Abstract
Study Design
Retrospective case series.
Purpose
To determine whether symptoms predict surgical outcomes for patients with discogenic low back pain (DLBP).
Overview of Literature
Specific diagnosis of DLBP remains difficult. Worsening of pain on flexion is a reported symptom of DLBP. This study sought to determine whether symptoms predict surgical outcomes for patients with DLBP.
Methods
We investigated 127 patients with low back pain (LBP) and no dominant radicular pain. Magnetic resonance imaging was used to select patients with disc degeneration at only one level. If pain was provoked during discography, we performed fusion surgery (87 patients). Visual analogue scale score and responses to a questionnaire regarding symptoms including worsening of pain on flexion or extension were assessed. Symptom sites before surgery were categorized into LBP alone, or LBP plus referred inguinal or leg pain. We followed 77 patients (average 3.0 years) and compared symptoms before surgery with surgical outcome.
Results
Sixty-three patients with a good outcome showed postsurgical pain relief (≥60% pain relief) and 14 patients with a poor outcome did not (<60% pain relief). In patients with good outcomes, worsening of LBP was evident in 65% of cases on flexion and in 35% on extension. However, these findings were not significantly different from those in patients with poor outcomes. The percentage of patients with LBP alone was significantly lower and the percentage of patients with LBP plus referred inguinal or leg pain was significantly higher in the group with good surgical outcome compared with patients in the group with poor surgical outcome (p<0.05).
Conclusions
Worsening of pain on extension may be a symptom of DLBP. Surgical outcomes were superior in patients with both LBP and either referred inguinal or leg pain compared with those having LBP alone.
Keywords: Lumbar, Intervertebral disc, Surgery, Pain
Introduction
Human intervertebral disc degeneration is a cause of back pain. The pathomechanism is not fully understood. Pain mechanisms have been explored using animal models of disc degeneration, samples harvested from painful human discs, magnetic resonance imaging (MRI) studies, and biomechanical studies [1,2]. Painful discs are characterized by a confluence of innervation, inflammation, and mechanical hypermobility [1,2].
Surgery for discogenic low back pain (DLBP) is challenging. A systematic review of discography as a diagnostic test for spinal pain found that it is a useful tool to evaluate imaging and pain when identifying patients with chronic DLBP [3]. However, the reliability of discography remains controversial [4]. Furthermore, psychogenic factors influence outcomes of surgery in patients with DLBP [5,6].
Low back pain (LBP) may originate from intervertebral discs and a physical test has been reported [7,8]. LBP, referred inguinal pain, and referred leg pain are seen in patients with DLBP [9]. Animal and human studies have shown that intervertebral discs are innervated by neurons from several levels of dorsal root ganglia (DRG) [10,11]. LBP is usually exacerbated on sustained sitting or forward bending of the trunk, both of which increase intradiscal pressure [7]. However, the validity of this symptom is unclear if patients are limited to those selected with DLBP. Furthermore, it is unclear whether the site of pain predicts the outcomes of surgery for DLBP.
In the current study, we sought to determine the validity of worsening of LBP on flexion as a symptom in patients selected with DLBP, and whether physical symptoms predict the outcome of treatment by surgical fusion in these patients.
Materials and Methods
1. Patients
We investigated 127 patients with a chief complaint of LBP. Patients opted for surgical treatment due to non-effective conservative treatment. MRI was used to select patients with disc degeneration at only one level. We initially excluded patients who had severe spondylolysis or disc degeneration with two or multilevel lesions, patients who had spinal stenosis with radicular pain, and patients who had previously undergone spinal surgery. Patients were categorized as having degenerated, bulging, or protruding discs, as previously described [12] Disc degeneration and vertebral bone marrow change were classified according to the Pfirrmann and Modic grading, respectively [13,14]. Three observers blinded to the diagnosis classified and evaluated the degenerated intervertebral discs and vertebral bone marrow changes. In the absence of consensus, agreement between two of the observers was used to grade the degenerated discs.
2. Indication for surgery using discography
Discography of intervertebral discs at one level was performed using a standard posterolateral approach with a 22-gauge needle (Becton Dickinson, Franklin Lakes, NJ, USA) in all 127 patients examined. For discography, the needle was inserted into the center of the disc under fluoroscopic control. Isovist 240 (0.4–3.2 mL; Schering, Osaka, Japan) was injected into each disc until severe pain was provoked or until contrast medium leaked out of the disc into the spinal canal. If pain was provoked during the discography, the patient was selected for subsequent surgical treatment (87 patients). Forty patients were excluded because the discography did not provoke pain.
3. Surgery
Patients with disc degeneration at only one level as seen on MRI, or who were positive for pain provocation on discography, underwent anterior discectomy and fusion surgery. We first performed the discectomy, cut the endplate at a thickness of 2 mm on both sides, and performed interbody fusion using iliac bone. Forty seven patients underwent stand-alone anterior fusion and 40 patients underwent anterior fusion with percutaneous posterior pedicle screw fixation at one level. The method used was dependent on the date of surgery. If the patient did not show bone fusion on the final follow-up X-ray, they were excluded.
4. Pain scores
Visual analogue scale (VAS) scores before surgery and at final follow-up after surgery were recorded. A questionnaire regarding symptoms including worsening of pain on standing, sitting, flexion, and extension was completed by each patient before surgery. Symptom sites before surgery were divided into LBP alone, LBP plus referred inguinal pain, and LBP plus referred leg pain.
5. Good and poor outcomes after surgery
We considered the surgery effective if patients indicated ≤60% of their presurgical VAS score after surgery. We defined these surgical outcomes as good. If the patients indicated >60% of their presurgical VAS score, we defined the surgical outcomes as poor.
6. Statistical analyses
Data were compared using an unpaired t test, chi-squared test, and one-way analysis of variance for repeated measurements. A p<0.05 was considered significant.
Results
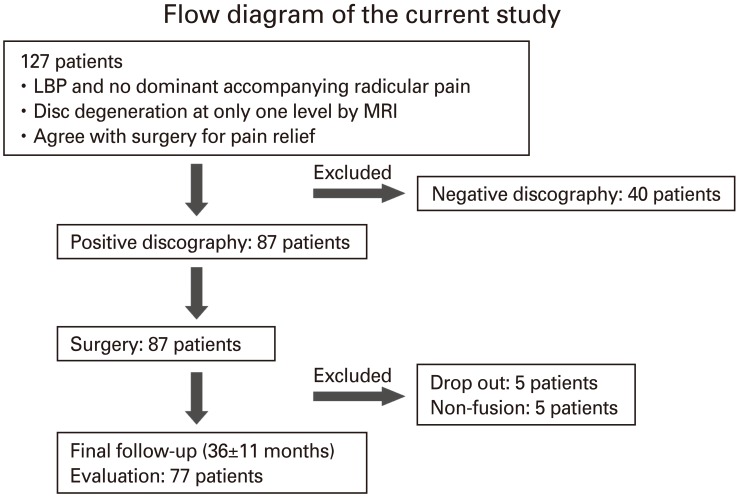
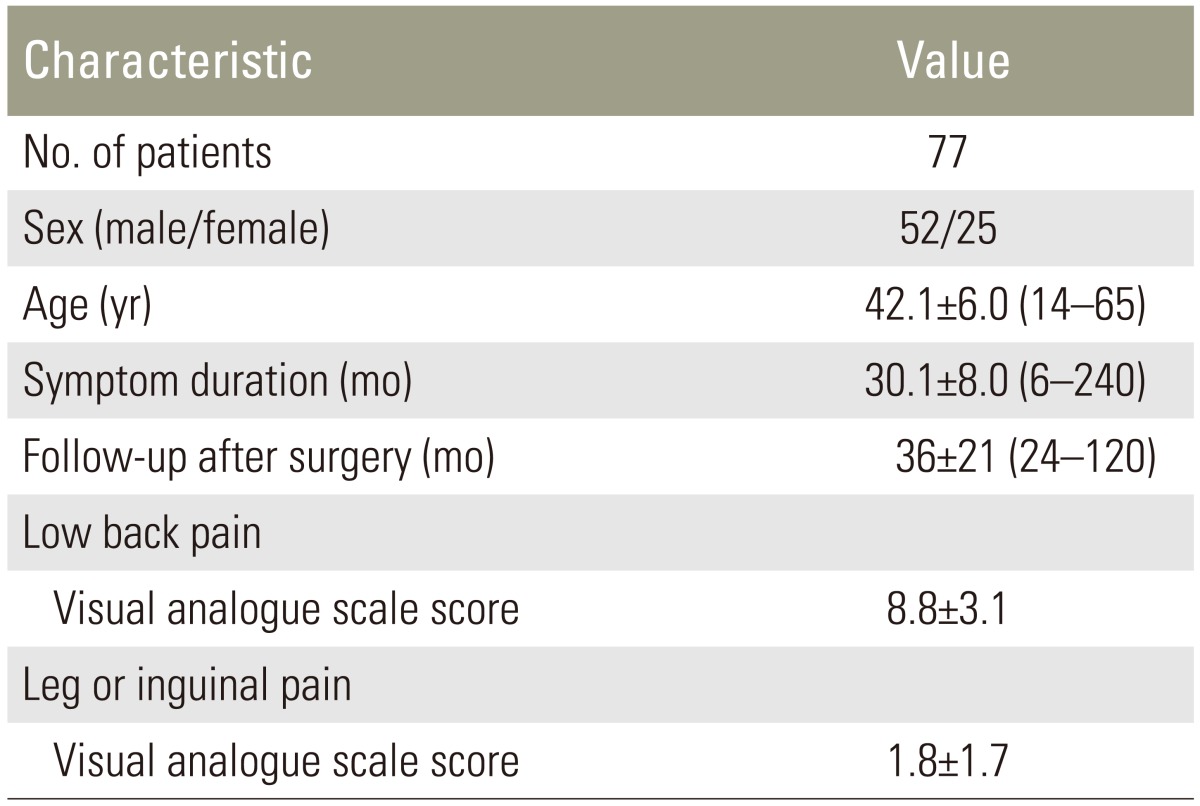
Fig. 1 shows a flow diagram of the study. A total of 127 patients with LBP and no dominant accompanying radicular pain were investigated. MRI was used to select patients showing disc degeneration at only one level. If pain was provoked during discography, we performed anterior interbody fusion surgery for patients in whom conservative therapy was not effective (87 patients, average age 42.1 years). At the final follow-up (36±11 months; mean±standard error of the mean, here and hereafter), five patients had dropped out because they failed to present at the hospital for unknown reasons. Five patients did not show solid fusion on X-ray films; they were excluded from evaluation. Ultimately, we evaluated the data from 77 patients. Table 1 shows the demographic characteristics of these 77 patients before surgery. Average LBP assessed using VAS score was 8.8±3.1 in 77 patients and referred leg or inguinal pain was 1.8±1.7 in 47 patients.
Fig. 1. Flow diagram of the study. LBP, low back pain; MRI, magnetic resonance imaging.
Table 1. Demographic characteristics.
Values are presented as mean (range).
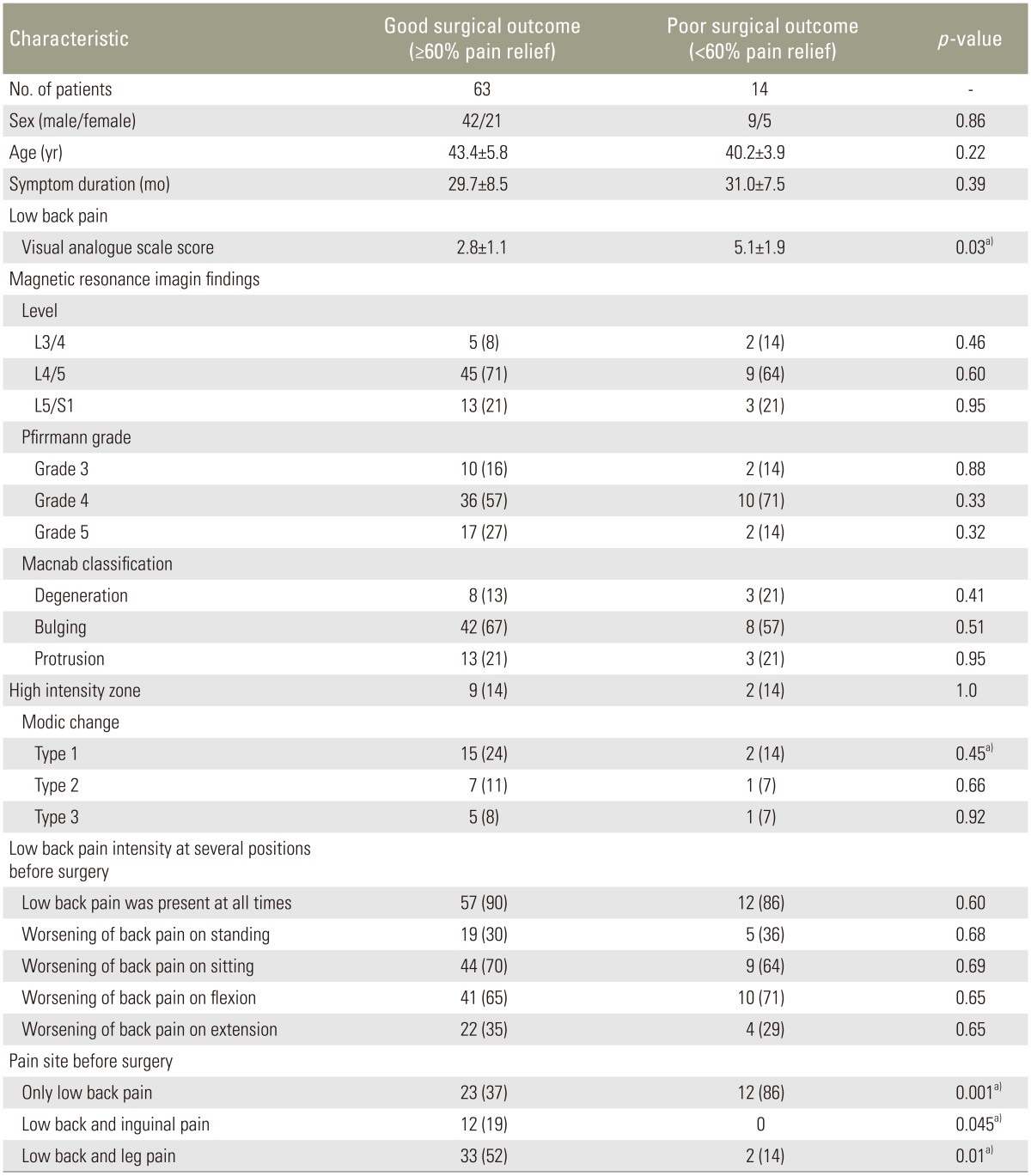
Table 2 shows data at final follow-up. Average VAS score was significantly improved after surgery. Sixty three patients indicated ≤60% of their presurgical VAS score after surgery (good outcome group). Fourteen patients indicated >60% of their presurgical VAS score after surgery (poor outcome group). There was no significant difference in the groups in the duration of symptoms before surgery, average age, or sex. We evaluated MRI findings in both groups before surgery. Between the two groups, there was also no significant difference in the level of the degenerated disc, disc degeneration based on the Pfirrmann grade, morphology of the disc based on the Macnab classification, or existence of a high intensity zone. However, there was significant difference in vertebral bone marrow change (Modic type 1) based on Modic's classification between two groups (p<0.05).
Table 2. Relation between surgical outcome, imaging, and symptom before surgery.
Values are presented as mean range or number (%).
a)A p<0.05 was considered significant.
Patients in groups with either good or poor outcome had intense LBP in several body positions before surgery. Presurgically, 90% of patients in the group with good surgical outcome had LBP present at all times, 30% of patients had worsening of LBP on standing, 70% on sitting, 65% on flexion, and 35% on extension. This pattern was similar in the group of patients with poor outcome. Therefore, differences in these symptoms did not predict surgical outcome (p>0.05). However, if the group with good outcome was defined as having true DLBP, worsening of back pain on extension was a symptom of DLBP.
Before surgery, 37% of patients in the group with good surgical outcome showed LBP alone, 19% showed low back and referred inguinal pain, and 52% showed low back and referred leg pain. The percentage of patients with LBP alone was significantly lower, and the percentage of patients with LBP plus referred inguinal or leg pain was significantly higher in the group with good surgical outcome compared with patients in the group with poor surgical outcome. We found less improvement of LBP after surgery in the group with LBP alone compared with patients with LBP plus referred inguinal or leg pain (p<0.05).
Discussion
Before surgery, worsening of LBP was found in 65% of patients in the group with good surgical outcomes on flexion, and in 35% on extension. Symptoms, such as worsening of back pain on flexion, extension, standing, or sitting, did not predict surgical outcome. However, surgical outcome was superior in patients with both LBP and either referred inguinal or leg pain compared with those with LBP alone.
Although discography is considered a useful diagnostic tool to identify patients with chronic discogenic LBP [3], discography is not highly predictive for identifying bona fide isolated intradiscal lesions primarily causing serious chronic LBP illness [4]. To avoid misdiagnosis before surgery, we selected patients with disc degeneration at a single level as seen on MRI, together with positive pain provocation on diagnostic discography. Furthermore, we categorized patients into those with either good or poor surgical outcome after fusion surgery. We consider that patients with a good or effective surgical outcome can be defined as having had true DLBP, and symptoms before surgery in patients from the group with an effective outcome may be reliable for albeit retrospective diagnosis of DLBP. We defined the surgery as effective if patients indicated ≤60% of their presurgical VAS score after surgery, and considered such patients as having had successful surgery. This criterion may not be definitive, however, we consider it better for the diagnosis of true DLBP compared with discography alone.
Many physicians consider an increase of back pain on flexion as a sign of DLBP. One study measured intervertebral intradiscal pressure in subjects in several positions and reported high pressure in the sitting and flexion positions [7]. These findings are consistent with the finding that back pain is usually exacerbated on sustained sitting or forward bending of the trunk [7,8]. In the current study, worsening of LBP was evident on standing in 30% of patients from the group with good surgical outcome, in 70% on sitting, in 65% on flexion, and in 35% on extension. These findings are similar to those of the aforementioned study. However, 35% of patients showed worsening of LBP on extension. We did not discern any significant difference in the outcomes of fusion surgery based on worsening of LBP in any of the various body positions before surgery. We conclude that pain worsens in various body positions in DLBP, but that any change in pain at various positions did not suggest improvement of surgical outcome.
Why does extension induce worsening pain in DLBP? Possibly because more sensory nerve fibers innervate the dorsal portion of the disc, compared with anterior portion of the disc [1]. MRI shows that the posterior disc contour abnormality is smaller in a flexion than in a neutral position, and larger in an extension position than in a neutral position [15]. The McKenzie exercise is an extension exercise used to evaluate patients with LBP. In one study, half of patients with DLBP were able to complete the McKenzie exercise. However, some were unable to complete the full range of extension during this exercise [16]. A full McKenzie physical evaluation was not tolerated in 36% of patients with DLBP diagnosed by discography. Furthermore, about half of the patients with DLBP were unable to benefit from the McKenzie evaluation [17].
In the current study, patients showed LBP alone or LBP plus referred inguinal or leg pain. However, the outcome of fusion surgery for patients with LBP plus referred inguinal or leg pain was superior to that in patients with LBP alone. The dorsal portion of the rat L5–6 disc is multisegmentally innervated by neurons from the T13 to L6 DRG [1,10]. Most of the sensory neurons innervating the L5–6 disc derive from the L2 DRG [1,10]. Blockade of the spinal nerves at the same level as the degenerated disc is effective for some patients with DLBP, but for other patients, blockade of L2 spinal nerves is effective [8,11]. Referred inguinal pain is seen in some patients with DLBP, and this symptom disappears after lumbar interbody fusion [9]. Referred inguinal or leg pain may originate from an intervertebral disc and these symptoms may help to distinguish true DLBP from other types of LBP.
Modic type 1 or 2 vertebral changes are associated with better surgical outcomes in patients with DLBP [18,19]. A randomized trial of disc prosthesis and rehabilitation in 154 patients having chronic DLBP for at least 1 year found patients with disc degeneration and Modic type 1 and 2 changes had a better surgical outcome compared with patients with rehabilitation alone [18]. Patients with chronic LBP, degenerated discs, and Modic type 1 changes undergoing fusion, had a more favorable outcome than those with no Modic change [19]. In the current study, there was no significant difference in the level of the degenerated disc, disc degeneration based on the Pfirrmann grading system, morphology of disc based on Macnab's classification, or existence of high intensity zone between patients in the group with good surgical outcome and patients in the group with poor outcome. However, there was significant difference in vertebral bone marrow change based on Modic's classification (Type 1) between patients in the group with good surgical outcome and patients in the group with poor outcome. Further study with more patients is needed to clarify this point.
There are some limitations to the current study. A systematic review showed factors such as smoking, long duration of LBP, long-term sick leave, comorbidity, depression, and work satisfaction have been identified as predictors of a poor outcome after spine surgery [5]. At the 12-months follow-up, patients with a good outcome have shown a marked improvement in their psychological status, while those with a poor outcome worsened [6]. We did not evaluate psychological status. Second, there is a possibility that pain seen in the current study originated from facet joints. However, we did not infiltrate the facet joints with anesthetic to determine whether pain originated from facet joints. Interbody fusion may be ineffective for facet joint pain.
Conclusions
Diagnosis of DLBP strictly based on MRI, discography outcomes, and surgical outcomes yielded 65% of patients with DLBP who showed worsening of LBP on flexion and 35% who showed worsening of LBP on extension. Surgical outcomes were superior in patients with both LBP and either referred inguinal or leg pain compared with those having LBP alone.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Ohtori S, Inoue G, Miyagi M, Takahashi K. Pathome-chanisms of discogenic low back pain in humans and animal models. Spine J. 2015;15:1347–1355. doi: 10.1016/j.spinee.2013.07.490. [DOI] [PubMed] [Google Scholar]
- 2.Lotz JC, Ulrich JA. Innervation, inflammation, and hypermobility may characterize pathologic disc degeneration: review of animal model data. J Bone Joint Surg Am. 2006;88(Suppl 2):76–82. doi: 10.2106/JBJS.E.01448. [DOI] [PubMed] [Google Scholar]
- 3.Buenaventura RM, Shah RV, Patel V, Benyamin R, Singh V. Systematic review of discography as a diagnostic test for spinal pain: an update. Pain Physician. 2007;10:147–164. [PubMed] [Google Scholar]
- 4.Carragee EJ, Lincoln T, Parmar VS, Alamin T. A gold standard evaluation of the "discogenic pain" diagnosis as determined by provocative discography. Spine (Phila Pa 1976) 2006;31:2115–2123. doi: 10.1097/01.brs.0000231436.30262.dd. [DOI] [PubMed] [Google Scholar]
- 5.den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15:527–536. doi: 10.1007/s00586-005-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Havakeshian S, Mannion AF. Negative beliefs and psychological disturbance in spine surgery patients: a cause or consequence of a poor treatment outcome? Eur Spine J. 2013;22:2827–2835. doi: 10.1007/s00586-013-2822-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nachemson AL. The lumbar spine an orthopaedic challenge. Spine. 1976;1:59–71. [Google Scholar]
- 8.Nakamura SI, Takahashi K, Takahashi Y, Yamagata M, Moriya H. The afferent pathways of discogenic low-back pain: evaluation of L2 spinal nerve infiltration. J Bone Joint Surg Br. 1996;78:606–612. [PubMed] [Google Scholar]
- 9.Oikawa Y, Ohtori S, Koshi T, et al. Lumbar disc degeneration induces persistent groin pain. Spine (Phila Pa 1976) 2012;37:114–118. doi: 10.1097/BRS.0b013e318210e6b5. [DOI] [PubMed] [Google Scholar]
- 10.Ohtori S, Takahashi K, Chiba T, Yamagata M, Sameda H, Moriya H. Sensory innervation of the dorsal portion of the lumbar intervertebral discs in rats. Spine (Phila Pa 1976) 2001;26:946–950. doi: 10.1097/00007632-200104150-00020. [DOI] [PubMed] [Google Scholar]
- 11.Ohtori S, Nakamura S, Koshi T, et al. Effectiveness of L2 spinal nerve infiltration for selective discogenic low back pain patients. J Orthop Sci. 2010;15:731–736. doi: 10.1007/s00776-010-1538-1. [DOI] [PubMed] [Google Scholar]
- 12.Macnab I. Spondylogenic backache: Soft tissue lesions. In: Macnab I, editor. Backache. Baltimore: Williams & Wilkins; 1977. pp. 91–96. [Google Scholar]
- 13.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 15.Zamani AA, Moriarty T, Hsu L, et al. Functional MRI of the lumbar spine in erect position in a superconducting open-configuration MR system: preliminary results. J Magn Reson Imaging. 1998;8:1329–1333. doi: 10.1002/jmri.1880080622. [DOI] [PubMed] [Google Scholar]
- 16.Donelson R, Silva G, Murphy K. Centralization phenomenon: its usefulness in evaluating and treating referred pain. Spine (Phila Pa 1976) 1990;15:211–213. [PubMed] [Google Scholar]
- 17.Laslett M, Oberg B, Aprill CN, McDonald B. Centralization as a predictor of provocation discography results in chronic low back pain, and the influence of disability and distress on diagnostic power. Spine J. 2005;5:370–380. doi: 10.1016/j.spinee.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Hellum C, Johnsen LG, Gjertsen O, et al. Predictors of outcome after surgery with disc prosthesis and rehabilitation in patients with chronic low back pain and degenerative disc: 2-year follow-up. Eur Spine J. 2012;21:681–690. doi: 10.1007/s00586-011-2145-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esposito P, Pinheiro-Franco JL, Froelich S, Maitrot D. Predictive value of MRI vertebral end-plate signal changes (Modic) on outcome of surgically treated degenerative disc disease: results of a cohort study including 60 patients. Neurochirurgie. 2006;52:315–322. doi: 10.1016/s0028-3770(06)71225-5. [DOI] [PubMed] [Google Scholar]