Abstract
Background
The aim of this study was to evaluate the accuracy and feasibility of an individualized thoracic pedicle screw placement guide plate produced by 3-D laser printing.
Material/Methods
Thoracic pedicle samples of 3 adult cadavers were randomly assigned for 3-D CT scans. The 3-D thoracic models were established by using medical Mimics software, and a screw path was designed with scanned data. Then the individualized thoracic pedicle screw placement guide plate models, matched to the backside of thoracic vertebral plates, were produced with a 3-D laser printer. Screws were placed with assistance of a guide plate. Then, the placement was assessed.
Results
With the data provided by CT scans, 27 individualized guide plates were produced by 3-D printing. There was no significant difference in sex and relevant parameters of left and right sides among individuals (P>0.05). Screws were placed with assistance of guide plates, and all screws were in the correct positions without penetration of pedicles, under direct observation and anatomic evaluation post-operatively.
Conclusions
A thoracic pedicle screw placement guide plate can be produced by 3-D printing. With a high accuracy in placement and convenient operation, it provides a new method for accurate placement of thoracic pedicle screws.
MeSH Keywords: Bone Plates; Bone Screws; Imaging, Three-Dimensional; Individuality
Background
With development of thoracic diseases and thoracic surgery skills, spinal posterior pedicle internal fixation has been clinically used to treat thoracic fractures and tumors, according to the spinal 3-column theory of Denis. It has become an important spinal fixation operation due to its slight operational trauma, short fixed segments, and high fixed strength [1]. Boucher [2] first reported a successful pedicle internal fixation in 1959, but it has not been applied widely until 1986, after Roy-Camille [3] reported excellent clinical efficacy of pedicle fixation in treating spinal fractures. However, the vertebral arch in the mid-upper thoracic vertebrates is relatively thinner and has more malformations, making screw placement difficult high risk. Complications of failed placement, such as spinal cord damage, injuries of great vessels around the vertebral bodies, fracture of pedicles, and thoracic nerve root injury, happen occasionally, posing a technical difficulty that needs to be solved.
Although intra-operative imaging positioning and screw placement under navigation have been popular research topics in recent years, and accuracy of screw placement has been improved, the high expense, complex process, and increased radiation risks during the operation have limited its adoption [4]. The clinical surgery needs an easy and cheap method to assist screw placement [5].
This article was based on, and made some improvements of, Lu’s method [6], which applied 3-D printing technique [7] in thoracic pedicle screw placement. Medical Mimics software, combined with 3-D laser printing technique, was used in manufacturing individualized thoracic pedicle screw guide plates, which could assist in accurate insertions. We also assess this technique.
Material and Methods
Study population
Three fresh adult cadavers were randomly assigned. There were 2 males and 1 female, with Han ethnicity and an average death age of 52.3 years (all provided by the Anatomy Dept. of Xuzhou Medical School). The T1 to T12 vertebral bodies were taken out of each body, with peripheral soft tissues wiped out and intervertebral discs preserved. A thin-layer 3-D CT scan was performed (Siemens, Germany) to exclude the samples with bone-structure damage such as fractures, occupation, or malformation of vertebral pedicles. A total of 36 vertebral bodies were included in this study.
Design and manufacture of thoracic pedicle screw placement guide plates
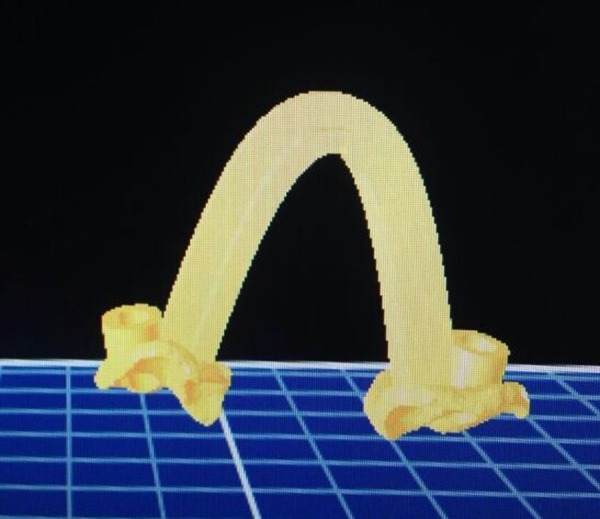
Samples were scanned with 3-D CT, and images with a DICOM format were obtained (the layer and scan thickness were all <1.25 mm). 3-D images of spines were produced by medical Mimics software and corresponding 3-D images of each vertebral body were designed with 3-D data from PTC CREO 3.0 (http://www.ptc.com/product/creo) and Geomagic (http://www.geomagic.com/en/products/design/overview) software. PTC CREO was used to design models and Geomagic was used in reverse engineering technique. A virtual screw panel was established on a vertebral model by MedCAD, which was parallel with the long axis of the pedicle (Figure 1) [8]. After the virtual screw was placed, an entry point and an axial leaning angle and sagittal dip angle of the screw were confirmed on 3-D reconstructive images. The screw panels were hollowed out and a 3.0×4.0 cylindrical panel formed reversely, which made a guide plate leading channel (Figure 2).
Figure 1.

A virtual screw panel was established on a vertebral model by MedCAD, which was parallel with the long axis of the pedicle.
Figure 2.
The corresponding 3-D guide plate was rebuilt according to the data.
In the manufacture of guide plates, the inner sides of guide plates and the bony structures of the backsides of vertebral bodies were made to completely fit with each other. Then the models were saved in STL format and transmitted to a SPS600 3-D printer (provided by Xi’an Jiaotong University). Individualized guide plates were printed by using photosensitive resin (Figure 3).
Figure 3.

Individualized 3-D guide plates were printed according to the specimens by using polylactic acid material.
Assessment of guide plate assistant thoracic pedicle screw placement and accuracy
Posterior soft tissues of vertebral bodies were cleared, and normal bony structure damage was avoided. The operator held the corresponding individualized guide plate in one hand, matched it up with the vertebral body, and kept it stable while the surgeon held the screw panel alongside the leading panel on the plate with the pedicle instrument open in the other hand. The opposite side was operated on in the same way (Figure 4). After the guide plate was removed, screws were placed alongside bilateral panels (Figure 5). The operative time of each screw placement was recorded. X-ray assistance or screw panels correction by exploration during placement should be avoided to reflect true assistant effects of guide plates. After placement of screws, the positional relation between the screw and the neighboring structures, such as vertebral body and spinal canal (Figure 6), were first directly observed, then all the samples for examination were dissected to assess the positional relationship between the screw and the neighboring structures (Figure 7).
Figure 4.

The surgeon held the screw panel alongside the leading panel on the 3-D plate. The opposite side was operated on in the same way.
Figure 5.

After the guide plate was removed, screws were placed alongside bilateral panels.
Figure 6.

The positional relationship between the screw and the neighboring structures such as screws, vertebral body, and spinal canal were first directly observed.
Figure 7.

All the samples for examination were dissected to assess the positional relationship between the screw and the neighboring structures, like the vertebral body and spinal canal.
Results
We measured 25 vertebral samples through 3-D CT scans and precisely rebuilt them into 3-D models using medical Mimics software. The corresponding individualized guide plates were established by medical Mimics software. Under assistance of guide plates, 50 pedicle screws were inserted bilaterally. During operations, guide plates and thoracic vertebral plates fit well and were stable. The operator could handle the plate with one hand during placement. No loosening or replacement happened during preparation of screw panels. The operative time of placement was 50 to 62 seconds, with an average time of 56.2 seconds. Post-operative direct observation showed a good positional relationship between screws and neighboring structures, such as vertebral bodies and vertebral canals, and no bony cortex was penetrated (Figure 6). The dissection showed that the 50 screws were all in pedicles and vertebral bodies, with proper length and angles (Figure 7).
Discussion
Clinical significance of manufacturing thoracic pedicle screw placement guide plates
With development of spinal surgery, internal fixation of posterior thoracic pedicle screw has grown increasingly important. A key point of this operation is the one-time accurate placement of pedicle screw, but this has been very difficult and has safety concerns because of anatomic characteristics of thoracic pedicles.
According to the spinal 3-column theory, placement of thoracic pedicle screw through pedicle bony channel better complied with the thoracic anatomic mechanical properties, which could improve spine stability compared with other internal fixations. With less trauma and a shorter fixed segment [9], a maximum number of active segments of spine can be maintained.
However, according to Kothe [10], thoracic pedicles were thin, short, and narrow, and the cortex was thin and fragile; therefore, thoracic pedicles easily broke. In addition, the angles of thoracic pedicles were often different from each other, which made the error rate of one-time placement of thoracic pedicle screws very high, thereby damaging peripheral tissues and leading to severe consequences [11].
In complex thoracic fractures or vertebral malformation, thoracic pedicles are more complex, and difficulties and risks of screw placement are higher. The penetration rate of free-hand insertion of thoracic pedicle screw [12] can be 30% to 40% [13,14]. Physicians started to consider safety of screw insertion as the most important factor in this operation. Some experts thought that thoracic pedicle screw fixation must be limited to spinal posterior column damage and 3-column damage with complete spinal cord injury [13]. Some even thought that other thoracic screw fixations must replace thoracic pedicle screw placement.
In order to remedy a lack of precision, many researches relied on imaging techniques in spinal surgeries, using intra-operative C-arm or CT imaging navigation [15] to assist accurate placement of pedicle screw placement, and achieved great improvement. The intra-operative imaging navigation screw placement technique played an important role in accurate placement of thoracic pedicle screws, which was considered as the best way to assess accuracy of pedicle screw placement [16]. But with errors brought by intra-operative position changes and spinal instability [17], and disadvantages such as a lack of real-time navigation, operating complexity, and high cost, this technique was not suitable for wide use. Therefore, a practical, less-expensive, and easy-spreading assistant screw placement method is necessary for clinical work.
Feasibility of guide plates assistant thoracic pedicle screw placement
With application of 3-D printing in orthopedic spinal surgeries, individualized production of guide plates improved accuracy of operations. The relatively simpler operation processes and higher safety of guide plates remedied limitations of imaging navigation. Some researchers have applied this technique in assisting cervical pedicle or vertebral plate screw placement, and proved that it could ensure accurate placement of screws. This study aimed to improve Lu’s [6] method: to select experimental thoracic samples, to design and produce individualized thoracic pedicle screw guide plates, and perform assistant screw placement. The pilot study showed that 3-D models of thoracic pedicle screw placement guide plates built using medical Mimics software could be used for establishing screw placement parameters by a surgeon on the basis of accurate assessment of thoracic pedicle-related anatomic structures. The individualized screw placement guide plates could be used for assisting screw placement and to ensure accurate insertion of screws.
Advantages of this study
Medical Mimics software used for guide plate designation could set accurate parameters and reduce data lost during process exchange between software, through which models had a higher compliance. The process of guide plate designation has been used in daily education and research, which more closely resembled clinical work, and could be used in demonstrative teaching. While producing the guide plate, a 3-D printer could print melted materials into formation layer by layer, with shorter time and lower cost, making it possible to use guide plates in emergent surgeries. Printing materials are made of medical biodegradable polylactic acid, which could be used in operations after sterilization by ethylene oxide at a low temperature, making it more convenient and less risky for clinical application. Radiation damage by C-arm or CT imaging navigation in traditional operations and high expense were reduced.
Limitations
Data transformation between 3-D CT scans and printing might have some errors or defects, which make models different from actual structures. Materials for printing are still limited and might have morphological changes from formation to usage, which could lead to small errors when plates are applied to vertebral bodies. But with development and perfection of 3-D printing technique and material science, these limitations could be overcome and clinical advantages would be predominant. In this study, vertebral bodies were removed from corpses, followed by thoracic pedicle screw placement, which might cause deviations when compared with placement during surgeries in real life. However, crew placement should also be done after complete exposure of vertebral plate in lumbar posterior approaches, which is not significantly different from the method of this study. Another limitation is that there was no comparison between actual surgeries and experiments on corpses in this study.
Conclusions
Thoracic pedicle screw placement guide plates can be produced by 3-D printing. With high accuracy in placement and convenient operation, it provides a new method for accurate placement of thoracic pedicle screws.
Footnotes
Source of support: Departmental sources
References
- 1.Yue JJ, Sossan A, Selgrath C, et al. The treatment of unstable thoracic spine fractures with transpedicular screw instrumentation: a 3-year consecutive series. Spine (Phila Pa 1976) 2002;27:2782–87. doi: 10.1097/00007632-200212150-00008. [DOI] [PubMed] [Google Scholar]
- 2.Boucher HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41-B:248–59. doi: 10.1302/0301-620X.41B2.248. [DOI] [PubMed] [Google Scholar]
- 3.Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–59. [PubMed] [Google Scholar]
- 4.Rajasekaran S, Avadhani A, Shetty AP. Axial translaminar screw placement using three-dimensional fluoroscopy-based navigation. Singapore Med J. 2011;52:15–18. [PubMed] [Google Scholar]
- 5.Le TV, Vivas AC, Baaj AA, et al. Optimal trajectory for the occipital condyle screw. J Spinal Disord Tech. 2014;27:93–97. doi: 10.1097/BSD.0b013e31824e52a6. [DOI] [PubMed] [Google Scholar]
- 6.Lu S, Xu YQ, Chen GP, et al. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg. 2011;16:240–48. doi: 10.3109/10929088.2011.605173. [DOI] [PubMed] [Google Scholar]
- 7.Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg. 2010;5:335–41. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 8.Lee JO, Buchowski JM, Lee KM, et al. Optimal trajectory for the occipital condylar screw. Spine (Phila Pa 1976) 2012;37:385–92. doi: 10.1097/BRS.0b013e31821fcdfe. [DOI] [PubMed] [Google Scholar]
- 9.Krag MH, Beynnon BD, Pope MH, et al. An internal fixator for posterior application to short segments of the thoracic, lumbar, or lumbosacral spine. Design and testing. Clin Orthop Relat Res. 1986:75–98. [PubMed] [Google Scholar]
- 10.Kothe R, O’Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle. An anatomic study. Spine (Phila Pa 1976) 1996;21:264–70. doi: 10.1097/00007632-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 11.Lien SB, Liou NH, Wu SS. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16:1215–22. doi: 10.1007/s00586-006-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 2004;29:333–42. doi: 10.1097/01.brs.0000109983.12113.9b. discussion 42. [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–6. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Merloz P, Tonetti J, Pittet L, et al. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res. 1998:39–48. doi: 10.1097/00003086-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Rao G, Brodke DS, Rondina M, Dailey AT. Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg. 2002;97:223–26. doi: 10.3171/spi.2002.97.2.0223. [DOI] [PubMed] [Google Scholar]
- 17.Holly LT, Foley KT. Percutaneous placement of posterior cervical screws using three-dimensional fluoroscopy. Spine (Phila Pa 1976) 2006;31:536–40. doi: 10.1097/01.brs.0000201297.83920.a1. discussion 41. [DOI] [PubMed] [Google Scholar]


