Abstract
Aims
Morbidity and mortality from drug overdose has decreased over three decades. This is credited to safer drugs and therefore better outcomes in overdose. We aimed to investigate changing prescriptions of antipsychotic medications and associated changes in antipsychotic overdoses over a 26‐year period.
Methods
All antipsychotic poisoning presentations to a tertiary referral toxicology unit between 1987 and 2012 were reviewed. Data were collected prospectively on demographics, ingestion information, clinical effects, complications and treatment. Rates of antipsychotic drug use in Australia were obtained from Australian government publications for 1990–2011 and linked to overdose admissions by postcode.
Results
There were 3180 antipsychotic overdoses: 1235 first generation antipsychotics, 1695 ‘atypical’ second generation antipsychotics and 250 lithium overdoses. Over 26 years, antipsychotic overdoses increased 1.8‐fold, with first generation antipsychotics decreasing to one‐fifth of their peak (≈80/year to 16) and second generation antipsychotics increasing to double this (≈160/year), olanzapine and quetiapine accounting for 78%. All antipsychotic overdoses had a median length of stay of 18.6 h, 15.7% admitted to intensive care unit, 10.4% ventilated and 0.13% died in hospital, which was the same for first generation compared to second generation antipsychotics. There was a 2.3‐fold increase in antipsychotic prescriptions over the same period; first generation antipsychotics declined whereas there was a dramatic rise in second generation antipsychotics, mainly olanzapine, quetiapine and risperidone (79%).
Conclusion
Over 26 years there was an increase in antipsychotic prescribing associated with an increase in antipsychotic overdoses. Although the type of antipsychotics changed, the morbidity and mortality remained the same, so that antipsychotics are an increasing proportion of overdose admissions.
Keywords: antipsychotics, epidemiology, drug overdose, poisoning
What is Already Known about this Subject
There has been a trend to prescribing drugs that are perceived as ‘safer’ to patients at risk of self‐harm
Many antipsychotic medications are prescribed for off‐label conditions
The adolescent age group in particular has seen an increase in antipsychotic medication usage
What this Study Adds
There has been a rapid rise in prescriptions of antipsychotic medication in Australia over the last 30 years
This increase is associated with an increase in admission for antipsychotic self‐poisoning
Although the ‘newer’ second generation antipsychotics are perceived as ‘safer’, there has been no reduction in morbidity or in‐hospital mortality from antipsychotic poisonings
Introduction
Deliberate self‐poisoning continues to be a major problem worldwide. The availability of medications, poisons and prescription trends are recognized important influences on the type of toxin taken in deliberate self‐poisoning, but other factors are also important. Antidepressant prescriptions changed from highly toxic tricyclic antidepressants to much less toxic selective serotonin reuptake antagonists, which significantly decreased the mortality and morbidity of antidepressant overdose 1, 2. However, despite massive increases in antidepressant prescriptions, there were smaller increases in numbers of antidepressant overdoses 2, an observation more difficult to explain. There have also been changes with other psychotropic medications, including second generation antipsychotics, anticonvulsants and anxiolytics. Only some of these have been demonstrated to lead to decreased toxicity in overdose (e.g. benzodiazepines replacing barbiturates as anxiolytics and sleeping tablets 3), and there is less information on the influence of prescription practices on deliberate self‐poisoning for these agents.
The toxicity profile of antipsychotics has potentially altered with the introduction of the newer ‘atypical’ or second generation antipsychotics and subsequent changes in prescription patterns. This may have improved side‐effect profiles, for example reduced extra‐pyramidal side‐effects 4. However, there is little information on the effect this change has had on rates of morbidity from deliberate self‐poisoning from these second generation antipsychotics.
We aimed to investigate the changing prescription trends of antipsychotic medications and compare this to the epidemiology of antipsychotic overdose for a 26‐year period in Greater Newcastle, Australia, where there is complete capture of deliberate self‐poisoning cases. We hypothesized that a switch to second generation antipsychotics would decrease the morbidity from antipsychotic overdoses.
Methods
This was a cohort study of consecutive presentations for an antipsychotic overdose treated by the Hunter Area Toxicology Service from January 1987 to December 2012. The Hunter Area Toxicology Service is a tertiary adult (>16 years of age) referral service for all toxicology admissions to feeder hospitals for a population over 500 000. All presentations are prospectively recorded using a fully relational Microsoft Access database separate from the hospital's main medical record system. Patient characteristics (age, sex, postcode) and clinical data (drug, dose and time of ingestion, co‐ingested substances, clinical effects, laboratory investigations and details of management and complications) are recorded on a proforma sheet on admission by emergency staff. The clinical history is collected again by a member of the toxicology team during the patient admission. Additional information including length of stay (LOS) and any complications (admission to intensive care unit [ICU], use of mechanical ventilation and death) are reviewed and recorded at a weekly meeting.
For this study, data were extracted from the database for all antipsychotics, including first and second generation antipsychotics and lithium. An overdose was defined as any deliberate self‐poisoning admission, or a small number of poisonings with therapeutic intent where patients took more than the recommended dose. If patients ingested more than one antipsychotic in overdose, these events were included as separate overdose admissions for this analysis.
Rates of antipsychotic drug use (standardized by the defined daily dose [DDD]) in Australia were obtained from Australian government publications for 1990 to 2011 and compared to the trends in overdose admissions over the same period 5. To allow this comparison, the analyses of population referenced data (i.e. rates) were restricted by postcode. The changes in total self‐poisoning within the four statistical subdivisions within this area were examined between 1991 and 2011.
The 95% confidence intervals were calculated with the Wilson's procedure with a continuity correction 6. Continuous variables were reported with a median and interquartile ranges, or ranges. All statistical and graphic analyses were conducted in GraphPad Prism (version 6; GraphPad Software, San Diego, CA).
Results
There were 3180 antipsychotic overdose admissions between 1987 and 2012, including 250 lithium poisonings (analytically confirmed in 208 [83%] of cases), 1695 newer second generation antipsychotic overdoses and 1235 first generation antipsychotic poisonings. The median age was 32 years (inter‐quartile range [IQR]: 24–41 years), 2081 were female (65.4%) and the median LOS was 18.6 h (IQR: 12.5–32.5h). Four patients died over this period, two from first generation antipsychotics (both thioridazine) and two from second generation antipsychotics (quetiapine and clozapine). No coingestants were taken in 155 of 1235 (12.6%) first generation antipsychotic poisonings and in 178 of 1695 (10.5%) second generation antipsychotic poisonings. Table 1 lists the 25 most common classes of drugs/toxins ingested with first generation compared to second generation antipsychotics.
Table 1.
List of the 25 most common drug classes ingested with first generation and second generation antipsychotics
| Coingestant class | First generation (%) | Second generation (%) |
|---|---|---|
| Benzodiazepines | 18.4 | 10.8 |
| Anticonvulsants | 10.1 | 12.2 |
| Alcohol | 7.8 | 10.8 |
| SSRIs | 7.7 | 12.7 |
| Other drugs | 6.4 | 6.4 |
| Paracetamol | 6.0 | 5.7 |
| TCAs | 5.5 | 1.2 |
| SNRIs | 5.0 | 9.6 |
| Antipsychotics (SGA) | 4.4 | — |
| Antipsychotics (FGA) | — | 3.9 |
| Anticholinergics | 4.4 | 1.4 |
| Lithium | 2.7 | 1.9 |
| Opioids | 1.9 | 2.5 |
| NSAIDs | 1.8 | 2.3 |
| Non‐therapeutic substances | 1.6 | 1.7 |
| MAOIs | 1.6 | 0.2 |
| Beta blockers | 1.6 | 1.5 |
| Antidepressants (other) | 1.5 | 3.7 |
| Sympathomimetics/amphetamines | 1.6 | 1.2 |
| Antibiotics | 1.1 | 0.4 |
| H2 antagonists | 1.0 | 0.2 |
| Antihistamines | 0.8 | 1.0 |
| Salicylates | 0.7 | 0.8 |
| ACE inhibitor | 0.7 | 0.8 |
| Statins | 1.1 | 0.4 |
Over the 26‐year period there was a 1.8‐fold increase in the number of antipsychotic overdose presentations per 100 000/population/year. Over the same time period there was a 2.3‐fold increase in total antipsychotic prescriptions. First generation antipsychotic prescribing declined (from 3.73 to 0.802 defined daily doses [DDD]/1000/day), whereas there was a dramatic rise in second generation antipsychotic prescriptions to 8.842 DDDs/1000/day, which mainly included olanzapine, quetiapine and risperidone (79% of total prescriptions) (Figures 1, 2).
Figure 1.
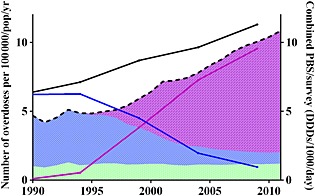
Changes in rates of use of antipsychotic drug groups and rates of antipsychotic overdoses. Shaded areas reflect prescription rates and lines reflect overdose presentations. Green represents lithium, blue first generation antipsychotics and purple atypical antipsychotics. (DDDs/1000/day = defined daily doses/1000 people/day). ( ) First generation antipsychotic overdoses, (
) First generation antipsychotic overdoses, ( ) Second generation antipsychotic overdoses, (
) Second generation antipsychotic overdoses, ( ) Total antipsychotic overdoses, (
) Total antipsychotic overdoses, ( ) Total antipsychotic prescriptions (shaded by class)
) Total antipsychotic prescriptions (shaded by class)
Figure 2.
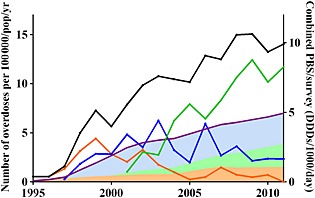
Changes in prescription rates of quetiapine, olanzapine and risperidone. Shaded areas reflect prescription rates and lines reflect overdose presentations. Black line represents total overdose data for quetiapine, olanzapine and risperidone, blue olanzapine, orange risperidone and green quetiapine. (DDDs/1000/day = defined daily doses/1000 people/day). ( ) Total OD data for quetiapine, risperidone and olanzapine, (
) Total OD data for quetiapine, risperidone and olanzapine, ( ) Olanzapine OD, (
) Olanzapine OD, ( ) Risperidone, (
) Risperidone, ( ) Quetiapine OD, (
) Quetiapine OD, ( ) Total all 3 prescription data
) Total all 3 prescription data
First generation antipsychotic overdoses decreased over the 26 years to one fifth of their early rate (from ≈80 to 16/year) with a total of 1235 presentations (Figure 1). The median age was 31 years (IQR: 25–40 years), 803 (65%) were female. The median LOS was 18.5 h (IQR: 13–32.2 h), 198 presentations (16%) were admitted to intensive care unit (ICU), 131 (10.6%) were ventilated and two (0.16%) died in hospital (Table 2).
Table 2.
Number (% of all drugs) of drugs usually obtained on prescription involved in self poisoning, and measures of morbidity (length of stay [median and interquartile range], intensive care unit (ICU) admission, ventilation, in‐hospital death)
| Drug | N (%) | LOS (h) | ICU (%) | Ventilated (%) | Deaths (%) |
|---|---|---|---|---|---|
| First generation | 1235 (3.6%) | 18.5 (13–32.2) | 198 (16.0%) | 131 (10.6%) | 2 (0.16%) |
| Atypical/newer | 1695 (4.9%) | 18 (11.9–29.9) | 259 (15.3%) | 178 (10.5%) | 2 (0.12%)* |
| Quetiapine | 899 (2.6%) | 17.8 (11.8–29.7) | 132 (14.7%) | 99 (11%) | 1 (0.1%) |
| Olanzapine | 422 (1.2%) | 20 (14–36.3) | 80 (19%) | 59 (14%) | 0 |
| Risperidone | 216 (0.6%) | 16.3 (6.5–21.5) | 14 (6.5%) | 7 (3.2%) | 0 |
| Lithium | 250 (0.7%) | 25.2 (14.9–69.6) | 42 (16.8%) | 22 (8.8%) | 0 |
| Total antipsychotics | 3180 (9.3%) | 18.6 (12.5–33.5) | 499 (15.7%) | 331 (10.4%) | 4 (0.13%) |
The second death from second generation antipsychotics was clozapine.
Second generation antipsychotic overdoses increased beginning in 1994, to recently double the early rate of first generation antipsychotics (≈160/year) with a total of 1695 presentations (Figure 1). Their median age was 32 years (IQR: 24–41 years), 1112 (65.6%) were female. The median LOS was 18 h (IQR: 12–30 h), 259 (15%) were admitted to the ICU and 178 (10.5%) ventilated with two (0.1%) deaths in hospital (Table 2). There was no significant difference between the LOS for first and second generation antipsychotics (P = 0.223; Mann‐Whitney test), and no significant difference in the proportion admitted to ICU (P = 0.615; χ2 test) or mechanically ventilated (P = 0.975; χ2 test). The drugs involved and the cause of death for the four patients that died is shown in Table 3.
Table 3.
Details of the four deaths from antipsychotic overdose
| Age/Sex | Antipsychotic | Coingestants | Description and cause of death |
|---|---|---|---|
| 70/F | Thioridazine* | Benztropine*, Clonazepam | Found unconscious and had multiple cardiac arrests in hospital. Extubated day 4 but persistent vegetative state and died two days later. Old myocardial infarct on post‐mortem. |
| 70/M | Thioridazine* | Nil | Found unconscious, multiple episodes of ventricular tachycardia/fibrillation, hypoxic brain injury, died 25 days later from pneumonia. |
| 25/M | Clozapine* | Nil | Coma, seizures within 2 h and then cardiac arrest and died despite resuscitation in the emergency department. |
| 31/M | Quetiapine* | Nil | Admitted with decreased level of consciousness. Over 10 h increasing respiratory depression, seizure and asystolic cardiac arrest. |
Confirmed analytically.
Quetiapine and olanzapine made up 78% of the second generation antipsychotic overdoses (899 and 422 presentations respectively). A comparison of the LOS, ICU admissions, ventilation and deaths for quetiapine, olanzapine and risperidone are detailed in Table 2. The LOS, ICU admission rate, ventilation rate for quetiapine and olanzapine were similar to all other antipsychotics, but the ICU admission and ventilation rate were lower for risperidone.
Discussion
Our results show that there has been an increase in admissions to our toxicology unit of antipsychotic poisonings over the study period. Over the same time period there has been an increase in the prescription of antipsychotic medications, in particular the newer second generation antipsychotics, mainly quetiapine and olanzapine. More importantly, our study shows the morbidity and in‐hospital mortality is the same for first and second generation antipsychotic poisonings. Therefore, the change from first generation to second generation antipsychotic overdose presentations and prescriptions has resulted in an absolute increase in overdose morbidity because the absolute numbers of antipsychotic overdoses has increased and the morbidity of antipsychotic poisoning remained unchanged.
Our study found that the type of antipsychotic (first or second generation) did not influence factors such as LOS, intensive care admission, ventilation and in‐hospital death. In a retrospective review of the Californian Poisons Center data 7, there were also increasing presentations of second generation antipsychotic overdoses between 1997 and 2006, but in contrast to our study, they reported higher rates of major adverse effects and death with the second generation agents. The reason for this is unclear but may be related to the smaller sample of first generation antipsychotics in their study, because it only included 10 years of data.
In addition to the generation of antipsychotic, we compared the outcomes for the three most common second generation antipsychotics: quetiapine, olanzapine and risperidone. We found that there was a difference between the second generation antipsychotics, with a much higher rate of ICU admission and ventilation for quetiapine and olanzapine compared to risperidone. This is likely to be because risperidone is rarely associated with central nervous system depression and coma, but is associated with more cases of extra‐pyramidal side‐effects 8.
The use and prescription of antipsychotic medication in Western countries, including Europe (although less so in France) and North America, has rapidly increased over the last two decades in adult, adolescent and paediatric populations 9, 10, 11, 12, 13, 14. Such a dramatic shift has sparked much debate about the appropriate use and need for antipsychotic medication, and current research has shown a large number of prescriptions are for off‐label use 9, 11, 15. Increasingly, antipsychotic medication is being prescribed to treat sleeping disorders, anxiety and mood disorders. The increased trend in prescriptions has appeared to correlate with the introduction of the newer second generation antipsychotic medication, with a perception that these are relatively ‘safe’ medications and marketed as such with fewer side‐effects, such as extra‐pyramidal effects 4. However, there is legitimate concern about the toxicity of these medications, including in therapeutic use 16, 17, in overdose 7, 18, 19, 20 and when abused 21, 22, 23, all of which are not always evident at the time of marketing. Olanzapine has been recognized as a major worry because it causes weight gain, alters glucose and lipid metabolism and may result in an increased risk of diabetes 16. This additional metabolic dysfunction only adds to the already increased risk of cardiac and metabolic disease associated with a diagnosis of schizophrenia 17. Some of these drugs have the potential for abuse, possibly because they are relatively safe and easy to access. This has been reported within prisons, by drug and alcohol services and emergency department presentations 21, 22, 23.
Our study adds to concerns about toxicity and shows that the morbidity and mortality from antipsychotic poisonings has not decreased, while the absolute numbers have almost doubled. There are no regulatory requirements for the pharmaceutical industry to study new drugs in overdose, even for psychiatric drugs, which are prescribed to a population of people at increased risk of deliberate self‐harm. There is thus generally a long delay until the consequences of poisoning with each new agent become apparent 24.
Although experience with antidepressant prescriptions and poisonings has been reassuring 2, with a steady reduction in the morbidity and mortality of antidepressant overdose 1, 2, 25, this pattern does not appear the same for antipsychotic medication. Similar to antidepressant medication, there has been a switch in prescribing from older to newer antipsychotic agents, and the rate of antipsychotic prescribing has increased significantly (2.3‐fold). However, in contrast to antidepressants, there has been a nearly proportional increase in antipsychotic overdoses over the same period as the increase in prescriptions. Adding to this, our finding that the second generation antipsychotics appear to be no safer in overdose than the first generation ones, there has been an increased burden of serious overdose presentations with antipsychotics.
Lithium was included in the study because it is classified as an antipsychotic by the World Health Organization. More importantly, the prescription rate and overdose rate of lithium was stable over the study period (Figure 1), providing evidence that there were no other systematic factors that influenced the changes in prescribing and overdose of the first and second generation antipsychotics.
Limitations of our study include selection and referral bias to a single site, which may include bias against less severe poisonings (patients not presenting or not being referred). There were no private emergency departments in this region during the period of the study, negating any loss to non‐public hospitals. Data on all admissions are collected prospectively, but review of cases is retrospective. All histories are collected at least twice by the attending clinicians, and although drug assays are not routinely performed, previous evidence suggests that patient history correlates with the drug taken in the vast majority of cases 26, 27.
A potential major limitation of the study was the large number of cases where a coingestant was taken, almost 90% for both first and second generation antipsychotics. However, Table 1 suggests that the types of coingestants were similar for first and second generation antipsychotics. The exceptions to this are other drug classes with changes over the period of the study, the main group being antidepressants. We have already demonstrated that the toxicity of antidepressants has decreased over time, further reinforcing the fact that the second generation antipsychotics are not less toxic in overdose.
A further limitation of the study is the lack of data regarding out of hospital deaths involving antipsychotic use. This may be important because changes in antipsychotics may increase or decrease early deaths, which may not affect hospital deaths. However, the shift towards selective serotonin reuptake inhibitor medication in the treatment of depression not only reduced mortality and morbidity in hospital, studies from the United Kingdom also clearly show these were mirrored in reduced out‐of‐hospital deaths 28.
Over the last two decades there has been an increase in antipsychotic prescribing associated with an increase in antipsychotic overdoses. Although the type of antipsychotics has changed during this time, there has been no decrease in morbidity with the second generation agents. This means that antipsychotic overdoses make up an increasing proportion of the burden of poisoned patients. A prospective toxicovigilance strategy, collecting data on toxicity in overdose, would be desirable for new antipsychotic agents.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: GKI is supported by an NHMRC Senior Research Fellowship 1061041. This was supported by an NHMRC Program Grant 1055176; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Author contributions
IB, NB and GKI conceived the study design. IB undertook data collection. IB and GKI reviewed all data. IB drafted the manuscript, all authors contributed substantially to its revision. IB takes responsibility for the paper as a whole.
The authors acknowledge the help of the many doctors, nurses and staff of the Calvary Mater Newcastle Emergency and Intensive Care units in the care and support of these patients.
Berling, I. , Buckley, N. A. , and Isbister, G. K. (2016) The antipsychotic story: changes in prescriptions and overdose without better safety. Br J Clin Pharmacol, 82: 249–254. doi: 10.1111/bcp.12927.
References
- 1. Stoner SC, Marken PA, Watson WA, Switzer JL, Barber MF, Meyer VL, Sommi RW Jr, Steele MT. Antidepressant overdoses and resultant emergency department services: the impact of SSRIs. Psychopharmacol Bull 1997; 33: 667–70. [PubMed] [Google Scholar]
- 2. Buckley NA, Whyte IM, Dawson AH, Isbister GK. A prospective cohort study of trends in self‐poisoning, Newcastle, Australia, 1987–2012: plus ça change, plus c'est la même chose. Med J Aust 2015; 202: 438–42. [DOI] [PubMed] [Google Scholar]
- 3. Buckley NA, McManus PR. Changes in fatalities due to overdose of anxiolytic and sedative drugs in the UK (1983–1999). Drug Saf 2004; 27: 135–41. [DOI] [PubMed] [Google Scholar]
- 4. Lieberman JA. Atypical antipsychotic drugs as a first‐line treatment of schizophrenia: a rationale and hypothesis. J Clin Psychiatry 1996; 57 (Suppl 11): 68–71. [PubMed] [Google Scholar]
- 5. Australian Statistics on Medicine 1991–2010 . Canberra: Commonwealth Department of Health & Ageing, 2013.
- 6. Newcombe RG. Two‐sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 1998; 17: 857–72. [DOI] [PubMed] [Google Scholar]
- 7. Ciranni MA, Kearney TE, Olson KR. Comparing acute toxicity of first‐ and second‐generation antipsychotic drugs: a 10‐year, retrospective cohort study. J Clin Psychiatry 2009; 70: 122–9. [DOI] [PubMed] [Google Scholar]
- 8. Page CB, Calver LA, Isbister GK. Risperidone overdose causes extrapyramidal effects but not cardiac toxicity. J Clin Psychopharmacol 2010; 30: 387–90. [DOI] [PubMed] [Google Scholar]
- 9. Verdoux H, Tournier M, Begaud B. Antipsychotic prescribing trends: a review of pharmaco‐epidemiological studies. Acta Psychiatr Scand 2010; 121: 4–10. [DOI] [PubMed] [Google Scholar]
- 10. Harrison JN, Cluxton‐Keller F, Gross D. Antipsychotic medication prescribing trends in children and adolescents. J Pediatr Health Care 2012; 26: 139–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pringsheim T, Gardner DM. Dispensed prescriptions for quetiapine and other second‐generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open 2014; 2: E225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Marston L, Nazareth I, Petersen I, Walters K, Osborn DP. Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open 2014; 4: e006135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Antia SX, Sholevar EH, Baron DA. Overdoses and ingestions of second‐generation antipsychotics in children and adolescents. J Child Adolesc Psychopharmacol 2005; 15: 970–85. [DOI] [PubMed] [Google Scholar]
- 14. Morrens M, Destoop M, Cleymans S, Van Der Spek S, Dom G. Evolution of first‐generation and second‐generation antipsychotic prescribing patterns in Belgium between 1997 and 2012: a population‐based study. J Psychiatr Pract 2015; 21: 248–58. [DOI] [PubMed] [Google Scholar]
- 15. Leslie DL, Mohamed S, Rosenheck RA. Off‐label use of antipsychotic medications in the Department of Veterans Affairs health care system. Psychiatr Serv 2009; 60: 1175–81. [DOI] [PubMed] [Google Scholar]
- 16. Newcomer JW. Second‐generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 2005; 19 (Suppl 1): 1–93. [DOI] [PubMed] [Google Scholar]
- 17. Ventriglio A, Gentile A, Stella E, Bellomo A. Metabolic issues in patients affected by schizophrenia: clinical characteristics and medical management. Front Neurosci 2015; 9: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morgan M, Hackett LP, Isbister GK. Olanzapine overdose: a series of analytically confirmed cases. Int Clin Psychopharmacol 2007; 22: 183–6. [DOI] [PubMed] [Google Scholar]
- 19. Isbister GK, Duffull SB. Quetiapine overdose: predicting intubation, duration of ventilation, cardiac monitoring and the effect of activated charcoal. Int Clin Psychopharmacol 2009; 24: 174–80. [DOI] [PubMed] [Google Scholar]
- 20. Isbister GK, Balit CR, Macleod D, Duffull SB. Amisulpride overdose is frequently associated with QT prolongation and torsades de pointes. J Clin Psychopharmacol 2010; 30: 391–5. [DOI] [PubMed] [Google Scholar]
- 21. Pilgrim JL, Drummer OH. The toxicology and comorbidities of fatal cases involving quetiapine. Forensic Sci Med Pathol 2013; 9: 170–6. [DOI] [PubMed] [Google Scholar]
- 22. Malekshahi T, Tioleco N, Ahmed N, Campbell AN, Haller D. Misuse of atypical antipsychotics in conjunction with alcohol and other drugs of abuse. J Subst Abuse Treat 2015; 48: 8–12. [DOI] [PubMed] [Google Scholar]
- 23. Mattson ME, Albright VA, Yoon J, Council CL. Emergency department visits involving misuse and abuse of the antipsychotic quetiapine: results from the Drug Abuse Warning Network (DAWN). Subst Abus 2015; 9: 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Buckley NA, Whyte IM, Dawson AH. Cardiotoxicity more common in thioridazine overdose than with other neuroleptics. J Toxicol Clin Toxicol 1995; 33: 199–204. [DOI] [PubMed] [Google Scholar]
- 25. McManus P, Mant A, Mitchell PB, Montgomery WS, Marley J, Auland ME. Recent trends in the use of antidepressant drugs in Australia, 1990–1998. Med J Aust 2000; 173: 458–61. [DOI] [PubMed] [Google Scholar]
- 26. Friberg LE, Isbister GK, Hackett LP, Duffull SB. The population pharmacokinetics of citalopram after deliberate self‐poisoning: a Bayesian approach. J Pharmacokinet Pharmacodyn 2005; 32: 571–605. [DOI] [PubMed] [Google Scholar]
- 27. von Mach MA, Weber C, Meyer MR, Weilemann LS, Maurer HH, Peters FT. Comparison of urinary on‐site immunoassay screening and gas chromatography‐mass spectrometry results of 111 patients with suspected poisoning presenting at an emergency department. Ther Drug Monit 2007; 29: 27–39. [DOI] [PubMed] [Google Scholar]
- 28. Handley SA, Flanagan RJ. Drugs and other chemicals involved in fatal poisoning in England and Wales during 2000–2011. Clin Toxicol (Phila) 2014; 52: 1–12. [DOI] [PubMed] [Google Scholar]


