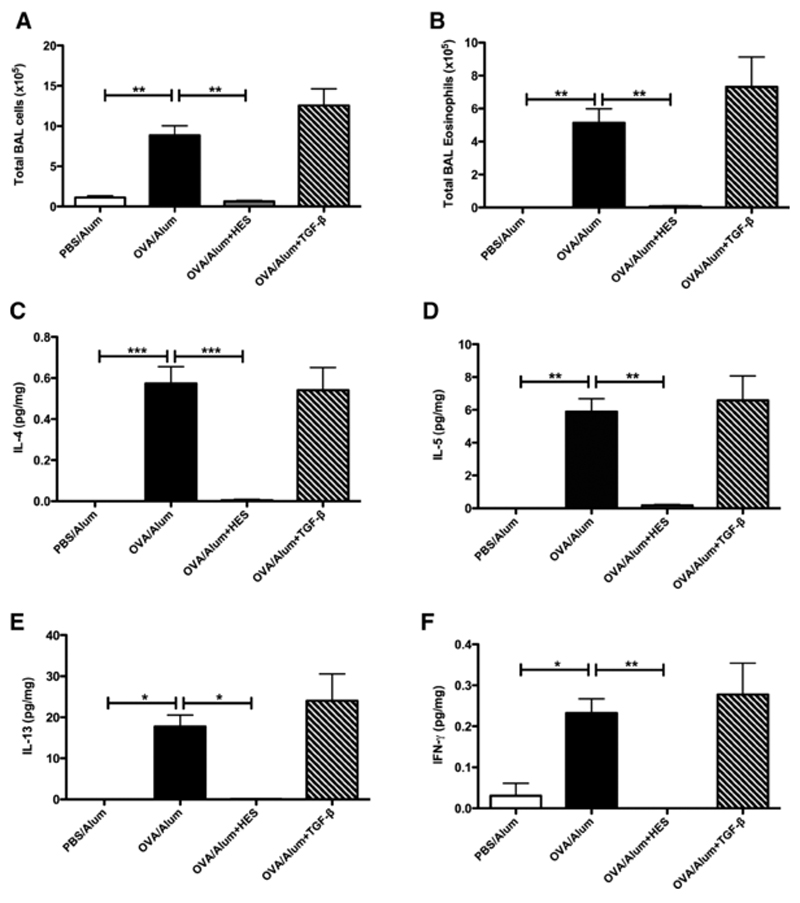
2.4. Inhibition by HES is not accounted for by the activity of TGF-β
Because HES contains a functional mimic of TGF-β, a known inhibitor of airway allergy [56], we compared the effects of 20 μg of HES administration with that of the equivalent activity of TGF-β (4 ng) [54]. As shown in Fig. 4, TGF-β co-administration showed no indication of any suppression of eosinophilic BAL infiltrates, in contrast to almost total ablation by HES (Fig 4 A, B). HES also suppressed IL-4, IL-5, IL-13 and IFN-γ expression in the lung homogenate, while TGF-β did not affect these cytokines (Fig 4 C-F); the abolition of the OVA-induced IFN-γ response gives further evidence that Th1 responsiveness does not replace the Th2 response following HES exposure. Levels of IL-10 in the lung were found not to differ between mice that had received HES and control mice (data not shown).
Figure 4. HES protects against asthma more potently than TGF-β.
20 μg HES or 4 ng recombinant TGF-β (TGF) were coadministered with each sensitisation injection of OVA-Alum on d0 and d14, and following challenge at days 28-30, lung tissue was collected and homogenised at day 31. (A) The total BAL cell numbers and (B) the SiglecF+CD11c− eosinophil numbers are shown. Levels of the cytokines (C) IL-4, (D) IL-5, (E) IL-13, (F) IFN-γ and IL-10 were measured using BD Flex sets, and normalised by dividing the cytokine concentration (in pg/ml) by the total protein concentration (in mg/ml) of the lung homogenate. Levels of IL-10 were below detection limits in this experiment, but were either unchanged or reduced with HES compared with that of OVA alone in other experiments where IL-10 was detectable. Results are representative of at least 2 experiments, each with 4-6 mice per group. Error bars are SEM. *p<0.05, **p<0.01, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
2.5. Type 2 innate response markers are suppressed by HES
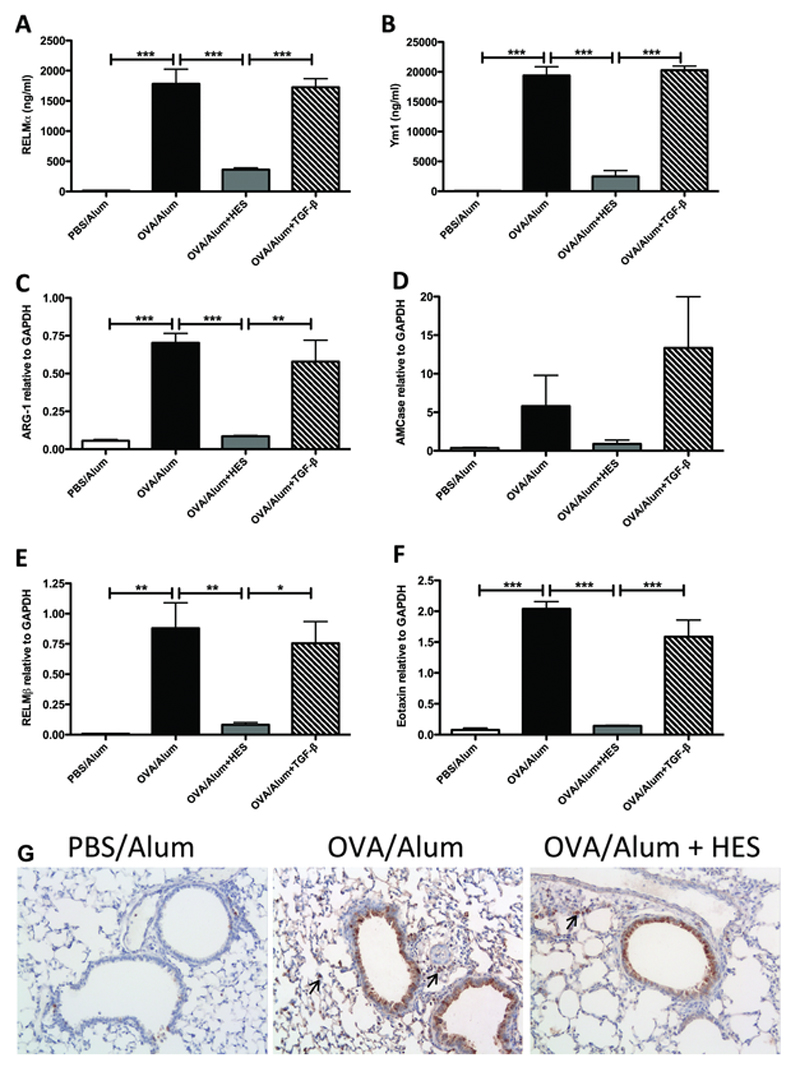
Key innate cell populations such as alternatively activated macrophages (AAM) are involved in both anti-parasite [57,58] and asthmatic [59,60] immune responses. Together with epithelial cells [61], AAMs express high levels of type 2 innate response markers, such as RELMα and Ym1. HES administration was found to potently suppress expression of both these products (Fig. 5 A, B). Real-time RT-PCR confirmed this finding (data not shown), with expression levels of additional type 2 innate response markers Arginase-1 and AMCase suppressed by HES (although AMCase did not reach statistical significance) (Fig. 5 C, D). Transcription of the type 2 response epithelial cell marker RELM-β was also reduced with HES administration (Fig. 5 E), as was the chemokine eotaxin/CCL11 (Fig. 5 F). Recombinant mammalian TGF-β could not replicate any of these effects of HES administration. Immunohistochemical staining for RELM-α (Fig 5 G) shows production both in epithelial and interstitial cells, many of which appear to be macrophages by morphology. Although overall RELMα staining was reduced with HES administration, production by both epithelial and interstitial cells could still be detected (Fig 5 G, right panel).
Figure 5. HES suppresses type 2 innate response markers while recombinant mammalian TGF-β cannot.
Cell-free BAL supernatants from the mice shown in Figure 4 were tested by ELISA for levels of (A) RELM-α and (B) Ym1 protein by ELISA. RNA was prepared from lung tissue and qRT-PCR used to assess levels of (C) Arg-1, (D) AMCase, (E) RELM-β and (F) eotaxin transcription relative to GAPDH. Data are representative of 2 repeat experiments, each with 4-6 mice per group. (G) Formalin-fixed lung tissue sections from 5 individual mice in the second experiment were stained for RELM-α by immunohistochemistry (5 mice per group). Arrows indicate interstitial cell staining. Error bars are SEM. *p<0.05, **p<0.01, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
2.6. T helper cytokine expression is suppressed by HES administration
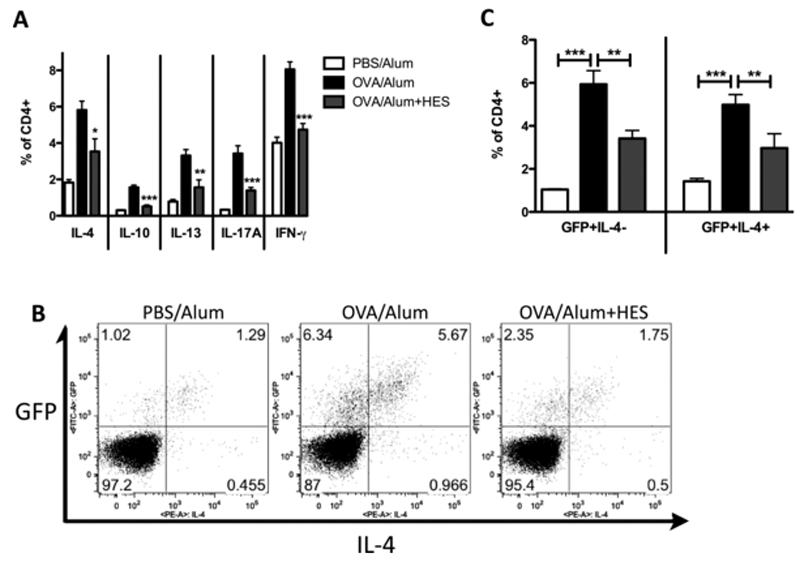
The innate and antibody responses associated with asthma were suppressed by HES, so we assessed whether this was accompanied by a reduced T cell cytokine response in the lung. We found that lung CD4+ T cell production of IL-4, IL-10, IL-13, IL-17A and IFN-γ were all suppressed by coadministration of HES (Figure 6 A). To distinguish whether suppression was due to reduced Th2 differentiation, or inhibition of cytokine production by Th2-committed T cells, we administered OVA with and without HES to 4-get mice; in these mice, commitment to the Th2 pathway initiates GFP production prior to the expression of IL-4 protein [62]. Co-staining of lung lymphocytes for GFP and intracellular IL-4 protein showed that HES coadministration reduced both GFP+IL-4− (committed to Th2 but not currently producing IL-4) and GFP+IL-4+ (Th2 cells currently producing IL-4) populations (Figure 6 B and C), indicating that HES interferes with the initial differentiation of Th2 cells.
Figure 6. HES treatment reduces T-cell cytokine production.
HES was co-administered with OVA-Alum sensitisations in 4-get mice. Following challenge at days 28-30, cells were prepared from liberase/DNAse-digested lung tissue, stimulated with PMA and Ionomycin in the presence of Brefeldin A, and stained for CD4 and intracellular IL-4, IL-10, IL-13, IL-17A and IFN-γ for flow cytometry. Shown are (A) the IL-4+, IL-10+, IL-13+, IL-17A+ and IFN-γ+ proportions of the CD4+ population, (B) representative flow cytometry plots of GFP vs IL-4 in CD4+ lymphocytes and (C) the proportions of CD4+ cells which were GFP+IL-4− and GFP+IL-4+.
Data are representative of 2 repeat experiments, each with 4-6 mice per group. Error bars are SEM. *p<0.05, **p<0.01, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
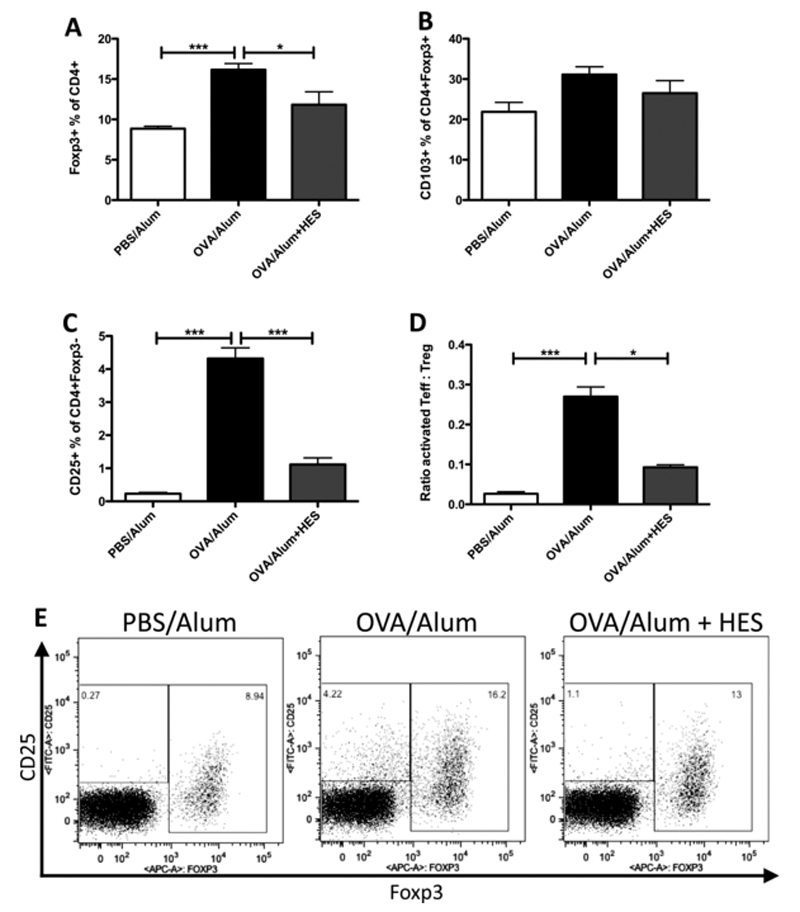
2.7. Treg cell numbers do not expand with HES treatment
HES has been previously shown to induce expression of the Treg cell canonical transcription factor Foxp3 in stimulated CD4+ cells in vitro [54]. We therefore assessed levels of CD4+Foxp3+ cells in the lung after HES administration. Fig. 7 A shows that Treg cell frequencies within the CD4+ population in the lung tissue are higher following OVA sensitisation alone than with HES co-administration. Activation of Treg cells, as assessed by CD103 expression by CD4+Foxp3+ cells, was also unaffected by HES administration (Fig 7 B). However, proportions of activated effector T helper cells (CD4+CD25+Foxp3−) are very significantly decreased with HES administration (Fig. 7 C). Hence the ratio of activated effector T helper to Treg cells is significantly reduced in mice receiving HES co-administration, potentially shifting the balance in favour of Tregs (Fig. 7 D). Representative FACS plots are shown in Fig 7 E.
Figure 7. HES treatment reduces Treg- and Teffector-cell accumulation.
20 μg HES was coadministered with each sensitisation injection of OVA-Alum on d0 and d14, and following challenge at days 28-30, cells were prepared from liberase/DNAse-digested lung tissue and stained for CD4, CD25, CD103 and Foxp3 for flow cytometry. Shown are (A) the Foxp3+ proportion of CD4+ cells, (B) the CD103+ proportion of CD4+Foxp3+ cells, (C) the percentage of CD25+ cells among CD4+Foxp3− cells, (D) the ratio of activated effector T cells (CD4+Foxp3−CD25+) to Treg cells (CD4+Foxp3+) and (E) representative flow cytometry plots of CD4+ cells showing Foxp3 versus CD25. Data are representative of 2 repeat experiments, each with 4-6 mice per group. Error bars are SEM. *p<0.05, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
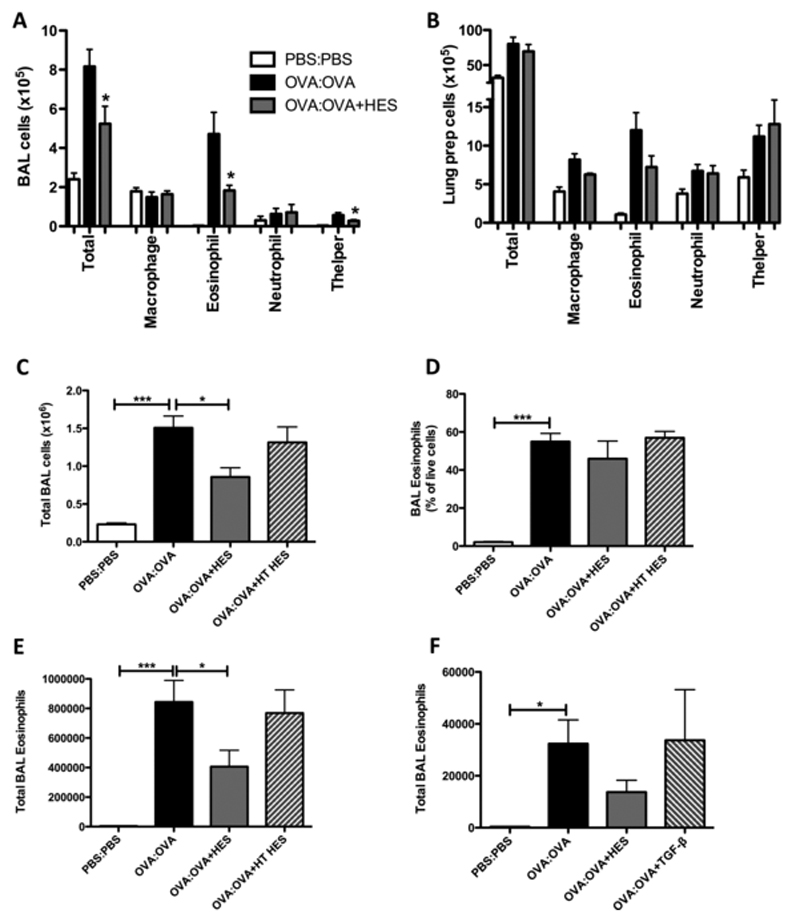
2.8. Inhibition of airway eosinophilia by HES administered with allergen challenge
To test the potential of HES components to suppress established responses, we next administered HES with the OVA intratracheal challenges to mice which had first been sensitised with OVA-alum alone. In this challenge model we again found significantly lower numbers of BAL total cells, eosinophils and CD4+ T helper cells (Fig. 8 A). However, in the lung tissue only eosinophils showed any marked negative trend, and none of the changes reached statistical significance (Fig 8 B). In this challenge setting, only intact and not heat-inactivated HES was able to suppress total (Fig 8 C) and eosinophil (Fig. 8 D) cell numbers, and the effect was primarily on eosinophil numbers rather than the proportions of eosinophils within the total inflammatory infiltrate (Fig. 8 E). As in HES at sensitisation, replacement of HES with an equivalent amount of recombinant mammalian TGF-β did not protect against eosinophil accumulation (Fig. 8 F).
Figure 8. HES treatment at challenge suppresses eosinophil responses, while heat-treated HES or mammalian TGF-β does not.
All mice were sensitised with OVA-Alum on d0 and d14, then 20 μg HES (or controls of 20 μg heat-treated HES (HT HES) or 4 ng recombinant mammalian TGF-β (TGF)) were coadministered with challenge of 20 μg OVA protein administered intratracheally on days 28-30. Bronchoalveolar lavage (BAL) cells and lung tissue for cell preparation were collected at day 31. Shown are (A) the numbers of total BAL cells and cell types, (B) the numbers of total lung preparation cells and cell types, (C) the total BAL cell numbers with HT HES control, (D) SiglecF+CD11c− BAL eosinophil numbers with HT HES control (E) SiglecF+CD11c− proportions of total BAL cells with HT HES control, and (F) SiglecF+CD11c− BAL eosinophil numbers with TGF-β control. Results are representative of 3 repeat experiments, each with 4-6 mice per group. Error bars are SEM. *p<0.05, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
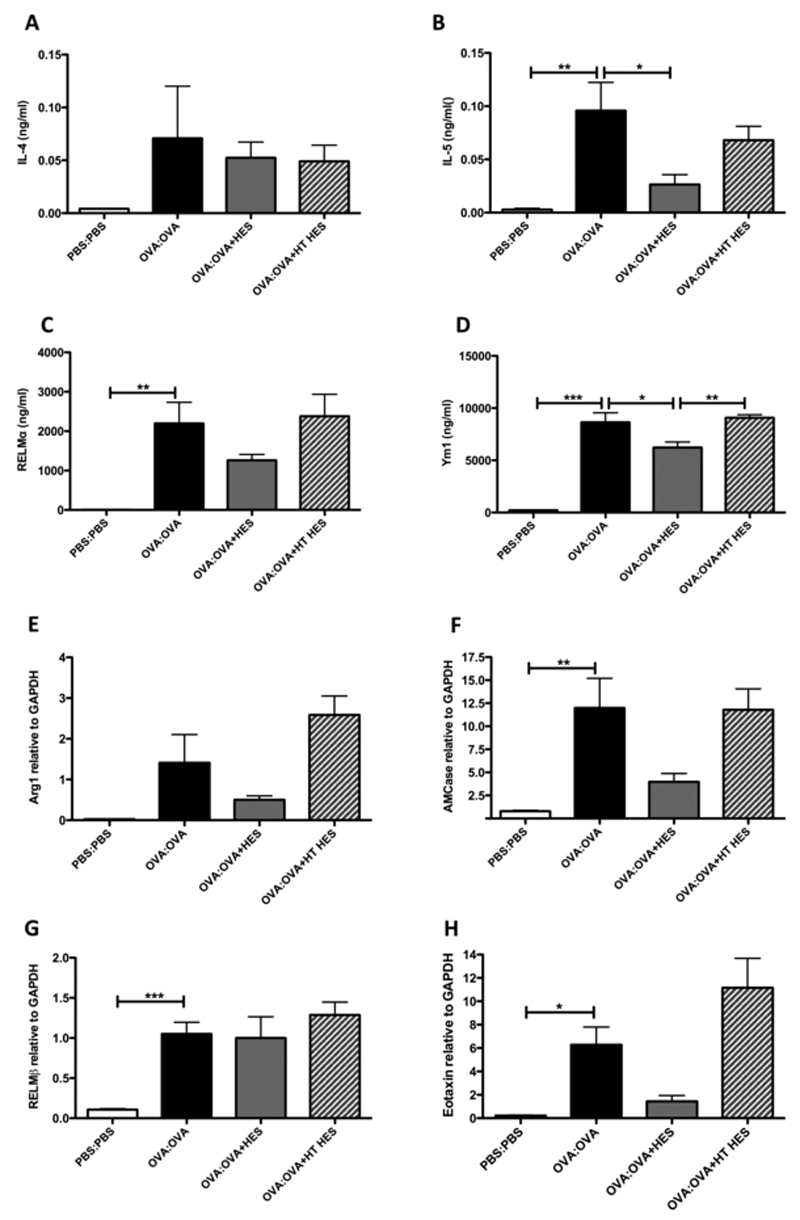
In recipients of intratracheal HES with OVA, BAL fluid also contained lower levels of IL-5, while IL-4 appeared unchanged (Fig. 9 A, B). Levels of RELM-α and Ym1 in the BALF were also lower with HES administration, and unaffected by heat-treated HES, although only attaining significance with Ym1 (Fig. 9 C, D). Transcription of the type 2 innate response markers Arginase-1 and AMCase again tended to be suppressed (Fig. 9 E, F), whereas RELM-β was unaltered (Fig. 9 G). Likewise, levels of eotaxin/CCL11 showed a downward trend with HES administration which was absent with heat-inactivated HES (Fig. 9 H).
Figure 9. HES treatment at challenge suppresses type 2 response markers.
Cell-free BAL supernatants from the experiment shown in Figure 8 B-D were tested (A, B) by CBA for levels of (A) IL-4 and (B) IL-5, and (C, D) by ELISA for levels of (C) RELM-α and (D) Ym1 protein. (E-H) RNA was prepared from lung tissue and qRT-PCR used to assess levels of (E) Arginase-1, (F) AMCase, (G) RELM-β and (H) eotaxin transcription relative to GAPDH. Results are representative of 2 repeat experiments, each with 4-6 mice per group. Error bars are SEM. * p<0.05, **p<0.01, ***p<0.001, one-way ANOVA, with a Tukey’s post test.
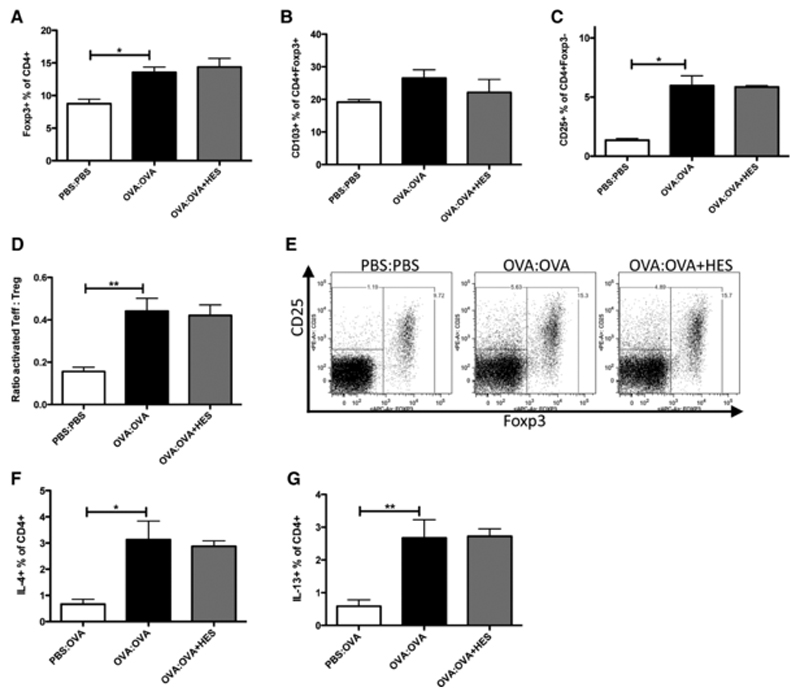
We again determined frequencies of Foxp3+ and CD103+Foxp3+ Tregs in allergic mice. Levels of Foxp3+, and CD103+Foxp3+ Tregs increased in OVA-sensitised and challenged animals, and in contrast to HES given at sensitisation, when HES was given at challenge this was unchanged (Fig. 10 A, B). CD4+Foxp3−CD25+ activated effector cells were again increased with asthma induction, and were also unchanged by HES administration (Fig. 10 C), as was the ratio of activated effector T helper cells (Fig 10 D). Representative FACS plots are shown in Fig. 10 E. To further examine the Th2 response with HES at challenge, lung tissue CD4+ cells were stained for intracellular IL-4 and IL-13 (Fig 10 F and G), but consistent with undiminished activation of Foxp3− T cells, no difference in expression of these Th2 cytokines was seen with HES at challenge.
Figure 10. HES at challenge does not affect T-cell accumulation or cytokine production in the lung.
(A-E) Lung tissue cells were prepared from the experiment shown in Figure 8A and stained for CD4, CD25, CD103 and Foxp3 for flow cytometry. Shown are (A) the Foxp3+ proportion of CD4+ cells, (B) the CD103+ proportion of CD4+Foxp3+ cells, (C) the percentage of CD25+ cells among CD4+Foxp3− cells, (D) the ratio of activated effector T cells (CD4+Foxp3−CD25+) to Treg cells (CD4+Foxp3+) and (E) representative flow cytometry plots of CD4+ cells showing Foxp3 verses CD25. Results are representative of 2 repeat experiments with 4-6 mice per group. (F, G) In the second experiment, lung tissue cells from 5 individual mice were stimulated with PMA, Ionomycin and Brefeldin A for 4 hours, and stained for CD4 and intracellular (F) IL-4 and (G) IL-13 by flow cytometry. Error bars are SEM. *p<0.05, **p<0.01, one-way ANOVA, with a Tukey’s post test.
3. Discussion
The influence of infections on the induction and progression of allergic disease is under increasing scrutiny in both epidemiological and experimental studies [63–65]. Helminth parasites in particular are associated with a degree of protection from allergic reactivity [3,4]. However, due to the heterogeneity of human exposure and the diversity of helminth species, current evidence is not always consonant with a causal link between infection and reduction of allergy [2]. Hence, investigations with defined laboratory models are essential to dissect the interactions that are likely to occur in humans, and to exploit any molecular principle from parasites that may be beneficial in ameliorating immunopathology.
In this report, we show that the murine intestinal helminth H. polygyrus releases soluble factors which potently suppress immune responses and pathology in an experimental model of allergic inflammation. These molecules suppress a wide span of innate and adaptive immune responses if co-administered with the initial sensitizing injections, and key markers of innate inflammation (in particular, eosinophilia) when given to mice only at the challenge phase. Because of the breadth of effects, and the fact that initial suppression is mediated by heat-stable components and the challenge inhibition by heat-labile molecules, we hypothesise that HES contains multiple suppressive factors, those that can suppress initiation of adaptive immune responses, and factors which inhibit recruitment or expansion of allergic innate effector cells to the lung.
The suppression of allergy when helminth products are given at sensitisation may be common to other parasites, as N. brasiliensis ES adsorbed with OVA on Alum reduces the subsequent allergic response [49]. However suppression of the BAL eosinophil response when ES is given at challenge has not, to our knowledge, been previously shown. A possible mechanism by which HES could inhibit sensitisation is by enzymatic modification of OVA; however, the fact that heat-treated HES is effective at sensitisation makes it unlikely that any enzymatic effect is responsible. While the protective component in the challenge setting is heat-labile, T cell responses to OVA are unchanged in this model, again arguing that there is no defect in presentation of OVA to T cells due to modification of the allergen. Hence, in both cases we favour the hypothesis that HES acts directly on inducer and effector components of the immune response.
In blocking adaptive responses, we found not only that lung Th2 cytokine levels were profoundly inhibited by HES co-administration at sensitisation, but also the Th1 cytokine IFN-γ, arguing that allergy inhibition was not achieved simply by immune deviation towards the Th1 mode. Intracellular cytokine staining showed suppression of Th2, Th1 and Th17 cells with HES co-administration and the suppression of OVA-specific antibody was also observed across all isotypes, consistent with this conclusion. Among the innate populations, the abrogation of eosinophil infiltration (along with eosinophil-stimulating factors IL-5 and eotaxin/CCL11) was highly significant, as this subset is most closely associated with airway pathology [66,67]. Downregulation of eotaxin in particular could lead to the suppression of eosinophil recruitment to the airways seen with HES administration at challenge. Due to the brief time-frame of the challenge protocol, this observation implies that HES may directly impact on the eosinophil population, and does not act indirectly through an adaptive (eg Th2) compartment which is unaffected by the challenge-only administration of HES.
We also observed striking changes in type 2 innate response markers. These markers, such as Ym1 and RELM-α, were initially discovered in alternatively activated macrophages, and more recently shown to be produced at high levels by epithelial cells in allergic inflammation models [61]). We had hypothesised that HES, similar to secretions from other helminths [68] can drive alternatively activated macrophages, which would in turn act in an immunosuppressive mode to block the Th2 allergic immune response. In contrast, we saw instead a highly significant reduction in type 2 innate response markers, indicating an unexpected inhibition of alternatively activated macrophages. Because these type 2 innate response markers are exquisitely Th2-dependent (through IL-4Rα), these changes might simply be downstream consequences of a suppressed Th2 response in the lung. However, the clear suppression of Ym1 by HES at challenge argues, as with eosinophils, that inhibition may act directly on innate cells and not through an intermediary Th2 cell. It is possible, however, that allergic eosinophil expansion is dependent upon AAMs in the lung, in a manner parallel to that recently reported for adipose tissue [69]. Because the apparent roles of AAMs in helminth immunity and asthma exacerbation vary between experimental models, it will be fascinating to dissect their activity further in this system, especially with the new range of specific antibodies and inhibitors of AMM products now becoming available [70].
When HES was administered with OVA at the sensitisation phase of the airway allergy model, we also observed downregulation of the type 2 immune response epithelial cytokine RELM-β. Interestingly, this molecule has been more closely associated with the intestinal epithelium, and in that setting acts as an innate defensin-like molecule to inhibit survival of H. polygyrus adult worms [71]. Inhibition of RELM-β in the airways may nevertheless contribute to amelioration of allergy, as RELM-β-deficient mice show reduced goblet cell hyperplasia and other inflammatory reactions following allergen challenge [72].
Mice treated with HES at sensitisation also showed very potent suppression of anti-OVA IgG1 and especially IgE responses. It is interesting to speculate how HES may interrupt humoral immunity so profoundly. H. polygyrus infection is known to induce a regulatory population of B cells, which can suppress airway allergy on transfer [31]. Thus, in the context of HES administration, suppression of OVA-specific IgE responses may reflect skewing of the B cell population to a regulatory phenotype. However, as shown by Wilson et al, neither infection with H. polygyrus [31] nor transfer of the regulatory B cell population [32] resulted in suppression of the allergen-specific IgG1 or IgE response. Therefore, HES may invoke a mechanism to inhibit anti-parasite antibody responses, which when co-administered with a bystander allergen (in this case, OVA), extends to that antigen also. In H. polygyrus infections, neither the T cell nor B cell mediated suppression of asthma is dependent on IL-10, and as no increase in total, or CD4+ T cell-derived, IL-10 was seen with HES administration, other host regulatory cytokines (eg TGF-β) may be involved.
Our results show that HES at sensitisation can potently inhibit Th2 responses and pathology in a widely-studied OVA-induced asthma model. This model depends on the systemic sensitisation of mice with OVA protein in an aluminium hydroxide adjuvant, inducing a Th2 response which can be recalled in the airways. However, the induction of allergy in humans is more likely to be induced directly in the airways by exposure to environmental allergens. Thus we are presently extending our results with other regimens giving allergen repeatedly without adjuvant directly into the airways. Furthermore, suppression of Th2 responses, however they are initiated, is of relevance not only to allergy and the control of Th2-mediated parasite expulsion from the host. For example, it has been noted that immunity induced by vaccines, most of which employ alum adjuvant, is suppressed in helminth endemic areas [17,73], possibly through pathways replicated by HES.
Our laboratory has recently completed a proteomic analysis of HES [51], which will facilitate identification of the molecular product(s) in HES that mediate protection. In addition to ascertaining the suppressive molecular principle(s) from H. polygyrus, future research needs also to characterise the immunological mechanism and pathway of suppression. In the first instance, the question should be addressed of which host cells are targeted by HES. Previous work on H. polygyrus infection has highlighted the parasite’s suppressive effects through dendritic cells [74–76], Tregs [31,77,78] and regulatory B cells [31]. Other work on products derived from H. polygyrus has shown roles for induction of suppressive dendritic cells [53] and Tregs [54]. HES contains a TGF-β mimic which is capable of inducing Tregs in vitro [54], and we hypothesised that HES could suppress allergic immune responses through this pathway. Our data, however, argues against suppression dependent on the TGF-β pathway or Treg induction: an equivalent amount of recombinant mammalian TGF-β could not suppress allergic immune responses at sensitisation or at challenge; HES suppression at sensitisation was heat-stable, while the HES TGF-β signal is heat-labile [54]; and Treg proportions, numbers and activation levels were lower with HES administration at sensitisation than in positive controls. Therefore we hypothesise that HES contains other immunomodulatory factors than the TGF-β mimic, and these are largely responsible for the suppressive effect seen with HES administration at sensitisation. When HES is administered challenge the suppression by HES is heat-labile and therefore the suppression could be due to the TGF-β mimic. However the Treg population was unchanged by HES administration at challenge and mammalian TGF-β could not replicate the suppressive effect, therefore we believe it is unlikely that the TGF-β mimic is entirely responsible. We are presently carrying out experiments using TGF-βR signalling inhibitors to formally exclude this possibility.
In summary, here we present data showing that HES administration can replicate the suppressive effects of H. polygyrus infection on airway allergy. These effects are likely to be mediated by multiple factors, and are unlikely to be solely attributed to the TGF-β-like activity contained in HES. As HES could also suppress airway eosinophilia once an immune response had been established, we propose that it may contain possible therapeutics for human disease. We are now using fractionation, proteomic and genomic techniques to attempt to identify the suppressive factor(s) in HES.
4. Materials and Methods
Parasites and HES
The life cycle of Heligmosomoides polygyrus bakeri was maintained as described elsewhere [79]. Adult excretory-secretory products were prepared as previously described [80], and when tested in the Limulus Amoebocyte Lysate assay (Lonza), was found to contain less than 0.1 IU LPS per μg protein. Heat-inactivation was performed by incubation at 100°C for 20 minutes. Class IV Ovalbumin and BSA were purchased from Sigma.
Mice
BALB/c or 4-get [62] (heterozygous with BALB/c) mice were bred in-house at the University of Edinburgh and accommodated according to Home Office regulations.
Airway allergy model
Induction of airway allergic inflammation was performed as previously described [31]. Briefly, mice were sensitised with two injections (d0 and d14) of 20 μg OVA precipitated with alum, i.p. At days 28, 29 and 30 mice were challenged with an aerosol of 1% OVA protein in PBS, or by intratracheal instillation of 20 μg OVA in PBS, as indicated. At day 31, the bronchoalveolar space was lavaged, and lungs taken for analysis. Serum was collected at this time point.
Lung histology and immunohistochemistry
Lungs were lavaged with, and collected into, 10 % buffered formalin, incubated overnight at 4°C, then transferred to 70% ethanol. Lungs were then paraffin embedded and sectioned, before being stained with standard protocols for Haemotoxylin and Eosin and Periodic Acid-Schiff. For immunohistochemical staining, sections were stained with rabbit anti-RELM-α (Peprotech), and a goat anti-rabbit secondary antibody (Vector labs). Staining was detected with horseradish peroxidase and 3,3-diaminobenzidine.
Flow cytometry
Single cell suspensions of lung tissue were prepared by digesting the right lobes of the lung in 2 U/ml liberase TL (Roche) and 80 U/ml DNase (Invitrogen) at 37°C with agitation for 25 min, followed by maceration through a 70 μm cell strainer. Cells were phenotyped by labelling with fluorescently-labelled antibodies to CD4, CD11b, CD11c, CD25, CD103, Foxp3, GR1, and SiglecF, or the relevant isotype controls before analysing by FACS (all antibodies from BD Biosciences).
Where intracellular cytokine staining was carried out, cells were stimulated for 4 hours at 37°C with 500 ng/ml Phorbol Myristate Acetate, 1 μg/ml Ionomycin and 10 μg/ml Brefeldin A (Sigma). Cells were stained for CD4, then permeabilised using the manufacturers instructions with the BD Biosciences Fixation/Permeabilisation kit. Cells were then stained for IFN-γ, IL-4, IL-10, IL-13 and IL-17A. After permeabilisation, GFP in 4-get mice was detected using polyclonal rabbit anti-GFP (Ebioscience), followed by anti-rabbit IgG-Alexa Fluor 488 (Invitrogen). Live/dead Aqua (Invitrogen) was used to exclude dead cells. Samples were analyzed by flow cytometry using Becton-Dickinson FACSCanto or LSR-II flow cytometers. BAL and lung tissue cell types were characterised as: CD11c+SiglecF+ (alveolar macrophages), SiglecF+CD11c− (eosinophils), CD11bhiCD11c−GR1hiSiglecF− (neutrophils) and CD4+CD11b− (T helper cells).
ELISA
Antibody levels in serum were measured on OVA-coated ELISA plates, and serial dilutions of serum. To measure IgE levels, serum was first depleted of IgG using 4 Fast Flow Protein G Sepharose beads (Amersham), according to the manufacturer’s instructions. IgG1 was detected with goat anti-mouse IgG1-HRP (Southern Biotech) and IgE was detected using rat anti-mouse IgE-biotin followed by streptavidin-alkaline phosphotase (Sigma).
The type 2 innate response markers RELM-α and Ym-1 were measured by ELISA, using the rabbit anti-mouse RELM-α, then biotinylated rabbit anti-mouse RELM-α, compared to a recombinant RELM-α standard (Peprotech), or the Chitinase 3-like/ECF-L (Ym1) Duoset kit (R&D Systems) according to manufacturer’s instructions.
Cytokine CBA
Cytokine levels were detected in cell-free BAL supernatant or lung homogenate. A section of the left lobe of the lung was homogenised using a Tissuelyser (QIAGEN) in 0.5 ml of 1x cell lysis buffer (Cell Signalling), containing 1 μM PMSF (Sigma). IL-4, IL-5, IL-10, IL-13, and IFN-γ levels were detected using BD CBA Flex-set kits, and were acquired on a BD FACSArray. Levels of cytokines in lung homogenates were normalised by dividing by total protein concentration, as assessed by Bradford assay compared to a BSA standard (Pierce).
RT-PCR
A section of the left lobe of the lung was homogenised on a Tissuelyser (QIAGEN) in Trizol reagent (Invitrogen), and RNA prepared according to manufacturers instructions. Reverse transcription was performed using 1-2 μg of RNA, 2 μl 10 reverse transcriptase buffer, 2 μl 25 mM dNTP mix, 1 μl of 50 U/μl MMLV reverse transcriptase, 0.5 μl of 40 U/μl RNAsin, 1 μl of 0.4 μg/ml Oligo dT primer, and made up to 20 μl with DEPC treated water. A PCR block (Peltier Thermal Cycler, MJ Research) was used for the transcription reaction, 20°C for 10 min, 37°C for 60 min, and 99°C for 5 min.
Transcript levels of the genes of interest were measured by real-time PCR using the Lightcycler 480 II (Roche). PCR amplifications were carried out in 10 μl total volume made up of 1 μl cDNA, 5 μl SYBR Green (Roche), 0.3 μl of each primer (10 μM) (Table), and 3.4 μl DEPC treated water (Ambion). The amplifications were performed using the following protocol: 30 s denaturation at 95°C, 5 s for primers to anneal at 65°C, 12 s elongation at 72°C, for 40 cycles. Primers used are shown in Table 1.
Table 1. Primers used for real-time PCR.
| Gene | Forward primer | Reverse primer | Amplicon length |
|---|---|---|---|
| Arg-1 | CAGAAGAATGGAAGAGTCAG | CAGATAT-GCAGGGAGT-CACC | 249 |
| AMCase | CCCTTG-GCA-TATC-CACTGA | ACAGAA-TCCACTGCC-TCCAG | 125 |
| GAPDH | ATGACA-TCAAGAA-GGTGGTG | CATACCA-GGAAATG-AGCTTG | 177 |
| RELM-β | CGTCTC-CCTTTTC-CCACTG | CAGGAG-ATCGTCTTAG-GCTCTT | 114 |
| Eotaxin | CACGGTCA-CTTCCTTC-ACCT | TGG-GGATCTT-CTTACT-GGTCA | 92 |
Statistics
All data was analysed using Prism 5 (Graphpad). Groups were analysed by one-way ANOVA, with a Tukey’s post test comparing all groups to the OVA only positive control. Unless otherwise indicated differences are not significant. *** = p<0.001, ** = p<0.01, * = p<0.05.
Acknowledgements
We gratefully acknowledge grant funding support from the Medical Research Council (MTO’G and KJF), the American Asthma Foundation (NB and HJMcS), Asthma UK (TES) and the Wellcome Trust. We also thank Yvonne Harcus and Elaine Robertson for assistance with the H. polygyrus life cycle.
Abbreviations
- AAM
alternatively activated macrophage
- AMCase
acidic mammalian chitinase
- BAL
bronchoalveolar lavage
- HES
H. polygyrus excretory-secretory products
- IBD
inflammatory bowel disease
- OVA
ovalbumin
- RELM
resistin-like molecule
Footnotes
Conflict of interest
The authors declare no financial or commercial conflict of interest.
References
- 1.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355:2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 2.Cooper PJ. Interactions between helminth parasites and allergy. Curr Opin Allergy Clin Immunol. 2009;9:29–37. doi: 10.1097/ACI.0b013e32831f44a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flohr C, Quinnell RJ, Britton J. Do helminth parasites protect against atopy and allergic disease? Clin Exp Allergy. 2009;39:20–32. doi: 10.1111/j.1365-2222.2008.03134.x. [DOI] [PubMed] [Google Scholar]
- 4.Smits HH, Everts B, Hartgers FC, Yazdanbakhsh M. Chronic helminth infections protect against allergic diseases by active regulatory processes. Current allergy and asthma reports. 2010;10:3–12. doi: 10.1007/s11882-009-0085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Araujo MI, Lopes AA, Medeiros M, Cruz AA, Sousa-Atta L, Solé D, Carvalho EM. Inverse association between skin response to aeroallergen and Schistosoma mansoni infection. Int Arch Allergy Immunol. 2000;123:145–148. doi: 10.1159/000024433. [DOI] [PubMed] [Google Scholar]
- 6.van den Biggelaar A, van Ree R, Roderigues LC, Lell B, Deelder AM, Kremsner PG, Yazdanbakhsh M. Decreased atopy in children infected with Schistosoma haematobium : a role for parasite-induced interleukin-10. Lancet. 2000;356:1723–1727. doi: 10.1016/S0140-6736(00)03206-2. [DOI] [PubMed] [Google Scholar]
- 7.Nyan OA, Walraven GEL, Banya WAS, Milligan P, Van Der Sande M, Ceesay SM, Del Prete G, McAdam KPWJ. Atopy, intestinal helminth infection and total serum IgE in rural and urban adult Gambian communities. Clin Exp Allergy. 2001;31:1672–1678. doi: 10.1046/j.1365-2222.2001.00987.x. [DOI] [PubMed] [Google Scholar]
- 8.Scrivener S, Yemaneberhan H, Zebenigus M, Tilahun D, Girma S, Ali S, McElroy P, et al. Independent effects of intestinal parasite infection and domestic allergen exposure on risk of wheeze in Ethiopia: a nested case-control study. Lancet. 2001;358:1493–1499. doi: 10.1016/S0140-6736(01)06579-5. [DOI] [PubMed] [Google Scholar]
- 9.Dagoye D, Bekele Z, Woldemichael K, Nida H, Yimam M, Hall A, Venn AJ, et al. Wheezing, allergy, and parasite infection in children in urban and rural Ethiopia. Am J Respir Crit Care Med. 2003;167:1369–1373. doi: 10.1164/rccm.200210-1204OC. [DOI] [PubMed] [Google Scholar]
- 10.Cooper PJ. Intestinal worms and human allergy. Parasite Immunol. 2004;26:455–467. doi: 10.1111/j.0141-9838.2004.00728.x. [DOI] [PubMed] [Google Scholar]
- 11.Lynch NR, Hagel I, Perez M, Di Prisco MC, Lopez R, Alvarez N. Effect of anthelmintic treatment on the allergic reactivity of children in a tropical slum. Journal of Allergy and Clinical Immunology. 1993;92:404–411. doi: 10.1016/0091-6749(93)90119-z. [DOI] [PubMed] [Google Scholar]
- 12.van den Biggelaar AH, Rodrigues LC, van Ree R, van der Zee JS, Hoeksma-Kruize YC, Souverijn JH, Missinou MA, et al. Long-term treatment of intestinal helminths increases mite skin-test reactivity in Gabonese schoolchildren. J Infect Dis. 2004;189:892–900. doi: 10.1086/381767. [DOI] [PubMed] [Google Scholar]
- 13.Flohr C, Tuyen LN, Quinnell RJ, Lewis S, Minh TT, Campbell J, Simmons C, et al. Reduced helminth burden increases allergen skin sensitization but not clinical allergy: a randomized, double-blind, placebo-controlled trial in Vietnam. Clin Exp Allergy. 2009 doi: 10.1111/j.1365-2222.2009.03346.x. [DOI] [PubMed] [Google Scholar]
- 14.Wilson MS, Maizels RM. Regulation of allergy and autoimmunity in helminth infection. Clin Rev Allerg Immunol. 2004;26:35–49. doi: 10.1385/CRIAI:26:1:35. [DOI] [PubMed] [Google Scholar]
- 15.Fallon PG, Mangan NE. Suppression of Th2-type allergic reactions by helminth infection. Nat Rev Immunol. 2007;7:220–230. doi: 10.1038/nri2039. [DOI] [PubMed] [Google Scholar]
- 16.Danilowicz-Luebert E, O'Regan NL, Steinfelder S, Hartmann S. Modulation of specific and allergy-related immune responses by helminths. J Biomed Biotechnol. 2011;2011:821578. doi: 10.1155/2011/821578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McSorley HJ, Maizels RM. Helminth infections and host immune regulation. Submitted for publication. 2012 doi: 10.1128/CMR.05040-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leonardi-Bee J, Pritchard D, Britton J. Asthma and current intestinal parasite infection: systematic review and meta-analysis. Am J Respir Crit Care Med. 2006;174:514–523. doi: 10.1164/rccm.200603-331OC. [DOI] [PubMed] [Google Scholar]
- 19.Smits HH, Hammad H, van Nimwegen M, Soullie T, Willart MA, Lievers E, Kadouch J, et al. Protective effect of Schistosoma mansoni infection on allergic asthma depends on intensity and chronicity of infection. J Allergy Clin Immunol. 2007;120:932–940. doi: 10.1016/j.jaci.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 20.Summers RW, Elliott DE, Qadir K, Urban JF, Jr, Thompson R, Weinstock JV. Trichuris suis seems to be safe and possibly effective in the treatment of inflammatory bowel disease. Am J Gastroenterol. 2003;98:2034–2041. doi: 10.1111/j.1572-0241.2003.07660.x. [DOI] [PubMed] [Google Scholar]
- 21.Summers RW, Elliott DE, Urban JF, Jr, Thompson RA, Weinstock JV. Trichuris suis therapy for active ulcerative colitis: a randomized controlled trial. Gastroenterology. 2005;128:825–832. doi: 10.1053/j.gastro.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Bager P, Arnved J, Rønborg S, Wohlfahrt J, Poulsen LK, Westergaard T, Petersen HW, et al. Trichuris suis ova therapy for allergic rhinitis: A randomized, double-blind, placebo-controlled clinical trial. J Allergy Clin Immunol. 2010;125:123–130. doi: 10.1016/j.jaci.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Blount D, Hooi D, Feary J, Venn A, Telford G, Brown A, Britton J, Pritchard D. Immunologic profiles of persons recruited for a randomized, placebo-controlled clinical trial of hookworm infection. Am J Trop Med Hyg. 2009;81:911–916. doi: 10.4269/ajtmh.2009.09-0237. [DOI] [PubMed] [Google Scholar]
- 24.Daveson AJ, Jones DM, Gaze S, McSorley H, Clouston A, Pascoe A, Cooke S, et al. Effect of hookworm infection on wheat challenge in celiac disease--a randomised double-blinded placebo controlled trial. PLoS ONE. 2011;6:e17366. doi: 10.1371/journal.pone.0017366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McSorley HJ, Gaze S, Daveson J, Jones D, Anderson RP, Clouston A, Ruyssers NE, et al. Suppression of inflammatory immune responses in celiac disease by experimental hookworm infection. PLoS ONE. 2011;6:e24092. doi: 10.1371/journal.pone.0024092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaze S, McSorley HJ, Daveson J, Jones D, Bethony JM, Oliveira LM, Speare R, et al. Characterising the mucosal and systemic immune responses to experimental human hookworm infection. PLoS Pathog. 2012;8:e1002520. doi: 10.1371/journal.ppat.1002520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Correale J, Farez M. Association between parasite infection and immune responses in multiple sclerosis. Ann Neurol. 2007;61:97–108. doi: 10.1002/ana.21067. [DOI] [PubMed] [Google Scholar]
- 28.Correale J, Farez M. Helminth antigens modulate immune responses in cells from multiple sclerosis patients through TLR2-dependent mechanisms. J Immunol. 2009;183:5999–6012. doi: 10.4049/jimmunol.0900897. [DOI] [PubMed] [Google Scholar]
- 29.Correale J, Farez MF. The impact of parasite infections on the course of multiple sclerosis. J Neuroimmunol. 2011;233:6–11. doi: 10.1016/j.jneuroim.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Broadhurst MJ, Leung JM, Kashyap V, McCune JM, Mahadevan U, McKerrow JH, Loke P. IL-22+ CD4+ T cells are associated with therapeutic Trichuris trichiura infection in an ulcerative colitis patient. Sci Transl Med. 2010;2:60ra88. doi: 10.1126/scitranslmed.3001500. [DOI] [PubMed] [Google Scholar]
- 31.Wilson MS, Taylor M, Balic A, Finney CAM, Lamb JR, Maizels RM. Suppression of allergic airway inflammation by helminth-induced regulatory T cells. J Exp Med. 2005;202:1199–1212. doi: 10.1084/jem.20042572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilson MS, Taylor MD, O'Gorman MT, Balic A, Barr TA, Filbey K, Anderton SM, Maizels RM. Helminth-induced CD19+CD23hi B cells modulate experimental allergic and autoimmune inflammation. Eur J Immunol. 2010;40:1682–1696. doi: 10.1002/eji.200939721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bashir ME, Andersen P, Fuss IJ, Shi HN, Nagler-Anderson C. An enteric helminth infection protects against an allergic response to dietary antigen. J Immunol. 2002;169:3284–3292. doi: 10.4049/jimmunol.169.6.3284. [DOI] [PubMed] [Google Scholar]
- 34.Kitagaki K, Businga TR, Racila D, Elliott DE, Weinstock JV, Kline JN. Intestinal helminths protect in a murine model of asthma. J Immunol. 2006;177:1628–1635. doi: 10.4049/jimmunol.177.3.1628. [DOI] [PubMed] [Google Scholar]
- 35.Elliott DE, Setiawan T, Metwali A, Blum A, Urban JF, Jr, Weinstock JV. Heligmosomoides polygyrus inhibits established colitis in IL-10-deficient mice. Eur J Immunol. 2004;34:2690–2698. doi: 10.1002/eji.200324833. [DOI] [PubMed] [Google Scholar]
- 36.Sutton TL, Zhao A, Madden KB, Elfrey JE, Tuft BA, Sullivan CA, Urban JF, Jr, Shea-Donohue T. Anti-Inflammatory mechanisms of enteric Heligmosomoides polygyrus infection against trinitrobenzene sulfonic acid-induced colitis in a murine model. Infect Immun. 2008;76:4772–4782. doi: 10.1128/IAI.00744-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hang L, Setiawan T, Blum AM, Urban J, Stoyanoff K, Arihiro S, Reinecker HC, Weinstock JV. Heligmosomoides polygyrus infection can inhibit colitis through direct interaction with innate immunity. J Immunol. 2010;185:3184–3189. doi: 10.4049/jimmunol.1000941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saunders KA, Raine T, Cooke A, Lawrence CE. Inhibition of autoimmune type 1 diabetes by gastrointestinal helminth infection. Infect Immun. 2006;75:397–407. doi: 10.1128/IAI.00664-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Q, Sundar K, Mishra PK, Mousavi G, Liu Z, Gaydo A, Alem F, et al. Helminth infection can reduce insulitis and type 1 diabetes through CD25- and IL-10-independent mechanisms. Infect Immun. 2009;77:5347–5358. doi: 10.1128/IAI.01170-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maizels RM, Hewitson JP, Murray J, Harcus Y, Dayer B, Filbey KJ, Grainger JR, et al. Immune modulation and modulators in Heligmosomoides polygyrus infection. Exp Parasitol. 2011 doi: 10.1016/j.exppara.2011.08.011. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mortimer K, Brown A, Feary J, Jagger C, Lewis S, Antoniak M, Pritchard D, Britton J. Dose-ranging study for trials of therapeutic infection with Necator americanus in humans. Am J Trop Med Hyg. 2006;75:914–920. [PubMed] [Google Scholar]
- 42.Harnett W, Harnett MM. Therapeutic immunomodulators from nematode parasites. Expert reviews in molecular medicine. 2008;10:e18. doi: 10.1017/S1462399408000720. [DOI] [PubMed] [Google Scholar]
- 43.Cançado GG, Fiuza JA, de Paiva NC, Lemos LD, Ricci ND, Gazzinelli-Guimarães PH, Martins VG, et al. Hookworm products ameliorate dextran sodium sulfate-induced colitis in BALB/c mice. Inflamm Bowel Dis. 2011 doi: 10.1002/ibd.21629. [DOI] [PubMed] [Google Scholar]
- 44.Ruyssers NE, De Winter BY, De Man JG, Loukas A, Pearson MS, Weinstock JV, Van den Bossche RM, et al. Therapeutic potential of helminth soluble proteins in TNBS-induced colitis in mice. Inflamm Bowel Dis. 2009;15:491–500. doi: 10.1002/ibd.20787. [DOI] [PubMed] [Google Scholar]
- 45.Johnston MJG, Wang A, Catarino MED, Ball L, Phan VC, MacDonald JA, McKay DM. Extracts of the rat tapeworm, Hymenolepis diminuta, suppress macrophage activation in vitro and alleviate chemically induced colitis in mice. Infect Immun. 2010;78:1364–1375. doi: 10.1128/IAI.01349-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Motomura Y, Wang H, Deng Y, El-Sharkawy RT, Verdu EF, Khan WI. Helminth antigen-based strategy to ameliorate inflammation in an experimental model of colitis. Clin Exp Immunol. 2009;155:88–95. doi: 10.1111/j.1365-2249.2008.03805.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Itami DM, Oshiro TM, Araujo CA, Perini A, Martins MA, Macedo MS, Macedo-Soares MF. Modulation of murine experimental asthma by Ascaris suum components. Clin Exp Allergy. 2005;35:873–879. doi: 10.1111/j.1365-2222.2005.02268.x. [DOI] [PubMed] [Google Scholar]
- 48.McConchie BW, Norris HH, Bundoc VG, Trivedi S, Boesen A, Urban JF, Jr, Keane-Myers AM. Ascaris suum-derived products suppress mucosal allergic inflammation in an IL-10 independent manner via interference with dendritic cell function. Infect Immun. 2006 doi: 10.1128/IAI.00720-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trujillo-Vargas CM, Werner-Klein M, Wohlleben G, Polte T, Hansen G, Ehlers S, Erb KJ. Helminth derived products inhibit the development of allergic responses in mice. Am J Respir Cell Mol Biol. 2007;175:336–344. doi: 10.1164/rccm.200601-054OC. [DOI] [PubMed] [Google Scholar]
- 50.Hewitson JP, Grainger JR, Maizels RM. Helminth immunoregulation: the role of parasite secreted proteins in modulating host immunity. Mol Biochem Parasitol. 2009;167:1–11. doi: 10.1016/j.molbiopara.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hewitson JP, Harcus Y, Murray J, van Agtmaal M, Filbey KJ, Grainger JR, Bridgett S, et al. Proteomic analysis of secretory products from the model gastrointestinal nematode Heligmosomoides polygyrus reveals dominance of Venom Allergen-Like (VAL) proteins. J Proteomics. 2011;74:1573–1594. doi: 10.1016/j.jprot.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hewitson JP, Filbey KJ, Grainger JR, Dowle AA, Pearson M, Murray J, Harcus Y, Maizels RM. Heligmosomoides polygyrus elicits a dominant nonprotective antibody response directed at restricted glycan and peptide epitopes. J Immunol. 2011;187:4764–4777. doi: 10.4049/jimmunol.1004140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Segura M, Su Z, Piccirillo C, Stevenson MM. Impairment of dendritic cell function by excretory-secretory products: A potential mechanism for nematode-induced immunosuppression. Eur J Immunol. 2007;37:1887–1904. doi: 10.1002/eji.200636553. [DOI] [PubMed] [Google Scholar]
- 54.Grainger JR, Smith KA, Hewitson JP, McSorley HJ, Harcus Y, Filbey KJ, Finney CAM, et al. Helminth secretions induce de novo T cell Foxp3 expression and regulatory function through the TGF-β pathway. J Exp Med. 2010;207:2331–2341. doi: 10.1084/jem.20101074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McSorley HJ, Grainger JR, Harcus YM, Murray J, Nisbet A, Knox DP, Maizels RM. daf-7-related TGF-β homologues from trichostrongyloid nematodes show contrasting life cycle expression patterns. Parasitology. 2010;137:159–171. doi: 10.1017/S0031182009990321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hansen G, McIntire JJ, Yeung VP, Berry G, Thorbecke GJ, Chen L, DeKruyff RH, Umetsu DT. CD4+ T helper cells engineered to produce latent TGF-b1 reverse allergen-induced airway hyperreactivity and inflammation. J Clin Invest. 2000;105:61–70. doi: 10.1172/JCI7589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kreider T, Anthony RM, Urban JF, Jr, Gause WC. Alternatively activated macrophages in helminth infections. Curr Opin Immunol. 2007;19:448–453. doi: 10.1016/j.coi.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Loke P, Gallagher I, Nair MG, Zang X, Brombacher F, Mohrs M, Allison JP, Allen JE. Alternative activation is an innate response to injury that requires CD4+ T cells to be sustained during chronic infection. J Immunol. 2007;179:3926–3936. doi: 10.4049/jimmunol.179.6.3926. [DOI] [PubMed] [Google Scholar]
- 59.Byers DE, Holtzman MJ. Alternatively activated macrophages as cause or effect in airway disease. Am J Respir Cell Mol Biol. 2010;43:1–4. doi: 10.1165/rcmb.2009-0407ED. [DOI] [PubMed] [Google Scholar]
- 60.Melgert BN, Oriss TB, Qi Z, Dixon-McCarthy B, Geerlings M, Hylkema MN, Ray A. Macrophages: regulators of sex differences in asthma? Am J Respir Cell Mol Biol. 2010;42:595–603. doi: 10.1165/rcmb.2009-0016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Munitz A, Cole ET, Atar-Karo D, Finkelman FD, Rothenberg ME. Resistin-like molecule alpha regulates IL-13-induced chemokine production but not allergen-induced airway responses. Am J Respir Cell Mol Biol. 2012 doi: 10.1165/rcmb.2011-0391OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Voehringer D, Shinkai K, Locksley RM. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity. 2004;20:267–277. doi: 10.1016/s1074-7613(04)00026-3. [DOI] [PubMed] [Google Scholar]
- 63.Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347:911–920. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 64.Schaub B, Lauener R, von Mutius E. The many faces of the hygiene hypothesis. J Allergy Clin Immunol. 2006;117:969–977. doi: 10.1016/j.jaci.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 65.Maizels RM, Pearce EJ, Artis D, Yazdanbakhsh M, Wynn TA. Regulation of pathogenesis and immunity in helminth infections. J Exp Med. 2009;206:2059–2066. doi: 10.1084/jem.20091903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hamelmann E, Gelfand EW. IL-5-induced airway eosinophilia--the key to asthma? Immunol Rev. 2001;179:182–191. doi: 10.1034/j.1600-065x.2001.790118.x. [DOI] [PubMed] [Google Scholar]
- 67.Lee JJ, Dimina D, Macias MP, Ochkur SI, McGarry MP, O'Neill KR, Protheroe C, et al. Defining a link with asthma in mice congenitally deficient in eosinophils. Science. 2004;305:1773–1776. doi: 10.1126/science.1099472. [DOI] [PubMed] [Google Scholar]
- 68.Allen JE, MacDonald AS. Profound suppression of cellular proliferation mediated by the secretions of nematodes. Parasite Immunol. 1998;20:241–247. doi: 10.1046/j.1365-3024.1998.00151.x. [DOI] [PubMed] [Google Scholar]
- 69.Wu D, Molofsky AB, Liang HE, Ricardo-Gonzalez RR, Jouihan HA, Bando JK, Chawla A, Locksley RM. Eosinophils sustain alternatively activated macrophages in adipose tissue. Science. 2011;332:243–247. doi: 10.1126/science.1201475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sutherland TE, Andersen OA, Betou M, Eggleston IM, Maizels RM, van Aalten D, Allen JE. Analyzing airway inflammation with chemical biology: dissection of acidic mammalian chitinase function with a selective drug-like inhibitor. Chem Biol. 2011;18:569–579. doi: 10.1016/j.chembiol.2011.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Herbert DR, Yang J-Q, Hogan SP, Groschwitz K, Khodoun MV, Munitz A, Orekov T, et al. Intestinal epithelial cell secretion of RELM-β protects against gastrointestinal worm infection. J Exp Med. 2009;206:2947–2957. doi: 10.1084/jem.20091268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mishra A, Wang M, Schlotman J, Nikolaidis NM, DeBrosse CW, Karow ML, Rothenberg ME. Resistin-like molecule-β is an allergen-induced cytokine with inflammatory and remodeling activity in the murine lung. Am J Physiol Lung Cell Mol Physiol. 2007;293:L305–313. doi: 10.1152/ajplung.00147.2007. [DOI] [PubMed] [Google Scholar]
- 73.Borkow G, Bentwich Z. Chronic parasite infections cause immune changes that could affect successful vaccination. Trends Parasitol. 2008;24:243–245. doi: 10.1016/j.pt.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 74.Balic A, Smith KA, Harcus Y, Maizels RM. Dynamics of CD11c+ dendritic cell subsets in lymph nodes draining the site of intestinal nematode infection. Immunol Lett. 2009;127:68–75. doi: 10.1016/j.imlet.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li Z, Liu G, Chen Y, Liu Y, Liu B, Su Z. The phenotype and function of naturally existing regulatory dendritic cells in nematode-infected mice. Int J Parasitol. 2011;41:1129–1137. doi: 10.1016/j.ijpara.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 76.Smith KA, Hochweller K, Hämmerling GJ, Boon L, Macdonald AS, Maizels RM. Chronic helminth infection mediates tolerance in vivo through dominance of CD11clo CD103– DC population. J Immunol. 2011;186:7098–7109. doi: 10.4049/jimmunol.1003636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Finney CAM, Taylor MD, Wilson MS, Maizels RM. Expansion and activation of CD4+CD25+ regulatory T cells in Heligmosomoides polygyrus infection. Eur J Immunol. 2007;37:1874–1886. doi: 10.1002/eji.200636751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rausch S, Huehn J, Kirchhoff D, Rzepecka J, Schnoeller C, Pillai S, Loddenkemper C, et al. Functional analysis of effector and regulatory T cells in a parasitic nematode infection. Infect Immun. 2008;76:1908–1919. doi: 10.1128/IAI.01233-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Camberis M, Le Gros G, Urban J., Jr . Animal model of Nippostrongylus brasiliensis and Heligmosomoides polygyrus. In: Coico R, editor. Current Protocols in Immunology. John Wiley and Sons, Inc; 2003. pp. 19.12.11–19.12.27. [DOI] [PubMed] [Google Scholar]
- 80.Harcus Y, Nicoll G, Murray J, Filbey K, Gomez-Escobar N, Maizels RM. C-type lectins from the nematode parasites Heligmosomoides polygyrus and Nippostrongylus brasiliensis. Parasitol Int. 2009;58:461–470. doi: 10.1016/j.parint.2009.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]