Abstract
The heterogeneity of spontaneous preterm birth (SPTB) requires an interdisciplinary approach to determine potential predictive risk factors of early delivery. The aim of this study was to investigate maternal whole blood gene expression profiles associated with spontaneous preterm birth (SPTB, <37 weeks) in asymptomatic pregnant women. The study population was a matched subgroup of women (51 SPTBs, 114 term delivery controls) who participated in the All Our Babies community based cohort in Calgary (n = 1878). Maternal blood at 17–23 (sampling time point 1, T1) and 27–33 weeks of gestation (T2) were collected. Total RNA was extracted and microarray was performed on 326 samples (165 women). Univariate analyses determined significant clinical factors and differential gene expression associated with SPTB. Thirteen genes were validated using qRT-PCR. Three multivariate logistic models were constructed to identify gene expression at T1 (Model A), T2 (Model B), and gene expression fold change from T1 to T2 (Model C) associated with SPTB. All models were adjusted for clinical factors. Model C can predict SPTB with 65% sensitivity and 88% specificity in asymptomatic women after adjusting for history of abortion and anaemia (occurring before T2). Clinical data enhanced the sensitivity of the Models to predict SPTB. In conclusion, clinical factors and whole blood gene expression are associated with SPTB in asymptomatic women. An effective screening tool for SPTB during pregnancy would enable targeted preventive approaches and personalised antenatal care.
Introduction
Preterm birth (PTB; birth before 37 weeks of gestation) is the greatest challenge facing contemporary obstetrics in both high and low resource settings. The World Health Organization estimated that 11% of all live births in 2010 were premature (15 million) and PTB rates are increasing [1]. Preterm related complications include death, lifelong sequelae including motor and sensory impairment [2] and immediate and long-term emotional and financial consequences for families, communities and the health care system [3, 4]. The prevention of PTB is essential for accelerating progress towards the United Nation’s Fourth Millennium Development Goal as the social and economic benefits of reducing the rate of PTB are enormous [5].
PTB is becoming a preventable disease. The use of progesterone [6–8], cervical cerclage [9] and antibiotics [10] in women at high risk of PTB are improving outcomes. However, these treatments are only useful in a subset of women [6–8]. The current screening tools to identify asymptomatic women at high risk of spontaneous PTB (SPTB) include clinical risk factor assessment [11], measuring cervical length [12, 13] and screening for fetal fibronectin (fFN) [14, 15]. These tools are limited by their low sensitivities (<50%), with some as low as 8% [11, 16]. The cornerstone of preventing PTB is to reliably identify these women and develop tools for risk stratification. This will assist the development and implementation of preventive measures as well as efforts to improve the clinical management of PTB. The multifactorial aetiologies and serious consequences of PTB highlight the need for a multidisciplinary approach to identify factors predictive of PTB [17].
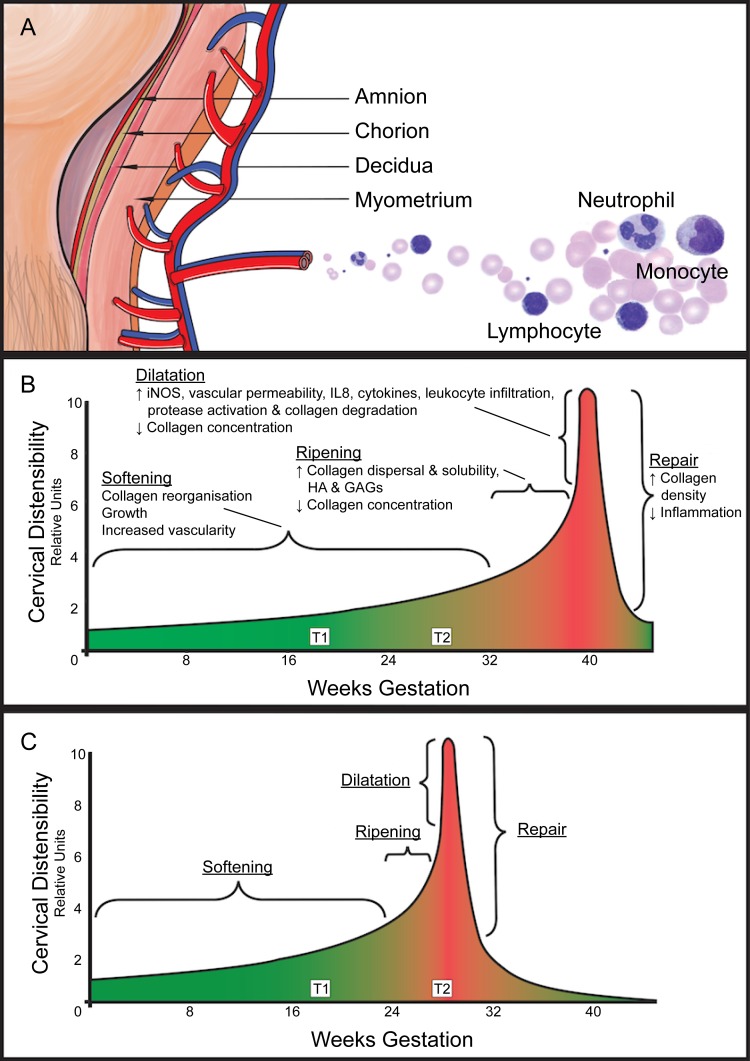
Parturition is a complex process that begins weeks before labour onset (Fig 1) [18, 19]. Labour is an inflammatory process with elevated levels of maternal circulating leukocytes [20] and increased leukocyte infiltration into the myometrium, decidua and cervix before and during labour [21, 22]. Whole blood mRNAs are assumed to be contributed, in part, by leukocytes and may reflect physiological processes. We postulate that maternal leukocytes circulating through gestational tissues (i.e. amnion, chorion, decidua, myometrium and cervix) during pregnancy are exposed to ‘signals’ from these tissues, and respond by altering their gene expression. An alternate postulate is that maternal leukocytes may be initiating and coordinating the process of parturition. This current study profiled whole blood mRNA collected from asymptomatic pregnant women and investigated the univariate association of whole blood gene expression at approximately 18 and 28 weeks of gestation with impending SPTB. Three multivariate models associated with SPTB were subsequently constructed using data at 18 weeks, 28 weeks, and from 18 to 28 weeks of gestation.
Fig 1. Parturition begins weeks before labour onset.
(A) Labour is an inflammatory process with elevated levels of maternal circulating leukocytes and increased leukocyte infiltration into the myometrium, decidua and cervix before and during labour. (B) Parturition is a long complex process that begins weeks before the onset of labour. The cervix gradually ripens and the myometrium switches from a quiescent to a contractile state. (C) In preterm birth, the cascade of events culminating in birth is transposed earlier in gestation. iNOS, induced nitric oxide synthase; IL8, interleukin 8; HA, hyaluronan; GAGs, glycosaminoglycans; T1, study samples collected at 17–23 weeks of gestation; T2, study samples collected at 27–33 weeks of gestation. Illustrations adapted from Word et al [18].
Materials and Methods
Patient Recruitment
The study population was drawn from a subset of women who participated in the All Our Babies (AOB) study, a community based longitudinal pregnancy cohort in Calgary, Alberta, Canada approved by the Conjoint Health Research Ethics Board, University of Calgary (Ethics #20821 and #22128). Pregnant women receiving prenatal viral serology testing were recruited through a partnership with Calgary Laboratory Service between May 2008 and December 2010. Written consent was obtained at the time of the first blood collection. Women also completed a survey about lifestyle, psychosocial and health care utilisation (prenatal care, social support, symptoms of stress, anxiety and depression, and breastfeeding) at <25 weeks, 34–36 weeks of gestation and 4 months postpartum [23].
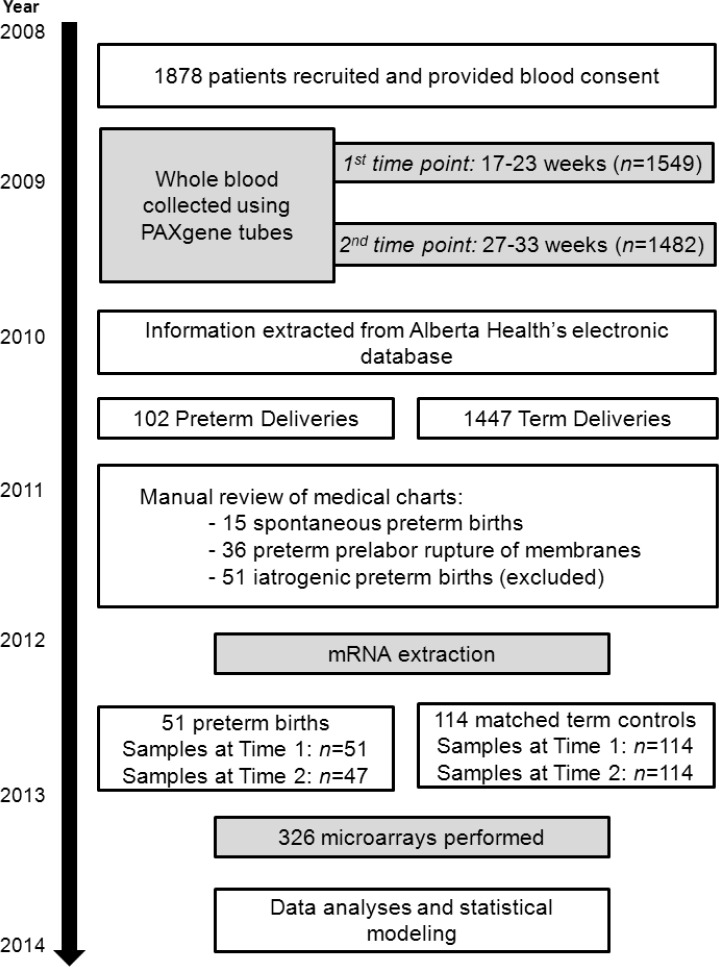
Detailed inclusion and exclusion criteria for the AOB study have been described [24]. Briefly, inclusion criteria were ≥18 years of age, gestation age <18 weeks at time of recruitment and singleton pregnancy. Exclusion criteria were multifetal pregnancy and pre-existing medical conditions (diabetes, high blood pressure, autoimmune disorders, kidney disease, cardiovascular disease or chronic infection). Clinical and antenatal records were extracted from the Alberta Health electronic database. Women who had PTB were confirmed by a manual review of the medical charts. Clinical data were unavailable for four women who delivered out of province at term. Fig 2 summarises the patient recruitment, patient phenotyping and selection process.
Fig 2. Flowchart outlining the recruitment, patient phenotyping and sample selection process for this study.
Spontaneous preterm labour (SPTL) is defined as spontaneous onset of labour ≤37 weeks of gestation resulting in preterm delivery. Preterm prelabour rupture of membranes (PPROM) is defined as spontaneous rupture of membranes at <37 weeks without labour, onset of spontaneous labour occurred at least 60 min after PPROM and subsequent preterm delivery. Term delivery is birth at ≥37 weeks of gestation irrespective of spontaneous onset or induction, vaginal delivery or caesarean section. In Calgary, anaemia is defined as <120 g/L of haemoglobin; oligohydramnios and polyhydramnios are diagnosed using an amniotic fluid index of <5 cm and >20 cm, respectively. Antepartum haemorrhage is defined as recurrent haemorrhage at ≤20 or >20 weeks of gestation. Urinary tract infection (UTI) was indicated positive by either microscopic or macroscopic urinalysis, or culture. Demographic, clinical, labour and delivery variables were analysed using one-way ANOVA, Student’s t-test, Chi-squared test or Fisher’s exact test (R, version 3.2.1).
Sample Collection and Processing
Maternal blood samples were collected at 17–23 (time point 1, T1) and 27–33 weeks of gestation (time point 2, T2) into four PAXgene blood RNA tubes (PreAnalytix/BD Canada, Mississauga, ON, Canada) and stored at -80°C until analysis.
RNA Extraction, Quality Check and Microarray
Total RNA was extracted using the PAXgene blood RNA Kit (PreAnalytix/QIAGEN, Toronto, ON, Canada) adhering to the manufacturer’s protocol. All samples had RNA integrity number of >7 (RNA 6000 Nano Kit and Agilent 2100 BioAnalyzer; Agilent Technologies, Santa Clara, CA) and were hybridised to Affymetrix Human Gene 2.1 ST (Affymetrix, Santa Clara, CA). Microarray was performed by The Centre for Applied Genomics (TCAG; The Hospital for Sick Children, Toronto, ON, Canada). Data were deposited into the National Center for Biotechnology Information Gene Expression Omnibus (accession number: GSE59491; https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE59491).
Differential Gene Expression Analyses
Microarray CEL files were normalised using Robust Multi-array Average (Bioconductor, R) [25], probes were annotated using Custom (Gene)Chip Definition Files for Entrez Gene (version 18) [26], gene expression lower than the 25th percentile were removed, and differential gene expression was analysed using limma [27] with multiple hypothesis testing (false discovery rate, FDR). limma analyses were adjusted for gestational age at sampling, significant demographic or clinical variables when appropriate (see S1 Text). Differential gene expression was initially performed between SPTL and PPROM at T1 or T2 to determine if any gene was differentially expressed between these two subtypes of SPTB. There was no differentially expressed gene between SPTL and PPROM, thus, SPTL and PPROM were combined into a SPTB group for all subsequent analyses. Five limma analyses were conducted. The first two limma analyses determined genes differentially expressed between women who had SPTBs and term deliveries at (1) T1 or (2) T2.
Investigating the temporal gene expression from T1 to T2 provides information about the progression of pregnancies that result in normal term deliveries or SPTBs. Hence, the third and fourth limma analyses were performed to identify genes displaying temporal changes from T1 to T2 within women who had (3) SPTB or (4) term deliveries. The fifth analysis was conducted to identify (5) genes whose expression fold change from T1 to T2 were different between SPTBs and term deliveries. Genes with FDR<0.05 were selected for qRT-PCR validation.
Gene Set Enrichment
Pre-ranked Gene Set Enrichment Analyses [28] was utilised to determine significantly enriched gene sets/pathways (Gene Ontology Biological Processes, Reactome, KEGG and BioCarta, versions 5.1) between women who had SPTBs and term deliveries at (1) T1 or (2) T2; gene sets associated with temporal changes within women who had (3) SPTBs or (4) term deliveries, and (5) gene sets that reflect the difference in gene expression fold change between SPTB and term delivery.
Qualitative Real Time PCR
Genes (limma FDR<0.05) that displayed >25% increase or >15% decrease, and CEL files with arbitrary intensity expression values of at least four were selected for qRT-PCR validation [29–31]. Primers were designed using Primer BLAST; pooled cDNA (paired samples from six women) were used to determine primer specificity and efficiency; and primer efficiencies (90%-105%) were determined using five-point standard curves. qRT-PCR was carried out in quadruplicate and quantification cycle (Cq) of all genes were <32. Gene expression was analysed using the 2(-Delta Delta Ct) method. Using CFX Manager 3.1 (BIO-RAD, Hercules, CA), qRT-PCR expression data were corrected for primer efficiencies and normalised to the geometric mean Cq of three optimised housekeeping genes (TBP, SDHA and YWHAZ [31]; average expression stability was M<0.5 [32]) to obtain the first Delta Ct. Wilcoxon test was used to compare the relative gene expression between paired samples (second Delta Ct). Correlation between microarray and qRT-PCR was performed using Spearman’s rho.
Multivariate Models Associated with Spontaneous Preterm Birth
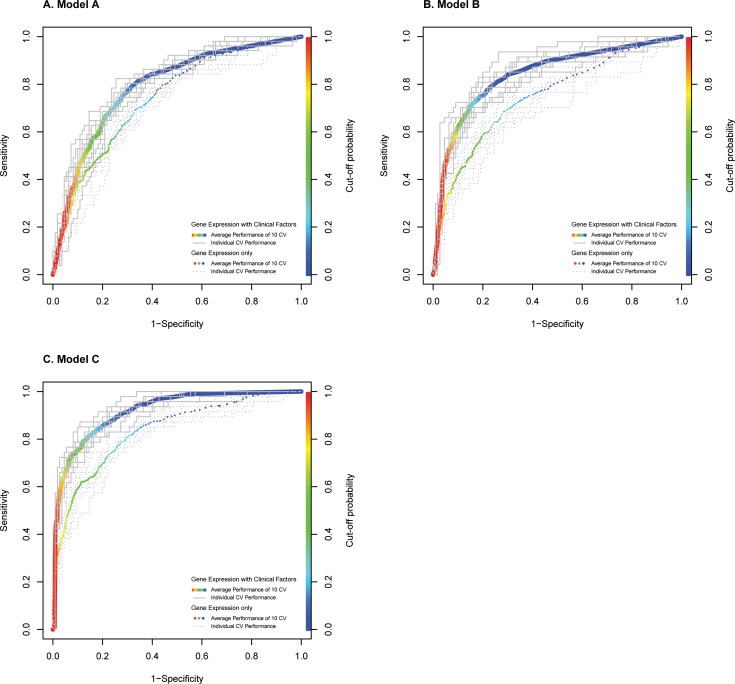
Three multivariate models were constructed to identify gene expression at T1 (Model A), T2 (Model B), and gene expression fold change from T1 to T2 (Model C) associated with SPTB (Statistical Analysis System, version 9.3, SAS Institute Inc, Cary, NC). Clinical factors occurring before T1 or T2 that were significant in univariate analyses were entered into separate clinical factor multivariate logistic regression analyses. Clinical factors occurring before T1 that remained significant in the multivariate clinical factor analysis were adjusted for in Model A; and significant clinical factors occurring before T2 in the multivariate clinical factor analysis were included for Models B and C. Gestational age were also accounted for in the Models (S1 Text). To assess validity, each Model was subjected to ten five-fold cross-validation with gene selection occurring at every fold. To evaluate the importance and effect of adjusting gene expression with clinical factors, models were also built without clinical factors (i.e. using gene expression only; S1 Text). The probability cut-off was 0.5, predictive performances such as area under receiver operator characteristic curve (ROC AUC) are the average of ten cross-validation runs. ROC AUCs were graphed using ROCR, R [33].
Results
After excluding iatrogenic PTB, there were 51 SPTB cases where 10 were extreme SPTB (<32 weeks) and four delivered before T2. The average time from PPROM until labour onset was 27.7 hours. Power calculations indicated that a control group of at least 85 term women was required to match 51 SPTB, with an effect size of 0.5, significance level of 0.05 and power of 0.8. Term delivery controls (n = 114, power = 0.84) were matched to SPTB cases drawn from baseline survey at <25 weeks of gestation by parity (no previous birth/at least one previous birth), maternal age (<35 years versus ≥35 years), pre-pregnancy body mass index (<18.5 kg/m2, 18.5–24.9 kg/m2, 25–29.9 kg/m2, ≥30 kg/m2), ethnicity (Caucasian versus non-Caucasian), and pre-pregnancy smoking status (yes/no). A total of 326 microarrays (165 women) were performed. Eleven clinical variables were significantly associated with SPTB (Table 1).
Table 1. Demographic, clinical, labour and delivery characteristics of the 165 participants.
| Spontaneous Preterm Birth (SPTB) | Term Birth | SPTL vs PPROM vs Term | SPTB vs Term | |||
|---|---|---|---|---|---|---|
| SPTL | PPROM | SPTL and PPROM | p-value | p-value | ||
| Patient Demographics | ||||||
| Women, n | 15 | 36 | 51 | 114 | ||
| Maternal age, mean years±SD | 31.1±4.9 | 31.3±4.6 | 31.2±4.7 | 31.1±4.7 | 0.910 | 0.850 |
| Pre-pregnancy BMI, mean±SD | 21.9±2.8 | 26.6±9.1 | 25.3±8.0 | 25.8±72 | 0.321 | 0.702 |
| Ethnicity | 0.559 | 0.946 | ||||
| Caucasian, n (%) | 10 | 29 | 39 (76.5) | 85 (74.6) | ||
| Non-Caucasian, n (%) | 5 | 7 | 12 (23.5) | 29 (25.4) | ||
| Smoking during pregnancy | 0.379 | 0.367 | ||||
| Yes, n (%) | 2 | 8 | 10 (19.6) | 14 (12.7) | ||
| No, n (%) | 13 | 28 | 41 (80.4) | 96 (87.3) | ||
| Consumption of alcohol during pregnancy | 0.021 | 0.038 | ||||
| Yes, n (%) | 3 | 4 | 7 (13.7) | 4 (3.6) | ||
| No, n (%) | 12 | 32 | 44 (86.3) | 106 (96.4) | ||
| Clinical Characteristics | ||||||
| Gravidity, mean±SD | 2.7±1.7 | 2.0±1.3 | 2.2±1.4 | 2.0±1.2 | 0.109 | 0.410 |
| Parity | 0.480 | 0.984 | ||||
| Nulliparous, n (%) | 6 | 21 | 27 (52.9) | 60 (54.5) | ||
| Multiparous, n (%) | 9 | 15 | 24 (47.1) | 50 (45.5) | ||
| History of previous PTB | 0.001 | 0.001 | ||||
| Previous PTB, n (%) | 4 | 7 | 11 (21.6) | 4 (3.6) | ||
| No previous PTB, n (%) | 11 | 29 | 40 (78.4) | 106 (96.4) | ||
| History of abortion | 0.002 | 0.001 | ||||
| At least one abortion, n (%) | 5 | 9 | 14 (27.5) | 8 (7.3) | ||
| No previous abortion, n (%) | 10 | 27 | 37 (72.5) | 102 (92.7) | ||
| Mode of conception | 0.188 | 0.267 | ||||
| Spontaneous conception, n (%) | 13 | 34 | 47 (92.2) | 106 (96.4) | ||
| Assisted reproductive technologies, n (%) | 2 | 2 | 4 (7.8) | 4 (3.6) | ||
| Oligohydramnios | 0.800 | 1.00 | ||||
| Present, n (%) | 0 | 2 | 2 (3.9) | 4 (3.6) | ||
| Absent, n (%) | 15 | 34 | 49 (96.1) | 106 (96.4) | ||
| Polyhydramnios | 0.002 | 0.094 | ||||
| Present, n (%) | 3 | 0 | 3 (5.9) | 1 (0.9) | ||
| Absent, n (%) | 12 | 36 | 48 (94.1) | 109 (99.1) | ||
| Gestational diabetes during pregnancy | 0.216 | 0.350 | ||||
| Present, n (%) | 2 | 3 | 5 (9.8) | 5 (4.5) | ||
| Absent, n (%) | 13 | 33 | 46 (90.2) | 105 (95.5) | ||
| Antepartum haemorrhage during pregnancy | 0.004 | 0.009 | ||||
| ≥1 episode of bleeding, n (%) | 7 | 9 | 16 (31.4) | 14 (12.7) | ||
| None, n (%) | 8 | 27 | 35 (68.6) | 96 (87.3) | ||
| Antepartum haemorrhage <20 weeks of gestation (i.e. threatened miscarriage) | 0.419 | 0.353 | ||||
| ≥1 episode, n (%) | 3 | 6 | 9 (17.6) | 12 (10.9) | ||
| None, n (%) | 12 | 30 | 42 (82.4) | 98 (89.1) | ||
| Antepartum haemorrhage >20 weeks of gestation | 0.021 | 0.262 | ||||
| ≥1 episode, n (%) | 6 | 4 | 10 (21.3) | 14 (12.7) | ||
| None, n (%) | 8 | 29 | 37 (78.7) | 96 (87.3) | ||
| Urinary tract infection during pregnancy | <0.001 | 0.001 | ||||
| Present, n (%) | 4 | 3 | 7 (14.0) | 1 (0.9) | ||
| Absent, n (%) | 11 | 32 | 43 (86.0) | 109 (99.1) | ||
| Urinary tract infection before first study sample | 0.029 | 0.029 | ||||
| Present, n (%) | 1 | 2 | 3 (6.0) | 0 (0.0) | ||
| Absent, n (%) | 14 | 33 | 47 (94.0) | 110 (100.0) | ||
| Urinary tract infection before second study sample | <0.001 | 0.003 | ||||
| Present, n (%) | 3 | 2 | 5 (10.0) | 0 (0.0) | ||
| Absent, n (%) | 12 | 33 | 45 (90.0) | 110 (100.0) | ||
| Anaemia during pregnancy | <0.001 | <0.001 | ||||
| Anaemic, n (%) | 4 | 8 | 12 (23.5) | 3 (2.7) | ||
| Non-anaemic, n (%) | 11 | 28 | 39 (76.5) | 107 (97.3) | ||
| Anaemia before first study sample | 0.099 | 0.099 | ||||
| Present, n (%) | 0 | 2 | 2 (3.9) | 0 (0.0) | ||
| Absent, n (%) | 15 | 34 | 49 (96.1) | 110 (100.0) | ||
| Anaemia before second study sample | <0.001 | <0.001 | ||||
| Present, n (%) | 4 | 8 | 12 (23.5) | 1 (0.9) | ||
| Absent, n (%) | 11 | 28 | 39 (76.5) | 109 (99.1) | ||
| Group B Streptococcus in vaginal tract (>36 weeks of gestation) | 0.071 | 0.043 | ||||
| Present, n (%) | 2 | 2 | 4 (7.8) | 24 (21.8) | ||
| Absent, n (%) | 13 | 34 | 47 (92.2) | 86 (78.2) | ||
| Placenta Praevia | 0.143 | 0.327 | ||||
| Present, n (%) | 0 | 3 | 3 (5.9) | 2 (1.8) | ||
| Absent, n (%) | 15 | 33 | 48 (94.1) | 108 (98.2) | ||
| Labour and Delivery Characteristics | ||||||
| Abruptio Placentae | 0.004 | 0.004 | ||||
| Yes, n (%) | 1 | 5 | 6 (11.8) | 1 (0.9) | ||
| No, n (%) | 14 | 31 | 45 (88.2) | 109 (99.1) | ||
| Chorioamnionitis | 0.004 | 0.004 | ||||
| Yes, n (%) | 1 | 5 | 6 (11.8) | 1 (0.9) | ||
| No, n (%) | 14 | 31 | 45 (88.2) | 109 (99.1) | ||
| Gestational age at delivery, mean weeks±SD | 33.5±2.6 | 33.6±2.6 | 33.6±2.6 | 39.2±1.2 | <0.001 | <0.001 |
| Birth weight, mean grams±SD | 2257±551 | 2363±618 | 2332±596 | 3384±473 | <0.001 | <0.001 |
| Neonatal Gender | 0.683 | 0.601 | ||||
| Male, n (%) | 8 | 22 | 30 (58.8) | 71 (64.5) | ||
| Female, n (%) | 7 | 14 | 21 (41.2) | 39 (35.5) | ||
Spontaneous preterm labour (SPTL); preterm prelabour rupture of membranes (PPROM); for continuous variables, one-way ANOVA or Student’s t-test was used for comparison; for categorical variables, Chi-squared test or Fisher’s test (when category size ≤4) was used.
Differential Gene Analysis using limma
There was no differentially expressed gene at FDR<0.05 but at FDR<0.10, there were 0 and 26 differentially expressed genes between women who had SPTB and term delivery at T1 and T2, respectively. There were 234 and 2329 genes that displayed significant temporal differences within women who had SPTBs or term deliveries, respectively (FDR<0.05). There was no gene whose expression fold change was significantly different between SPTB and term delivery. All differential gene expression data are in S1 Table.
Gene Set Enrichment
Significantly enriched gene sets are in S2 Table (FDR <0.05). At both sampling time points, gene sets and pathways associated with inflammation were upregulated in women with SPTBs compared to women who had term deliveries (n = 37 upregulated gene sets at T1, n = 103 at T2; 22 common gene sets). These inflammatory pathways include leukocyte migration, lysosomes, NF-kB activation, pathways involving cytokines and their receptors (e.g. IL1, IL2, IL6, IFN, IL1R, TNFR2, CCR3, CXCR4 and CD40) as well as toll-like and NOD-like receptor signalling. In contrast, women with SPTBs had lower RNA metabolism, RNA processing and T cell activation (including CTLA4 pathway) compared to women who had term deliveries (n = 163 downregulated gene sets at T1, n = 100 at T2; 77 common gene sets).
As pregnancy progressed from T1 to T2, women who had SPTBs demonstrated increased cellular proliferation, cell migration signalling pathway (by L1) and extracellular matrix degradation involving lysosomes (n = 32 upregulated gene sets), and decreased cellular transcription (n = 1 downregulated gene set). In women with term deliveries, there was increased signalling for cell migration, haemostasis, apoptosis and immune response (n = 114 upregulated gene sets); while there was decreased lymphocyte activation and NCAM cell adhesive interactions as pregnancy progressed to T2 (n = 36 downregulated gene sets). When investigating whether any gene set was enriched for genes whose expression fold change were different between SPTBs and term deliveries, there was no up-regulated gene set but “membrane fusion” (n = 1) was significantly down-regulated in SPTB.
qRT-PCR Validation
Validation was performed on 192 samples randomly chosen from 48 women who had term deliveries (96 paired-samples) and 50 SPTBs (92 paired-samples, 4 single samples at T1). This resulted in using two 384-well plates to screen for each gene of interest. Genes which had significant temporal expression within women who had SPTBs or term deliveries were subjected to validation (S3 Table). Thirteen unique genes were successfully validated using qRT-PCR (p<0.05, Wilcoxon test). There was a significant correlation between microarray and qRT-PCR data (Spearman’s rho = 0.934, p<0.001).
Multivariate Models Associated with Spontaneous Preterm Birth
Clinical Factors
Significant clinical variables determined after delivery (placental abruption, chorioamnionitis, gestational age at delivery and birth weight), during late gestation (Group B streptococcus) or those that did not achieve significance before T2 were not considered. Significant clinical factors with events occurring before T1 were alcohol consumption, history of PTB, history of abortion and UTI before T1. History of PTB (p = 0.0024) and history of abortion (p = 0.0025) remained significant in the clinical factor multivariate analysis and were adjusted for in Model A. Alcohol consumption, history of PTB, history of abortion, UTI before T2 and anaemia before T2 were significant clinical factors with events occurring before T2; history of abortion (p = 0.0002) and anaemia before T2 (p = 0.0003) remained significant in the clinical factor multivariate analysis and were included in Models B and C.
Multivariate Gene Expression Models
After adjusting for gestational age and clinical factors, candidate genes were incorporated into multivariate logistic regressions (stepwise selection) to build Models A, B and C (Table 2). As the prevalence of SPTB in this study was 31% (51 SPTB out of 165 total deliveries; higher than the average PTB rate of 10%), positive and negative predictive values, and false positive and negative rates must be interpreted with caution as these values are dependent on the prevalence of the disease, i.e. PTB in the study population, whilst sensitivity, specificity and ROC AUC are prevalence independent.
Table 2. Multivariate models (Models A, B and C) associated with spontaneous preterm birth (SPTB) at 17–23 (T1) and 27–33 (T2) weeks of gestation.
| Average of ten five-fold cross validations (cut-off = 0.5) | ||||||||
|---|---|---|---|---|---|---|---|---|
| ROC AUC | Sensitivity (%) | Specificity (%) | Positive Predictive Value* (%) | Negative Predictive Value* (%) | False Positive Rate* (%) | False Negative Rate* (%) | ||
| SPTB models with gene expression and significant clinical factors included | ||||||||
| A | ZNF605, LRRC41, PCDHGA12, ABT1, THBS3, VNN1, history of PTB and history of abortion | 0.780 | 52.4 | 84.3 | 61.0 | 79.2 | 15.7 | 47.6 |
| B | LOC100128908, CST13P, EEF1D, RPH3A, TRBV6-6, PLEC, MIR601, ZNF16, history of abortion and anaemia | 0.838 | 62.3 | 87.3 | 67.8 | 84.5 | 12.7 | 37.7 |
| C | LOC100128908, MIR3691, LOC101927441, CST13P, ACAP2, ZNF324, SH3PXD2B, TBX21, history of abortion and anaemia | 0.841 | 64.7 | 88.3 | 70.1 | 85.4 | 11.7 | 35.3 |
| SPTB models with gene expression only | ||||||||
| A | - | 0.703 | 44.3 | 81.5 | 52.5 | 76.0 | 18.5 | 55.7 |
| B | - | 0.748 | 46.2 | 86.5 | 59.6 | 79.0 | 13.5 | 53.8 |
| C | - | 0.758 | 52.6 | 84.3 | 58.7 | 80.7 | 15.7 | 47.4 |
Area under receiver operator curve (ROC AUC)
*As the prevalence of SPTB in this study was 31% (51 SPTB and 114 term deliveries), positive predictive value, negative predictive value, false positive rate and false negative rate must be interpreted with caution as they are dependent on the prevalence of the disease, i.e. PTB in the study population, whilst sensitivity, specificity and ROC AUC are prevalence independent.
The ROC AUCs of Models A, B and C with clinical factors were 11.0%, 12.0% and 10.9% higher than the ROC AUCs of their corresponding Models without clinical factors (Fig 3). This resulted in 18.3%, 34.8% and 23.0% increased sensitivity, and 3.4%, 0.9% and 4.7% increased specificity in Models A, B and C with clinical factors, respectively, when compared to Models without clinical factors. Models B and C were more sensitive than Model A (62.3% and 64.7% versus 52.4%), most likely due to the shorter time frame from sampling at T2 to SPTB (average of 4.7 weeks after T2).
Fig 3.
The area under receiver operator characteristic curves of Models A, B and C after ten five-fold cross-validation (CV) runs. These three multivariate models were constructed to identify gene expression associated with spontaneous preterm birth (SPTB) at 17–23 weeks (A; Model A) and 27–33 weeks (B; Model B); and gene expression fold change from 17–23 to 27–33 weeks of gestation associated with SPTB (C; Model C). Models with clinical factors are represented using solid lines; Models without clinical factors are represented using dotted lines. The rainbow bar on the right of each plot displays cut-off probabilities. The colour of the points along the average CV curve reflects its respective cut-off probability to obtain the desired sensitivity and specificity.
Discussion
This study profiled pregnant whole blood mRNA and investigated the association of whole blood gene expression with impending SPTB in asymptomatic women at two clinically relevant time points. T1 generally corresponds to when fetal anatomy ultrasound scan is performed and T2 is when blood is collected for gestational diabetes screening. This large, paired and unique dataset also provide glimpses of pregnancy progression that result in either SPTB or term delivery. The eleven clinical variables significantly associated with SPTB agree with previous reports [13, 34–39]. Although the association of inflammation with the general physiology of labour at term or preterm gestation is well documented [22, 31, 40, 41], our paired data and gene set enrichment analyses show for the first time, that inflammation is consistently elevated at 17–23 and 27–33 weeks of gestation in the blood of asymptomatic women who had SPTBs compared to women with term deliveries. Lastly, the integration of clinical data alongside gene expression enhanced the sensitivity of our models to predict SPTB.
Gene set analyses provide biological knowledge of how genes interact and orchestrate pathways. Despite not observing any significant gene at FDR<0.05, numerous gene sets were significantly associated with SPTB. We hypothesized that circulating maternal leukocytes pick up ‘signals’ from gestational tissues and respond by altering their gene expression. The most striking gene set enrichment result was that women who had SPTBs have increased interleukin signalling, mainly driven by IL1 and IL6, and leukocyte migration into gestational tissues as early as 18 weeks compared to women who had term deliveries. The early migration of leukocytes into the cervix may accelerate its ripening process and lead to SPTB (Fig 1C) [18, 42]. The increased signalling of IL1 and IL6 can also contribute to SPTB by increasing oxytocin and prostaglandin production leading to accelerated cervical ripening [43–45], early myometrial contractions [46–48] and premature fetal membranes rupture [49, 50].
Our AOB cohort is representative of the pregnant population in urban centres across Canada [23, 51]. The SPTB rate in the state of Alberta is 6.2% [52]. We expected about 110 SPTBs from 1878 AOB participants, but only 51 SPTBs were identified after manual chart review. Thus, our AOB population was not enriched with women at high risk of SPTB. Nevertheless, the predictive models developed in our AOB cohort may offer unique possibilities for research, clinical care and resource utilization. The key to preventing SPTB is the early identification of asymptomatic women at increased risk. The ability to identify these women can aid study groups to focus on high risk women and avoid unnecessary (and expensive) research on those destined for term delivery when evaluating new interventions to prevent PTB. The development of a SPTB predictive tool will also allow further refinement of the subsets of women who will benefit from the existing preventive strategies of progesterone therapy [8, 53], cervical cerclage [54, 55] or pessary [56].
Many research studies have investigated tools to identify high-risk asymptomatic women. For example, the absence of fFN in the cervicovaginal fluid is a classic negative predictor of PTB [14, 15], especially for symptomatic women [57]. Dekker et al. reported average predictive capacity for SPTB and PPROM using clinical risk factors, cervical length and uterine artery Doppler ultrasound measurements at 19–21 weeks of gestation [11]. They also reported a minimal overlap of risk factors for SPTB and PPROM, highlighting the heterogeneous condition of PTB. We attempted but were unable to separately assess SPTL and PPROM due to small sample sizes. Kuhrt et al. recently developed a validated tool comprising of cervical length, fFN, history of SPTB/PPROM to predict high-risk asymptomatic women with ROC AUCs ranging from 0.77 to 0.99, sensitivity between 54.5% and75.0%, and specificity between 63.5% and 97.7% [13]. The performances of our Models B and C are comparable to Kuhrt et al. In addition, it might be more advantageous to screen for biomarkers in maternal blood as blood is easily accessible, minimally invasive and can be collected in most women as part of standard antenatal care [31, 58]. This is in contrast to fFN screening where the test is limited to a subset of eligible women, e.g. had no prior vaginal/cervical examination, unprotected sexual intercourse and/or antepartum haemorrhage.
Models B and C are promising SPTB screening tools since most PTBs occur after 28 weeks of gestation [59]. The slight difference in predictive efficacies between Models B and C, and the simplicity of obtaining one sample at T2 makes Model B more clinically applicable. It is important to note that although the predictive efficacies for our Models were reported using a 0.5 cut-off (Table 2), cut-off probability thresholds can be tailored for clinical use, e.g. a higher sensitivity test is required to predict SPTB (Fig 3). Collectively, given the multiple aetiologies of SPTB, a set of diagnostic markers including biochemical, clinical variables, cervical length as well as whole blood gene expression may improve SPTB prediction in asymptomatic women in the future.
In conclusion, this current work has shown that clinical factors and whole blood gene expression are associated with SPTB in asymptomatic women. Gene set enrichment analyses revealed elevated inflammation in women who had SPTBs. Our study did not assess fFN or cervical length data as they were not routinely collected. More studies are needed in other populations to validate our Models and compare them with fFN and/or cervical length. Additional factors such as psychosocial (e.g. prenatal stress and anxiety) can also be included. The ability to implement an effective screening test during antenatal care for SPTB would enable strategic and personalised antenatal care, to improve outcomes for infants and families.
Supporting Information
(XLSX)
(XLSX)
(DOC)
(DOCX)
Acknowledgments
The authors acknowledge the contribution and support of AOB team members and our participants. The authors also acknowledge Heather Kehler, MSc and Sara Gracie, MSc for their contribution to the overall implementation of the AOB protocol, including data collection, management and community communications (University of Calgary); Dr Sally Yoo-Bolstad, PhD and Dr Liz King, PhD for sample processing (University of Calgary); Dr Chao Lu, PhD and Lan He, MSc (TCAG) for their services with the Agilent BioAnalyzer and Affymetrix microarrays.
Data Availability
Data were deposited into the National Center for Biotechnology Information Gene Expression Omnibus (accession number: GSE59491).
Funding Statement
This work was supported by Alberta Innovates Health Solutions (Interdisciplinary Team Grant #200700595) and Global Alliance to Prevent Prematurity and Stillbirth (GAPPS award #12006). YJH was supported by a Canadian Institutes of Health Fellowship. Calgary Laboratory Services provided support in the form of salary for LdK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born too soon: the global epidemiology of 15 million preterm births. Reproductive health. 2013;10 Suppl 1:S2 10.1186/1742-4755-10-S1-S2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johansson AM, Domellof E, Ronnqvist L. Long-term influences of a preterm birth on movement organization and side specialization in children at 4–8 years of age. Dev Psychobiol. 2014. [DOI] [PubMed] [Google Scholar]
- 3.Treyvaud K, Lee KJ, Doyle LW, Anderson PJ. Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr. 2014;164(3):515–21. 10.1016/j.jpeds.2013.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Preterm birth. Causes, consequences, and prevention Behrman RE, Butler AS, editors. Washington DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 5.Howson CP, Kinney MV, McDougall L, Lawn JE. Born too soon: preterm birth matters. Reproductive health. 2013;10 Suppl 1:S1 10.1186/1742-4755-10-S1-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–9. [DOI] [PubMed] [Google Scholar]
- 7.DeFranco EA, O'Brien JM, Adair CD, Lewis DF, Hall DR, Fusey S, et al. Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):697–705. [DOI] [PubMed] [Google Scholar]
- 8.Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, Moawad AH, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–85. [DOI] [PubMed] [Google Scholar]
- 9.Alfirevic Z, Owen J, Carreras Moratonas E, Sharp AN, Szychowski JM, Goya M. Vaginal progesterone, cerclage or cervical pessary for preventing preterm birth in asymptomatic singleton pregnant women with a history of preterm birth and a sonographic short cervix. Ultrasound Obstet Gynecol. 2013;41(2):146–51. 10.1002/uog.12300 [DOI] [PubMed] [Google Scholar]
- 10.Hutzal CE, Boyle EM, Kenyon SL, Nash JV, Winsor S, Taylor DJ, et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a metaanalysis. Am J Obstet Gynecol. 2008;199(6):620 e1-8. 10.1016/j.ajog.2008.07.008 [DOI] [PubMed] [Google Scholar]
- 11.Dekker GA, Lee SY, North RA, McCowan LM, Simpson NA, Roberts CT. Risk factors for preterm birth in an international prospective cohort of nulliparous women. PLoS One. 2012;7(7):e39154 10.1371/journal.pone.0039154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Care AG, Sharp AN, Lane S, Roberts D, Watkins L, Alfirevic Z. Predicting preterm birth in women with previous preterm birth and cervical length >/ = 25 mm. Ultrasound Obstet Gynecol. 2014;43(6):681–6. 10.1002/uog.13241 [DOI] [PubMed] [Google Scholar]
- 13.Kuhrt K, Smout E, Hezelgrave N, Seed PT, Carter J, Shennan AH. Development and validation of a tool incorporating cervical length and quantitative fetal fibronectin to predict spontaneous preterm birth in asymptomatic high-risk women. Ultrasound Obstet Gynecol. 2016;47(1):104–9. 10.1002/uog.14865 [DOI] [PubMed] [Google Scholar]
- 14.Duhig KE, Chandiramani M, Seed PT, Briley AL, Kenyon AP, Shennan AH. Fetal fibronectin as a predictor of spontaneous preterm labour in asymptomatic women with a cervical cerclage. BJOG. 2009;116(6):799–803. 10.1111/j.1471-0528.2009.02137.x [DOI] [PubMed] [Google Scholar]
- 15.Abbott DS, Hezelgrave NL, Seed PT, Norman JE, David AL, Bennett PR, et al. Quantitative fetal fibronectin to predict preterm birth in asymptomatic women at high risk. Obstetrics and gynecology. 2015;125(5):1168–76. 10.1097/AOG.0000000000000754 [DOI] [PubMed] [Google Scholar]
- 16.Menon R, Torloni MR, Voltolini C, Torricelli M, Merialdi M, Betran AP, et al. Biomarkers of spontaneous preterm birth: an overview of the literature in the last four decades. Reprod Sci. 2011;18(11):1046–70. 10.1177/1933719111415548 [DOI] [PubMed] [Google Scholar]
- 17.Pennell CE, Jacobsson B, Williams SM, Buus RM, Muglia LJ, Dolan SM, et al. Genetic epidemiologic studies of preterm birth: guidelines for research. Am J Obstet Gynecol. 2007;196(2):107–18. [DOI] [PubMed] [Google Scholar]
- 18.Word RA, Li XH, Hnat M, Carrick K. Dynamics of cervical remodeling during pregnancy and parturition: mechanisms and current concepts. Semin Reprod Med. 2007;25(1):69–79. [DOI] [PubMed] [Google Scholar]
- 19.Heng YJ, Liong S, Permezel M, Rice GE, Di Quinzio MKW, Georgiou HM. Human cervicovaginal fluid biomarkers to predict term and preterm labour. Frontiers in Physiology. 2015;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuan M, Jordan F, McInnes IB, Harnett MM, Norman JE. Leukocytes are primed in peripheral blood for activation during term and preterm labour. Molecular human reproduction. 2009;15(11):713–24. 10.1093/molehr/gap054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osman I, Young A, Ledingham M, Thomson AJ, Jordan F, Greer IA, et al. Leukocyte density and pro-inflammatory cytokine expression in human fetal membranes, decidua, cervix and myometrium before and during labour at term. Mol Hum Reprod. 2003;9(1):41–5. [DOI] [PubMed] [Google Scholar]
- 22.Thomson AJ, Telfer JF, Young A, Campbell S, Stewart CJ, Cameron IT, et al. Leukocytes infiltrate the myometrium during human parturition: further evidence that labour is an inflammatory process. Hum Reprod. 1999;14(1):229–36. [PubMed] [Google Scholar]
- 23.McDonald SW, Lyon AW, Benzies KM, McNeil DA, Lye SJ, Dolan SM, et al. The All Our Babies pregnancy cohort: design, methods, and participant characteristics. BMC pregnancy and childbirth. 2013;13 Suppl 1:S2 10.1186/1471-2393-13-S1-S2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gracie SK, Lyon AW, Kehler HL, Pennell CE, Dolan SM, McNeil DA, et al. All Our Babies Cohort Study: recruitment of a cohort to predict women at risk of preterm birth through the examination of gene expression profiles and the environment. BMC pregnancy and childbirth. 2010;10:87 10.1186/1471-2393-10-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irizarry RA, Hobbs B, Collin F, Beazer-Barclay YD, Antonellis KJ, Scherf U, et al. Exploration, normalization, and summaries of high density oligonucleotide array probe level data. Biostatistics. 2003;4(2):249–64. [DOI] [PubMed] [Google Scholar]
- 26.Dai M, Wang P, Boyd AD, Kostov G, Athey B, Jones EG, et al. Evolving gene/transcript definitions significantly alter the interpretation of GeneChip data. Nucleic Acids Res. 2005;33(20):e175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smyth GK. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol. 2004;3:Article3. [DOI] [PubMed] [Google Scholar]
- 28.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci U S A. 2005;102(43):15545–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morey JS, Ryan JC, Van Dolah FM. Microarray validation: factors influencing correlation between oligonucleotide microarrays and real-time PCR. Biol Proced Online. 2006;8:175–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dallas PB, Gottardo NG, Firth MJ, Beesley AH, Hoffmann K, Terry PA, et al. Gene expression levels assessed by oligonucleotide microarray analysis and quantitative real-time RT-PCR—how well do they correlate? BMC Genomics. 2005;6:59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heng YJ, Pennell CE, Chua HN, Perkins JE, Lye SJ. Whole blood gene expression profile associated with spontaneous preterm birth in women with threatened preterm labor. PLoS One. 2014;9(5):e96901 10.1371/journal.pone.0096901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vandesompele J, De Preter K, Pattyn F, Poppe B, Van Roy N, De Paepe A, et al. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol. 2002;3(7):research0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sing T, Sander O, Beerenwinkel N, Lengauer T. ROCR: visualizing classifier performance in R. Bioinformatics. 2005;21(20):3940–1. [DOI] [PubMed] [Google Scholar]
- 34.Räisänen S, Gissler M, Saari J, Kramer M, Heinonen S. Contribution of risk factors to extremely, very and moderately preterm births—register-based analysis of 1,390,742 singleton births. PLoS One. 2013;8(4):e60660 10.1371/journal.pone.0060660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Makhlouf MA, Clifton RG, Roberts JM, Myatt L, Hauth JC, Leveno KJ, et al. Adverse Pregnancy Outcomes among Women with Prior Spontaneous or Induced Abortions. Am J Perinatol. 2014;31(9):765–72. 10.1055/s-0033-1358771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gilbert NM, O'Brien VP, Hultgren S, Macones G, Lewis WG, Lewis AL. Urinary tract infection as a preventable cause of pregnancy complications: opportunities, challenges, and a global call to action. Glob Adv Health Med. 2013;2(5):59–69. 10.7453/gahmj.2013.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van den Broek NR, Jean-Baptiste R, Neilson JP. Factors associated with preterm, early preterm and late preterm birth in Malawi. PLoS One. 2014;9(3):e90128 10.1371/journal.pone.0090128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baig SA, Khan N, Baqai T, Fatima A, Karim SA, Aziz S. Preterm birth and its associated risk factors. A study at tertiary care hospitals of Karachi, Pakistan. J Pak Med Assoc. 2013;63(3):414–8. [PubMed] [Google Scholar]
- 39.Yi SW, Han YJ, Ohrr H. Anemia before pregnancy and risk of preterm birth, low birth weight and small-for-gestational-age birth in Korean women. Eur J Clin Nutr. 2013;67(4):337–42. 10.1038/ejcn.2013.12 [DOI] [PubMed] [Google Scholar]
- 40.Enquobahrie DA, Williams MA, Qiu C, Muhie SY, Slentz-Kesler K, Ge Z, et al. Early pregnancy peripheral blood gene expression and risk of preterm delivery: a nested case control study. BMC pregnancy and childbirth. 2009;9:56 10.1186/1471-2393-9-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Osman I, Young A, Jordan F, Greer IA, Norman JE. Leukocyte density and proinflammatory mediator expression in regional human fetal membranes and decidua before and during labor at term. J Soc Gynecol Investig. 2006;13(2):97–103. [DOI] [PubMed] [Google Scholar]
- 42.Liggins GC. Cervical ripening as an inflammatory reaction In: Ellwood DA, Anderson ABM, Embrey MP, editors. The cervix in pregnancy and labour. Edinburgh: Churchill-Livingstone; 1989. p. 1–9. [Google Scholar]
- 43.Ulmsten U, Wingerup L, Belfrage P, Ekman G, Wiqvist N. Intracervical application of prostaglandin gel for induction of term labor. Obstetrics and gynecology. 1982;59(3):336–9. [PubMed] [Google Scholar]
- 44.Watari M, Watari H, DiSanto ME, Chacko S, Shi GP, Strauss JF 3rd. Pro-inflammatory cytokines induce expression of matrix-metabolizing enzymes in human cervical smooth muscle cells. Am J Pathol. 1999;154(6):1755–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schmitz T, Leroy MJ, Dallot E, Breuiller-Fouche M, Ferre F, Cabrol D. Interleukin-1beta induces glycosaminoglycan synthesis via prostaglandin E2 pathway in cultured human cervical fibroblasts. Mol Hum Reprod. 2003;9(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Friebe-Hoffmann U, Chiao JP, Rauk PN. Effect of IL-1beta and IL-6 on oxytocin secretion in human uterine smooth muscle cells. Am J Reprod Immunol. 2001;46(3):226–31. [DOI] [PubMed] [Google Scholar]
- 47.Kennard EA, Zimmerman PD, Friedman CI, Kniss DA. Interleukin-1 beta induces cyclooxygenase-2 in cultured human decidual cells. Am J Reprod Immunol. 1995;34(2):65–71. [DOI] [PubMed] [Google Scholar]
- 48.Rauk PN, Chiao JP. Interleukin-1 stimulates human uterine prostaglandin production through induction of cyclooxygenase-2 expression. Am J Reprod Immunol. 2000;43(3):152–9. [DOI] [PubMed] [Google Scholar]
- 49.Romero R, Durum S, Dinarello CA, Oyarzun E, Hobbins JC, Mitchell MD. Interleukin-1 stimulates prostaglandin biosynthesis by human amnion. Prostaglandins. 1989;37(1):13–22. [DOI] [PubMed] [Google Scholar]
- 50.Fortunato SJ, Menon R. IL-1 beta is a better inducer of apoptosis in human fetal membranes than IL-6. Placenta. 2003;24(10):922–8. [DOI] [PubMed] [Google Scholar]
- 51.Leung BM, McDonald SW, Kaplan BJ, Giesbrecht GF, Tough SC. Comparison of sample characteristics in two pregnancy cohorts: community-based versus population-based recruitment methods. BMC Med Res Methodol. 2013;13:149 10.1186/1471-2288-13-149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Public Health Agency of Canada. Perinatal Health Indicators for Canada 2011. Ottawa, ON: 2012.
- 53.da Fonseca EB, Bittar RE, Carvalho MH, Zugaib M. Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: a randomized placebo-controlled double-blind study. Am J Obstet Gynecol. 2003;188(2):419–24. [DOI] [PubMed] [Google Scholar]
- 54.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstetrics and gynecology. 2005;106(1):181–9. [DOI] [PubMed] [Google Scholar]
- 55.Simcox R, Seed PT, Bennett P, Teoh TG, Poston L, Shennan AH. A randomized controlled trial of cervical scanning vs history to determine cerclage in women at high risk of preterm birth (CIRCLE trial). Am J Obstet Gynecol. 2009;200(6):623 e1-6. 10.1016/j.ajog.2009.03.010 [DOI] [PubMed] [Google Scholar]
- 56.Goya M, Pratcorona L, Merced C, Rodo C, Valle L, Romero A, et al. Cervical pessary in pregnant women with a short cervix (PECEP): an open-label randomised controlled trial. Lancet. 2012;379(9828):1800–6. 10.1016/S0140-6736(12)60030-0 [DOI] [PubMed] [Google Scholar]
- 57.Honest H, Bachamann LM, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervicovaginal fetal fibronectin test in predicting risk of spontaneous preterm birth: systematic review. BMJ. 2002;325(7359):301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Heng YJ, Taylor L, Larsen BG, Chua HN, Pung SM, Lee MW, et al. Albumin decrease is associated with spontaneous preterm delivery within 48 h in women with threatened preterm labor. J Proteome Res. 2015;14:457–66. 10.1021/pr500852p [DOI] [PubMed] [Google Scholar]
- 59.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: Final data for 2012. National Vital Statistics Reports. 2013;62(9). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
(DOC)
(DOCX)
Data Availability Statement
Data were deposited into the National Center for Biotechnology Information Gene Expression Omnibus (accession number: GSE59491).