Abstract
Objective
To compare the effects of propofol and thiopental on haemodynamics, awareness and newborns in pregnant women undergoing elective caesarean section.
Methods
Seventy pregnant women were assigned into two equal groups. For anaesthesia induction, 2 mg kg−1 propofol (Group P) and 5 mg kg−1 thiopental (Group T) were administered. Maternal haemodynamic parameters and bispectral index (BIS) values were recorded before induction, in 1-minute intervals within the first 10 minutes after induction and in 5-minute intervals thereafter, during skin incision, uterine incision, removal of infant, uterine sutures, skin sutures, eye opening and extubation in all cases. Cord blood gas analysis and 1- and 5-minute APGAR scores were recorded. In all cases, a keyword was spelled to ear during removal of the infant, and at the first postoperative hour, patients were questioned. Important time periods of surgery and anaesthesia and also the first postoperative hour haemodynamic values, pain scores, nausea and vomiting were noted.
Results
The demographic data were similar among cases. In Group T, systolic arterial pressure (SAP), diastolic arterial pressure (DAP) and mean arterial pressure (MAP) at the first 2 minutes after induction and heart rate (HR) at almost all time points were significantly higher. BIS values from induction to the eighth minute and skin incision, uterine incision and removal of the infant were lower in Group P. No patient remembered the keyword spelled, while 4 patients reported dreaming during general anaesthesia. The effects of propofol and thiopental sodium on 1- and 5-minute APGAR scores, cord blood gas values and postoperative visual analogue scale (VAS) scores were similar.
Conclusion
Propofol is a more appropriate anaesthetic agent than thiopental in anaesthesia for caesareans, since it provides better anaesthestic depth and more rapid recovery.
Keywords: Caesarean section, propofol, thiopental sodium, bispectral index, intraoperative awareness
Introduction
Regional techniques in caesarean sections are popular because of their advantages to mothers and newborns. However, the administration of general anaesthesia takes an important place in cases of coagulopathy, infection in the area of regional anaesthesia administration, hypovolemia, severe foetal distress and rejection of regional anaesthesia by the patient (1).
During caesarean sections performed under general anaesthesia, the problem of intraoperative awareness has often occurred in mothers under the effect of neuromuscular blockers as a result of rapid sequence induction application, non-use of opioids and benzodiazepine until delivery and use of low concentration volatile agents for reducing the newborn’s depression to the minimum, and this issue has recently become more important (2). In patients having intraoperative awareness, sleep disorder, dreams and nightmares, anxiety disorders and post-traumatic stress disorder may develop (3, 4). Therefore, the choice of induction agent and administration dose has critical importance in the caesarean sections of patients having a high risk for anaesthetic awareness.
Propofol and thiopental sodium are induction agents frequently used in anaesthetic practices. Although propofol is a frequently used intravenous anaesthetic drug at present, there are some concerns about the possibility of neonatal depression and adequate depth of anaesthesia (2). For both propofol and thiopental, there are no specific data on the most appropriate dose for avoiding anaesthetic awareness.
Awareness during caesarean section was first determined using the isolated forearm technique by Tunstal et al. (5), but later studies revealed that the isolated forearm technique is insufficient for the determination of awareness (6, 7). The use of bispectral index (BIS) monitoring for determining the awareness is new. BIS not only helps the adjustment of drug dose for the most appropriate anaesthetic depth but also decreases the amount of drug used, provides the rapid recovery of patients and prevents awareness during anaesthesia (8, 9).
In this study, it was aimed to investigate the effects of propofol and thiopental sodium, which are used in induction and on haemodynamics, intraoperative awareness, postoperative recovery, and newborns for pregnant women in whom elective caesarean section was planned under general anaesthesia.
Methods
The study was initiated after having obtained ethics committee approval from the ethics committee of Istanbul Umraniye Training and Research Hospital (Study Protocol No: 2012/43) and written informed consents from the patients who participated in this study. The study involved seventy 37–40 weeks pregnant women for whom elective caesarean section was planned under general anaesthesia, who were included in the American Society of Anaesthesiologists (ASA) I–II risk group and who were aged 18 years and above. Patients with known allergy to study drugs, cardiopulmonary disease, liver and kidney failure, preeclampsia or eclampsia, history of alcohol or substance addiction, multiple pregnancies, preterm pregnancies, foetal growth retardation and emergency cases were excluded from the study. It was planned to eliminate the patients with uncontrollable haemodynamic state and severe bleeding.
The patients underwent end-tidal carbon dioxide (etCO2) and BIS (Infinity® BISx® SmartPod®) monitoring in addition to routine monitoring [electrocardiogram, non-invasive blood pressure, peripheral oxygen saturation (SpO2)]. Preoxygenation with 4 L min−1 100% oxygen was applied to all patients for 3 min. The patients were then randomly divided into two groups. For induction, 2 mg kg−1 propofol was administered to the patients in the propofol group (Group P, n=35), 5 mg kg−1 thiopental sodium was given to the patients in the thiopental sodium group (Group T, n=35) and 0.6 mg kg−1 rocuronium was given to all patients. Endotracheal intubation was performed for all patients. The maintenance of anaesthesia was provided with 1.5% sevoflurane in a mixture of 50% O2 and 50% N2O. Immediately after the birth of the baby, an infusion was administered in 15 units of oxytocin crystalloid and 10 units of oxytocin iv bolus with 1 μg kg−1 of fentanyl.
The administration of iv fluid loading for hypotension [mean arterial pressure (MAP)<50 mm Hg], 5 μg ephedrine iv in case of no response and 0.5 mg atropine iv for bradycardia [heart rate (HR)<50 beats min−1] were planned for all patients. Moreover, additional administration of 0.5 mg kg−1 fentanyl was planned for the possibility of an increase in the basal value of MAP by 20% or more.
All patients were applied with 1 mg kg−1 tramadole hydrochloride and 20 mg tenoxicam iv while suturing the uterus to provide postoperative analgesia. Anaesthetic agents were discontinued when the skin was sutured. In all patients, systolic arterial pressure (SAP), diastolic arterial pressure (DAP), MAP, HR, SpO2, etCO2 and BIS values were recorded before incision, after incision (every minute for 10 min and then every 5 min) and during skin incision, uterus incision, birth of baby, uterus suture, skin suture, eye opening and extubation. Following the delivery, a vein blood sample was taken from the cord blood in all patients, and blood gas analysis was performed. The examination of the newborn was conducted by a paediatrician, and Apgar scores were recorded at the 1st and 5th minutes.
During the birth of the baby, a key word was whispered into the ears of all patients, and they were asked whether they remembered this word at the 1st hour postoperatively. The time from the discontinuance of anaesthetic agents to extubation (extubation time), from anaesthesia induction to delivery (delivery time), from uterus incision to delivery (time of the birth of the baby), from discontinuance of anaesthetic agents to the establishment of place–time co-operation (co-operation time), from the initiation of anaesthetic agents to their discontinuance (anaesthesia time), from the duration of operation and discontinuance of anaesthesia to reaching the Aldrete recovery score of 9 (recovery time) were recorded. Furthermore, the doses of additionally administered drugs were also recorded.
The haemodynamic values, pain levels [via visual analogue scale (VAS)], nausea-vomiting state and intraoperative awareness state of the patients were evaluated and recorded at the 1st hour postoperatively.
Statistical analysis
While evaluating the findings of the study, the Number Cruncher Statistical System (NCSS) 2007and Power Analysis and Sample Size (PASS) 2008 Statistical Software (Utah, USA) programs were used for statistical analyses. In addition to descriptive statistical methods (mean, standard deviation, median, frequency and percentage), Student’s t-test was employed in intergroup comparisons of the parameters displaying normal distribution in the evaluation of quantitative data. On the other hand, Mann–Whitney U test was used for intergroup comparisons of parameters not showing normal distribution. Paired-sample test was used for within- group comparisons of parameters displaying normal distribution, and Wilcoxon signed-rank test was employed for within-group comparisons of parameters not displaying normal distribution. Moreover, chi-square test was used for comparing qualitative data. The value of p<0.05 was considered to be significant.
Results
The study was conducted in 70 patients [divided into Group P (propofol, n=35) and Group T (thiopental, n=35)] who were admitted to the Anaesthesiology Clinic of Istanbul Umraniye Training and Research Hospital between 1 February and 30 June, 2012. No patient was excluded from the study.
There was no statistically significant difference between the groups with regard to age, height, weight, body mass index (BMI), gestational week and number of pregnancies (Table 1).
Table 1.
Comparison of demographic features
| Demographic data | Group T (n=35) Mean±SD |
Group P (n=35) Mean±SD |
+p |
|---|---|---|---|
| Age (year) | 28.43±4.48 | 29.20±5.71 | 0.532 |
| Body weight (kg) | 81.23±10.06 | 78.94±11.32 | 0.375 |
| Height (m) | 1.61±0.50 | 1.59±0.40 | 0.063 |
| BMI (kg m−2) | 30.95±3.60 | 30.95±4.11 | 0.998 |
| Gestational week (week) | 38.97±0.28 | 39.09±0.32 | 0.117 |
| ++p | |||
| Number of pregnancies | 2.46±0.89 | 2.63±1.03 | 0.345 |
Group T: thiopental; Group P: propofol; BMI: body mass index; SD: standard deviation;
Student’s t-test;
Mann–Whitney U test. p<0.05
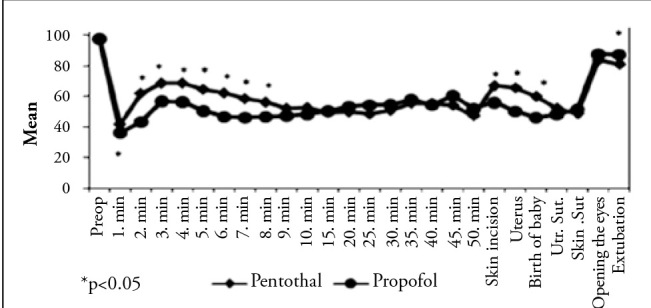
In the comparison of HR values between the groups, it was found that the HR values of Group T were higher than those of Group P before the anaesthesia induction and at the 1st, 2nd, 3rd, 5th, 6th, 7th, 8th, 9th, 10th, 15th, 20th, 25th and 35th minutes after the induction (p<0.05) (Figure 1).
Figure 1.
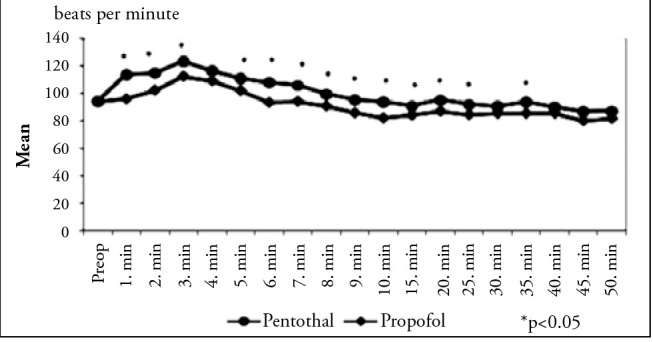
Measurements of heart rates (HR) according to the groups
In within-group comparisons of HRs, considering the preoperative values, a statistically significant increase was observed at the measurements performed within the first 7 minutes (p<0.05) in Group T. On the other hand, in Group P, a statistically significant increase was observed at the 2nd, 3rd, 4th and 5th minutes (p<0.05), and a statistically significant decrease was seen at the 9th, 10th, 15th, 20th, 25th, 30th, 35th and 40th minutes (p<0.05). It was found that the SAP values were significantly higher in Group T than in Group P at the 1st and 2nd minutes after the induction (p<0.05) (Figure 2).
Figure 2.
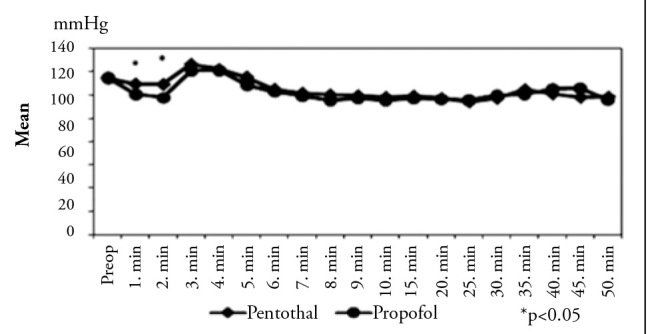
Measurements of systolic arterial pressure (SAP) according to the groups
In within-group comparison of SAP in Group T, a statistically significant increase at the 3rd and 4th minutes after the induction (p<0.05) and also a statistically significant decrease at other measurement times compared with the preoperative values were observed. On the other hand, considering the preoperative values in Group P, a statistically significant decrease was found at almost all measurement times (p<0.05).
The DAP values were higher in Group T than in Group P at the 1st and 2nd minutes after the induction and were higher in Group P than in Group T at the 20th and 25th minutes after the induction (p<0.05). However, the DAP values were similar in both groups at other measurement times (Figure 3).
Figure 3.
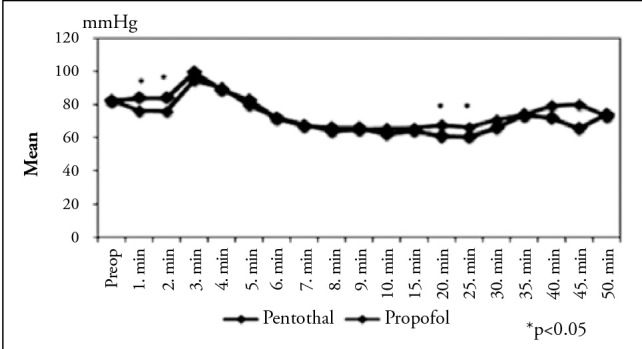
Measurements of diastolic arterial pressure (DAP) according to the groups
In within-group comparisons of DAP, for both groups, a statistically significant increase was observed at the 3rd and 4th minutes after the induction compared with the preoperative values (p<0.05), but a significant decrease was seen at other measurement times (p<0.05).
It was found that MAP was higher in Group T than in Group P at the 1st and 2nd minutes after the induction (p<0.05), which was statistically significant (Figure 4).
Figure 4.
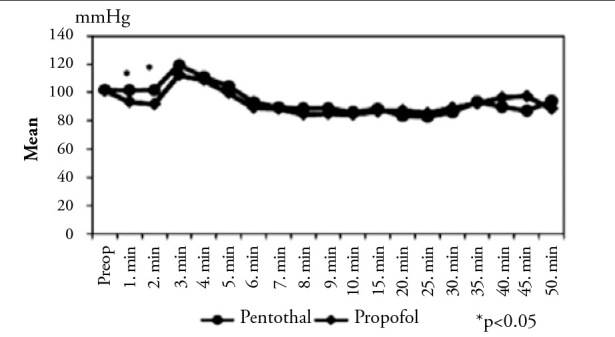
Measurements of mean arterial pressure (MAP) according to the groups
In within-group comparisons of MAP, a statistically significant increase was observed at the 3rd and 4th minutes after the induction compared with the preoperative values in Group T and at the 4th minute in Group P (p<0.05), and a statistically significant decrease was observed at other measurement times for all patients (p<0.05). In both groups, the etCO2 and SpO2 values were similar and in a normal interval.
It was revealed that the BIS values were significantly higher at the first 8 min after the induction and during skin incision, uterus incision and the birth of the baby in Group T and during extubation in Group P (p<0.05) (Table 2) (Figure 5).
Table 2.
BIS values
| BIS | Group T (n=35) Mean±SD |
Group P (n=35) Mean±SD |
p |
|---|---|---|---|
| Preoperative | 97.89±0.32 | 97.83±0.45 | 0.545 |
| 1st minute | 41.80±13.13 | 36.00±9.10 | 0.036* |
| 2nd minute | 62.06±13.65 | 43.26±13.34 | 0.001** |
| 3rd minute | 68.69±8.70 | 56.77±15.36 | 0.001** |
| 4th minute | 68.74±8.13 | 56.26±15.22 | 0.001** |
| 5th minute | 64.63±11.31 | 50.43±15.62 | 0.001** |
| 6th minute | 62.29±12.78 | 46.40±13.98 | 0.001** |
| 7th minute | 58.49±13.56 | 45.89±12.54 | 0.001** |
| 8th minute | 56.26±13.71 | 46.49±13.21 | 0.003** |
| 9th minute | 52.26±13.07 | 47.17±13.15 | 0.109 |
| 10th minute | 52.66±13.23 | 48.14±13.84 | 0.168 |
| 15th minute | 49.66±12.08 | 50.34±13.62 | 0.824 |
| 20th minute | 49.86±12.23 | 53.23±12.48 | 0.258 |
| 25th minute | 48.44±11.82 | 54.26±12.59 | 0.054 |
| 30th minute | 50.97±14.26 | 54.53±16.43 | 0.347 |
| 35th minute | 55.63±13.59 | 57.76±14.42 | 0.563 |
| 40th minute | 55.38±16.43 | 54.44±15.42 | 0.855 |
| 45th minute | 54.27±16.28 | 60.42±21.38 | 0.445 |
| 50th minute | 47.43±14.72 | 51.83±21.34 | 0.680 |
| Skin incision | 67.11±9.17 | 55.94±16.13 | 0.002** |
| Uterus incision | 65.69±9.28 | 50.17±15.99 | 0.001** |
| Birth of baby | 60.09±12.71 | 46.09±14.37 | 0.001** |
| Uterus suture | 52.37±12.48 | 48.03±13.14 | 0.161 |
| Skin suture | 48.80±10.41 | 51.57±12.92 | 0.327 |
| Eye opening | 83.77±8.94 | 87.69±7.63 | 0.053 |
| Extubation | 81.14±8.07 | 87.34±6.16 | 0.002** |
BIS: bispectral index; Group T: thiopental; Group P: propofol; SD: standard deviation; Student’s t-test.
p<0.05;
p<0.01
Figure 5.
Measurements of bispectral index (BIS) according to the groups
No statistically significant difference was found between the groups in terms of delivery time, time of the birth of the baby, extubation time, co-operation time and anaesthesia and operation duration (p>0.05) (Table 3).
Table 3.
Evaluations of times
| Group | Group T (n=35) Mean±SD |
Group P (n=35) Mean±SD |
p |
|---|---|---|---|
| Induction-delivery time | 6.30±1.19 | 6.26±1.05 | 0.909 |
| Uterine incision-delivery time | 0.88±0.25 | 0.82±0.19 | 0.226 |
| Extubation time | 6.70±1.57 | 6.58±2.94 | 0.827 |
| Co-operation time | 7.86±1.90 | 7.22±2.74 | 0.258 |
| Operation duration | 35.83±8.59 | 37.39±10.09 | 0.488 |
| Anaesthesia duration | 35.78±9.25 | 34.89±8.89 | 0.681 |
Student’s t-test; p<0.05. Group T: thiopental; Group P: propofol; SD: Standard deviation
Intraoperative bradycardia, tachycardia, hypotension and hypertension were not observed in any patient. Between the groups, there was no statistically significant difference in terms of the mean Apgar scores at the 1st and 5th minutes after the induction and the umbilical vein blood gas values (Table 4, 5).
Table 4.
Evaluations of APGAR measurements
| APGAR | Group T (n=35) Mean±SD (Median) |
Group P (n=35) Mean±SD (Median) |
p |
|---|---|---|---|
| APGAR 1st minute | 8.80±0.83 (9) | 8.63±0.97 (10) | 0.145 |
| APGAR 5th minute | 9.94±0.23 (9) | 9.80±0.53 (10) | 0.219 |
Mann-Whitney U test. p<0.05. Group T: thiopental; Group P: propofol; SD: standard deviation
Table 5.
Umbilical cord vein blood gas measurements
| Umbilical vein blood gas | Group T (n=35) Mean±SD |
Group P (n=35) Mean±SD |
p |
|---|---|---|---|
| PH | 7.33±0.05 | 7.34±0.03 | 0.264 |
| PCO2 | 45.13±9.53 | 44.13±6.20 | 0.606 |
| PO2 | 38.98±11.78 | 43.44±21.73 | 0.290 |
| SpO2 | 72.22±18.22 | 71.76±15.48 | 0.912 |
| GLUCOSE | 68.14±13.65 | 69.66±10.40 | 0.604 |
| LACTATE | 16.91±7.07 | 15.06±4.58 | 0.197 |
| HCO3 | 21.99±1.60 | 22.21±1.05 | 0.498 |
| BE | −2.01±1.89 | −1.26±1.40 | 0.067 |
Student’s t-test. p<0.05. Group T: thiopental; Group P: propofol; PCO2: partial carbon dioxide pressure; PO2: partial oxygen pressure; SpO2: peripheral oxygen saturation; HCO3: bicarbonate; BE: base excess; SD: standard deviation
While no significant difference was detected between the groups with regard to the SAP, DAP, MAP, HR, SpO2 and VAS measurements at the 1st hour postoperatively, the recovery time was found to be significantly lower in Group P (p<0.01) (Table 6).
Table 6.
Evaluations of postoperative haemodynamics, VAS, recovery, awareness and side effects
| Postoperative 1st hour | Group T (n=35) Mean±SD |
Group P (n=35) Mean±SD |
+p |
|---|---|---|---|
| Systolic arterial pressure | 125.74±12.97 | 124.97±12.99 | 0.804 |
| Diastolic arterial pressure | 77.66±9.92 | 75.46±10.46 | 0.307 |
| Mean arterial pressure | 92.09±10.71 | 91.37±11.18 | 0.786 |
| Heart rate | 76.49±8.14 | 73.49±9.44 | 0.159 |
| SpO2 | 98.17±1.09 | 97.74±1.27 | 0.135 |
| Visual analogue scale (VAS) | 6.03±1.72 | 5.49±1.61 | 0.178 |
| Recovery time (min) | 11.70±1.95 | 9.87±2.67 | 0.002* |
| n (%) | n (%) | ||
| ++Administration of ondansetron hydrochloride | 9 (25.7) | 7 (20.0) | 0.569 |
| +++Administration of additional oxytocin | 3 (8.6) | 1 (2.9) | 0.614 |
| ++Nausea-vomiting | 9 (25.7) | 7 (20.0) | 0.569 |
| Remembering the key word | 0 (0) | 0 (0) | - |
| +++Dreaming/hearing a sound | 2 (5.7) | 2 (5.7) | 1.000 |
Student’s t-test;
Chi-square test;
Fisher’s Exact test; p<0,05;
p<0,01;
Group T: thiopental; Group P: propofol; SpO2: peripheral oxygen saturation
In the evaluation performed at the 1st hour postoperatively, while no patient remembered the key word whispered during the intervention, four stated that they dreamed or heard a voice under anaesthesia. No statistically significant difference was observed between the groups in terms of ondansetron hydrochloride administration at the 1st hour postoperatively, additionally administered oxytocin, nausea-vomiting, dreaming/hearing a noise and remembering the key word (p>0.05) (Table 6).
Discussion
Our study is one of the rare studies investigating the effects of induction agents on haemodynamics, intraoperative awareness, newborns, and postoperative recovery in caesarean sections performed under general anaesthesia. Our study demonstrated that the use of propofol in anaesthesia induction suppressed the haemodynamic response to intubation better and that it provided better haemodynamic stability, better depth of anaesthesia and more rapid postoperative recovery.
Moore et al. (10) conducted a study with 42 pregnant women to investigate the effects of propofol and thiopental on mothers’ haemodynamics, and they compared the use of 2,15 mg kg−1 propofol and 4.53 mg kg−1 thiopental in induction. They reported that blood pressure values are lower from induction until delivery in using propofol. Valtonen et al. (11) reported that the use of propofol 2.5 mg kg−1 and thiopental 5 mg kg−1 in caesarean sections display similar effects on intraoperative haemodynamics. In our study, it was observed that propofol caused less increase in blood pressure during laryngoscopy and intubation and provided better haemodynamics during intervention.
The determination of awareness in patients under general anaesthesia remains a problem in spite of modern anaesthetic techniques at present (12). Çakmak et al. (13) compared the use of pentothal and propofol in induction in 61 pregnant women and found that propofol provides better a depth of anaesthesia in the induction-delivery process. Similarly, Lee et al. (14) reported that propofol is a more appropriate agent for preventing intraoperative awareness in the early period of caesarean section and for providing adequate anaesthesia compared with pentothal. Different from other studies, in our study, the BIS values and haemodynamic parameters were recorded during the whole procedure and at important times during the intervention, and we investigated the depth of anaesthesia, intraoperative awareness and its haemodynamic effects for two induction agents, postoperative recovery and the effects of two agents on the postoperative haemodynamics, postoperative nausea-vomiting and VAS scores. Similar to the findings of the studies by Çakmak et al. (13) and Lee et al. (14), BIS values were apparently low from induction until the 8th minute in the propofol group, and it was also observed that the BIS values were higher at important times such as skin incision, uterus incision and birth of the baby in the thiopental sodium group. It was found that propofol provided better depth of anaesthesia in the period until delivery and that the effects of both anaesthetic agents on BIS were similar.
It was stated that intraoperative awareness under general anaesthesia occurs at a rate ranging from 0.1% to 0.9%. Caesarean sections have been defined as a risk factor for the development of awareness under general anaesthesia (15, 16). In a study conducted with 3000 patients who underwent caesarean section under general anaesthesia, the frequency rate of remembering anything and the frequency of dreaming were reported to be 0.9% and 7%, respectively (17). Kim et al. (18) conducted a study with 50 pregnant women and revealed that the use of 2.5 mg kg−1 propofol in induction was not different from 4 mg kg−1 pentothal in terms of intraoperative awareness. They also stated that they found awareness at similar rates in three patients from the propofol group and four patients from the pentothal group.
Different from other studies, in our study, the patients were told a key word at the time of the birth of the baby when the risk of awareness was considered to be high, and they were then questioned about this word postoperatively. While no patient remembered the key word, a total of four patients (two from the propofol group and two from the thiopental group) specified that they dreamed during general anaesthesia or that they heard a voice (5.7% frequency). The dreams were not related to the intervention or the key word.
Apgar scoring and cord blood gas analysis are among the parameters used for determining the general well-being of newborns (19). In the study by Mahjoobifard et al. (20) comparing propofol and thiopental induction in pregnant women, they found that Apgar scores at the 1st and 5th minutes are apparently high in the propofol group. In many clinical studies, it was emphasized that the effects of propofol and thiopental use in induction on Apgar scores and cord blood gas values are similar (21–23). In our study, the effects of propofol and thiopental sodium on the Apgar scores and cord blood gas values at the 1st and 5th minutes were found to be similar.
Today, anaesthetic agents used for obstetric anaesthesia are desired not to cause perioperative complications but rather to provide rapid recovery and to lead to fewer postoperative side effects. In many clinical studies on caesarean sections, it was mentioned that propofol is superior to thiopental sodium in induction with regard to recovery time and that it provides more rapid recovery (11, 24, 25). We also found in our study that the use of propofol provided more rapid recovery despite the fact that the co-operation times were similar.
Khahan et al. (25) conducted a study with 70 pregnant women who underwent general anaesthesia and reported that propofol provides a decrease in the need of analgesics during the postoperative first 2 h compared with thiopental. In two other clinical studies comparing the use of propofol and thiopental sodium in induction in caesarean sections, it was detected that the effect of propofol on the need for additional oxytocin and maternal blood loss is similar to that of thiopental sodium (21, 26). In our study, it was found that there was no difference between propofol and thiopental sodium with regard to the postoperative VAS values. Moreover, although it was statistically insignificant, the use of propofol caused postoperative nausea-vomiting and administration of additional oxytocin in less number of patients.
At present, because BIS monitoring is not a routine implementation, the efficiency of BIS monitoring in reducing the risk for awareness during caesarean sections should be evaluated by further studies. Another limitation of our study is that the interviews that were performed for questioning anaesthetic awareness at the 1st hour postoperatively were not repeated several times at different intervals.
Conclusion
In this study, it was revealed that the effects of propofol and thiopental sodium on intraoperative awareness, VAS scores, newborn’s Apgar scores and cord blood gases were similar. However, it was observed that the use of propofol suppressed the haemodynamic response to intubation more effectively and provided more depth of anaesthesia during induction-delivery process and more rapid postoperative recovery. Although both agents can be safely used in caesarean sections, it was observed that the use of propofol is more advantageous than thiopental because it provides adequate anaesthetic depth and more rapid recovery.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of İstanbul Ümraniye Training and Research Hospital (Protocol No: 2012/43).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - V.Ç.; Design - V.Ç., A.Y.; Supervision - A.Y., N.B.; Funding - V.Ç., A.Y., N.Ç.; Materials - V.Ç.; Data Collection and/or Processing - V.Ç.; Analysis and/or Interpretation - V.Ç., A.Y., N.B., N.Ç., Ö.B.; Literature Review - V.Ç., A.Y., N.Ç., Ö.B.; Writer - V.Ç.; Critical Review - V.Ç., A.Y., N.B., N.Ç., Ö.B.; Other - V.Ç., A.Y.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Birnbach DJ, Browne IM. Obstetric Anesthesia. In: Miller RD, editor. Miller’s Anesthesia. 6. baskı. Aydın D. İzmir; 2010. pp. 2307–45. Çev. Ed. [Google Scholar]
- 2.Robins K, Lyons G. Intraoperative awareness during general anesthesia for cesarean delivery. Anesth Analg. 2009;109:886–90. doi: 10.1213/ane.0b013e3181af83c1. http://dx.doi.org/10.1213/ane.0b013e3181af83c1. [DOI] [PubMed] [Google Scholar]
- 3.Leslie K, Chan MT, Myles PS, Forbes A, McCulloch TJ. Posttraumatic stress disorder in aware patients from the B-Aware trial. Anesth Analg. 2010;110:823–8. doi: 10.1213/ANE.0b013e3181b8b6ca. http://dx.doi.org/10.1213/ANE.0b013e3181b8b6ca. [DOI] [PubMed] [Google Scholar]
- 4.Ghoneim MM, Block RI, Haffarnan M, Mathews MJ. Awareness during anesthesia: risk factors, causes and sequelae: a rewiew of reported cases in the literature. Anesth Analg. 2009;108:527–35. doi: 10.1213/ane.0b013e318193c634. http://dx.doi.org/10.1213/ane.0b013e318193c634. [DOI] [PubMed] [Google Scholar]
- 5.Tunstall ME. Awareness, caesarean section and the isolated forearm technique. Anaesthesia. 1990;45:686. doi: 10.1111/j.1365-2044.1990.tb14405.x. http://dx.doi.org/10.1111/j.1365-2044.1990.tb14405.x. [DOI] [PubMed] [Google Scholar]
- 6.Grover VK, Bharti N. Measuring depth of anesthesia-an overview on the currently available monitoring systems. The Indian Anaesthetists’ Forum. 2008;9:1–32. [Google Scholar]
- 7.Ghoneim MM. Awareness during anesthesia. Anesthesiology. 2000;92:597–602. doi: 10.1097/00000542-200002000-00043. http://dx.doi.org/10.1097/00000542-200002000-00043. [DOI] [PubMed] [Google Scholar]
- 8.Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Sysy Rev. 2007:CD003843. doi: 10.1002/14651858.CD003843.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358:1097–108. doi: 10.1056/NEJMoa0707361. http://dx.doi.org/10.1056/NEJMoa0707361. [DOI] [PubMed] [Google Scholar]
- 10.Moore J, Bill KM, Flynn RJ, McKeating T, Howard PJ. A comparison between propofol and thiopentone as induction agents in obstetric anaesthesia. Anesthesia. 1989;44:753–7. doi: 10.1111/j.1365-2044.1989.tb09263.x. http://dx.doi.org/10.1111/j.1365-2044.1989.tb09263.x. [DOI] [PubMed] [Google Scholar]
- 11.Valtonen M, Kanto J, Rosenberg P. Comparasion of propofol and thiopentone for induction of anesthesia for elective cesarean section. Anesthesia. 1989;44:758–62. doi: 10.1111/j.1365-2044.1989.tb09264.x. http://dx.doi.org/10.1111/j.1365-2044.1989.tb09264.x. [DOI] [PubMed] [Google Scholar]
- 12.Bischoff P, Rundshagen I. Awareness under general anesthesia. Dtsch Arztebl Int. 2011;108:1–7. doi: 10.3238/arztebl.2011.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cakmak S, Olguner C, Karci A, Tasdögen A, Korkmaz H, Yılmaz M, et al. Propofol decreases bispectral index during the induction-delivery period in caesarean section. European J Anesthesiology. 2006;23:179. http://dx.doi.org/10.1097/00003643-200606001-00643. [Google Scholar]
- 14.Lee HJ, Chon JY, Sung CH. Reevaluation of thiopental and propofol using bispectral index in the early period of cesarean section. Koeran J Anesthesiol. 2007;52:49–54. http://dx.doi.org/10.4097/kjae.2007.52.1.49. [Google Scholar]
- 15.Sebel PS, Bowdle TA, Ghoneim MM, Ranpil IJ, Podilla RE, Gan TJ, et al. The incidence of awareness during anesthesia: a multicenter United States study. Anesth Analg. 2004;99:833–9. doi: 10.1213/01.ANE.0000130261.90896.6C. http://dx.doi.org/10.1213/01.ANE.0000130261.90896.6C. [DOI] [PubMed] [Google Scholar]
- 16.Wang E, Zhi YE, Yundan P, Zangbin S, Changsheng H, Hui L, et al. Incidence and risk factors of intraoperative awareness during general anesthesia. J Cent South Univ (Med Sci) 2011;36:671–5. doi: 10.3969/j.issn.1672-7347.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Lyons G, Macdonald R. Awareness during caesarean section. Anaesthesia. 1991;46:62–4. doi: 10.1111/j.1365-2044.1991.tb09321.x. http://dx.doi.org/10.1111/j.1365-2044.1991.tb09321.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim SB, Choi YS, Lee IO. Comparasion of effects of propofol and thiopental as induction agent for cesarean section on succinylcoline, maternal consciousness and APGAR score. Korean J Anesthesiol. 1995;28:221–7. [Google Scholar]
- 19.Rolbin SH, Cohen MM, Levinton CM, Kelly EN, Farine D. The premature infant: Anaesthesia for cesarean delivery. Anesth Analg. 1994;78:912–7. doi: 10.1213/00000539-199405000-00013. http://dx.doi.org/10.1213/00000539-199405000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Mahjoobifard M, Dadras MM, Panahipour A, Dadras MA. The comparasion of propofol with thiopental as induction drug on neonatal APGAR during elective cesarean section. Zahedan J of Research in Medical Sciences. 2011;13:35–9. [Google Scholar]
- 21.Mercan A, El-Kardawy H, Khalil M, Al-Subaie H, Bakhamees HJ. A prospective, randomized comparasion of the effects of thiopental and propofol on bispectral index during caesarean section till delivery of newborn. M E J Anesth. 2012;21:699–704. [PubMed] [Google Scholar]
- 22.Marzieh L, Mohammad A, Malihah G, Taghi M. Comparative study of effect of general anesthesia with thiopental and propofol on APGAR score of neonate and uterine relaxation in cesarean section. Iranian Journal of Obstetrics, Gynecology and Infertility. 2012;15:30. [Google Scholar]
- 23.Gin T, Gregory MA, Oh TE. The haemodynamic effects of propofol and thiopentone for induction of caesarean section. Anaesth Intensive Care. 1990;18:175–9. doi: 10.1177/0310057X9001800203. [DOI] [PubMed] [Google Scholar]
- 24.So SY, Park JH, Park HK, Song HS, Choe H, Han YJ. Maternal and neonatal effects of thiopental sodium-enflurane-N2O and propofol-N2O anesthesia for cesarean section. Korean J Anesthesiol. 1996;30:470–8. [Google Scholar]
- 25.Khahan B. The comparasion of propofol with thiopental on neonatal APGAR during cesarean section. J Shahrekord Univ Med Sci. 2007;9:10–4. [Google Scholar]
- 26.Djordjevic B, Stojilkovic MP, Mostic T, Vojvodic LJ, Loncar SD. Propofol and thiopentone in elective cesarean section: effect on the mother and neonate. Vojnosanit Pregl. 1998;55:601–4. [PubMed] [Google Scholar]


