Abstract
Objectives
Gastroesophageal reflux is common but remains a controversial disease to diagnose and treat and little is known about the role of reflux testing in predicting clinical outcomes, particularly in children at risk for extraesophageal reflux complications. The aim of this study was to determine if rates of hospitalization were affected by reflux burden even after adjusting for aspiration risk.
Methods
We prospectively recruited, between 2009-2014, a cohort of pediatric patients with suspected extraesophageal reflux disease who were referred for reflux testing and underwent both multichannel intraluminal impedance with pH (pH-MII) and modified barium swallow studies. A subset of patients also underwent bronchoalveolar lavage with pepsin analysis. We determined their rates of hospitalization for a minimum of one year following pH-MII testing.
Results
We prospectively enrolled 116 pediatric patients who presented for care at Boston Children's Hospital and underwent both pH-MII and modified barium swallow studies. There was no statistically significant relationship between reflux burden measured by pH-MII or bronchoalveolar pepsin and total number of admissions or number of admission nights even after adjusting for aspiration status (p>0.2). There were no statistically significant relationships between reflux burden by any method and the number or nights of urgent pulmonary admissions before or after adjusting for aspiration risk (p > 0.08).
Conclusions
Even in aspirating children, reflux burden did not increase the risk of hospitalization. Based on these results, routine reflux testing cannot be recommended even in aspirating children, as the results do not impact clinically significant outcomes.
Keywords: Gastroesophageal reflux disease, aspiration, multichannel intraluminal impedance with pH (pH-MII), pepsin
Introduction
Gastroesophageal reflux disease 1 remains one of the most common reasons for visits to pediatric primary care providers and specialists and is often a difficult disease to both diagnose and treat because of the large number of symptoms attributed to reflux2-4. Current national guidelines issued by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) advise a step-wise approach for evaluation and treatment of GERD but wide variability on testing persists in the community5,6. The NASPGHAN guidelines further recommend that reflux testing with pH probes and multichannel intraluminal impedance with pH be pursued for the evaluation of extraesophageal symptoms however, little is known about the role of testing in predicting clinical outcomes.
A variety of testing modalities have been developed to try to determine if patients' symptoms might be related to reflux events5,7. Over the past decade, multichannel intraluminal impedance with pH (pH-MII) has become the dominant test for evaluating reflux burden8. This approach allows for assessment of both acid and non-acid reflux along with correlation of symptoms with impedance measurements. The sensitivity of the tool is superior to the standard pH probe, particularly in children taking acid suppression and who therefore have a relatively greater non-acid reflux burden9-13. pH-MII also offers another important advantage to children with extraesophageal symptoms; the pH-MII catheter can measure the height of the refluxate which is important if the question at hand is, does this reflux reach the proximal esophagus and the pharynx putting the patient at risk for aspiration of gastric contents.
One population that frequently undergoes testing is children with impaired airway protection, children with oropharyngeal dysphagia with resultant aspiration during swallowing. Many providers worry that patients with swallowing dysfunction who cannot protect their airway are at greater risk for aspiration of refluxed gastric contents. Therefore, in many centers, it is common practice to evaluate the possible risk of aspiration from below (i.e. aspiration from reflux) using pH-MII testing in addition to aspiration from above (i.e. aspiration during swallowing). In fact, patients with recurrent aspiration pneumonias often undergo anti-reflux surgery in an effort to reduce esophageal and airway reflux exposure 14-17. Despite this concern, recent studies have shown that anti-reflux surgery can cause its own complications and often does not reduce rates of hospitalizations18,19. Furthermore studies using pH-MII may not predict clinical response to fundoplication, we do not know if pH-MII predicts other clinical outcomes20,21. No studies have been done to determine if pH-MII testing predicts risk of hospitalization, including in high-risk patients with oropharyngeal dysphagia
The aim of the current study was to determine if reflux burden measured by pH-metry, MII and lung pepsin positivity, a biomarker of reflux-related lung disease, predicted future risk of hospitalization, particularly in children that aspirate.
Methods
We prospectively recruited a cohort of pediatric patients, ages 1-18 years old, with a suspected diagnosis of GERD who were referred for reflux testing at Boston Children's Hospital between 2009 to 2014. Patients with fundoplication and enterally fed patients were excluded. Only patients with atypical symptoms or symptoms which do not respond to standard reflux therapies undergo pH-MII testing at Boston Children's Hospital. All patients underwent both multichannel intraluminal impedance with pH (pH-MII) and modified barium swallow 22 studies. A sub-group of patients also had bronchoscopy, performed at the discretion of the primary pulmonologist, with pepsin collection. pH-MII studies were manually analyzed by one investigator (R.R.). MBS studies followed the standard protocol used at Boston Children's Hospital during which the subject starts with thin liquids and then advances to nectar thick and then honey thick and then purees and solids or to the highest age appropriate consistency. MBS studies were read by a speech language pathologist and attending radiologists and were considered abnormal if there was evidence of aspiration or penetration. Pepsin analysis was performed by Western blot using previously described methods23.
pH-MII testing results were coded for acid, non-acid and pH-only reflux episodes as previously defined. pH-MII testing was considered abnormal if the pH was <4 for >6% of the study time or if there were greater than 73 reflux episodes detected by the impedance sensors during the study time5,24. Proximal reflux burden was calculated by summing the proximal-most bolus clearance and dividing by the total study duration.
Patients were followed for a minimum of 1 year after the initial MBS to determine the number, length and types of hospitalizations as well as comorbidities based on medical record review. Hospitalizations were categorized into total and urgent hospitalizations, pulmonary or gastrointestinal hospitalizations and total hospitalization days, pulmonary days and gastrointestinal days. Urgent hospitalizations were defined as unplanned admissions through the Emergency Room at Boston Children's Hospital. Elective hospitalizations were defined as planned admissions for elective reasons such as planned surgical procedures. Because there was no statistically significant difference in any of the hospitalization rates in patients with and without pathologic reflux in the year following pH-MII testing or during the total duration of follow-up, hospitalization data are presented from the total duration of follow-up rather than one year follow up.
The primary outcome of the study was to determine, in children with a diagnosis of GERD and extraesophageal symptoms, if there were differences in the number of total hospitalizations between patients with and without evidence of pathologic reflux. Hospital admission data are presented as mean number of days ± standard error and mean number of admissions ± standard error. Hospital admission data were then adjusted for aspiration status. A negative binomial regression model was fit to consider predictors of hospitalization days and admissions. Finally, to minimize the likelihood of hidden confounders influencing hospitalization numbers, we created a model using a propensity score, which accounted for other comorbidities such as neurologic status. Outcomes were tested using the Student t test or the Wilcoxon rank-sum test. Data analysis was generated using SAS version 9.4.
The present study was approved by the Institutional Review Board at Boston Children's Hospital.
Results
A total of 116 patients were prospectively recruited. The mean age of patients in the study was 5.7 ± 0.4 years. The patients were followed for a mean of 4.0 ± 0.2 years from the date of recruitment. A subgroup of 97 patients had bronchoalveolar lavage pepsin collection and analyses. Eighty-four patients (72% of subjects) were off acid suppression therapy at the time of their pH-MII study. None of our study subjects were on metaclopramide or baclofen. Only 2 of 116 patients were on erythromycin. No significant difference in reflux parameters (percent of time with pH less than 4, number of acid events, number of non-acid events, total number of events, percent proximal reflux, and percent distal reflux) was found between patients on or off proton pump inhibitors (p>0.1).
Twenty-five patients (22% of subjects) had an abnormal MBS; 52% of those studies were abnormal due to aspiration and 48% due to penetration on MBS. 24 patients (21% of subjects) had abnormal impedance testing and 32 patients (28% of subjects) had abnormal pH testing. 34/97 patients (35% of subjects) were found to be BAL pepsin positive. The mean number of total and urgent admissions were 3.5 ± 0.1 and 2.4 ± 0.2 respectively. The mean number of total and urgent admit nights were 6.6 ± 1.1 and 3.5 ± 0.9 respectively.
Subjects were assessed for comorbidities in 7 different disease categories. Thirty-four percent of patients had neurologic comorbidities, 65% of patients had ENT comorbidities, 92% percent of patients had pulmonary comorbidities, 7% had cardiac comorbidities, 12% had metabolic/genetic comorbidities, 11% had immunology comorbidities, and 19% had gastrointestinal comorbidities. The most common comorbid diagnoses in each of these respective categories were developmental delay (15% of subjects), laryngeal cleft (29% of subjects), and asthma (66% of subjects). There were no differences in the comorbidities in patients with and without pathologic reflux (p>0.4) except for a higher rate of abnormal pH-metry in children with cardiac disease (p=0.04).
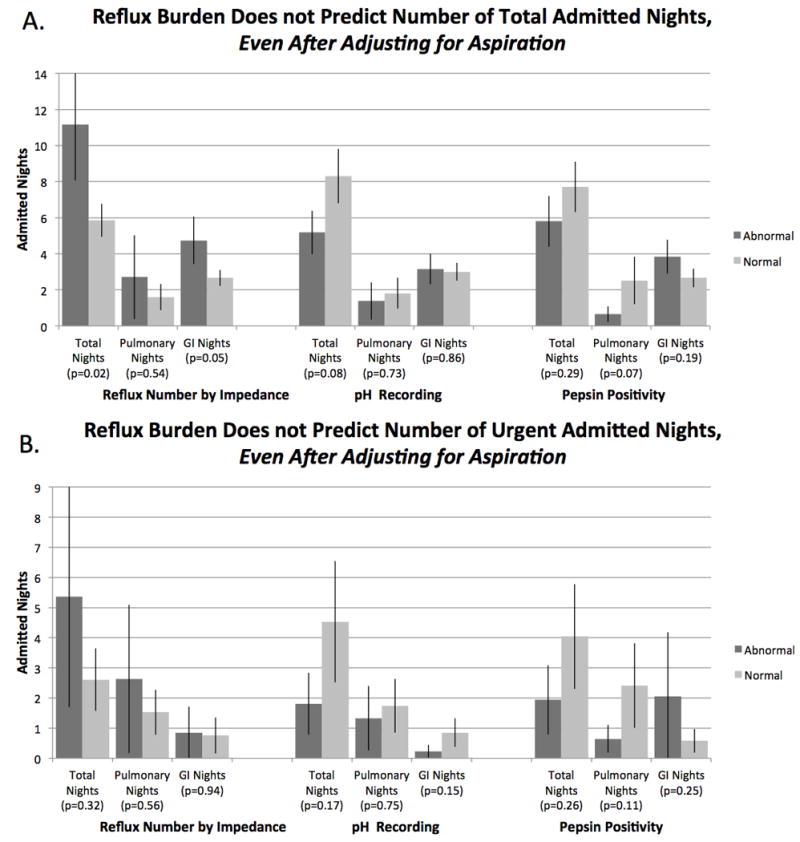
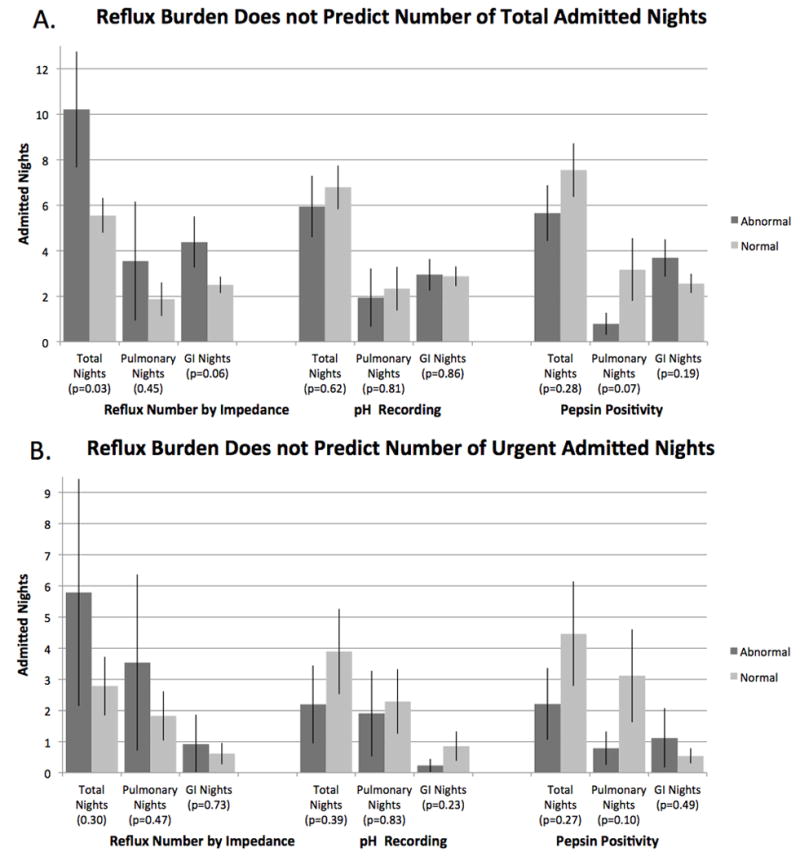
As shown in Figures 1-4, there was no significant relationship between any reflux parameter and the number of total or urgent admissions, the number of total or urgent admitted nights, or the number of total or urgent pulmonary or gastrointestinal admissions even after adjusting for aspiration. The only significant relationship was between an abnormal number of reflux episodes and total admission nights before and after adjusting for aspiration status (p=0.03, 0.02); however, the comparison was not statistically significant for urgent admission nights (p=0.30, 0.32) and reflects the elective admissions related to other comorbidities (for example, elective surgeries). In a subgroup analysis of 3 patient subgroups (normal MBS and normal pH-MII testing, normal MBS and abnormal pH-MII testing, and abnormal MBS regardless of reflux testing), there were no significant differences in the total number of admissions (p=0.22) and total hospitalization days (p=0.17) between the three groups.
Figure 1. Reflux burden as measured by impedance, pH recording, and pepsin positivity on bronchoscopy does not predict number of total (A) or urgent (B) admissions.
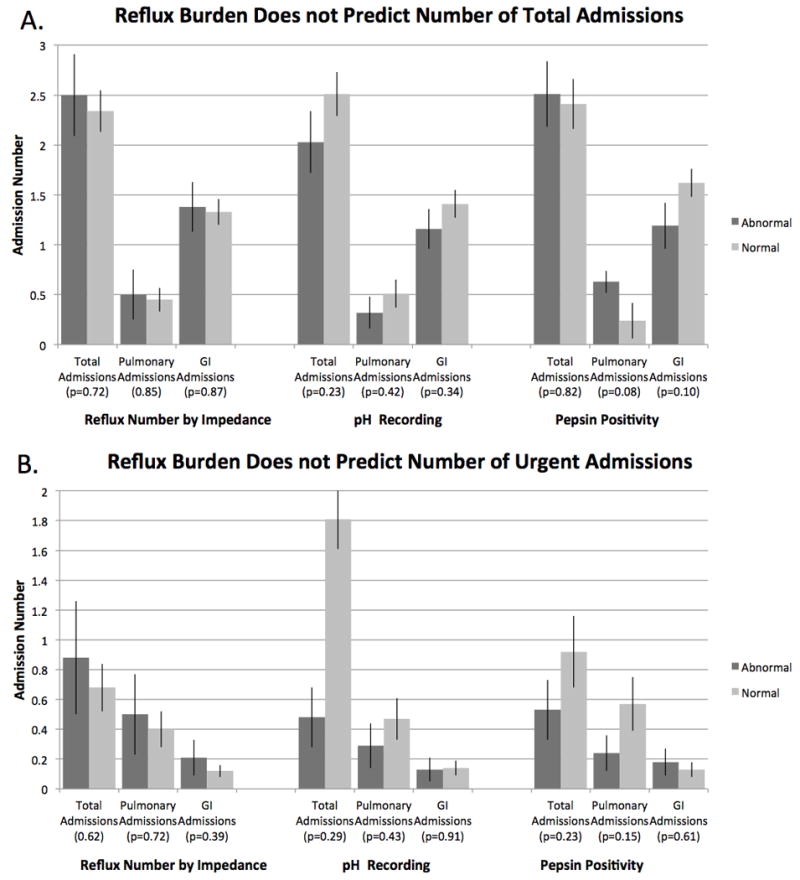
Figure 4. Reflux burden as measured by impedance, pH recording, and pepsin positivity on bronchoscopy does not predict number of total (A) or urgent (B) admitted nights, even after adjusting for aspiration on MBS.
There was no significant positive correlation between the percent of time reflux was in the proximal esophagus and the number of admissions (r=-0.242, p=0.01) or the number of admission nights (r=-0.207, p=0.03). There was no significant positive correlation between the percentage of full column reflux events and the number of admissions (r=-0.194, p=0.04) or the number of admission nights (r=-0.152, p=0.1). Lastly, the average pH-MII symptom index (# symptoms associated with reflux/total # of symptoms) was 36.6 ± 22.7% and there was no significant correlation between a positive symptom index and the number of pulmonary or gastrointestinal admission (p>0.2).
In our study population, 108 subjects out of 116 had upper GI endoscopy with biopsy performed and 24% had evidence of microscopic esophagitis. There were no differences in the total number of hospitalizations or days of hospitalization between those patients with and without esophagitis (p=0.16).
In a negative binomial model adjusted for propensity scores, there was no significant relationship between total admissions, total hospitalization nights, urgent hospitalizations, urgent hospitalization nights and any reflux parameter (total number of reflux episodes, percent time with pH<4, and pepsin) with the exception of pepsin positivity and number of hospitalization nights (p=0.02). However, in this latter model, pepsin positivity was associated with a lower number of mean hospitalizations (4.1 (2.6, 6.5)) than pepsin negative patients (8.4 (6.1, 11.5), p=0.02) so the significance is in the opposite direction than expected.
Discussion
This is the first study to address the impact of gastroesophageal reflux hospitalization risk in the pediatric population. Although GERD is one of the most common diagnoses in childhood and is frequently blamed for a variety of extraesophageal symptoms including cough, stridor, and aspiration pneumonias, the role of reflux as a cause of increased morbidity is not known3,4,25. In this study, we found that reflux burden, as detected by pH-MII and pepsin positivity, does not impact rates of hospitalization, even in children that aspirate and have neurologic comorbidities, a population felt to be at highest risk for extraesophageal reflux complications. There are three possible explanations for this: 1) reflux really has little impact on hospitalizations; 2) the methods by which we measure reflux are imperfect; or 3) any reflux, even “normal” amounts, can be problematic in patients with a predisposition for reflux complications.
First, there is very little known about the impact of gastroesophageal reflux on hospitalization rates. In a single adult study, a history of gastroesophageal reflux or proton pump inhibitor use did not predict risk of hospitalization for aspiration pneumonia or the development of acute respiratory distress syndrome (ARDS)26. While no comparable studies have been done in pediatrics, Barnhart et al studied a cohort of neurologically impaired children some of whom underwent gastrostomy tube placement and some of whom underwent gastrostomy tube placement with prophylactic fundoplication to reduce the potential risk of reflux-related hospitalizations14. The authors found that reflux-related hospitalizations did not differ in the year following surgery, regardless of whether the patient had anti-reflux surgery or not, suggesting that reflux is not a driver of hospitalizations in children with feeding difficulties. Therefore, our data combined with the current literature suggests that there seems to be little impact of reflux burden on hospitalizations, even in the medically complex patient.
A second argument is that we see no difference in hospitalizations because pH-MII is the wrong tool to assess reflux burden. Unfortunately, there is no clear gold standard (clinical history, pH-metry, or pH-MII) that consistently predicts response to therapy9,27,28. Currently, based on the NASPGHAN algorithm for the diagnosis of extraesophageal symptoms, pH-metry or pH-MII are recommended to clarify the role of reflux-related symptoms, so this is the test upon which we chose to diagnose reflux5. However, because catheter-based methods may not reflect the impact of reflux on the lung, we also chose to include pepsin measurement from bronchoscopy fluid when possible as an alternative diagnostic tool and even then we did not see a relationship between pepsin on bronchoalveolar lavage and hospitalizations.
A third argument is that any reflux, even with totals within the “normal” range can be pathologic for high-risk patients. In this study, we found that the mean total number of reflux episodes by pH-MII was 42±11 episodes in patients with an abnormal MBS and who were pepsin positive, suggesting that refluxed gastric contents can reach the lung at values lower than the pathologic cut off of 73 episodes. Additional studies are needed to determine if there is another cut off that is more predictive of outcomes in patients at high risk for complications but our results suggest that the standard impedance cut off values are not predictive of clinical outcome.
Based on the results of our study, we cannot routinely recommend the use of pH-metry or pH-MII testing to predict which patients are at risk for more severe extraesophageal disease, defined as increased risk of hospitalization. Our data support the currently available data on fundoplications, which suggest that reflux-related hospitalizations may not improve after fundoplication, even in children felt to be at high risk for reflux-related lung disease (i.e. children with neurologic compromise). In a study by Goldin et al, 22% of patients had more reflux related hospitalizations after fundoplication than before and a study by Lee et al showed that rates of hospitalization for respiratory symptoms (aspiration pneumonia, respiratory distress, and pneumonia) were identical before and after fundoplication18,19. One of the limitations to these and other earlier fundoplication studies is that objective measures of swallowing function were not pursued so one of the arguments is that patients did not improve after fundoplication because they continue to aspirate during swallowing29. Our paper is the first of which we are aware that addresses the interrelationship between abnormal swallow function and reflux burden, which strengthens the findings in this study, that reflux burden does not impact clinical outcome, even in patients with oropharyngeal dysphagia.
There are some limitations to our study. First, adjusting for comorbidities affecting hospitalizations is difficult. To address this, we adjusted, in several models, for aspiration status, for neurologic status and propensity score in which we accounted for all of the comorbidities. Regardless of how we adjusted for comorbidities, we did not find a significant difference in hospitalizations except that there was a significant relationship between an abnormal impedance study and hospitalization nights. However, we did not find a significant relationship with urgent admissions or pulmonary or GI admissions suggesting that patients with more reflux may be admitted more for elective testing or procedures, suggesting a difference in unmeasurable comorbidities. The goal of this paper however was to determine if reflux burden predicts hospitalizations for pulmonary admissions, particularly in children who aspirate, and we feel that we have shown that this is not the case, regardless of how comorbidities were measured.
A second limitation is that cause of hospitalization was determined by medical record review and sometimes the reason for admission is multifactorial. For this reason, our primary outcome was whether reflux affected total admissions, which does not involve judgment about the primary reason for admission and even with this as the primary outcome, we still did not find a relationship between reflux burden and hospitalizations. Lastly, it is possible that hospitalization is not a complete measure of aspiration morbidity since this does not account for other types of urgent visits that did not result in admission or other pulmonary outcomes such as medication use, outpatient pneumonia diagnoses or missed days of school. However, the focus of the current study was on the most severe marker of morbidity, hospitalization risk.
In conclusion, we do not recommend reflux testing to predict risk for hospitalizations, even in patients who are traditionally thought to be at high risk for extraesophageal complications. Based on the results of the present study, the utility of routine reflux testing, particularly in children who aspirate, may need to be reevaluated. Reflux testing is costly and uncomfortable, and now, based on these results, may not impact clinical outcomes.
Figure 2. Reflux burden as measured by impedance, pH recording, and pepsin positivity on bronchoscopy does not predict number of total (A) or urgent (B) admissions, even after adjusting for aspiration on MBS.
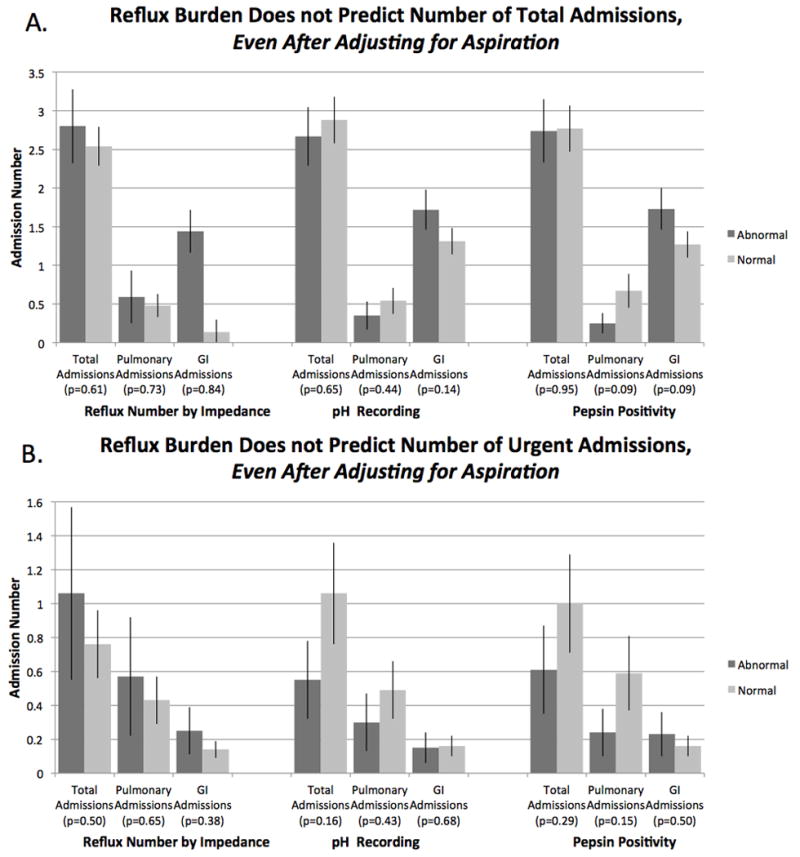
Figure 3. Reflux burden as measured by impedance, pH recording, and pepsin positivity on bronchoscopy does not predict number of total (A) or urgent (B) admitted nights.
What is Known.
Reflux testing is a commonly performed in children, particularly with atypical symptoms.
Children with impaired airway protection (oropharyngeal dysphagia with resultant aspiration) are frequently tested.
The utility of reflux testing in predicting hospitalization risk is unknown.
What is New.
pH-MII testing results do not predict subsequent hospitalization risk even in high risk patients.
Airway pepsin results do not predict subsequent hospitalization risk even in high risk patients.
Children with oropharyngeal dysphagia with subsequent aspiration are not at greater risk for hospitalizations based on their reflux burden.
Acknowledgments
All authors approved the final version of this article. DRD and RLR had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. DRD, JA, NJ, PM, KL and RLR contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript. This work was supported by the Translational Research Program at Boston Children's Hospital and by R01 DK097112-01 from the National Institutes of Health. The authors have no conflicts of interest relevant to this article to disclose.
Source of Funding: This work was supported by the Translational Research Program at Boston Children's Hospital, the NASPGHAN Foundation/Astrazeneca Research Award for Diseases of the Upper Tract, and by R01 DK097112-01 from the National Institutes of Health.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Prior abstract presentation: This work was presented in part at the NASPGHAN Annual Meeting, Atlanta, GA, October 2014.
References
- 1.Mizgerd JP. Lung infection--a public health priority. PLoS Med. 2003:e76. doi: 10.1371/journal.pmed.0030076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forbes D, Lim A, Ravikumara M. Gastroesophageal reflux in the 21st century. Curr Opin Pediatr. 2013;25:597–603. doi: 10.1097/MOP.0b013e328363ecf5. [DOI] [PubMed] [Google Scholar]
- 3.Hershcovici T, Fass R. Step-by-step management of refractory gastresophageal reflux disease. Dis Esophagus. 2013;26:27–36. doi: 10.1111/j.1442-2050.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- 4.Orenstein SR. Controversies in pediatric gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 1992;14:338–48. doi: 10.1097/00005176-199204000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Vandenplas Y, Rudolph CD, Di Lorenzo C, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) J Pediatr Gastroenterol Nutr. 2009;49:498–547. doi: 10.1097/MPG.0b013e3181b7f563. [DOI] [PubMed] [Google Scholar]
- 6.Lightdale JR, Gremse DA. Gastroesophageal reflux: management guidance for the pediatrician. Pediatrics. 2013;131:e1684–95. doi: 10.1542/peds.2013-0421. [DOI] [PubMed] [Google Scholar]
- 7.Yellon RF, Goyal A. What is the best test for pediatric gastroesophageal reflux disease? Laryngoscope. 2013;123:2925–7. doi: 10.1002/lary.23656. [DOI] [PubMed] [Google Scholar]
- 8.Wenzl TG, Benninga MA, Loots CM, et al. Indications, methodology, and interpretation of combined esophageal impedance-pH monitoring in children: ESPGHAN EURO-PIG standard protocol. J Pediatr Gastroenterol Nutr. 2012;55:230–4. doi: 10.1097/MPG.0b013e3182592b65. [DOI] [PubMed] [Google Scholar]
- 9.Rosen R. Gastroesophageal reflux in infants: more than just a pHenomenon. JAMA Pediatr. 2014;168:83–9. doi: 10.1001/jamapediatrics.2013.2911. [DOI] [PubMed] [Google Scholar]
- 10.Rosen R, Amirault J, Giligan E, et al. Intraesophageal pressure recording improves the detection of cough during multichannel intraluminal impedance testing in children. J Pediatr Gastroenterol Nutr. 2014;58:22–6. doi: 10.1097/MPG.0b013e3182a80059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosen R, Amirault J, Johnston N, et al. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr Pulmonol. 2014;49:1090–6. doi: 10.1002/ppul.22949. [DOI] [PubMed] [Google Scholar]
- 12.Rosen R, Hart K, Nurko S. Does reflux monitoring with multichannel intraluminal impedance change clinical decision making? J Pediatr Gastroenterol Nutr. 2011;52:404–7. doi: 10.1097/MPG.0b013e3182078081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosen R, Lord C, Nurko S. The sensitivity of multichannel intraluminal impedance and the pH probe in the evaluation of gastroesophageal reflux in children. Clin Gastroenterol Hepatol. 2006;4:167–72. doi: 10.1016/s1542-3565(05)00854-2. [DOI] [PubMed] [Google Scholar]
- 14.Barnhart DC, Hall M, Mahant S, et al. Effectiveness of fundoplication at the time of gastrostomy in infants with neurological impairment. JAMA Pediatr. 2013;167:911–8. doi: 10.1001/jamapediatrics.2013.334. [DOI] [PubMed] [Google Scholar]
- 15.Koch OO, Kaindlstorfer A, Antoniou SA, et al. Comparison of results from a randomized trial 1 year after laparoscopic Nissen and Toupet fundoplications. Surgical endoscopy. 2013;27:2383–90. doi: 10.1007/s00464-013-2803-0. [DOI] [PubMed] [Google Scholar]
- 16.Lasser MS, Liao JG, Burd RS. National trends in the use of antireflux procedures for children. Pediatrics. 2006;118:1828–35. doi: 10.1542/peds.2006-1185. [DOI] [PubMed] [Google Scholar]
- 17.Rangel SJ. To fundo or not to fundo? JAMA Pediatrics. 2013;167:896–7. doi: 10.1001/jamapediatrics.2013.2402. [DOI] [PubMed] [Google Scholar]
- 18.Goldin AB, Sawin R, Seidel KD, et al. Do antireflux operations decrease the rate of reflux-related hospitalizations in children? Pediatrics. 2006;118:2326–33. doi: 10.1542/peds.2006-2212. [DOI] [PubMed] [Google Scholar]
- 19.Lee SL, Shabatian H, Hsu JW, et al. Hospital admissions for respiratory symptoms and failure to thrive before and after Nissen fundoplication. J Pediatr Surg. 2008;43:59–63. doi: 10.1016/j.jpedsurg.2007.09.020. discussion 63-55. [DOI] [PubMed] [Google Scholar]
- 20.Francis DO, Goutte M, Slaughter JC, et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121:1902–9. doi: 10.1002/lary.21897. [DOI] [PubMed] [Google Scholar]
- 21.Rosen R, Levine P, Lewis J, et al. Reflux events detected by pH-MII do not determine fundoplication outcome. J Pediatr Gastroenterol Nutr. 2010;50:251–5. doi: 10.1097/MPG.0b013e3181b643db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jolley SG, Johnson DG, Roberts CC, et al. Patterns of gastroesophageal reflux in children following repair of esophageal atresia and distal tracheoesophageal fistula. J Pediatr Surg. 1980;15:857–62. doi: 10.1016/s0022-3468(80)80293-4. [DOI] [PubMed] [Google Scholar]
- 23.Johnston N, Knight J, Dettmar PW, et al. Pepsin and carbonic anhydrase isoenzyme III as diagnostic markers for laryngopharyngeal reflux disease. Laryngoscope. 2004;114:2129–34. doi: 10.1097/01.mlg.0000149445.07146.03. [DOI] [PubMed] [Google Scholar]
- 24.Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–43. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 25.Campanozzi A, Boccia G, Pensabene L, et al. Prevalence and natural history of gastroesophageal reflux: pediatric prospective survey. Pediatric. 2009;123:779–83. doi: 10.1542/peds.2007-3569. [DOI] [PubMed] [Google Scholar]
- 26.Lee A, Festic E, Park PK, et al. Characteristics and outcomes of patients hospitalized following pulmonary aspiration. Chest. 2014;146:899–907. doi: 10.1378/chest.13-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Pol RJ, Smits MJ, Venmans L, et al. Diagnostic accuracy of tests in pediatric gastroesophageal reflux disease. J Pediatr. 2013;162:983–7. e1–4. doi: 10.1016/j.jpeds.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 28.van der Pol RJ, van den Ouweland M, Loots CM, et al. Follow-Up After pH-Metry and pH-Impedance in Pediatric Gastroesophageal Reflux Disease. J Pediatr Gastroenterol Nutr. 2015;60:224–9. doi: 10.1097/MPG.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 29.Fox D, Barnard J, Campagna EJ, et al. Fundoplication and the pediatric surgeon: implications for shared decision-making and the medical home. Acad Pediatr. 2012;12:558–66. doi: 10.1016/j.acap.2012.07.006. [DOI] [PubMed] [Google Scholar]


