Abstract
Objective
To investigate the effects of general anaesthesia and general+epidural anaesthesia on the stress response which was evaluated with the adrenocorticotrophic hormone (ACTH), cortisol, insulin, and glucose levels and the haemodynamic parameters.
Methods
Forty two, American Society of Anesthesiologists physiologic status I–II, patients undergoing hip and knee arthroplasty were randomized into two groups; general anaesthesia (Group G) and general anaesthesia+epidural anaesthesia (Group E). Epidural anaesthesia: patients in Group E received epidural anaesthesia with 0.5% bupivacaine, a lumbar epidural catheter was placed and after achieving sensorial block at T10 dermatome, general anaesthesia was commenced. General anaesthesia was standardized in both groups. Further, plasma ACTH, cortisol, insulin and glucose levels were determined at preoperative=t1, after the surgical incision=t2, postoperative 2nd hour=t3 and postoperative 24th hour=t4. Perioperative heart rate, blood pressures, pain scores and morphine consumption were also determined.
Results
ACTH levels were higher in Group G than Group E [Group G, t2: 71.4±39.9 pg mL−1, t3: 578.6±566.1 pg mL−1, Group E, t2: 20.2±16.2 pg mL−1, t3: 56.3±73.6 pg mL−1 (p<0.001)]. Cortisol, was higher in Group G compared with Group E [Group G, t3: 33.4±13.1 μg dL−1, t4: 34.1±22.5 μg dL−1, Group E, t3: 19.1±10.3 μg dL−1, t4: 21.3±8.1 μg dL−1 (p=0.001 and p=0.002)]. The insulin levels were higher compared with the baseline values at t3, and glucose was higher at t3 and t4 in both groups. Haemodynamic parameters were stable in Group E, and pain scores and morphine consumption were higher in Group G than in Group E.
Conclusion
Our results suggest that epidural anaesthesia combined with general anaesthesia suppressed the stress response, which was evaluated with ACTH, cortisol levels and haemodynamic parameters; however, this method was ineffective to attenuate the increase in glucose and insulin levels.
Keywords: ACTH, arthroplasty, epidural anaesthesia, cortisol, insulin, stress response
Introduction
A series of neuroendocrine, metabolic and inflammatory changes that occur after surgical trauma for maintaining homeostasis constitute the stress response (1, 2). The surgical incision initiates the stress response by stimulating the sympathetic nervous system through afferent nerve endings and the hypothalamic–adrenal cortex axis (1–3). Mainly, the secretions of catabolic hormones, such as pituitary hormones and catecholamines, increase, whereas the secretions of anabolic hormones, such as insulin and testosterone, decrease (1, 3, 4). The aim of these changes is to provide the redistribution of energy substrates and to increase the intravascular volume through gluconeogenesis, glycolysis, proteolysis, lipolysis and fluid-sodium retention (1, 3, 4). The stress response, which basically protects the organism by elevating blood glucose and blood pressure, can also prove harmful for the organism if increased significantly. Some complications, including thromboembolism, stress ulcers, heart failure, infarction and pulmonary failure, develop due to excessive mobilization of reserves, catabolised metabolism, increased oxygen consumption, negative nitrogen balance, insulin resistance and fluid-sodium retention (4).
Suppression of the surgical stress response can positively affect postoperative results (4–7). Minimally invasive surgical techniques, regulation of nutrition, pain control, hormonal treatments and protection of normothermia are some of the methods used to this end (6). Anaesthesia techniques are also used for modifying the surgical stress response (7). The investigation of the surgical stress response with different anaesthetic agents and techniques in many types of surgeries is still of interest to many researchers (8–11). Many of these studies are related to abdominal surgery. Because the stress response is also associated with characteristics of the surgery, the effects of anaesthetic techniques on the stress response in different types of surgeries should be investigated (7, 11, 12). The effect of combined administration of epidural anaesthesia with general anaesthesia on the stress response in arthroplasties has not been studied yet. Because arthroplasty leads to an apparent surgical stress response, the presenting study has been conducted with patients undergoing arthroplasty (13–17).
The aim of this prospective randomized study was to compare the effects of general anaesthesia alone with the effects of combined epidural anaesthesia and general anaesthesia on the surgical stress response in hip and knee arthroplsty. The surgical stress response was evaluated in terms of the plasma adrenocorticotropic hormone (ACTH), cortisol, insulin and glucose levels along with haemodynamic parameters.
Methods
The study was conducted after obtainig ethical approval from the Ethics Committee of the Ministry of Health Dışkapı Yıldırım Beyazıt Education and Research Hospital and written informed consents from the patients.
The study included 42 American Society of Anaesthesiologists (ASA) physical status I–II patients, aged between 20–60 years, undergoing elective orthopaedic knee and hip arthroplasty and having a Homeostasis Model Assessment score (HOMA) (8) <2.1. The exclusion criteria were: contraindications for epidural anaesthesia; peripheral neuropathy; neuroendocrine diseases; kidney, liver and cardiovascular diseases; the use of any drug that could affect haemodynamics, the immune system, hormonal and metabolic states; and the history of alcohol or drug addiction. The patients were educated on patient-controlled analgesia (PCA) one day before the surgery.
All surgeries were performed before 11.00 a.m. for providing the conformity between measurements of endocrine parameters and diurnal rhythms. The patients fasted overnight and were hydrated with 500 mL Ringer’s lactate solution 30 min before the anaeshesia induction, premedication was provided with 0.05 mg kg−1 intravenous (iv) midazolam.
Patients were monitored with electrocardiography (DII) peripheral oxygen saturation (SpO2), non-invasive blood pressure and tympanic body temperature. Baseline values were recorded. Peripheral vein and radial artery cannulations were performed. İnvasive blood pressure was monitored after radial artery cannulation.
The patients were divided into 2 groups by randomly drawing lots from a sealed envelope: the groups were the general anaesthesia group (Group G) and the general anaesthesia+epidural anaesthesia group (Group E).
Epidural anaesthesia was administered with 15–20 mL 0.5% bupivacaine through an epidural catheter inserted into the L3–4 or L4–5 space in the Group E patients. Sensory block was evaluated with a pin-prick test every 5 minutes. After the sensory block reached T10 level, general anaeshesia was commenced.
General anaeshesia was provided with 2–3 mg kg−1 propofol, 1 μg kg−1 fentanyl and 0.1 mg kg−1 vecuronium for induction and intubation and maintained with sevoflurane in a mixture of oxygen and nitrous oxide in both groups.
The patients were ventilated to achieve normocarbia. All patients received 8 mL kg hour−1 Ringer’s lactate solution. Blood loss was replaced with colloids and packed red blood cells if needed. Intravenous fluids and blood were warmed and intraoperative normothermia was assured with warming blankets. Heart rate (HR), systolic arterial pressure (SAP), diastolic arterial pressure (DAP) and the mean arterial pressure (MAP) were measured every 5 minutes during surgery. Changes in MAP and HR >20% from the baseline values were considered as hypertension and tachycardia and were treated with 50 μg fentanyl iv. HR <45 beat min−1 was considered as bradycardia and was treated with 0.5 mg iv atropine, MAP <25% or <60 mmHg was considered as hypotension and was treated with 250 mL iv crystalloid fluid bolus and/or with 5 mg iv ephedrine. All adverse events and treatments were recorded. The amount of intraoperative blood loss was calculated from the blood accumulated in the surgical suction canister and from the surgical gauzes. Blood transfusion and the amount of the fluids administered were recorded. In Group G, PCA infusion was initiated 15 minutes before the end of the surgery. The patients who were extubated according to clinical extubation criteria were transferred to the recovery room after anaesthesia and haemodynamic parameters were evaluated at 10-minute intervals. When the Aldrete (18) score was ≥9, the patients were transferred to the clinic. The duration of surgery was recorded.
Postoperative analgesia was provided with intravenous PCA in Group G (Morphine HCL, loading dose: 5 mg; basal infusion: 0.3 mg hour−1; bolus dose: 1 mg; lock-out time: 15 minutes) and with epidural PCA in Group E (Morphine HCL, loading dose: 2 mg; bolus dose: 1 mg; lock-out time: 30 minutes; 4-hour limit: 3 mg). Postoperative analgesia was evaluated with visual analogue scale (VAS, 0: no pain; Vas, 10: most severe pain imaginable) at the 1st, 2nd, 3rd, 6th, 12th and 24th hours. Total morphine use of patients and side effects (nausea, vomiting, itching, hypotension, urinary retention and respiratory depression) were recorded.
Evaluation of the stress response
Arterial blood samples were collected at preoperative (t1), post-surgical incision (t2), postoperative 2nd hour (t3) and postoperative 24th hour (t4) and were placed on ice. Serum was obtained by centrifugation at 2000 g. Samples were kept at −70°C until they were analysed in the clinical biochemistry laboratory. The cortisol (reference interval, 6.2–19.4 μg dL−1 between 07:00–10:00 a.m. and 2.3–11.9 μg dL−1 between 04:00–08:00 p.m.), ACTH (reference interval, 7.2–63.6 pg mL−1 between 07:00–10:00 a.m.) and insulin levels (reference interval 2.6–24.9 U mL−1) were measured with the electrochemiluminescence immunological test method (Roche Modular EVO E-170 Hormone Autoanalyser). The glucose levels (reference interval, 70–110 mg dL−1) were measured with the UV test method (Roche Hitachi P 1600 autoanalyser).
Statistical analysis
The data were analysed using Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) Windows 11.5 software. The normality of the distribution of continuous variables was examined with Shapiro–Wilk test. Descriptive statistics were expressed as mean ± standard deviation or median (minimum value–maximum value) for continuous variables and as the number of cases (n) and percentage (%) for nominal variables. The presence of significant difference was evaluated with Student’s t-test in terms of the means between the groups and with Mann–Whitney U test for median values. Nominal variables were analysed with Pearson’s Chi-Square test or Fisher’s exact chi-square test. The difference with regard to repeating haemodynamic measurements in the groups was evaluated with repetitive measurement variance analysis and Friedman analysis. In the case of a significant result, Bonferroni correction multiple comparison test or Bonferroni correction with Wilcoxon signed-rank test were performed to determine which value caused the difference. A p<0.05 value was considered statistically significant. To maintain Type I error under control in all possible multiple comparisons, Bonferroni correction was used. The sample size calculation was based on a randomized prospective research comparing the effects of two different anaesthesia techniques on cortisol change. According to this evaluation, 21 patients were needed in each group for the detection of the difference between two groups with 80% power and 0.05 alpha error (19).
Results
The study was completed with 40 patients. Two patients were excluded from the study due to surgical complications. The groups were similar in terms of patient characteristics, the duration of surgery and the amount of bleeding (Table 1). No difference was found between the groups with regard to preoperative HR, blood pressure, cortisol, ACTH, insulin and glucose levels.
Table 1.
Patient characteristics, duration of surgery, intraoperative blood loss and intraoperative fluid replacement compared between groups
| Variables | Group G (n=20) | Group E (n=20) | p |
|---|---|---|---|
| Age (year)a | 65.8±10.1 | 61.5±8.8 | 0.163† |
| Gender Female/Male (n) | 13/7 | 13/7 | 1.0† |
| Body weight (kg)a | 79.3±11.6 | 73.7±6.5 | 0.067† |
| Arthroplasty Knee/Hip (n) | 14/6 | 12/8 | 0.507¶ |
| Duration of surgery (min)b | 95 (90–120) | 100 (91.2–122.2) | 0.429¥ |
| Intraoperative bleeding (mL)a | 300±60 | 267±68 | 0.05† |
| Fluid replacement (mL)a | 2433±377 | 2302±265 | 0.06† |
Values in amean±standard deviation, (n)number of patients, b median (min-max). Group G:general anaesthesia, Group E: epidural+general anaesthesia Statistics:
Student’s t-test,
Pearson’s Chi-Square Test,
Mann–Whitney U Test.
No difference between the groups.
There was a significant difference between the groups in terms of ACTH levels. ACTH levels were significantly higher in Group G than in Group E (p=0.004). In Group G, compared with the preoperative levels, ACTH levels increased after surgical incision (t1: 33.2±13.9 pg mL−1, t2: 71.4±39.9 pg mL−1, p=0.001). ACTH reached its highest level at the postoperative 2nd hour (t3: 578.6±566.1 pg mL−1, p<0.001) and returned to normal levels at the postoperative 24th hour (42.5±47.7 pg mL−1).
In Group E, compared with the baseline levels, no difference was observed in the change of ACTH levels within time. ACTH levels were found to be 20.2±16.2 pg mL−1 after incision and 56.3±73.6 pg mL−1 (p=0.05) at the postoperative 2nd hour (Table 2).
Table 2.
The changes in the plasma adrenocorticotropic hormone (ACTH), cortisol, insulin and glucose levels in time compared between groups
| Variables | Group G | Group E | pa |
|---|---|---|---|
| Preoperative ACTH | 33.2±13.9 | 30.2±11.1 | 0.056 |
| Post-incision ACTH | 71.4±39.9* | 20.2±16.2 | <0.001† |
| ACTH at postop 2 hour | 578.6±566.1¶ | 36.3±41.9 | <0.001† |
| ACTH at postop 24 hour | 42.5±47.7 | 9.4±3.4 | <0.001† |
| *, ¶pb | <0.001 | 0.05 | |
| Preoperative cortisol | 17.5±5.4 | 17.4±5 | 0.925 |
| Post-incision cortisol | 15.9±7.8 | 17.4±7.1 | 0.383 |
| Cortisol at postop 2 hour | 33.4±13.1* | 19.1±10.3 | 0.001† |
| Cortisol at postop 24 hour | 34.1±22.5¶ | 21.3±8.1 | 0.002† |
| *, ¶pb | <0.001 | 0.712 | |
| Preoperative insulin | 13.1±9 | 12.9±7.0 | 0.445 |
| Post-incision insulin | 13.2±35.9 | 9.9±8.0 | 0.134 |
| Insulin at postop 2 hour | 14.7±28.8 | 9.1±3.7 | 0.289 |
| Insulin at postop 24 hour | 27.6±22.8* | 24.0±9.3* | 0.758 |
| *pb | <0.001 | <0.001 | |
| Preoperative glucose | 113.5±15.3 | 108±5.7 | 0.265 |
| Post-incision glucose | 118.1±11.2 | 112.4±10.0 | 0.072 |
| Glucose at 2 hour | 143.8±18.6* | 120±10.3* | <0.001† |
| Glucose at 24 hour | 155.8±19.2¶ | 145.2±9.0¶ | 0.054 |
| *, ¶pb | 0.001 | 0.001 |
Group G: general anaesthesia, Group E: epidural+general anaesthesia. Values are mean ±standard deviation. Statistics: Variance Analysis,
Bonferroni Correction with Wilcoxon signed-rank test.
Significant difference compared with the preoperative values,
Significant difference between the groups.
On the other hand, there was a significant difference between the groups in terms of cortisol levels. Cortisol was significantly higher in Group G than in Group E. The cortisol levels in Group G were t1: 17.5±5.4 μg dL−1, t2: 15.9±7.8 μg dL−1, t3: 33.4±13.1 μg dL−1 and t4: 34.1±22.5 μg dL−1. The increase in the cortisol levels reached significance at the postoperative 2nd hour (p=0.001) and remained high at the postoperative 24th hour (p=0.004). In the intra-group comparisons of Group E, compared with the preoperative levels, no difference was detected in the cortisol levels during the whole research process (p=0.712) (Table 2).
In both groups, insulin levels at the postoperative 24th hour were found to be higher than the preoperative levels. The highest insulin levels at t4 were detected to be 27.6±22.8 U mL−1 in Group G and 24.0±9.3 U mL−1 in Group E (p<0.001 and p<0.001). There was no statistically significant difference between the groups in terms of insulin levels (Table 2).
Glucose levels gradually increased in both groups. A significant increase was found at the postoperative 2nd hour (143.8±18.6 mg dL−1) and 24th hour (155.8±19.2 mg dL−1) in Group G. Similarly, a significant increase was observed in Group E at the postoperative 2nd (120±10.3 mg dL−1) and 24th (145.2±9.0 mg dL−1) hours (p=0.001). The increase at the postoperative 2nd and 24th hours was more apparent in Group G (p<0.001 and p=0.024) (Table 2).
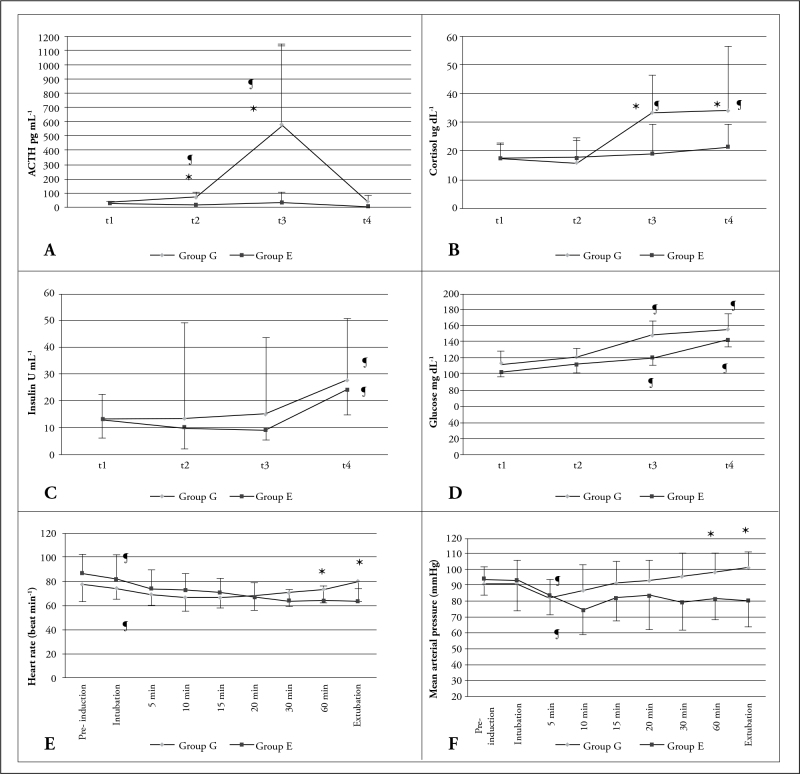
HR values decreased after anaesthesia induction in both groups and increased at the intraoperative 1st hour and postoperative 12th hour in Group G (p<0.001). MAP values were higher in Group G than in Group E at the intraoperative 30th and 60th minutes and during extubation. HR and MAP values were lower in Group E than the respective preoperative values at more than one measurement performed during the monitorization procedure. The ACTH, cortisol, insulin and glucose levels and the changes in HR and MAP values are presented in Figure 1 for both groups.
Figure 1.
A–F. Comparison of the general anaesthesia (Group G) and general anaesthesia+epidural anaesthesia (Group E) groups with regard to the adrenocorticotropic hormone (ACTH), cortisol, insulin and glucose levels and the changes in the heart rate (HR) and mean arterial pressure (MAP) over time
A, B: Suppressed ACTH and cortisol levels in Group E.
C, D: Increased insulin and glucose levels in both groups.
E, F: Heart rate (HR) and mean arterial pressure (MAP) values lower than pre-induction values at many measurements performed during the whole monitoring.
t1: pre-induction, t2: post-incision, t3: postoperative 2nd hour, t4: postoperative 24th hour.
¶significant difference compared with pre-induction value, *significant difference between groups
All values in mean±standard deviation
It was observed that sufficient analgesia was provided during the study in both groups (in both groups, the mean VAS score was ≤3). However, when the groups were compared, VAS scores for pain of Group E were found to be lower than those of Group G at the postoperative 1st, 2nd, 3rd and 6th hours. VAS pain scores of the groups at the postoperative 12th and 24th hours were similar (Table 3). The use of morphine was different for both groups. It was 49.1 (30.7–63.5) mg in Group G and 10.3 (7.1–13.7) mg in Group E (p=0.001) (Table 3).
Table 3.
Visual analogue scale (VAS) pain scores, morphine consumption and complications compared between groups
| Variables | Group G n=20 | Group E n=20 | p | |
|---|---|---|---|---|
| 1. hour | 3 (2–5) | 1 (1–3) | <0.001† | |
| Postoperative | 2. hour | 4 (3–5) | 1 (0–2) | <0.001† |
| VASa * | 3. hour | 3 (2–5) | 1 (0–2) | <0.001† |
| 6. hour | 3 (2–5) | 1 (1–2) | <0.001† | |
| Morphine Consumption (mg)a | 49.1 (30.7–63.5) | 10.3 (7.1–13.7) | 0.001γ | |
| Complication (n) | 13 (65.0%) | 12 (60.0%) | 0.744¶ | |
| Nausea-vomiting (n) | 11 (55.0%) | 12 (60.0%) | 0.749¶ | |
| Urinary retention (n) | 7 (35.0%) | 5 (25.0%) | 0.490¶ | |
Group G:general anaesthesia, Group E: epidural+general anaesthesia.
Values are median (min-max), (n) numbers of occurences (frequencies) Statistical evaluation with
Friedman Test and Bonferroni Correction with Wilcoxon Signed-rank Test,
Pearson’s Chi-Square Test,
Mann-Whitney U Test.
VAS scores and morphine consumption were different betweem groups.
The incidence of postoperative complications was similar between the treatment groups. Nausea/vomiting was observed in 11 patients in Group G (55%) and in 12 patients from Group E (60%) (p=0.749). Urinary retention was seen in 6 patients in Group G (35%) and in 5 patients from Group E (25%) (p=0.490).
Discussion
Surgical trauma causes a stress response that is characterized by changes in the hormonal and autonomic nervous system activity, inflammation, immune depression and pain (1). This study demonstrated that epidural anaesthesia combined with general anaesthesia and epidural analgesia provided heampdynamic stability, prevented the the increase in cortisol and ACTH levels but did not affect the insulin and glucose levels in patients undergoing elective hip and knee arthroplasty. Lower postoperative pain scores and lower morphine consumption suggested that addition of epidural anaesthesia to general anaesthesia could partially suppress the surgical stress response through the prevention of afferent nociceptive imput.
The most distinct stress response that occurs in association with surgical stimuli and the anaesthesia technique are the haemodynamic changes. The release of adrenalin from the presynaptic nerve endings as a result of nociceptive stimuli and stimulation of increased catecholamine secretion from the adrenal medulla initiate the stress response which expresses itself with tachycardia and hypertension (3, 6). In our study, compared with the preoperative values, HR and MAP values decreased in both groups after anaesthesia induction. It was observed that both anaesthesia techniques were effective in the suppression of the haemodynamic response associated with anaesthesia applications such as laryngoscopy and intubation. At many measurements, HR and MAP values were higher in Group G than in Group E. The HR and MAP values were lower during the whole monitorization in Group E than in Group G. It was thought that lower MAP values in Group E might have resulted from better suppression of the surgical stress response through the inhibition of nociceptive stimuli and with the vasodilatation caused by epidural anaesthesia.
Cortisol and ACTH levels are among the sensitive indicators of stress response (7). Surgery is one of the powerful stimuli for ACTH and cortisol secretions, and plasma levels of these hormones increase within minutes following the initiation of the surgery. Basal cortisol level is 400 mmol L−1, and it can increase up to 1500 mmol L−1 depending on the severity of surgery (3). Although ACTH levels are normally expected to decrease depending on increasing cortisol levels, this control mechanism can be impaired after surgery, and both hormone levels can rise. In this study, in Group G, ACTH levels increased by more than 2 times after incision and by more than 7 times at the postoperative 2nd hour compared with the baseline levels. Cortisol levels increased 2-fold compared with the basal levels at the postoperative 2nd and 24th hours. On the other hand, an increase was observed in ACTH and cortisol levels in Group E however this did not reach statistically significance.
Elevated catecholamine levels after surgical incision leads to an increase in blood glucose concentration through glycogenosis and gluconeogenesis. Increased blood glucose stimulates insulin secretion. Insulin has an anabolic effect. It helps utilisation of glucose and the production of glycogen and decreases lipolysis and protein breakdown. This mechanism can be inadequate during trauma, and a functional insulin deficiency, called insulin resistance, develops in the organism (6). Studies have shown that insulin sensitivity can decrease to as much as 50% (20). The degree of insulin resistance depends on the severity of surgery. Hip and knee arthroplasties lead to high levels of stress response. Our study demonstrated that the administration of epidural anaesthesia in hip and knee arthroplasties can inhibit the increase of insulin secretion intraoperatively however insulin resistance stil can develop on the postoperative 1st day.
In studies on anaesthesia techniques used for suppressing the stress response, both regional and intravenous anaesthesia techniques have been investigated (7, 10–12). The efficiency of intravenous anaesthesia techniques or drug administration during intraoperative period is restricted to the intraoperative period (4, 21). Nonetheless, it can be suggested that regional anaesthesia applications, especially with catheter applications, can be effective for suppressing the stress response in the postoperative period too, and it will be convenient to use them in orthopaedic interventions.
In a study comparing the intravenous PCA, 3-1 block and epidural anaesthesia techniques in patients undergoing knee arthroplasty, although pain scores were similar and sufficient analgesia was provided in all groups the best stress response control was accomplished with epidural anaesthesia (22). Beyazıt et al. (23) conducted another study and applied combined spinal epidural anaesthesia to the patients who underwent knee arthroplasty. The authors provided postoperative analgesia with epidural levobupivacaine–fentanyl and demonstrated that the stress response could be suppressed. Another study showed that epidural 45 μg kg−1 morphine, which was administered 45 minutes before knee arthroplasty, prevented the increase in cortisol secretion (17). There are also negative results concerning the control of stress response with regional anaesthesia in arthroplasty. Al Oweidi et al. (24) administered preemptive 2% epidural ropivacaine in order to modify the endogenous opioid response and continued the infusion for 11–20 hours. The authors reported that despite sufficient analgesia they could not suppress the stress response which was evaluated with the plasma beta-endorphin, ACTH and cortisol concentrations. Moreover, Bagry et al. (25) revealed that continuous lumbar plexus and sciatic block application with 2% ropivacaine did not suppress the stress response in knee arthroplasty.
Because afferent nerve impulses and activation of the autonomic nerve system and other reflexes with pain can be a major factor to initiate the of endocrine metabolic responses, pain control is a powerful method for the supression of the surgical stress response. Despite the analgesic efficiency of non-steroid anti-inflammatory drugs, their effects on metabolic changes in surgical patients are minimal, and they are recommended to be used as a part of a multimodal approach for the suppression of stress response. The effect of low-dose systemic opioids is also similar (4). Epidural patient-controlled analgesia is the most effective analgesic method after major surgeries (5). It was demonstrated that despite their capacity for the suppression of intraoperative stress response, epidural opioids are not as effective as continuous local anesthetic infusions, in the postoperative period (5). During spinal or epidural anaesthesia the level of the sensory block and the region of the surgical intervention has an effect on the control of the stress response. In this study, the distribution of epidural anaesthesia was assured to be at the T10 level in all patients. In the postoperative period, only opioid was used because epidural local anaesthetic infusion could delay mobilization (26). Pain scores of patients were monitored for postoperative 24 hours, and lower VAS pain scores were observed with epidural PCA. Partial suppression of stress response despite efficient pain control suggests that mechanisms apart from afferent nerve impulses can be effective in the occurrence of stress response.
Insulin resistance can occur independent of typical stress hormones (7). Besides, it is known that epidural anaesthesia and analgesia can reduce postoperative insulin resistance only in patients with preoperative insulin resistance (8). The absemce of a difference between the groups in terms of insulin levels may be related to the fact that that the study population included patients without preoperative insulin resistance.
Leukocytes activated in response to tissue damage, fibroblasts and cytokines secreted from endothelial cells play an important role in the inflammatory response that occurs in response to surgery. Local anesthetics can display their anti-inflammatory action by inhibiting the release of some anti-inflammatory mediators and neutrophil and macrophage functions (27). It is suggested that the positive results associated with epidural anaesthesia, cocerning pain and thromboembolism, can be related not only to the blockade of afferent impulses but also to the anti-inflammatory effects of local anaesthetics (27). It has been reported that epidural anaesthesia suppresses early inflammatory response and protects cytokine balance in the postoperative period. However, this is still controversial (1). In this study, it was thought that the effect of anaesthesia technique on cytokine response to the surgery was restricted because it could not prevent tissue trauma and the cytokine response, thus causing insulin resistance.
The stress response characterized by hyperglycaemia, insulin resistance and increased catecholamine, cortisol and ACTH levels can cause impairment in the intake and storage of glucose into the muscle tissue in the postoperative period, increased muscle protein breakdown and muscle weakness by forming a negative nitrogen balance. Therefore, the suppression of this response can provide benefit especially in orthopaedic surgery (15). We found that the addition of epidural anaesthesia to general anaesthesia, which provided sensory block at the T10 level with 0.5% bupivacaine in the intraoperative period, and the postoperative administration of epidural PCA with morphine could suppress the stress response partially. In patients who are subjected to epidural catheterisation, the continuance of local anaesthetics also during the postoperative period can be more efficient for suppressing the stress response with an anti-inflammatory effect. However, as the doses and side effects of this procedure along with the type of local anaesthetic used are not known yet, further studies should be conducted on this topic.
Conclusion
In our study, we found that the combined administration of epidural anaesthesia with general anaesthesia during elective knee and hip arthroplasties suppressed the stress response, which was evaluated with haemodynamic variables, ACTH and cortisol levels. However, it could not prevent the increase in insulin and glucose levels.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Dışkapı Yıldırım Beyazıt Training and Research Hospital.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Y.S., D.Y., H.G.; Design - Y.S., D.Y., H.G.; Supervision - Y.S., D.Y., H.G.; Funding - Y.S., D.Y., H.G.; Materials - Y.S., O.Ç.; Data Collection and/or Processing - Y.S., O.Ç., D.Y.; Analysis and/or Interpretation - Y.S., D.Y., H.G.; Literature Review - Y.S., D.Y.; Writer - Y.S., D.Y., H.G., O.Ç.; Critical Review - D.Y., H.G.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Gibbison B, Angelini GD, Lightman SL. Dynamic output and control of the hypothalamic-pituitary-adrenal axis in critical illness and major surgery. Br J Anaesth. 2013;111:347–60. doi: 10.1093/bja/aet077. http://dx.doi.org/10.1093/bja/aet077. [DOI] [PubMed] [Google Scholar]
- 2.Fant F, Tina E, Sandblom D, Andersson SO, Magnuson A, Hultgren-Hornkvist E, et al. Thoracic epidural analgesia inhibits the neuro-hormonal but not the acute inflamatory stress responcse after radical retropubic prostatectoy. Br J Anaesth. 2013;110:747–57. doi: 10.1093/bja/aes491. http://dx.doi.org/10.1093/bja/aes491. [DOI] [PubMed] [Google Scholar]
- 3.Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85:109–17. doi: 10.1093/bja/85.1.109. http://dx.doi.org/10.1093/bja/85.1.109. [DOI] [PubMed] [Google Scholar]
- 4.Kehlet H. Manuplation of the metabolic response in clinical practice. World J Surg. 2000;24:690–5. doi: 10.1007/s002689910111. http://dx.doi.org/10.1007/s002689910111. [DOI] [PubMed] [Google Scholar]
- 5.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–17. doi: 10.1093/bja/78.5.606. http://dx.doi.org/10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 6.Burton D, Nicholson G, Hall G. Endocrine and metabolic response to surgery. Continuing education in anaesthesia. Critical Care and Pain. 2004;4:144–7. http://dx.doi.org/10.1093/bjaceaccp/mkh040. [Google Scholar]
- 7.Marana E, Colicci S, Meo F, Marana R, Proietti R. Neuroendocrin stress response in gynecological laparoscopy: TIVA with propofol versuss sevoflurane anesthesia. J Clin Anesth. 2010;22:250–5. doi: 10.1016/j.jclinane.2009.07.011. http://dx.doi.org/10.1016/j.jclinane.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Donatelli F. Epidural anesthesia and analgesia decrease the postoperative incidence of insulin resistance in preoperative insulin-resistant subjects only. Anesth Analg. 2007;104:1587–93. doi: 10.1213/01.ane.0000261506.48816.5c. http://dx.doi.org/10.1213/01.ane.0000261506.48816.5c. [DOI] [PubMed] [Google Scholar]
- 9.Thanapal MR, Tata MD, Tan AJ, Subramaniam T, Tong JM, Palayan K, et al. Pre-emptive intraperitoneal local anaesthesia: an effective method in immediate post-operative pain management and metabolic stress response in laparoscopic appendicectomy, a randomized, double-blinded, placebo-controlled study. ANZ J Surg. 2014;84:47–51. doi: 10.1111/j.1445-2197.2012.06210.x. http://dx.doi.org/10.1111/j.1445-2197.2012.06210.x. [DOI] [PubMed] [Google Scholar]
- 10.Özütürk B, Ersoy A, Altan A, Uygur LM. Comparison of the effects of remifentanyl and dexmedetomidine infusions on haemodynamic parameters and thyroid hormones. Turk J Anaesth Reanim. 2013;41:206–10. doi: 10.5152/TJAR.2013.39. http://dx.doi.org/10.5152/TJAR.2013.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tutaş B, Tütüncü AÇ Ekici B, Altındaş F, Kaya G. Comparison of the effects of epidural and intrvenous analgesia on stress response in laparoscopic hiatal hernia surgery. Turk J Anaesth Reanim. 2012;40:144–53. http://dx.doi.org/10.5222/JTAICS.2012.144. [Google Scholar]
- 12.Bogdorf PJ, Ionescu TI, Houweling PL, Knape JT. Large-dose intrathecal sufentanil prevents the hormonal stress response during major abdominal surgery: a comparison with intravenous sufentanil in a prospective randomized trial. Anesth Analg. 2004;99:1114–20. doi: 10.1213/01.ANE.0000131728.68125.4E. http://dx.doi.org/10.1213/01.ANE.0000131728.68125.4E. [DOI] [PubMed] [Google Scholar]
- 13.Hall GM, Peerbhoy D, Shenkin A, Parker CJ, Salmon P. Hip and knee arthroplasty: a comparison and the endocrine, metabolic anti inflammatory responses. Clin Sci. 2000;98:71–9. http://dx.doi.org/10.1042/CS19990169. [PubMed] [Google Scholar]
- 14.Leopold SS, Casnellie MT, Warme WJ, Dougherty PJ, Wingo ST, Shott S. Endogenous cortisol production in response to knee arthroscopy and total knee arthroplasty. J Bone Joint Surg Am. 2003;85:2163–7. doi: 10.2106/00004623-200311000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Ljungqvist O, Soop M, Hedstrom M. Why metabolism matters in elective orthopedic surgery. A review. Acta Orthopedica. 2007;78:610–5. doi: 10.1080/17453670710014293. http://dx.doi.org/10.1080/17453670710014293. [DOI] [PubMed] [Google Scholar]
- 16.Bjornsson GL, Thorsteinsson L, Gudmundsson KO, Jonsson H, Jr, Gudmundsson S, Gudbjornsson B. Inflammatory cytokines in relation to adrenal response following total hip replacement. Scand J Immunol. 2007;65:99–105. doi: 10.1111/j.1365-3083.2006.01872.x. http://dx.doi.org/10.1111/j.1365-3083.2006.01872.x. [DOI] [PubMed] [Google Scholar]
- 17.Kılıçkan L, Toker K. The effects of preemptive intravenous versus preemptive epidural morphine on postoperative analgesia and surgical stress response after orthopaedic procedures. Minerva Anestesiol. 2000;66:649–55. [PubMed] [Google Scholar]
- 18.Aldrete JA. The post-anaesthesia recovery score revisited. J Clin Anaesth. 1995;7:89–91. doi: 10.1016/0952-8180(94)00001-k. http://dx.doi.org/10.1016/0952-8180(94)00001-K. [DOI] [PubMed] [Google Scholar]
- 19.Marana E, Annetta MG, Meo F, Parpaglioni R, Galeone M, Maussier ML, et al. Servoflurane improves the neuroendocrine stress response during laparoscopic pelvic surgery. Can J Anaesth. 2003;50:348–54. doi: 10.1007/BF03021031. http://dx.doi.org/10.1007/BF03021031. [DOI] [PubMed] [Google Scholar]
- 20.Sato H, Carvalho G, Sato T, Lattermann R, Matsukawa T, Schricker T. The association of preoperative glycemic control, intraoperative insulin sensitivity, and outcomes after cardiac surgery. J Clin Endocrinol Metab. 2010;95:4338–44. doi: 10.1210/jc.2010-0135. http://dx.doi.org/10.1210/jc.2010-0135. [DOI] [PubMed] [Google Scholar]
- 21.Ljunggren S, Hahn RG. Oral nutrition or water loading before hip replacement surgery; a randomized clinical trial. Trials. 2012;13:97. doi: 10.1186/1745-6215-13-97. http://dx.doi.org/10.1186/1745-6215-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams HA, Saatweber P, Schmitz CS, Hecker H. Postoperative pain management in orthopaedic patients: no differences in pain score, but improved stress control by epidural anaesthesia. Eur J Anaesthesiol. 2002;19:658–65. doi: 10.1017/s0265021502001084. http://dx.doi.org/10.1097/00003643-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Bayazit EG, Karaaslan K, Ozturan K, Serin E, Kocoglu H. Effect of epidural levobupivacaine and levobupivacaine with fentanyl on stres response and postoperative analgesia after total knee replacement. Int J Clin Pharmacol Ther. 2013;51:652–9. doi: 10.5414/CP201862. http://dx.doi.org/10.5414/CP201862. [DOI] [PubMed] [Google Scholar]
- 24.Al Oweidi AS, Klasen J, Al-Mustafa MM, Abu-Halaweh SA, Al-Zaben KR, Massad IM, et al. The impact of long-lasting preemptive epidural analgesia before total hip replacement on the hormonal stress response. A prospective, randomized, doubleblind study. Middle East J Anesthesiol. 2010;20:679–84. [PubMed] [Google Scholar]
- 25.Bagry H, de la Cuadra Fontaine JC, Asenjo JF, Bracco D, Carli F. Effect of a continuous peripheral nerve block on the inflammatory response in knee arthroplasty. Reg Anesth Pain Med. 2008;33:17–23. doi: 10.1016/j.rapm.2007.06.398. http://dx.doi.org/10.1016/j.rapm.2007.06.398. [DOI] [PubMed] [Google Scholar]
- 26.Binici Bedir E, Kurtulmuş T, Başyiğit S, Bakır U, Sağlam N, Saka G. A comparison of epidural analgesia and local infiltration analgesia methods in pain control following total knee arthroplasty. Acta Orthop Traumatol Turc. 2014;48:73–9. doi: 10.3944/AOTT.2014.3256. http://dx.doi.org/10.3944/AOTT.2014.3256. [DOI] [PubMed] [Google Scholar]
- 27.Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology. 2000;93:858–75. doi: 10.1097/00000542-200009000-00038. http://dx.doi.org/10.1097/00000542-200009000-00038. [DOI] [PubMed] [Google Scholar]