Abstract
Diaphragmatic hernia is usually congenital. However, it is rarely traumatic and can stay asymptomatic. In this report, we aimed to present the anaesthetic management of a patient with diaphragmatic hernia due to previous trauma (14 years ago), which was diagnosed incidentally during surgery for rectal cancer. The patient (53 years, 56 kg, 165 cm, American Society of Anaesthesiologist (ASA) II), to whom laparoscopic surgery was planned because of rectal cancer, had a history of falling from a height 14 years ago. Preoperatively, the patient did not have any sign except small right diaphragmatic elevation on the chest x-ray. After induction, maintenance of anaesthesia was continued with sevoflurane and O2/N2O. The patient was given a 30° Trendelenburg position. When the trochars were inserted by the surgeon, the diaphragmatic hernia was seen on the right part of the diaphragm, which was hidden by the liver. The surgery was continued laparoscopically but with low pressure (12 mmHg), because the patient did not have any haemodynamic and respiratory instability. The patient, who had stable haemodynamic parameters and no respiratory complications during the operation, was transferred to the ward for monitorised care. Traumatic diaphragmatic hernias can be detected incidentally after a long period of acute event. In our case, it was diagnosed during laparoscopic surgery. The surgery was completed with appropriate and careful haemodynamic monitoring and low intra-abdominal pressure under inhalational anaesthesia without any impairment in the patient’s haemodynamic and respiratory parameters.
Keywords: Traumatic diaphragmatic hernia, anaesthesia, general, oxygen, nitrous oxide
Introduction
Diaphragm is the most important respiratory muscle (1). Diaphragmatic hernias, which occur because of a defect on the diaphragm, may be congenital or acquired. Traumatic diaphragm hernias, which are in the acquired group, are detected in 0.8%–1.6% of obtuse trauma events (2). They are generally detected during the period of hospital stay at the early stage following the trauma. However, at the post-traumatic stage, they may be concealed because of different organ injuries or lack of clinical and screening findings. After the discharge, the patients may continue their normal life without any problem, and the trauma that causes the diaphragmatic hernia may be forgotten. (3). There are incidents in literature that are detected by coincidence 20 years after the trauma, although they are rare (4).
In this case presentation, we aimed to share the anaesthesia method of a patient that has a history of falling from a height 14 years ago and whose diaphragmatic hernia is detected by coincidence during the laparoscopic rectal surgery.
Case Presentation
The routine laboratory values and electrocardiography (ECG) were normal in the pre-operative anaesthesia evaluation of a male patient who was 53-years-old, 56 kg, 165 cm, American Society of Anaesthesiologist (ASA) II and who planned to undergo “low anterior resection and loop ileostomy” because of rectal cancer diagnosis. Right lung sounds were decreased because of auscultation, and the right diaphragm was elevated in the chest X-ray. At the pulmonology consultation, rale (+) at the right chest lower zones was detected, and FVC was 66%, FEV1 was 67% and MEF was 65% in the pulmonary function test (PFT). Chronic obstructive pulmonary disease (COPD) and acute bronchitis were diagnosed. In treatment, Cefuroxime Sodium (Multisef ) 750 mg iv, Salbutamol (Ventolin) inhaler neb 4 × 1, Fluticasone Propionate (Flixotide) 2 × 1 and Acetyl cysteine (Asist) amp 2 × 1 iv were administered and control examination after a week was suggested. It was stated that the patient’s auscultation findings were recovered at the second pulmonary consultation and PFT values were as follows: FVC, 88%; FEV1, 85% and MEF, 76%. Thus, the patient could be operated and continuance of preoperative bronchodilator treatment was recommended.
After the surgery decision was made and the written informed consent was obtained from the patient, he was taken to the operating room and routine monitorization, arterial blood pressure (ABP), electrocardiography, peripheral oxygen saturation (SpO2), end tidal carbon dioxide (ETCO2,) and bispectral analysis (BIS) were conducted (Drager Infinity Delta, Telford, PA, USA). By performing intravenous cannulation on the left hand of the patient, 4 mL kg−1 h−1 of 0.9% sodium chloride infusion was started. In anaesthesia induction, by doing thiopental sodium 480 mg, rocuronium bromide 0.6 mg kg−1, morphine HCl 3 mg after iv 2 mg midazolam, orotracheal intubation was performed. Sevoflurane 1.0% and O2-N2O 50%-50% were started for maintenance. Volume control ventilation (VCV) was applied with an anaesthesia device (Drager Fabius Plus, Telford, PA, USA), with the following parameters of tidal volume: 7 mL kg−1 and frequency: 10 min−1. The upper limit of the alveolar pressure was set as 35 cmH2O. Remifentanil (UltivaTM inj 1 mg vial, GlaxoSmith-Kline, Belgium) infusion (0.05 μg kg−1 min−1) was administered to the patient with an infusion pump (Body Guard 323 Multi Therapy Ambulatory Infusion Pump, B. Braun, Melsungen, Germany). Considering that the duration of the operation would be long, left radial artery cannulation (20 G arterial catheter-Bio-flon, Hayrana, India) and left brachial vein catheterization (Cavafix Certo 375 B.Braun, Melsungen, Germany) for invasive arterial pressure were performed, and central venous pressure (CVP) was monitored to observe the haemodynamic parameters carefully.
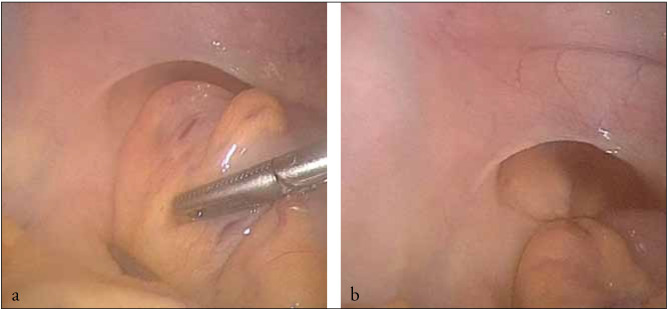
The patient was subsequently taken to the position of 30° Trendelenburg. After placement of trocars by the surgical team and administration of intra-abdominal CO2 insufflation with 14 mmHg, inspection was started. A large hernia that covered the right half of the diaphragm and the half portion of the liver was observed (Fig. 1a, b). In this period, the patient’s ABP was 104/67 mmHg, heart rate (HR) was 73 beat min−1, SpO2 was 100%, ETCO2 was 25 mmHg and hemodynamic parameters were stable. After the consultation with the surgical team, it was decided that operation would be continued as a laparoscopic surgery with low pressure (12 mmHg) because the patient did not have any haemodynamic and respiratory disorders. Considering the long duration of the present operation and the general situation of the patient (malignancy), it was decided not to interfere in the diaphragmatic hernia.
Figure 1.
a, b. Intraoperative image of diaphragmatic hernia
The haemodynamic follow-ups of the patient afterwards were observed between the following values: ABP: 120-97/87-62 mmHg, HR: 64–68 beats min−1, SpO2: 99%–100%, ETCO2: 28–32 mmHg and BIS: 39–43. Arterial blood gas (ABG) values, respiration parameters and CVP were monitored punctiliously. At the seventh hour, the patient’s Trendelenburg position was straightened and he was placed in the supine position and was subsequently administered 4500 mL crystalloid and 1000 mL colloid fluid in total. Total urine was 1000 mL and haemorrhage was 70 mL. Before Trendelenburg, CVP was measured as 12 cmH2O and after Trendelenburg it was 17–19 cmH2O. Thirty minutes before the anaesthesia was terminated, pain treatment was performed with Tramadole HCl (Contramal, Abdi İbrahim, İstanbul) 100 mg iv and Tenoxicam (Oksamen, Mustafa Nevzat, İstanbul) vial iv. The patient who was extubated after the operation was followed by a 2-h monitorization in the recovery room (ABP: 150/86 mmHg, HR: 81 beats min−1 SPO2: 97%). In addition, paracetamol (perfalgan, Bristol Myers Squibb, New York, USA) vial 1 g iv was administered for the pain treatment. Salbutamol inhaler was applied. The patient was sent from the recovery room with the values of ABP: 145/80 mmHg, HR: 78 beats min−1 and SPO2: 96% (at room air) to the general surgery ward for monitorization.
On postoperative day 1, surgical examination showed that the general status of the patient was good; his haemodynamic parameters were within normal limits and stable and he had no pain. The ABP values taken at the room condition were pH: 7.37, PO2: 69.3 mmHg, PCO2: 38.3 mmHg, SO2: 95.2, K: 3.2 mmol/L, Na: 134 mmol/L, Ca: 4.05 mmol/L, Cl: 115 mmol/L, glucose: 179 mmol/L, HCO3: 22.4 mmol/L, Lac: 17 mmol/L and base excess (BE): −2.3 mmol/L. Liver and kidney function test results were within normal limits. The patient was discharged from hospital on postoperative day 5 without any problem.
Discussion
Diaphragm is the largest respiratory muscle that separates the thorax and abdominal cavity. Diaphragmatic hernias are separated into two types: congenital and acquired. While congenital diaphragmatic hernias are due to a defect that progresses at the embryologic period, acquired defects, which are rarely seen, occur because of a trauma in the ratio of 74% (5). Among the trauma related ones, although right hemidiaphragmatic injuries are rarer than left hemidiaphragmatic injuries, they constitute 35% of all diaphragmatic traumas (6). It is stated that the liver forms a barrier and retards the diagnosis in this type of injuries (7). Therefore, diaphragmatic injuries are detected at a later stage for patients with a history of fall, and the diagnosis is made by coincidence at the rate of 41.3% during laparotomy, thoracotomy or autopsy (8). In addition, in our case, traumatic diaphragmatic hernia stayed asymptomatic for 14 years and it was detected during laparoscopy by coincidence.
Non-specific symptoms such as dyspnoea, tachypnea, cough, chest or abdominal pain may be seen in traumatic diaphragmatic hernias (1). If there is no other pathology that requires emergency surgery in the patient, surgical repair of diaphragm rupture can be performed later (9). In addition, in our case, no symptoms that can be related to diaphragmatic hernia were detected until he underwent rectal operation. Moreover, because rectal operation duration was long and the patient would be operated again for ileostomy closing, it was decided not to perform the repair of diaphragmatic hernia during the first operation.
Laparoscopic surgery is used in increasing rates for the operations that once required open surgery (10). Meanwhile, the patients can be taken to a deep Trendelenburg position (>30°) and pneumoperitoneum can be performed. At the situations where intra-abdominal pressure is above the 12 mmHg pressure level with pneumoperitoneum, it has been stated that chest compliance decreases and maximal inspiratory pressure increases. It is stated that this change observed in respiratory parameters is related to pneumoperitoneum rather than the degree of Trendelenburg position (11). In a study in which three groups were compared as young (<45 years), middle aged (45–64 years) and old (>64 years), a significant difference was found in PaO2 and PaCO2 values in pneumoperitoneum and the deep Trendelenburg position between the young and old groups. It was measured that PaO2 values in the young age group were higher than the elderly group and PaCO2 values were lower. It was stated that the age related emphysematous changes in lungs caused this situation. In the study in which the maximal pressure limit was 35 cmH2O and ETCO2 value was between 4–4.67 kPa for airway, it was stated that mechanic ventilation parameters must be set carefully with respect to the ETCO2 values during the operation (12). In our case, the alveolar maximal pressure limit for mechanic ventilation was accepted as 35 cmH2O.
In the studies conducted till today, it was stated that the deep Trendelenburg position and carbon dioxide (CO2) insufflation increase HR and mean arterial pressure (MAP) (13). On the contrary to cholecystectomy and hysterectomy, laparoscopic colon surgery requires longer anaesthesia and surgery duration (14). Effects of long-term pneumoperitoneum on cardiovascular system are different from those that are observed in short-term laparoscopic surgeries (15). Some available studies in which intra-abdominal pressure reached the 20 cmH2O level indicate that cardiac output (CO) increases or does not change (16). Falabella et al. (17) detected a slight but insignificant increase in CO in patients who were taken to the 45° deep Trendelenburg position and a slight but inconsiderable decrease in CO at the initiation of Trendelenburg-pneumoperitoneum during the 170-min insufflation period (Supine position CO: 5.3 L min−1, after Trendelenburg CO: 5.9 L min−1, after pneumoperitoneum CO: 4.9 L min−1). In the study of Klopfenstein et al. (18), in patients who had long-term pneumoperitoneum and laparoscopic colon surgery, arterial pH and base deficit were stable and within normal intervals, whereas MAP and HR significantly increased. A correlation that was not consistent and had decreasing reliability as the surgery duration increased was detected between ETCO2 and PaCO2 values. In a study conducted among laparoscopic sigmoidectomy cases, it was indicated that CO2 insufflation and increased intraabdominal pressure caused an increase in plasma lactate level and a decrease in arterial pH in long laparoscopic surgeries. In this study, the duration of pneumoperitoneum was stated as 220–255 min (19). In our case, pneumoperitoneum duration was 420 min, and our patient’s ventilation parameters and haemodynamic and respiratory values were within physiological limits during this period. Furthermore, arterial blood gas values observed during the operation were within the normal limits (Table 1).
Table 1.
ABG and hemodynamic values
| pH | pO2 | pCO2 | SpO2 (%) | HCO3 | HR | ABP | |
|---|---|---|---|---|---|---|---|
| Peroperative 1. Hour | 7.37 | 157 mmHg | 40 mmHg | 99 | 23.5 mmol/L | 73/dk | 104/67 mmHg |
| Peroperative 3. Hour | 7.3 | 152 mmHg | 44 mmHg | 99 | 20.6 mmol/L | 62/dk | 97/62 mmHg |
| Peroperative 7. Hour | 7.33 | 172 mmHg | 40.5 mmHg | 99 | 21 mmol/L | 68/dk | 120/87 mmHg |
| Postoperative 1. day | 7.37 | 69,3 mmHg | 38.3 mmHg | 99 | 22.4 mmol/L | 83/dk | 127/81 mmHg |
ABG: arterial blood gas; HR: heart rate; ABP: arterial blood pressure
Although there are studies suggesting that N2O which is applied in high doses (60%) in laparoscopic surgery creates cardiovascular stimulation, which gradually decreases with long term gas inhalation, there are other studies revealing that a 2–10 h application of 50%–60% N2O does not have a negative effect on the lungs, liver, brain and peripheral nerves (20, 21). Therefore, we also used N2O/O2 in our anaesthesia planning while monitoring haemodynamic and respiratory parameters carefully in the peroperative stage. Throughout the anaesthesia applied for 8 h and 25 min, there was no problem related to the cardiovascular system in our case. Liver and kidney tests which were conducted postoperatively were within normal limits.
Conclusion
In addition to the conditions that are unfavourable for the anaesthesia, such as long operation duration, Trendelenburg position and insufflation, diaphragmatic hernia detected by coincidence may make the anaesthesia management more difficult. We think that in asymptomatic patients intraoperatively diagnosed with diaphragmatic hernia similar to our case, long-time laparoscopic surgical interventions can be successfully performed with close haemodynamic and ABP monitoring, low pressure and proper ventilator settings by using N2O.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Cocept - M.Ö.; Design - M.Ö., P.Y.Y.; Supervision - N.B.; Funding - M.Ö., P.Y.Y.; Materials - M.Ö.; Data Collection and/or Processing - M.Ö.; Analysis and/or Interpretation - M.Ö., P.Y.Y., Ş.G.T.; Literature Review - M.Ö., P.Y.Y.; Writer - M.Ö., P.Y.Y., Ş.G.T.; Critical Review - N.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hwang SW, Kim HY, Byun JH. Management of patients with traumatic rupture of the diaphragm. Korean J Thorac Cardiovasc Surg. 2011;44:348–54. doi: 10.5090/kjtcs.2011.44.5.348. http://dx.doi.org/10.5090/kjtcs.2011.44.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansor KA. Trauma to the diafragm. Chest Surg Clin N Am. 1997;7:373–83. [PubMed] [Google Scholar]
- 3.Carter BN, Giuseffi J, Felson B. Traumatic diaphragmatic hernia. Am J Roentgenol Radium Ther. 1951;65:56–72. [PubMed] [Google Scholar]
- 4.Shreck GL, Toalson TW. Delayed presentation of traumatic rupture of the diaphragm. J Okla State Med Assoc. 2003;96:181–3. [PubMed] [Google Scholar]
- 5.Kuppusamy A, Ramanathan G, Gurusamy J, Ramamoorthy B, Parasakthi K. Delayed diagnosis of traumatic diaphragmatic rupture with herniation of the liver: a case report. Ulusal Travma ve Acil Cerrahi Derg. 2012;18:175–7. doi: 10.5505/tjtes.2012.79477. http://dx.doi.org/10.5505/tjtes.2012.79477. [DOI] [PubMed] [Google Scholar]
- 6.Chunghtai T, Ali S, Sharkey P, Lins M, Rizoli S. Update on managing diaphragmatic rupture in Blunt trauma:a review of 208 consecutive cases. Can J Surg. 2009;52:177–81. [PMC free article] [PubMed] [Google Scholar]
- 7.Boulanger BR, Milzman DP, Rosati C, Rodriguez A. A comparison of right and left blunt traumatic diaphragmatic rupture. J Trauma. 1993;35:255–60. doi: 10.1097/00005373-199308000-00014. http://dx.doi.org/10.1097/00005373-199308000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Dwari AK, Mandal A, Das SK, Sarkar S. Delayed presentation of traumatic diaphragmatic rupture with herniation of the left kidney and bowel loops. Case Rep Pulmonol. 2013;2013:814632. doi: 10.1155/2013/814632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergeron E, Clas D, Ratte S, Beauchamp G, Denis R, Evans D, et al. Impact of deferred treatment of blunt diaphragmatic rupture: a 15-year experience in six trauma centers in Quebec. J Trauma. 2002;52:633–40. doi: 10.1097/00005373-200204000-00004. http://dx.doi.org/10.1097/00005373-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 10.McKernan JB, Laws HL. Laparascopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7:26–8. doi: 10.1007/BF00591232. http://dx.doi.org/10.1007/BF00591232. [DOI] [PubMed] [Google Scholar]
- 11.Rauh R, Hemmerling TM, Rist M, Jacobi KE. Influence of pneumoperitoneum and patient positioning on respiratory system compliance. J Clin Anesth. 2001;13:361–5. doi: 10.1016/s0952-8180(01)00286-0. http://dx.doi.org/10.1016/S0952-8180(01)00286-0. [DOI] [PubMed] [Google Scholar]
- 12.Takahata O, Kunisawa T, Nagashima M, Mamiya K, Sakurai K, Fujita S, et al. Effect of age on pulmonary gas exchange during laparascopy in the Trendelenburg lithotomy position. Acta Anaesthesiol Scand. 2007;51:687–92. doi: 10.1111/j.1399-6576.2007.01311.x. http://dx.doi.org/10.1111/j.1399-6576.2007.01311.x. [DOI] [PubMed] [Google Scholar]
- 13.Hirvonen EA, Nuutinen LS, Kauko M. Hemodynamic changes due to Trendelenburg positioning and pneumoperitoneum during laparascopic hysterectomy. Acta Anaesthesiol Scand. 1995;39:949–55. doi: 10.1111/j.1399-6576.1995.tb04203.x. http://dx.doi.org/10.1111/j.1399-6576.1995.tb04203.x. [DOI] [PubMed] [Google Scholar]
- 14.Darzi A, Hill AD, Henry M, Guillou PJ, Monson JR. Laparacopic assisted surgery of the colon. Operative technique. Endosc Surg Allied Technol. 1993;1:13–5. [PubMed] [Google Scholar]
- 15.Wittgen CM, Andrus CH, Fitzgerald SD, Baudendistel LJ, Dahms TE, Kaminski DL. Analysis of the hemodynamic and ventilatory effects of laparascopic cholecystectomy. Arch Surg. 1991;126:997–1000. doi: 10.1001/archsurg.1991.01410320083011. http://dx.doi.org/10.1001/archsurg.1991.01410320083011. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham AJ. Anesthetic implications of laparascopic surgery. Yale Journal of Biology and Medicine. 1998;71:551–78. [PMC free article] [PubMed] [Google Scholar]
- 17.Falabella A, Moore-Jeffries E, Sullivan MJ, Nelson R, Lew M. Cardiac function during steep Trendelenburg position and CO2 pneumoperitoneum for robotic assisted prostatectomy:a trans-oesophageal Doppler probe study. Int J Med Robotics Comput Assist Surg. 2007;3:312–31. doi: 10.1002/rcs.165. http://dx.doi.org/10.1002/rcs.165. [DOI] [PubMed] [Google Scholar]
- 18.Klopfenstein CE, Schiffer E, Pastor CM, Beaussier M, Francis K, Soravia C, et al. Laparoscopic colon surgery: unreliability of end-tidal CO2 monitoring. Acta Anaesthesiol Scand. 2008;52:700–7. doi: 10.1111/j.1399-6576.2007.01568.x. http://dx.doi.org/10.1111/j.1399-6576.2007.01568.x. [DOI] [PubMed] [Google Scholar]
- 19.Taura P, Lopez A, Lacy AM, Anglada T, Beltran J, Fernandez-Cruz L, et al. Prolonged pneumoperitoneum at 15 mmHg causes lactic asidosis. Srg Endosc. 1998;12:198–201. doi: 10.1007/s004649900633. http://dx.doi.org/10.1007/s004649900633. [DOI] [PubMed] [Google Scholar]
- 20.Kawamura R, Stanley TH, English JB, Hill GE, Liu WS, Webster LR. Cardiovascular responses to nitrous oxide exposure for two hours in man. Anesth Analg. 1980;59:93–9. http://dx.doi.org/10.1213/00000539-198002000-00003. [PubMed] [Google Scholar]
- 21.Lampe G, Wauk LZ, Donegan JH, Pitts LH, Jackler RK, Litt LL. Effect on outcome of prolonged exposure of patients to nitrous oxide. Anesth Analg. 1990;71:586–90. http://dx.doi.org/10.1213/00000539-199012000-00002. [PubMed] [Google Scholar]