Abstract
Study objective
The 2010 provision of the Patient Protection and Affordable Care Act (ACA) extended eligibility for health insurance for young adults aged 19 to 25 years. It is unclear, however, how expanded coverage changes health care behavior and promotes efficient use of emergency department (ED) services. Our objective was to use population-level emergency department data to characterize any changes in diagnoses seen in ED among young adults since the implementation of the ACA dependent coverage expansion.
Methods
We performed a difference-in-differences analysis of 2009 to 2011 ED visits from California, Florida, and New York, using all-capture administrative data to determine how the use of ED services changed for clinical categories after the ACA provision among young adults aged 19 to 25 years compared with slightly older adults unaffected by the provision, aged 26 to 31 years.
Results
We analyzed a total of 10,158,254 ED visits made by 4,734,409 patients. After the implementation of the 2010 ACA provision, young adults had a relative decrease of 0.5% ED visits per 1,000 people compared with the older group. For the majority of diagnostic categories, young adults’ rates and risk of visit did not change relative to that of slightly older adults after the implementation of the ACA. However, although young adults’ ED visits significantly increased for mental illnesses (2.6%) and diseases of the circulatory system (eg, nonspecific chest pain) (4.8%), visits decreased for pregnancy-related diagnoses and diseases of the skin (eg, cellulitis, abscess) compared with that of the older group (3.7% and 3.1%, respectively).
Conclusion
Our results indicate that increased coverage has kept young adults out of the ED for specific conditions that can be cared for through access to other channels. As EDs face capacity challenges, these results are encouraging and offer insight into what could be expected under further insurance expansions from health care reform.
INTRODUCTION
Young adults represent a unique population with distinct health care needs. Although they are generally healthy, they also have high rates of preventable diseases and injuries.1 Studies suggest that young adults rely heavily on emergency department (ED) care for their health care needs, and in California adults aged between 19 and 34 years had a 15% increase in ED visits from 2005 to 2010.2,3 High ED utilization among young adults could reflect many factors, including lack of insurance, limited access to primary care, and redirection from other care facilities. As EDs face cost containment4 and crowding issues,5 it is increasingly important for policymakers to address high ED utilization across all populations to improve the efficiency and quality of the health care system.
In September 2010, the Patient Protection and Affordable Care Act (ACA) enacted a specific provision geared toward young adults aged 19 to 25 years to expand insurance coverage, the dependent coverage expansion. This provision enabled young adults to remain as dependents on their parents’ private health insurance policies. Studies suggest that the 2010 provision increased the proportion of health care visits covered by private insurers,6–8 with non-Hispanic whites demonstrating greater net gains in coverage compared with other race or ethnic groups.9
Other studies indicate that dependent coverage expansion was associated with an overall decrease in ED utilization among young adults compared with an older population.10,11 However, these modest decreases in ED utilization provide little insight on how expanded insurance coverage affects overall changes in health care use behavior and in which medical conditions these reductions occur. Specific knowledge distinguishing the medical conditions for which young adults continue to seek care in the ED from those for which use has decreased can shed light onto how the health care system is addressing the underlying needs of young adults and guide future policies targeting this population.
This study examines changes pre- versus post-ACA in rates of diagnosis-specific ED visits by young adults aged 19 to 25 years in 3 US states compared with adults aged 26 to 31 years during the same period who were unaffected by the 2010 provision. For each diagnosis group, we estimated both the change in the number of ED visits per year and the change in the risk of ever visiting the ED for young adults compared with the control group pre- versus post-ACA. Given previous reports of racial disparities in the expansion coverage,9,10 we also sought to explore these changes across race and ethnic groups.
MATERIALS AND METHODS
Study Design and Setting
We performed a retrospective analysis of 2009 to 2011 ED visits to determine how the use of ED services changed for discrete clinical categories before versus after the ACA’s dependent coverage expansion among young adults aged 19 to 25 years. We compared service use with that of a control group of slightly older adults aged 26 to 31 years, who were unaffected by the ACA provision. ED visits were obtained from all-capture longitudinal state ED databases and state inpatient databases in California, Florida, and New York, thus capturing ED encounters that resulted in discharge or admission to a hospital. The state inpatient database and state ED database are distributed by the Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project.12
Selection of Participants
A pre-ACA period was defined from September 1, 2009, through August 31, 2010, 1 year preceding the provision’s implementation, and a post-ACA period from January 1 through December 31, 2011. We excluded the period from September 1 through December 31, 2010, to avoid uncertainties about when insurance plans renewed, as other studies have done.8,10 We extracted 11,413,240 ED encounters made by patients aged 19 to 31 years in these 2 periods. We excluded records that did not have a visit linkage number (9%) or were from out of state (3%).
Methods of Measurement
Each visit was categorized by primary discharge diagnosis into one of 18 diagnostic groups, using the Clinical Classifications Software provided by the Agency for Healthcare Research and Quality.13 The software collapses more than 14,000 International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes into 18 discrete, clinically meaningful categories. Two Clinical Classifications Software categories were excluded from the analysis, conditions originating in the perinatal period and residual and unclassified codes, because one category was not applicable to our population and the second could not provide meaningful information about the reason for the ED visit.
For each period, we counted the number of ED visits a person had for each of the Clinical Classifications Software categories. We used Healthcare Cost and Utilization Project’s anonymized person-specific linkage identification to aggregate across visits. Next, we used census data to calculate the number of people in each state who did not visit the ED during each period. Specifically, we first counted the observed ED visitors aggregated by race or ethnicity, sex, age, and state. For race or ethnicity, we used the following categories: non-Hispanic white, black, Hispanic, and other. Using Census Bureau population data,14 we estimated the number of residents in each demographic group. Finally, to estimate the number people who never visited the ED (ie, had 0 visits) we subtracted the number of ED visitors in each demographic group from the number of state residents in that same demographic group; we used the 2010 population estimates for the pre-ACA period and the 2011 estimates for the post-ACA period. We thus constructed a person-level data set representing the entire young adult population in the states included in the study, in which nonvisitors were included and represented as each having zero visits.
Primary Data Analysis
The primary outcome of interest was the number of ED visits for each Clinical Classifications Software category per person per period. A secondary outcome was the number of residents in each demographic category who used the ED at least once for a given software category and period relative to the total number of residents in that demographic category.
For each diagnostic category, we estimated the association between the coverage expansion and ED visits per person among 19- to 25-year-olds, using the control group (aged 26 to 31 years) to account for changes that would have occurred over time even without the ACA; we report results as visits per 1,000 people. We used a difference-in-differences approach to account both for pre-ACA differences between the treated group and control group and for secular trends that affected both groups.15 Specifically, a difference-indifference analysis assessed the difference between the secular changes observed in the treated group and the secular changes observed in the control group. The difference between these 2 changes was the difference-in-difference estimate.
To adjust for differences in population demographics, we used a negative binomial regression to model the change in the number of ED visits per person associated with the ACA. A negative binomial model is an extension of Poisson regression that is appropriate when there is overdispersion, which was likely in our case, given the number of people with 0 visits. Within a regression model, the difference-indifference estimate is represented with an indicator in the model constructed by the interaction of period and age group. Using this regression framework, we then added race, sex, state, and a linear term for age as covariates to adjust for differences in these factors between groups and periods. We used the variable age 2 ways. First, we used age as a grouping variable that was meant to differentiate the 2 groups for the difference-in-differences analysis. To control for potential within-group confounding, we also added an additional linear term for age within each group. Therefore, we did not need to assume, for example, that rates were homogenous between 19- and 25-year-olds. Like Poisson regression, a negative binomial model estimates a change in rate, so the difference-in-differences parameter is a difference in rates.
We estimated the number of visits saved by the ACA in the 3 states by using the model to predict the expected total number of visits by residents aged 19 to 25 years in 2011 if the coverage expansion had not occurred for a given state. From that estimated mean, we subtracted the expected total visits under the ACA, according to the model. The difference between these 2 totals was our estimate of visits saved.
We also analyzed the binary outcome of whether an individual ever visited the ED for a given Clinical Classifications Software category. We used a difference-in-differences approach for this analysis as well, which we estimated with a relative risk regression to calculate percentage change in the probability of having any visits, adjusting for race, sex, age by year, and state.16
To explore subgroup differences, we also estimated the relative change in the likelihood of each category of expected primary payer, again using a relative risk difference-in-differences model, treating each payer category as a separate binary outcome.
Sensitivity Analyses
We performed 2 sensitivity analyses in our study. Results were stratified by state and sex to ensure that these effects were similar within regions and sex. Also, we isolated the young adult group to 22- to 23-year-olds and 28- to 29-year-olds and performed these analyses separately to test the stability of our results, given the transient college-age population.
The analyses were performed with the R statistical computing environment (version 3.0.3; Vienna, Austria), and SAS (version 9.4; SAS Institute, Inc., Cary, NC).
RESULTS
We analyzed a total of 10,158,254 ED visits made by 4,734,409 patients (Table 1). After the 2010 ACA provision, young adults (aged 19 to 25 years) had an absolute increase of 9.2 ED visits per 1,000 people, which was 1.7 fewer than the increase among the older group (10.9 visits per 1,000 people) (Table 1). Patient demographics statistically differed between the 2 age groups and pre- versus post-ACA, although these differences were not clinically meaningful (Table 2). We found an increase in the relative change in the likelihood of visits covered by private insurance among young adults pre- versus post-ACA compared with that of the control population (12.5%; 95% confidence interval [CI] 12.0% to 13.0%) and a decrease in the proportion of self-paid visits (−7.9; 95% CI −8.3 to −7.5) and Medicaid visits (−4.1; 95% CI −4.5 to −3.6) (Table 3).
Table 1.
Aggregated ED visits and patients by age group, 2009 to 2011.*
| Policy Period | Age Group, Years | ED Visits, No. (%) | ED Visits per 1,000 Population† | ED Patients, No. (%) |
|---|---|---|---|---|
| Pre-ACA | 19–25 | 2,788,217 (56.1) | 371.5 | 1,588,087 (56.9) |
| Pre-ACA | 26–31 | 2,178,582 (43.9) | 334.7 | 1,202,288 (43.1) |
| Post-ACA | 19–25 | 2,896,497 (55.8) | 380.7 | 1,635,584 (56.8) |
| Post-ACA | 26–31 | 2,294,958 (44.2) | 345.6 | 1,246,290 (43.2) |
| Total | 10,158,254 | 4,734,409 |
Authors’ analysis of data from the 2009 to 2011 state inpatient databases and state ED databases from California, Florida, and New York.
Based on the 2010 US Census Bureau data. The pre-ACA period is September 1, 2009, to August 31, 2010. The post-ACA period is January 1 to December 31, 2011.
Table 2.
Characteristics of patients using the ED according to age group, 2009 to 2011.
| Age, Years
|
||||
|---|---|---|---|---|
| Characteristic | 19–25, Pre-ACA | 19–25, Post-ACA | 26–31, Pre-ACA | 26–31, Post-ACA |
| Sex, % | ||||
| Female | 58.8 | 58.8 | 57.8 | 58.0 |
| Male | 41.2 | 41.2 | 42.2 | 42.0 |
| Race, % | ||||
| White | 44.9 | 43.9 | 45.3 | 44.9 |
| Black | 21.5 | 21.7 | 19.9 | 20.2 |
| Hispanic | 23.6 | 24.2 | 23.1 | 23.2 |
| Other | 10.0 | 10.2 | 11.6 | 11.7 |
| State, % | ||||
| California | 36.9 | 36.8 | 37.6 | 37.3 |
| Florida | 29.1 | 29.1 | 28.6 | 28.9 |
| New York | 34.0 | 34.2 | 33.7 | 33.8 |
Table 3.
Estimated percentage change in probabilities of ED visits per person according to primary expected payer and age group, 2009 to 2011.*
| Age, Years, %
|
Model-Estimated Change in Probability of Payer, % (95% CI)† | ||||
|---|---|---|---|---|---|
| Expected Primary Payer | 19–25, Pre-ACA | 19–25, Post-ACA | 26–31, Pre-ACA | 26–31, Post-ACA | |
| Medicare | 1.4 | 1.6 | 3.5 | 3.9 | −0.6 (−2.2 to 1.1) |
| Medicaid | 28.8 | 35.2 | 26.4 | 33.7 | −4.1 (−4.5 to −3.6) |
| Private insurance | 32.8 | 29.4 | 35.9 | 28.7 | 12.5 (12.0 to 13.0) |
| Self-pay | 29.9 | 26.9 | 26.7 | 26.2 | −7.9 (−8.3 to −7.5) |
California, Florida, and New York state inpatient database and state ED database data sets, 2009 to 2011.
The modeled relative change in the probability of each payer category was estimated with Poisson relative-risk regression analysis, with change after the implementation of the ACA provision measured by the interaction of the post-ACA period and the younger age group.
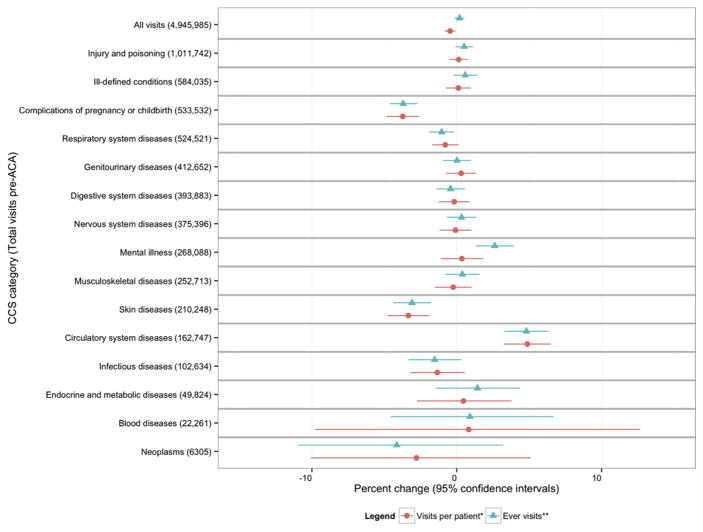
Overall, we estimated a relative decrease of 0.5% (95% CI −0.8% to −0.1%) in the number of ED visits per 1,000 people compared with that of slightly older adults (Figure and Table 4). Of the 16 diagnostic categories evaluated, the most common diagnoses for ED visits were injury and poisoning (20%), ill-defined conditions (12%), and complications of pregnancy (11%) (Table 5). The reduction we found indicates approximately 14,000 ED visits saved in the 3 states in 2011. For the majority of the diagnostic categories, young adults’ rates of visits did not change significantly relative to that of slightly older adults. Similarly, young adults’ relative risk of ever visiting the ED for most diagnostic categories did not change significantly after dependent coverage expansion. However, the relative risk of a young adult to ever visit the ED increased by 2.6% for mental illnesses and by 4.8% for diseases of the circulatory system (eg, nonspecific chest pain, cardiac dysrhythmias) compared with that of slightly older adults. On the other hand, there were significant decreases in relative rates of number of ED visits for pregnancy-related diagnoses (−3.7%) and diseases of the skin (eg, cellulitis, abscess) (−3.3%).
Figure.
Estimated changes in ED use, according to primary reason for visit (Clinical Classifications Software category), 2009 to 2011.* *Congenital anomalies were not included in the figure for visual purposes because of large CIs.
Table 4.
Changes in ED use according to primary reason for visit (Clinical Classifications Software category), 2009 to 2011.
| CCS Category | Estimated Change in Number of Visits, % (95% CI)* | Estimated Change in Probability of Visit, %† |
|---|---|---|
| Overall | −0.5 (−0.8 to −0.1) | 0.2 (−0.1 to 0.5) |
| Injury and poisoning | 0.1 (−0.5 to 0.8) | 0.5 (−0.1 to 1.1) |
| Ill-defined conditions | 0.1 (−0.8 to 1.0) | 0.6 (−0.2 to 1.4) |
| Complications of pregnancy or childbirth | −3.7 (−4.9 to −2.6) | −3.7 (−4.6 to −2.7) |
| Respiratory system diseases | −0.8 (−1.7 to 0.1) | −1.0 (−1.9 to −0.2) |
| Genitourinary diseases | 0.3 (−0.7 to 1.3) | 0 (−0.9 to 1.0) |
| Digestive system diseases | −0.2 (−1.2 to 0.9) | −0.4 (−1.4 to 0.6) |
| Nervous system diseases | −0.1 (−1.2 to 1.0) | 0.3 (−0.7 to 1.3) |
| Mental illness | 0.4 (−1.1 to 1.8) | 2.6 (1.3 to 3.9) |
| Musculoskeletal diseases | −0.2 (−1.5 to 1.0) | 0.4 (−0.8 to 1.6) |
| Skin diseases | −3.3 (−4.8 to −1.9) | −3.1 (−4.4 to −1.8) |
| Circulatory system diseases | 4.9 (3.3 to 6.5) | 4.8 (3.3 to 6.3) |
| Infectious diseases | −1.3 (−3.2 to 0.6) | −1.5 (−3.3 to 0.3) |
| Endocrine and metabolic diseases | 0.5 (−2.8 to 3.8) | 1.4 (−1.4 to 4.4) |
| Blood diseases | 0.8 (−9.8 to 12.7) | 0.9 (−4.6 to 6.7) |
| Neoplasms | −2.8 (−10.1 to 5.1) | −4.1 (−11.0 to 3.2) |
| Congenital anomalies | 16.6 (−5.4 to 43.6) | 14.9 (−2.0 to 34.7) |
CCS, Clinical Classifications Software.
The modeled relative change in the number of ED visits per patient was estimated with a negative binomial model, with change after the implementation of the ACA provision measured by the interaction of the post-ACA period and the younger age group.
The modeled change in the probability of young adults ever using the ED pre-ACA versus post-ACA was estimated with Poisson relative-risk regression analysis, with change after the implementation of the ACA provision measured by the interaction of the post-ACA period and the younger age group.
Table 5.
ED visits according to primary reason for visit (Clinical Classifications Software category), 2009 to 2011.*
| CCS Category | N | % |
|---|---|---|
| Injury and poisoning | 2,055,890 | 20.24 |
| Ill-defined conditions | 1,205,135 | 11.86 |
| Complications of pregnancy or childbirth | 1,094,982 | 10.78 |
| Respiratory system diseases | 1,041,848 | 10.26 |
| Genitourinary diseases | 859,943 | 8.47 |
| Digestive system diseases | 811,099 | 7.98 |
| Nervous system diseases | 777,789 | 7.66 |
| Mental illness | 567,686 | 5.59 |
| Musculoskeletal diseases | 525,720 | 5.18 |
| Skin diseases | 433,129 | 4.26 |
| Circulatory system diseases | 341,208 | 3.36 |
| Infectious diseases | 205,313 | 2.02 |
| Endocrine and metabolic diseases | 103,157 | 1.02 |
| Blood diseases | 69,239 | 0.68 |
| Neoplasms | 46,435 | 0.46 |
| Congenital anomalies | 13,095 | 0.13 |
California, Florida, and New York state inpatient database and state ED database data sets, 2009 to 2011.
Our results were robust to different specifications, as determined by the sensitivity analyses. The results remained similar even when stratified by state and sex (Table E1, available online at http://www.annemergmed.com). When the group was isolated to 22- to 23-year-olds and 28- to 29-year-olds, the magnitude of our coefficient estimates was larger than in the full study sample (−1.2%; 95% CI −1.9% to −0.6%), which estimated a reduction of approximately 11,000 visits in the 3 states, accounting for more than 75% of the total visits saved among all young adults (Table E2, available online at http://www.annemergmed.com).
LIMITATIONS
These results are based on data from 3 states and thus may not be generalizable to other states with different policies and population characteristics. We are unable to account for patient mobility. It is possible that patients sought ED care outside their state of residence or moved out of state during the study period, which could be an important factor among this young age group. The fact that the sensitivity analysis of 22- to 23-year-olds produced similar results increases our confidence that the results were not strongly associated with mobility over time.
The ACA’s dependent coverage extension took effect on September 23, 2010. However, the date when the provision began to actually affect an individual’s coverage depended on when insurance contracts were renewed. This might have led to errors in the assignment of dependent coverage status for some observations. We excluded September 1 to December 31, 2010, from the analysis to reduce such measurement error. We were not able to track individuals’ insurance status changes over time; however, at the aggregate level we found that at the population level, the proportion of ED visits covered by private insurance increased by 12% among young adults pre- versus post-ACA and self-paid visits decreased by 7.9% compared with those of slightly older adults (Table 3).
For our analyses, we used a negative binomial model, which is an extension of the more common Poisson regression. The Poisson model assumes that the mean and variance of the outcome (number of visits) are equal. The negative binomial adds an additional parameter to the variance estimate to allow it to be larger than the mean. The primary situation under which the negative binomial model would be inappropriate would be if the variance were less than the mean. This is a condition rarely observed in practice and not supported by the current analysis.
Finally, we assessed changes in complications in pregnancy and childbirth. This outcome can change when there is an overall decrease in the number of pregnancies in the population either from economic recovery or increased access to contraceptives.
DISCUSSION
One year after the implementation of the 2010 ACA dependent coverage expansion provision, young adults aged 19 to 25 years had a statistically significant estimated relative decrease of 0.5% in the number of ED visits per 1,000 people compared with that of slightly older adults unaffected by the provision, an implied reduction of approximately 14,000 visits within these states. Classifying young adult ED visits into discrete clinical categories, we found no change in ED utilization for conditions unlikely to be affected by insurance coverage, such as injuries and poisoning, blood diseases (eg, coagulation disorders), and congenital anomalies. However, our results indicate that increased coverage has kept young adults out of the ED and reduced the number of ED visits for specific conditions—in particular, complications of pregnancy and skin diseases (eg, cellulitis, skin abscess)—that can be cared for through access to other channels. Yet, after insurance expansion, young adults were more likely to visit the ED for mental health issues and circulatory system diseases (eg, nonspecific chest pain, cardiac dysrhythmias) compared with the control population.
Our results add to recent analyses10,11 by identifying specific diseases that were significantly affected by insurance expansion. Overall, complications of pregnancy and skin diseases (eg, cellulitis, abscesses) were the only diagnostic categories that significantly decreased among young adults after the 2010 provision. Complications of pregnancy were among the top reasons young adults visited the ED, and this diagnostic group demonstrated the largest reduction in ED visits after the ACA implementation. Before the ACA implementation, even individuals with insurance coverage often lacked prenatal and maternity care—a major source of health care expenditure for young adults—because many private plans did not cover this expense.17,18 With expanded insurance coverage and the other mandatory maternal and prenatal benefits under the ACA,19 it appears that young adults are less reliant on the ED for their maternal health care needs.
Young adults also significantly decreased their risk of visiting the ED for respiratory diseases after the 2010 provision compared with the control population. This is a significant gain for the ACA because before it, young adults with asthma had poor access to non-ED care, and even when covered, they often did not use nonemergency care.20,21 Increased access to primary and specialty care facilities outside of the ED could account for the decrease we found. As young adults gain insurance coverage, non-ED management of diseases such as asthma could reduce their reliance on ED care. It is likely that with expanded insurance coverage under the ACA, young adults have the option to seek care for nonemergency conditions outside the ED, which has resulted in an overall decrease in ED visits among young adults since the 2010 provision among this diagnostic category.
After dependent care expansion, however, our results show that young adults were more likely to ever visit the ED for mental illnesses and circulatory system diseases, such as nonspecific chest pain. Recent studies have found an increase in ED visits for mental illness, even for uninsured individuals.22 These results suggest that significant barriers to nonemergency care continue to exist for mental health issues, barriers beyond insurance coverage, such as cost sharing,23 availability of mental health professionals,24 and stigma associated with seeking mental health services,25 which could play a particularly substantial role in this young population.
We found significant changes in ED utilization for specific conditions after the dependent coverage expansion. Our results indicate that increased coverage has kept young adults out of the ED for specific diseases—in particular, complications of pregnancy and skin diseases—that can be cared for through access to other channels. However, we found that almost exclusively white and black young adults, not including Hispanics, experienced the decreases in use for these conditions. Finally, our data suggest young adults are more likely to visit the ED for mental health issues than they would have been without the insurance expansion. These results offer insight into the debate over the effect of expanded insurance coverage on ED utilization and suggest that it decreased ED visits for certain nonurgent diagnoses.
Supplementary Material
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Footnotes
Author contributions: TH-B conceived and designed the study and drafted the article. All authors provided statistical advice on study design, analyzed the data, and contributed substantially to article revision. TH-B takes responsibility for the paper as a whole.
Presented at the Academy Health Annual Research Meeting (ARM), June 2015, Minneapolis, MN.
References
- 1.Park MJ, Paul Mulye T, Adams SH, et al. The health status of young adults in the United States. J Adolesc Health. 2006;39:305–317. doi: 10.1016/j.jadohealth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 2.Hsia RY, Nath JB, Baker LC. Emergency department visits by children, adolescents, and young adults in California by insurance status, 2005–2010. JAMA. 2014;312:1587–1588. doi: 10.1001/jama.2014.9905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsia RY, Brownell J, Wilson S, et al. Trends in adult emergency department visits in California by insurance status, 2005–2010. JAMA. 2013;310:1181–1183. doi: 10.1001/jama.2013.228331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morganti K, Bauhoff S, Blanchard J, et al. The Evolving Role of Emergency Departments in the United States. Rand Corporation; Santa Monica, CA: 2013. [PMC free article] [PubMed] [Google Scholar]
- 5.Adams JG. Emergency department overuse: perceptions and solutions. JAMA. 2013;309:1173–1174. doi: 10.1001/jama.2013.2476. [DOI] [PubMed] [Google Scholar]
- 6.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307:913–914. doi: 10.1001/jama.307.9.913. [DOI] [PubMed] [Google Scholar]
- 7.Cantor JC, Monheit AC, DeLia D, et al. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47:1773–1790. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mulcahy A, Harris K, Finegold K, et al. Insurance coverage of emergency care for young adults under health reform. N Engl J Med. 2013;368:2105–2112. doi: 10.1056/NEJMsa1212779. [DOI] [PubMed] [Google Scholar]
- 9.O’Hara B, Brault MW. The disparate impact of the ACA–Dependent Expansion across population subgroups. Health Serv Res. 2013;48:1581–1592. doi: 10.1111/1475-6773.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez-Boussard T, Burns CS, Wang NE, et al. The Affordable Care Act reduces emergency department use by young adults: evidence from three states. Health Aff (Millwood) 2014;33:1648–1654. doi: 10.1377/hlthaff.2014.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antwi YA, Moriya AS, Simon K, et al. Changes in emergency department use among young adults after the Patient Protection and Affordable Care Act’s dependent coverage provision. Ann Emerg Med. 2015;65:664–672. doi: 10.1016/j.annemergmed.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality; Human and Health Services, editor. HCUP databases. Rockville, MD: Agency for Healthcare Research & Quality; 2013. [Google Scholar]
- 13.Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS) Rockville, MD: Agency for Healthcare Research & Quality; 2014. Available at http://www.ahrq.gov/data/hcup/ccs.htm#download. [Google Scholar]
- 14.US Census Bureau. Current Population Survey: Annual Social and Economic Supplements. Washington, DC: US Census Bureau; 2014. [Google Scholar]
- 15.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312:2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 16.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 17.Garrett D. [Accessed January 10, 2015];Turning to fairness: insurance discrimination against women today and the Affordable Care Act. 2012 Available at: http://www.nwlc.org/sites/default/files/pdfs/nwlc_2012_turningtofairness_report.pdf.
- 18.Postolowski C. Without Maternity Coverage: The Need for Special Enrollment in Health Insurance Marketplaces During Pregnancy. Young Invicibles; 2014. [Google Scholar]
- 19.Sonfield A, Pollack HA. The Affordable Care Act and reproductive health: potential gains and serious challenges. J Health Politics Policy Law. 2013;38:373–391. doi: 10.1215/03616878-1966342. [DOI] [PubMed] [Google Scholar]
- 20.Chua KP, Schuster MA, McWilliams JM. Differences in health care access and utilization between adolescents and young adults with asthma. Pediatrics. 2013;131:892–901. doi: 10.1542/peds.2012-2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halterman JS, Montes G, Shone LP, et al. The impact of health insurance gaps on access to care among children with asthma in the United States. Ambul Pediatr. 2008;8:43–49. doi: 10.1016/j.ambp.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Hsia RY, Nath JB, Baker LC. California emergency department visit rates for medical conditions increased while visit rates for injuries fell, 2005–11. Health Aff (Millwood) 2015;34:621–626. doi: 10.1377/hlthaff.2014.0471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration. Affordability Most Frequent Reason for Not Receiving Mental Health Services. Human & Health Services; 2013. [Google Scholar]
- 24.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 25.Saxena S, Thornicroft G, Knapp M, et al. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.