Abstract
Study Design
Randomized controlled trial.
Purpose
To contrast the efficacy of two exercise programs—multifidus retraining program (MRP) and traditional back exercises (TBE)—on pain and functional disability in individuals with chronic low back pain.
Overview of Literature
Low back pain is a common musculoskeletal disorder. Mechanical low back pain does not involve nerve roots. Stability of the spine is provided by the ligaments and muscles of the lower back and abdomen. Although weakness of the superficial trunk and abdominal muscles are the primary risk factors, recent studies have demonstrated the involvement of weakness and lack of control of the deep trunk muscles, especially the multifidus and transverse abdominis muscles. Therefore, exercises to restore optimal lumbar multifidus function are important in rehabilitation strategies.
Methods
Thirty individuals were randomly assigned to receive TBE, where exercises focused on the superficial muscles of abdomen and low back (control, group A) and MRP, where exercises focused on the deep multifidus muscles fibers (experimental, group B). Groups were examined to find the effect of these exercises on visual analog scale rated pain (visual analogical scale) and functional disability assessed by the Oswestry disability questionnaire. The exercise program lasted for 6 weeks on alternate days, with 20 repetitions of each exercise, with each move held for 5–8 seconds. Subjects were evaluated at the start of the study and after completion of the 6-week exercise program.
Results
As compared to baseline, both treatments were effective in relieving pain and improving disability (p<0.001). The MRP group had significant gains for pain and functional disability when compared to the TBE group (both p<0.001).
Conclusions
Both techniques lessen pain and reduce disability. MRP is superior to TBE in reducing pain and improving function.
Keywords: Chronic low back pain, Multifidus retraining, Segmental stabilization, Back exercises, Multifidus exercises
Introduction
A well aligned and flexible spine is important for an active and healthy life. Chronic low back pain (CLBP) is defined as back pain lasting more than 12 weeks [1]. This pain is a common musculoskeletal disorder affecting 80% of people some time in their lives [2]. The majority of lower back pain stems from benign musculoskeletal problems and is referred to as non-specific low back pain; it may be due to muscle or soft tissues sprain or strain [3], particularly in instances where pain arises suddenly during physical loading of the back, with the pain lateral to the spine. Over 99% of back pain instances fall within this category [4]. About 60%–80% of the population in industrialized countries like India, United States, Europe, Finland, and the Netherlands suffering from back pain; it is the second most common health problem after headache [5]. Stability of the spine is provided through ligaments and muscles of the back, lower back and abdomen.
Mechanical low back pain (MLBP) is a mechanically-derived, musculoskeletal back pain not involving nerve root compression or serious spinal diseases [6]. Prevalence is higher in young and active adults [7]. Causes of MLBP typically are attributed to an acute traumatic event, but they may also include cumulative trauma as an etiology [8]. The severity of an acute traumatic event varies widely, from twisting of the back to being involved in a motor vehicle collision. MLBP due to cumulative trauma tends to occur more commonly in the workplace. A systematic study review implicated a sedentary lifestyle, defined by the authors as including sitting for prolonged periods at work and during leisure time, as a risk factor for MLBP [9].
Low back pain (LBP) is usually self-limiting, with almost 90% of cases resolving within 6–12 weeks [10]. However, recurrence is high (84%) [11]. Risk factors for recurrence include weakness [11], excessive fatigability [12], lack of multifidus muscle recovery [13] and atrophy [13,14], which eliminate segmental stability.
Weakness of the superficial trunk and abdominal muscles is an important risk factor for LBP [15]. Strengthening these muscles markedly improves CLBP and decreases functional disability [16]. Another independent risk factor for CLBP is weakness and lack of motor control of deep trunk muscles, such as the lumbar multifidus (LM) and transversus abdominis (TrA) muscles [13,17]. Dysfunction of the LM crucially influences the etiology and recurrence of LBP [13,14,18]. Therefore, exercises to restore optimal LM function are a common aspect of current rehabilitation strategies [19,20]. More recently, attention has focused on the deepest fibers of the LM [17,20,21].
Understanding the anatomical structure that is painful differs from the disorder itself, and is important in order to give proper treatment. Thinking in the terms of integrated function and dysfunction might be more appropriate in diagnosis and treatment of back pain.
Therefore, in this study, we compared the efficacy of the multifidus retraining program (MRP) with conventional strengthening of abdominal and trunk muscles on pain and functional capacity in CLBP. Our hypothesis was that the MRP is more efficient than the muscle strength in the improvement of CLBP.
Materials and Methods
This study was approved by the ethical committee and research department of the Maharashtra Institute of Physiotherapy, Latur, India.
Thirty subjects (18 males and 12 females) who were computer professionals and who had at least a 2-year history of CLBP were selected and divided into two groups by purposive random sampling with 15 subjects (9 males and 6 females) in each group. One group (group A) was treated with traditional back exercise (TBE) and the other (group B) with MRP. All subjects completed the Handler 10-minute screening test for chronic back pain to rule out psychological pain. The inclusion criteria for the study were back pain felt between T12 and the gluteal folds that had lasted at least 3 months, age between 20 and 35 years, willingness to participate, ability to participate in an exercise program safely and no cognitive impairments that would limit their participation. The exclusion criteria were previous spinal surgery, trauma, rheumatologic disorders, spine infections, spine exercise training in the 3 months before the onset of the study, vertebral fracture, spinal abnormalities (scoliosis, kyphosis), inter vertebral disk prolapse, spondylolisthesis, pregnancy, malignancy, congenital abnormalities, ankylosing spondylitis, hernia, visceral problems, fibromyalgia and myofascial pain. Participants received a clear explanation of the study and provided their written informed consent.
1. Procedures
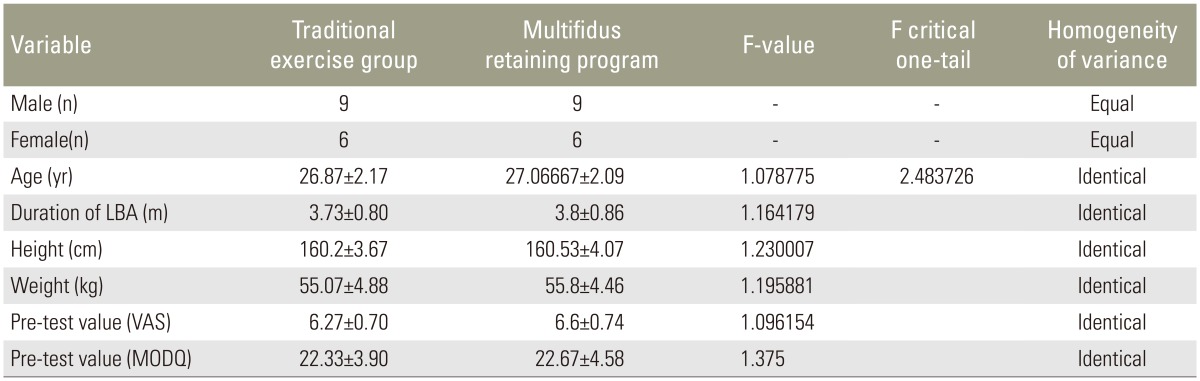
Demographic data including age, sex, height and weight were documented for descriptive statistical analysis (Table 1). The subjects were familiarized with the Oswestry disability questionnaire and visual analogue scale (VAS) rating of pain. These instruments were designed to give information about the back pain, which affects their ability to manage in everyday life. The patients were asked to answer all questions by placing a mark in the one box that most closely described their present condition. The pre-test scoring of both the assessment tools were done and documented. Functional outcome and pain perception were assessed with Oswestry disability questionnaire and VAS, respectively. Subjects were then randomized to the two groups as describe above. Homogeneity of variance between the groups were identical in terms of age, height, weight, pre-VAS and Oswestry disability questionnaire (MODQ) score (Table 1).
Table 1. Demographic data and homogeneity of variance.
Values are presented as mean±standard deviation.
LBA, low back pain; VAS, visual analogue scale; MODQ, Oswestry disability questionnaire.
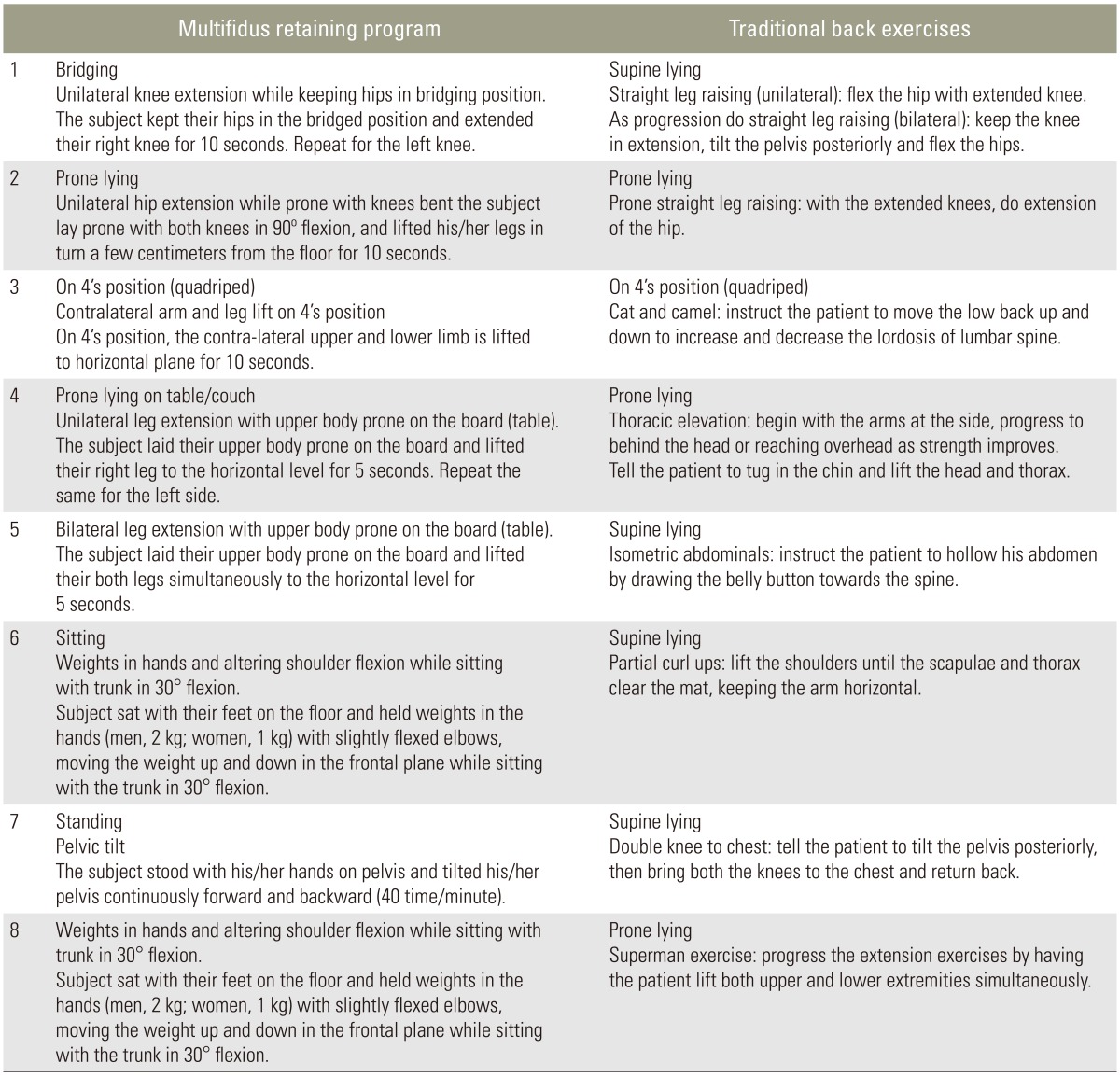
Both groups received exercise for 6 weeks. Based on the previous research [20,22], the exercises for MRP were designed to retrain the multifidus muscle. TBE consisted of strengthening and stretching of superficial abdominal and back muscles (Table 2). The exercise program was supervised by a physiotherapist in the outpatient department and the exercise register for each subject was maintained. Each exercise was meant to be repeated 20 times with a 5–8 seconds hold of each exercise. Exercise was on alternate days for 6 weeks. Subjects were allowed to rest for 2–4 minutes in between each set of exercise. The study was a pre-test and post-test experimental two group study. The subjects underwent pre-test at the starting of the study and the post-test was recorded after completion of the exercise program for 6 weeks.
Table 2. Exercise program.
2. Assessments
Assessment of severity of pain and functional disability was done at baseline and at the end of the treatment.
3. Pain
Pain was assessed using a VAS consisting of a 10 cm line, with the left extremity indicating "no pain" and the right extremity indicating "unbearable pain." Participants were asked to use the scale to indicate their current level of pain. Higher values suggested more intense pain. The pre- and post-exercise values of both MRP and TBE were documented and the mean and standard deviation (SD) was calculated for statistics.
4. Functional Disability
Functional disability was estimated by the Oswestry disability questionnaire, a functional scale assessing the impact of LBP on daily activities. There are many functional questionnaires available for the measurement and evaluation of LBP; we felt the Oswestry questionnaire was the most appropriate. The scoring was done by adding the values circled by the subject for each of the 10 individual questions and the disability is commanded as mild or no disability (0%–20%), moderate disability (21%–40%), severe disability (41%–60%), incapacity (61%–80%) and restricted to bed (81%–100%). The pre- and post-exercise values of the TBE and MRP groups were documented and the mean and SD was calculated and recorded for statistical analysis.
Results
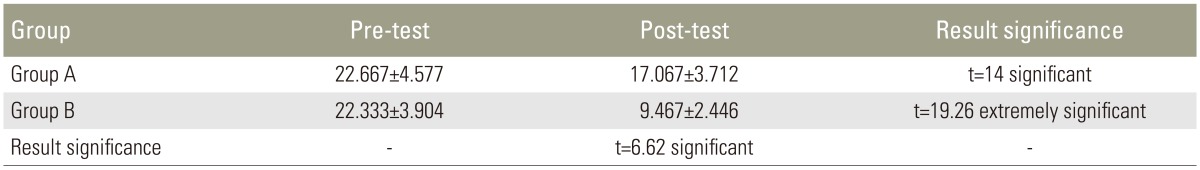
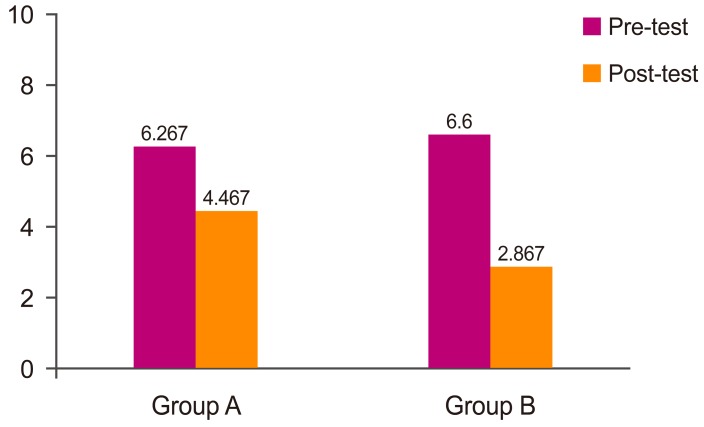
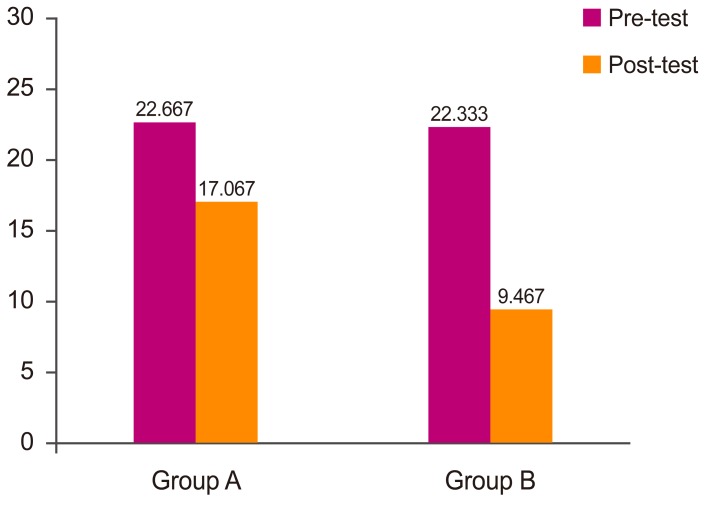
Statistical analysis was done using the SPSS ver. 16 (SPSS Inc., Chicago, IL, USA) software to find the average and the standard deviation of age, duration, height, weight, VAS and disability score in both groups. "F" test was done identify the equality of the variance between the group and showed identical in all the above factors between the groups (Table 1). Analysis using paired t-test of pre and post value for both the groups showed significant improvement in both groups. Pain after exercise in group A (4.467) and group B (2.867) were analyzed using unpaired T-test value (6.32) at p≤0.001 levels. Similarly the functional disability after exercise in group A (17.067) and group B (9.467) were analyzed using unpaired T-test value (6.62) at p≤0.001 level showed that MRP produced greater improvement than TBE (Tables 3, 4, Figs. 1, 2).
Table 3. Data analysis and result of the VAS score between group A and B.
Values are presented as mean±standard deviation.
VAS, visual analogue scale.
Table 4. Data analysis and result of the ODQ disability score between group A and B.
Values are presented as mean±standard deviation.
ODQ, Oswestry disability questionnaire.
Fig. 1. Visual analogue scale. Group A, traditional back exercises; Group B, multifidus retraining exercises.
Fig. 2. Oswestry disability questionnaire. Group A, traditional back exercises; Group B, multifidus retraining exercises.
Discussion
This study aimed to compare the efficacy of MRP and TBE in the relief the pain and improving the functional disability of CLBP among computer professionals with an extended history of LBP. Both exercise regimens were effective in relieving pain and in decreasing functional impairment, but MRP provided better relief of pain and improved functional outcome in the CLBP patients.
Bergmark [13] categorized the trunk muscles in to local and global muscle system based on their main mechanical roles in stabilisation. The local muscles are capable of controlling the stiffness and intervertebral relationship of spinal segments and posture of lumbar spine [6,23]. The current focus of back pain rehabilitation has evolved from global to local muscle systems with the recognition that local muscles are important in control of segmental spinal stability. Evidence from biomechanical, morphological, histochemical, electromyography and muscle fiber studies has implicated the multificus muscles in 2/3 of the segmental stability of the spine.
Waddell et al. [24] concluded that LBP patients often avoid using their back in everyday life situations because of fear of pain and its consequences. We suspect that prolonged sitting posture at a computer workstation as well as lack of exercise that is the norm for many computer professionals may lead to the weakness of the multifidus muscle. This speculation is supported by previous findings findings that disuse leads to the atrophy of the back muscles especially the LM muscle, and an exercise program produces functional improvement [25,26]. Segmental instability may cause functional disorders and strain as well as pain [27]. Uni-segmental muscles of the lumbar spine, such as the multifidus muscle, may provide segmental control and are the primary segmental stabilizers of the spine in lumbar region [28]. One study identified selective atrophy of the LM after the first episode of back pain; the atrophy was unlikely to revert without specific training, and the lower muscular stability predisposed an individual to further episodes of LBP [17]. Our findings also support this view; the MRP group had better outcome in comparison with the generalized back exercise program. Both multifidus and transverse abdominis muscles have been suggested as primary stabilizers of the lumbar segment, minimizing compressive forces on spinal structures [29]. The inter-segmental LM is the most important muscle in the stabilization of spine [30]. Presently, poor endurance of the multifidus muscle was linked with increased recurrence of LBP.
Although many aspects of treatment for the LBP remain controversial, the superiority of active exercise to inactivity is uncontested [29]. Presently, both the active traditional and multifidus exercises were beneficial for LBP. Specific exercise treatment is more effective than other types of other conservative management of LBP [31]. We hypothesize that the pain and the disability in these patients may be due to the segmental instability caused by the weakness of LM muscles. A specific exercise program to retrain these weak muscle fibers improves the function.
MRP showed significant improvements in relieving pain and functional disability in this study and previous research [31] when compared to TBE. The better results of the MRP group may reflect the fact that this training program concentrates on the deep back segmental stabilizer muscle, the LM, which is week in professionals who sit for prolonged periods. The MRP regimen produced better pain reduction and functional improvement compared to TBE, which is consistent with the fact that the deep muscles provide segmental stability to the back. Subjects in the TBE group performed exercises to strengthen the superficial muscles of the abdomen and trunk. The resulting reduction of pain and improvement in the function ability of CLBP subjects is consistent with prior findings [16].
Even after pain remission in patients with LBP, proper deep muscle reestablishment often does not occur, with specific physical therapy focusing on those muscles being necessary [13]. Our findings suggest that both protocols are of clinical utility in the improvement of CLBP.
Conclusions
Both the MRP and TBE regimens reduced the pain and functional disability effectively in individuals with CLBP. The improvements were superior for those receiving MRP in computer professionals with CLBP.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
This study was approved by the ethical committee and research department of the Maharashtra Institute of Physiotherapy, Latur, India.
References
- 1.Rozenberg S. Chronic low back pain: definition and treatment. Rev Prat. 2008;58:265–272. [PubMed] [Google Scholar]
- 2.Lower Back Pain Fact Sheet [Internet] Bethesda: National Institute of Neurological Disorders and Stroke; 2016. [cited 2016 May 15]. Available from: http://www.ninds.nih.gov/disorders/backpain/detail_backpain.htm. [Google Scholar]
- 3.Lumbago [Internet] Dublin, Ireland: Medmedia Group; 2015. [cited 2016 May 15]. Available from: http://www.irishhealth.com/article.html?id=577&ss=Lumbago. [Google Scholar]
- 4.Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60:3072–3080. doi: 10.1002/art.24853. [DOI] [PubMed] [Google Scholar]
- 5.Brotzman SB, Wilk KE. Clinical orthopaedic rehabilitation. Philadelphia: Mosby; 2003. [Google Scholar]
- 6.Schuldiner I. The relationship between low back instability and low back pain. Alexandria: American Physical Therapy Association; 1998. [Google Scholar]
- 7.De Vitta A. A lombalgia e suas relacoes com o tipo de ocupacao, com a idade e o sexo. Rev Bras Fisioter. 1997;1:67–72. [Google Scholar]
- 8.Heuch I, Hagen K, Heuch I, Nygaard O, Zwart JA. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine (Phila Pa 1976) 2010;35:764–768. doi: 10.1097/BRS.0b013e3181ba1531. [DOI] [PubMed] [Google Scholar]
- 9.Chen SM, Liu MF, Cook J, Bass S, Lo SK. Sedentary lifestyle as a risk factor for low back pain: a systematic review. Int Arch Occup Environ Health. 2009;82:797–806. doi: 10.1007/s00420-009-0410-0. [DOI] [PubMed] [Google Scholar]
- 10.Skinner HB. Current diagnosis & treatment in orthopedics. New York: Lange; 2000. [Google Scholar]
- 11.Vleeming A. Movement, stability, and low back pain: the essential role of the pelvis. New York: Churchill Livingstone; 1997. [Google Scholar]
- 12.Donatelli R, Wooden MJ. Orthopaedic physical therapy. New York: Churchill Livingstone; 2001. [Google Scholar]
- 13.Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine (Phila Pa 1976) 1996;21:2763–2769. doi: 10.1097/00007632-199612010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976) 1994;19:165–172. doi: 10.1097/00007632-199401001-00009. [DOI] [PubMed] [Google Scholar]
- 15.Bayramoglu M, Akman MN, Kilinc S, Cetin N, Yavuz N, Ozker R. Isokinetic measurement of trunk muscle strength in women with chronic low-back pain. Am J Phys Med Rehabil. 2001;80:650–655. doi: 10.1097/00002060-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. 2004;107:176–190. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Richardson C, Hodges PW, Hides J Manipulation Association of Chartered Physiotherapists. Therapeutic exercise for lumbopelvic stabilization: a motor control approach for the treatment and prevention of low back pain. New York: Churchill Livingstone; 2004. [Google Scholar]
- 18.Hodges P, Holm AK, Hansson T, Holm S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976) 2006;31:2926–2933. doi: 10.1097/01.brs.0000248453.51165.0b. [DOI] [PubMed] [Google Scholar]
- 19.Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine (Phila Pa 1976) 2001;26:E243–E248. doi: 10.1097/00007632-200106010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Leo Rathinaraj AS, Sreeja MT, Arun B, Sundar KS, Premlal R. A surface electromyographic study to assess the effect of spinal segmental stabilization [multifidus] exercise program in chronic mechanical low back pain patients. Eur Orthop Traumatol. 2012;3:161–168. [Google Scholar]
- 21.Whittaker JL. Ultrasound imaging for rehabilitation of the lumbopelvic region: a clinical approach. New York: Churchill Livingstone; 2007. [Google Scholar]
- 22.Richardson CA, Jull GA. Concepts of assessment and rehabilitation for active lumbar stability. In: Boyling JD, Palastanga N, editors. Grieve's modern manual therapy. 2nd ed. London: Churchill Livingstone; 1994. pp. 705–720. [Google Scholar]
- 23.Richardson C. Therapeutic exercise for spinal segmental stabilization in low back pain scientific basis and clinical approach. New York: Churchill Livingstone; 1999. [Google Scholar]
- 24.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 25.Mayer TG, Smith SS, Keeley J, Mooney V. Quantification of lumbar function. Part 2: Sagittal plane trunk strength in chronic low-back pain patients. Spine (Phila Pa 1976) 1985;10:765–772. [PubMed] [Google Scholar]
- 26.Cooper RG, St Clair Forbes W, Jayson MI. Radiographic demonstration of paraspinal muscle wasting in patients with chronic low back pain. Br J Rheumatol. 1992;31:389–394. doi: 10.1093/rheumatology/31.6.389. [DOI] [PubMed] [Google Scholar]
- 27.Grieve GP. Lumbar instability. Physiotherapy. 1982;68:2–9. [PubMed] [Google Scholar]
- 28.Panjabi MM. The stabilizing system of the spine: Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5:383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Kankaanpaa M, Taimela S, Airaksinen O, Hanninen O. The efficacy of active rehabilitation in chronic low back pain: effect on pain intensity, self-experienced disability, and lumbar fatigability. Spine (Phila Pa 1976) 1999;24:1034–1042. doi: 10.1097/00007632-199905150-00019. [DOI] [PubMed] [Google Scholar]
- 30.Wilke HJ, Wolf S, Claes LE, Arand M, Wiesend A. Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine (Phila Pa 1976) 1995;20:192–198. doi: 10.1097/00007632-199501150-00011. [DOI] [PubMed] [Google Scholar]
- 31.O'Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976) 1997;22:2959–2967. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]