Abstract
Patient: Male, 20
Final Diagnosis: Dermographism
Symptoms: Unusual skin reaction to trauma
Medication: —
Clinical Procedure: —
Specialty: Dentistry
Objective:
Unusual clinical course
Background:
Dermographism is a type of physical urticaria that can be induced by writing on the skin. It occurs in 2–5% of the population and is considered to be a normal physiological phenomenon. However, in a small subset of patients, it can be symptomatic and may affect the quality of life. The etiology of this disease remains unclear.
Case Report:
Herein, we present a case of dermographism in a 20-year-old male and discuss the involvement of the oral mucosa in this condition.
Conclusions:
Although this condition is well known to occur in the skin, we believe this condition is rarely discussed among dentists. All healthcare providers, especially dentists, should know its potential to cause complications during dental procedures.
MeSH Keywords: Allergy and Immunology, Oral Manifestations, Skin Abnormalities
Background
Dermographism (or dermatographism) is a type of physical urticaria that can be induced by writing on the skin [1]. Firm pen strokes on the skin can initiate this condition. The condition is composed of multiple stages, beginning with red lines, followed by broadening of the erythema and linear wheal formation that subsequently fades within ∼45 min [2]. It occurs in 2–5% of the population in both children and adults. There is a slight female predominance in children and it can appear anywhere on the skin, but it is least reported on the scalp and genitalia [3–5].
Dermographism can be symptomatic in a small subset of patients, and it may affect their quality of life. It is usually diagnosed based on a patient history and can be confirmed using a dermographometer (a spring-loaded stylus) to apply graded, defined amounts of pressure on the skin (e.g., 3600 g/cm2) [1,3,5]. Biopsy specimens only show dermal edema with a few perivascular mononuclear cells [5].
Patients with dermographism are generally healthy, but several recent studies reported it to occur in thyroid diseases, infections, diabetes mellitus, scabies, psychological problems, and during menopause [2,5]. It can also develop after the use of drugs such as penicillin, cephalosporin, famotidine, and atorvastatin [5,6].
In the literature, few details are available about oral mucosal symptoms and/or complications that can be associated with dermographism.
Case Report
A 20-year-old Middle-Eastern male dental student reported an unusual skin reaction to trauma. He does not smoke tobacco, drink alcohol, or use any illegal substances. He began experiencing these symptoms when he was 11 years old. He had noticed that every time he fell down and experienced any trauma, a well-defined area of his skin became elevated. As he progressed through middle and high school, he discovered that when he wrote on his skin, the area became elevated along the line of writing. Additionally, confined swelling appeared on his skin when he wore a watch or a ring. None of these symptoms were painful and he experienced no associated subjective symptoms except for the heat that he sensed at the location. When the trauma occurred, it would take 5 min for the skin manifestation to appear and 45 min to 1 h for it to go away. He is healthy with no medical problems and is not taking any medications. He has no known allergies. Regarding his family history, his father had hypertension, hypercholesterolemia, and diabetes mellitus, but there was no family history of any similar skin condition. His hematological parameters were within normal limits.
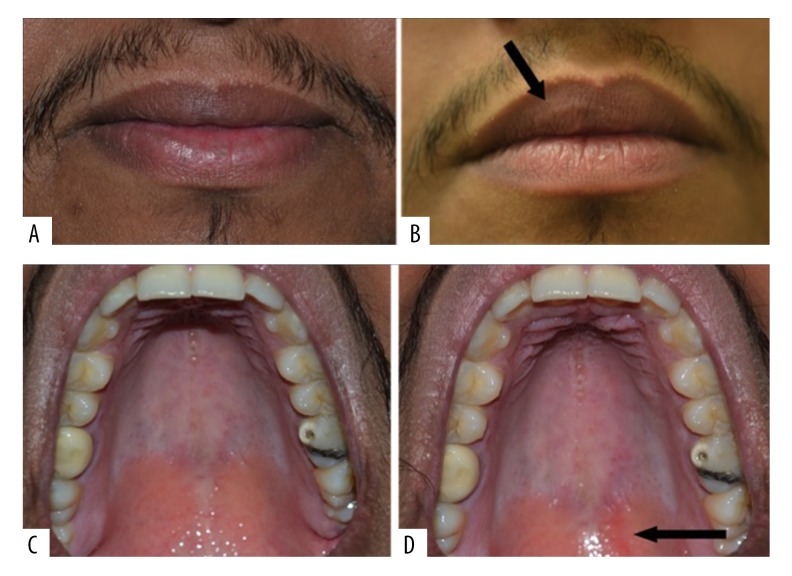
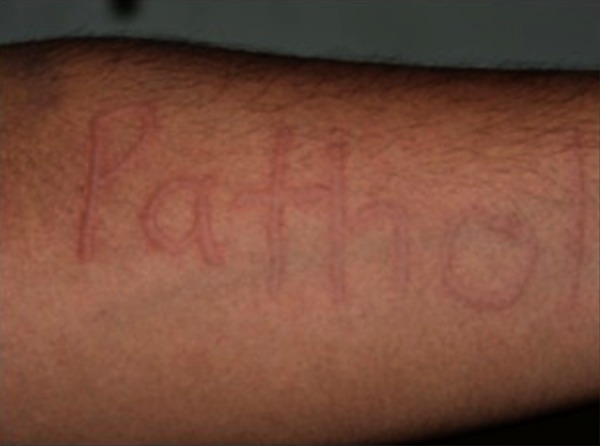
With patient consent, we induced urticaria in the clinic (Figure 1) by writing “oral path” on his flexural arm surface using a dull pen. After 2 min, the wheal began to appear on his arm and it remained visible, although faint, 1 h later. We were interested to learn if the same manifestation could occur in the mouth, especially as the patient reported feelings of fullness and heat in his mouth after eating popcorn or food with sharp edges. We induced it on the vermillion of his lip (Figure 2A, 2B) and intraorally (Figure 2C, 2D). He sensed heat in both locations. There was some evidence of linear swelling on the vermillion boarder of his lip and slight linear redness was observed in his palate.
Figure 1.
Dermographism (skin writing), a writing-induced patholgy, appeared as erythemtous wheals in the flexture of the arm after 2 min of provocation with the blunt end of a pen.
Figure 2.
Oral manifestations of dermographism on the (A) lip before applying pressure, (B) upper lip after 2 min of applying pressure, and (C) normal palatal mucosa. The patient exhibited (D) slight redness along the line of pressure.
The patient showed dermographism “dermatographic urticaria” in his mouth. No treatments were provided. The condition has not affected his quality of life in any way and no clinical changes were detected at a 1-year follow-up.
Discussion
Dermographism, simple dermographism, dermatographic urticaria, pressure dermographism, and urticarial factitia are synonymous for a chronic physical urticaria in which a skin wheal occurs at a site of trauma [7]. Delayed dermographism is a subgroup of dermographism. Other types of physical urticaria are classified according to the cause, duration, and frequency of symptoms [5,8,9].
Although Lewis initially described dermographism in 1924 as vascular reaction to stroking, its full clinical features and symptoms, possible triggers, and complications, as well as the involvement of the oral mucosa, are rarely described [10]. The mechanism underlying this condition remains unclear. It has been suggested that IgE plays a role in this reaction by inducing the release of histamine and other inflammatory mediators from mast cells, such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), which results in vasodilatation, swelling, inflammatory cells infiltrate, and redness [2,7]. In 2013, Ralph reported evidence of the possible involvement of a neural mechanism through release of peptide mediators that are able to cause vasodilation at a site of pressure [11].
The lesions of dermographism appear as erythematous wheals after 2 min of trauma or pressure on skin, which then disappear within 1 h, while in the oral cavity minute edema occurred only at the site to which pressure has been applied. This condition can be accompanied by thyroid disease (hypothyroidism or hyperthyroidism), psychological problems, allergic disease, diabetes mellitus, inflammatory disorders (e.g., adult-onset Still’s disease), and drug reactions [3,5,11,12].
In our case, the disease was first noticed when he was a child. His clinical features were typical for simple dermographism according to his history and provocation tests. Because it was a simple form of dermographism and the patient had not reported any stress-induced lesions, associated systemic conditions, or angioedema, his prognosis was good and his disease is not expected to affect his quality of life. A dentist should be aware of this condition in a patient to avoid the development of complications during or after comprehensive dental procedures, like sever soft-tissue edema of the tongue, lips, or palate from exerted pressure, which may lead to breathing difficulties and suffocation. In the literature, only 1 case of simple dermographism has been reported with sudden swelling of the upper and lower lips after routine dental treatment, which disappeared after 2 h without further complications. That patient had reported a history of previous swelling in response to localized pressure on the face and back [12]. In our present case, the patient had not previously experienced problems during his dental treatment, which included restoration and extractions. However, he did report experiencing a feeling of fullness and heat that lingered for a few minutes after eating “sharp-edged” food. Furthermore, the provocation test that we performed on his lip showed a slight elevation. For patients with these conditions, we recommend performing a detailed medical history, allergic reactions tests, and clinical provocation tests to confirm the diagnosis and severity of the condition in order to avoid unexpected swelling or complications. Jauhar et al. suggested a different approach for the dental management of severe delayed dermographism, which included restorative, prosthodontic, and surgical procedures [12]. They recommend a preventive approach for these patients along with simple, non-aggressive procedures, and a minimum application of pressure. Dermographism should be included in the differential diagnosis of facial or oral swelling with angioedema (acquired or hereditary).
Conclusions
This condition is rarely discussed among dentists despite being commonality and its potential to cause complications of breathing, suffocation, or even death due to edema during or after dental procedures, because dermographism can present in oral cavity.
Abbreviations:
- NGF
nerve growth factor;
- BDNF
brain-derived neurotrophic factor
Footnotes
Competing interests
The authors confirm they have no conflicts of interest regarding this article.
References:
- 1.Abajian M, Młynek A, Maurer M. Physical urticaria. Curr Allergy Asthma Rep. 2012;12:281–87. doi: 10.1007/s11882-012-0269-0. [DOI] [PubMed] [Google Scholar]
- 2.Wong RC, Fairley JA, Ellis JA, Arbor A. Clinical review dermographism: A review. J Am Acad Dermatology. 1984;11:1076–81. doi: 10.1016/s0190-9622(84)70222-2. [DOI] [PubMed] [Google Scholar]
- 3.Schoepke N, Młynek A, Weller K, et al. Symptomatic dermographism: An inadequately described disease. J Eur Acad Dermatology Venereol. 2015;29:708–12. doi: 10.1111/jdv.12661. [DOI] [PubMed] [Google Scholar]
- 4.Mlynek A, Vieira dos Santos R, Ardelean E, et al. A novel, simple, validated and reproducible instrument for assessing provocation threshold levels in patients with symptomatic dermographism. Clin Exp Dermatol. 2013;38:360–66. doi: 10.1111/ced.12107. [DOI] [PubMed] [Google Scholar]
- 5.Taşkapan O, Harmanyeri Y. Evaluation of patients with symptomatic dermographism. J Eur Acad Dermatol Venereol. 2006;20:58–62. doi: 10.1111/j.1468-3083.2005.01372.x. [DOI] [PubMed] [Google Scholar]
- 6.Adcock BB, Hornsby LB, Jenkins K. Dermographism: an adverse effect of atorvastatin. J Am Board Fam Pract. 2001;14:148–51. [PubMed] [Google Scholar]
- 7.Abajian M, Schoepke N, Altrichter S, et al. Physical urticarias and cholinergic urticaria. Immunol Allergy Clin North Am. 2014;34:73–88. doi: 10.1016/j.iac.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Zuberbier T, Asero R, Bindslev-Jensen C, et al. EAACI/GA2LEN/EDF/WAO guideline: Definition, classification and diagnosis of urticaria. Allergy Eur J Allergy Clin Immunol. 2009;64:1417–26. doi: 10.1111/j.1398-9995.2009.02179.x. [DOI] [PubMed] [Google Scholar]
- 9.Kontou-Fili K, Borici-Mazi R, Kapp A, et al. Physical urticaria: Classification and diagnostic guidelines. An EAACI position paper. Allergy. 1997;52:504–13. doi: 10.1111/j.1398-9995.1997.tb02593.x. [DOI] [PubMed] [Google Scholar]
- 10.Lewis T. Vascular reactions of the skin to injury. I. Reaction to stroking; Urticaria factitia. Heart. 1924;11:119–39. [Google Scholar]
- 11.Ralph JW. Evidence for a role of neural pathways in dermographism. Br J Dermatol. 2013;169:1362–63. doi: 10.1111/bjd.12506. [DOI] [PubMed] [Google Scholar]
- 12.Jauhar S, Staines K, McQueen M, et al. Dermographism and delayed pressure urticaria. Oral Surgery Oral Med Oral Pathol Oral Radiol Endodontology. 2007;103:774–79. doi: 10.1016/j.tripleo.2006.11.052. [DOI] [PubMed] [Google Scholar]