Abstract
Background
Sulfadoxine–pyrimethamine (SP) is recommended for prophylactic treatment of malaria in pregnancy while artemisinin combination therapy is the recommended first-line anti-malarial treatment. Selection of SP resistance is ongoing since SP is readily available in health facilities and in private drug shops in sub-Saharan Africa. This study reports on the prevalence and distribution of Pfdhps mutations A540E and A581G in Tanzania. When found together, these mutations confer high-level SP resistance (sometimes referred to as ‘super-resistance’), which is associated with loss in protective efficacy of SP-IPTp.
Methods
DNA samples were extracted from malaria-positive blood samples on filter paper, used malaria rapid diagnostic test strips and whole blood collected from eight sites in seven administrative regions of Tanzania. PCR–RFLP and SSOP-ELISA techniques were used to genotype the A540E and A581G Pfdhps. Data were analysed using SPSS version 18 while Chi square and/or Fischer Exact tests were used to compare prevalence between regions.
Results
A high inter-regional variation of Pfdhps-540E was observed (χ2 = 76.8, p < 0.001). High inter-regional variation of 581G was observed (FE = 85.3, p < 0.001). Both Tanga and Kagera were found to have the highest levels of SP resistance. A high prevalence of Pfdhps-581G was observed in Tanga (56.6 %) in northeastern Tanzania and in Kagera (20.4 %) in northwestern Tanzania and the 540–581 EG haplotype was found at 54.5 and 19.4 %, respectively. Pfdhps-581G was not detected in Pwani and Lindi regions located south of Tanga region.
Conclusions
Selection of SP super-resistant Pfdhps A581G is highest in northern Tanzania. Variation in distribution of SP resistance is observed across the country: northeastern Tanga region and northwestern Kagera region have highest prevalence of SP super-resistance markers, while in Pwani and Lindi in the southeast the prevalence of super-resistance was zero. More studies should be conducted to understand the factors underlying the remarkable heterogeneity in SP resistance in the country.
Keywords: Plasmodium falciparum, Sulfadoxine-pyrimethamine, SP-resistance, SP-super resistance, Anti-malarial drugs, Tanzania, Drug resistance, Malaria, Mutations, Parasites, Polymorphisms
Background
Emergence and spread of Plasmodium falciparum resistance to chloroquine (CQ) and sulfadoxine-pyrimethamine (SP) forced the adoption of artemisinin-based combination therapy (ACT) as first-line anti-malarial drugs in most sub-Saharan African countries (SSA) by 2007 [1]. Since the introduction of ACT, SP has remained the combinational drug for ACT (SP-artesunate) used in a few SSA countries, or as a prophylactic drug in intermittent preventive treatment of malaria during pregnancy (IPTp) where three or more treatment doses of SP are administered on a monthly basis after the first trimester. SP as a prophylaxis is also used in infancy (IPTi) and as a seasonal malaria chemoprevention (SMC) in children [2–4]. SMC in particular, where SP is combined with amodiaquine, is currently being implemented in West African countries (Chad, The Gambia, Niger, Mali, Senegal, Guinea) [5], and it has been shown to be cost effective in reducing childhood morbidity and mortality due to malaria [6].
SP acts by inhibiting the folic acid synthesis in the malaria parasite; sulfadoxine and pyrimethamine inhibit the Plasmodium falciparum enzymes dihydropteroate synthetase (DHPS) and dihydrofolate reductase (DHFR), respectively [7, 8]. Resistance to sulfadoxine and pyrimethamine is caused by mutations in the P. falciparumdhps and dhfr genes, respectively. Pfdhfr single-point mutations causing amino acid changes in N51I, C59R and S108 N are the most common mutations associated with pyrimethamine resistance in SSA [9, 10] and the combination of these forming the triple Pfdhfr IRN mutation is highly prevalent in SSA [11, 12]. Regarding sulfadoxine resistance, Pfdhps mutations S436A/C/F, A437G, K540E, A581G, and A613S/T have been observed globally [13, 14] and S436A/C/F, A437G and G540E are commonly observed in SSA [11]. The combination of the Pfdhfr triple and the Pfdhps double (A437G, K540E) mutations collectively form the quintuple mutations [7, 15] which confers high-level SP resistance and is a significant predictor of SP P. falciparum treatment failure [16–18]. The evolution of the Pfdhps mutations normally occurs after the Pfdhfr triple mutations and thus the presence of Pfdhps double mutations indicates presence of quintuple mutations.
In SSA, the highest prevalence of SP resistance markers has been documented in East Africa where the quintuple mutation has been shown to approach fixation [12]. Evidence shows that the quintuple mutation emerged in the 1990s and in Tanzania as high as over 60 % was detected in 1998 [19], while a recent survey documented more than 95 % quintuple mutation, in 2011 [20]. In 2010, the World Health Organization (WHO), through its malaria advisory committee made a recommendation that SP-IPTi should be implemented only in areas where prevalence of the quintuple mutation, as represented by the Pfdhps 540E, is less than 50 % [21]. Given the high prevalence of the 540E in East Africa, this policy has led to the restricted recommendation of SP-IPTi to West Africa where the 540E mutation (and hence the quintuple mutation) is low or absent [11]; currently, SP-IPTi is only implemented in Chad [5].
In areas where the quintuple mutation is high, IPTp with SP does not prevent placental malaria but may continue to protect against severe pregnancy outcomes [22–25]. WHO has continued to recommend use of at least three SP-IPTp doses even in such areas where the quintuple mutations are high [26].
The emergence of an additional Pfdhps mutation that is 581G in areas where the quintuple mutant is well established has been documented in two major foci in East Africa [12]. Furthermore, in Tanzania in particular, the prevalence of the 581G has reached 55 % in the northeast [27]. Growing evidence from studies performed mainly in Tanzania indicates that presence of the Pfdhps 581G (sextuple mutant parasites), is associated with reduced SP-IPTp efficacy by: (1) a reduction in the protection period of SP-IPTp from 4 to 2 weeks [23]; (2) increased parasitaemia [23, 28] and recently, from a study in Malawi [29], also increased placental parasitaemia [28]; (3) increased risk of severe malaria in offspring [30]; and, (4) low birth weight in new-borns from mothers undergoing SP-IPTp in Tanzania [31]. Thus, the emergence of sextuple mutants seems to have a direct impact on the efficacy of the IPTp using SP. The existing information on the 581G distribution in Tanzania is scarce, mainly confined to the region of Tanga, and may not be evenly distributed across the country. A recent systematic review and meta-analysis of the influence of the Pfdhps 581G mutation on SP-IPTp has shown that when the prevalence of 581G is >10 %, IPTp with SP does not protect against low birth weight [32]. For a proper, evidence-based implementation of IPTp programme and an understanding of regions where the strategy may be compromised, a countrywide monitoring of the mutations is important. This study reports on the status of Pfdhps K540E and A581G in Tanzania.
Methods
Filter paper blood spot, whole blood and used malaria rapid diagnostic test strips collected in previous studies between June 2010 and August 2011 in seven regions of mainland Tanzania were used for this study, as previously described [33]. The study sites included Mwanza (Misungwi district) and Kagera (Muleba district) around Lake Victoria in the northwestern zone, Tanga (Muheza and Bondo) in the northeastern zone, Mtwara (Tandahimba and Mtwara-Urban), Coastal Region (Kibiti-Rufiji) and Lindi Region (Nachingwea) in the southeastern zone and Mbeya (Kyela and Rungwe districts) in the southwestern zone. The DNA samples were extracted using Chelex-100 method [34]. Genotyping for Pfdhps K540E and A581G was performed using polymerase chain reaction-restriction fragment length polymorphisms (PCR-RFLP) and polymerase chain reaction-single strand oligonucleotide probes-enzyme linked immunosorbent assay (PCR-SSOP-ELISA) methods described by others [35–37]. All PCR reagents and restriction endonucleases were purchased from New England Biolabs (Ipswich, MA, USA). Primers were purchased from Biolegio (Nijmegen, The Netherlands). Prevalence was calculated for each genotype, excluding mixed infections in both individual genotype prevalence and in 540-581 haplotype analysis. Only a few mixed infections were observed in A581G (Table 1). Maps were constructed using ArcGIS version 10.2. The study received ethical approval from the Kilimanjaro Christian Medical University College Research Ethics Review Committee.
Table 1.
Distribution of Pfdhps K540E and A581G polymorphisms among regions in Tanzania
| 540 | 581 | Haplotypes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Region | Site | K | E | K/E | Total (n) | A | G | A/G | Total (n) | KA | KG | EA | EG | Total (n) |
| Mwanza | Misungwi | 4 (3.0) | 129 (97.0) | 0 | 133 | 118 (95.2) | 6 (4.8) | 0 | 124 | 4 (3.2) | 0 (0.0) | 114 (91.9) | 6 (4.8) | 124 |
| Mbeya | Multiple sites | 3 (2.0) | 150 (98.0) | 0 | 153 | 143 (93.5) | 9 (5.9) | 1 (0.7) | 153 | 3 (2.0) | 0 (0.0) | 140 (92.1) | 9 (5.9) | 152 |
| Mtwara | Tandahimba and Mtwara urban | 30 (36.1) | 53 (63.9) | 0 | 83 | 76 (95.2) | 4 (4.8) | 0 | 80 | 29 (34.9) | 1 (1.2) | 50 (60.2) | 3 (3.6) | 83 |
| Lindi | Nachingwea | 24 (27.3) | 64 (72.7) | 0 | 88 | 88 (100) | 0 | 0 | 88 | 24 (27.3) | 0 (0.0) | 64 (72.7) | 0 (0.0) | 88 |
| Tanga | Bondo | 10 (8.6) | 106 (91.4) | 0 | 116 | 46 (40.6) | 64 (56.6) | 3 (2.7) | 113 | 7 (6.4) | 4 (3.6) | 39 (35.5) | 60 (54.5) | 110 |
| Muheza | 5 (5.7) | 83 (94.3) | 0 | 88 | 43 (48.9) | 45 (51.1) | 0 | 88 | 5 (5.7) | 0 (0.0) | 38 (43.2) | 45 (51.1) | 88 | |
| Pwani | Rufiji | 23 (23.7) | 74 (76.3) | 0 | 97 | 100 (100) | 0 | 0 | 100 | 23 (23.7) | 0 (0.0) | 74 (76.3) | 0 (0.0) | 97 |
| Kagera | Muleba | 8 (4.7) | 162 (95.3) | 0 | 170 | 86 (79.6) | 22 (20.4) | 0 | 108 | 4 (3.7) | 1 (0.9) | 82 (75.9) | 21 (19.4) | 108 |
| Total | 107 | 821 | 0 (0) | 928 | 700 | 150 | 4 | 854 | 99 (13.2) | 6 (0.6) | 601 (70.1) | 144 (16.0) | 850 | |
Data are given as sample size and prevalence (%) in brackets
Results
Pfdhps K540E and A581G distribution
A total of 1024 samples were available for the study from eight sites in seven regions; 928 and 854 were successfully genotyped for Pfdhps K540E and A581G, respectively. Genotypes are summarized in Table 1. The prevalence of the 540E mutation was generally high in all regions with the highest observed in Mbeya (98.0 %) and the lowest in Mtwara (63.9 %). Mtwara, Lindi and Pwani regions had significantly lower prevalence of 540E (average 71.3 %) compared to the rest of the country (average 92.4 %) (χ2 = 76.8, p < 0.001). For the 581G mutation, Muheza and Bondo sites in Tanga region had the highest prevalence at 51.1 and 56.6 %, respectively, followed by Kagera region (Muleba) where 20.4 % was recorded. Contrarily, the 581G mutation was absent in Pwani and Lindi regions and, again by comparing the southeast Mtwara, Lindi and Pwani regions against the rest of the country, only 1.5 % of the 581G was recorded in these three regions compared to 22.6 % in the rest (FE = 85.3, p < 0.001) (Table 1; Fig. 1).
Fig. 1.
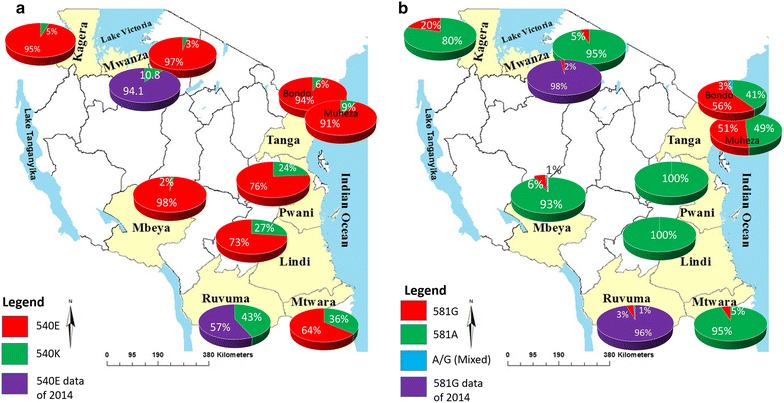
Regional sites and distribution of Pfdhps polymorphisms in Tanzania. a Pfdhps K540E and b Pfdhps A581G. Mutants are shown in red and wild types in green. Mixed genotypes are shown in light blue. All samples were collected in 2010/2011 except data shown in purple. Shown in purple is preliminary data for samples collected in 2014 for Mwanza and Ruvuma regions where similarity in Pfdhps 540E and 581G prevalence between Ruvuma and neighbouring Mtwara region is observed
Pfdhps haplotypes
Construction of Pfdhps K540E-A581G haplotypes was performed and is shown in Table 1. The most prevalent haplotype was the EA ranging from 35.5 to 92.1 %. This is due to the high prevalence of the 540E as opposed to the 581G. The double mutant EG haplotype was most prevalent in Tanga, both in Muheza (51.1 %) and Bondo (54.5 %); it was observed at 3.6 % in Mtwara and 19.4 % in Kagera, while being absent in Pwani and Lindi.
Discussion
Historically, pyrimethamine has been in use in Tanga region since the 1950s [38]. In 1954 resistance to a weekly prophylactic dose of pyrimethamine was reported in Tanga and this was the first resistance report in Tanzania and in Africa [39]. SP continued both as the second-line treatment drug [chloroquine (CQ) was the first-line drug] and for malaria prophylaxis until 2001, when it was declared the first-line drug due to high levels of CQ resistance [40]. However, since resistance to SP had already emerged, at least in some parts of the country, SP policy in 2001 was considered a temporary solution [41] and was replaced by ACT by 2006 [42].
In the East African region, the prevalence of molecular markers of SP resistance has been increasing since the emergence of the first resistance-conferring mutations in the 1950s. During the past decade, many of these mutations in Pfdhfr and Pfdhps have approached fixation levels, while newer mutations are still increasing [20, 27, 43, 44]. Given the importance of preventing malaria in pregnancy, the growing evidence of declining effectiveness of the IPTp strategy in areas of high prevalence of quintuple and sextuple Pfdhfr/Pfdhps haplotypes and the lack of an alternative to SP for use in IPTp, then the monitoring of SP resistance is crucial [45]. This is the first multi-site study in Tanzania to report on countrywide prevalence of these markers of SP resistance of immediate importance. The Pfdhps A581G mutation was first reported at low prevalence of 1.6 and 1.2 % in Mlimba (Morogoro) and Matema (Mbeya), respectively, in 2005 [46]. Surveys done in Tanga (Hale) in 2006 and 2007 found the mutation at prevalence of up to 54 % [27, 47]. In this study, Tanga region represents the highest prevalence of Pfdhps 581G followed by Kagera region. Highest levels of molecular markers of resistance (or tolerance) to other anti-malarial drugs, such as CQ, have also been recorded in Tanga when compared to other regions in Tanzania regarding mutations in Pfcrt (reviewed in [33]) and artemether-lumefantrine regarding the Pfmdr1 marker [48]. Furthermore, occurrence of the South Asian CQ-resistant Pfcrt haplotype SVMNT was also reported in Tanga for the first time [49].
Local drug pressure is mainly related to local malaria endemicity, which meaning that resistance levels may vary between different regions in Tanzania, due to their differences in malaria endemicity. The whole of Tanzania is endemic to malaria, but the Indian Ocean coastal strip (Tanga, Coastal, Dar es Salaam, Lindi, Mtwara) and the Lake Victoria shores (Mwanza, Kagera) have generally higher malaria endemicity compared to the rest of the country. The high malaria endemicity in, especially, Tanga and Kagera may therefore partly explain the observed high resistance to SP in these regions due to increased drug pressure relative to other regions. However, the differences in levels of resistance markers between these regions compared to the Coastal region, which also represents high malaria endemicity, leads to speculation that other local factors are contributing to local expansion of the 581G mutant parasites. Such factors may be related to local movement of the population and the in- and out-flow of people carrying parasites from one area to another. For instance, according to a study by Pindolia et al. [50], the Dodoma region is a major source of both human movement and malaria movement. Pindolia and colleagues have shown that while the majority of both human and malaria movement is directed towards the central and the western parts of the country, which do not represent major sources of super resistance (mainly Mbeya and Mwanza), the majority of the malaria movement was directed towards Mwanza (where there is some degree of resistance). This implies that the malaria movement does not correlate positively with resistance. Tanga, however, which represents the highest level of SP resistance was found to represent only internal movement and no major in- or out-flow or neither people nor malaria, indicating that perhaps this setting is more isolated and prone to resistance emergence and accumulation, perhaps due to a lack of in-flow of new and diverse parasite genotypes.
Furthermore, the southern parts of the Tanzania have a lower level of SP resistance, whereas the trends shown in the present study point to the northeastern and northwestern parts bordering Kenya and Uganda, respectively, having relatively higher levels of SP resistance. It is possible that cross-border spread of resistance contributes to these observations. For instance, in western Kenya, Pfdhps 540E and 581G have been reported to have increased, respectively, from 33.1 and 0 % in 1996 to 99.2 and 5.3 % in 2009 [43]. Related trends have also been reported in the same area in Kenya [51] although the reported prevalence of 581G is much lower than in Tanga and Kagera regions. In Uganda, a study performed in central Uganda reported Pfdhps 581G at 3.3 %, while another in western Uganda reported 36 % [28, 52].
Considering the combined Pfdhps K540E-A581G haplotypes, the EG haplotype (540E–581G) was observed at highest prevalence (>50 %) in Tanga region (both in Muheza and Bondo sites) and in Kagera (>20 % in Muleba). This haplotype is common in South America and Cambodia [53] thus it unclear whether this has independently evolved in Tanzania or other factors such as importation account for this. The EA highest in Mbeya and Mwanza regions (>90 %) was considered an East African haplotype, while the rarely observed wild-type KA is common in West Africa. A rare KG haplotype in was observed in Tanga. The KG is thought to evolve from the EG haplotype and is common in Cambodia and Venezuela [53]. The overall distribution of Pfdhps mutation and especially the EG haplotype indicates that P. falciparum sensitivity to SP vary largely across the country, with implication for SP-IPTp implementation. Despite the large sample set from across Tanzania used in this study, it is not clear if a greater variability can be found if further sampling is performed. Furthermore, intra-regional variability in resistance has been observed, for instance, for the case of Bondo and Muheza within Tanga region. Further preliminary mapping of the Pfdhps K540E-A581G haplotypes using 2014 samples from Songea in Ruvuma region, which is placed somewhat between Mtwara and Mbeya, observed a prevalence of the EG haplotype of 2 % (Fig. 1), which does not differ much from the 5 % in neighbouring Mtwara region. A similar observation was made for Mwanza.
Sporadic evidence shows that although ACT is the current first-line anti-malarial for treatment of uncomplicated malaria, the lack of proper healthcare services, especially in rural communities in Tanzania, as well as the availability of other anti-malarials in drug shops, encourages self-medication with non-standard regimens, including SP [54, 55]. It is important for national malaria control programmes and Ministries of Health to limit the availability of drugs such as SP to IPTp and/or IPTi programmes only. Furthermore, consideration for differentiated regional implementation of SP-IPTp based on differences in resistance levels may be important prior to availability of alternatives to SP. Sustained monitoring of molecular markers of SP resistance, especially super-resistance markers, should be continued with countrywide coverage in order to enable time-point specific assessment.
Conclusions
Selection of SP resistance in Tanzania is high with variable distribution of Pfdhps A581G SP super-resistance marker across the country. The northeastern Tanga region and the northwest Mwanza and Kagera regions have high prevalence of SP super resistance that may spread to other regions of the country. This variable distribution of SP super resistance may have implications for the current IPTp policy and its outcome in Tanzania. Until alternative drugs for IPTp are available, routine monitoring of clinical outcome of IPTp and continuous monitoring of SP super-resistance markers is necessary.
Authors’ contributions
RAK conceived the idea, designed the study, analysed the data, and wrote the manuscript. RDK performed laboratory work and participated in data analysis and writing the manuscript. SN participated in data interpretation and writing the manuscript. CK and JGN participated in sample collection, laboratory work and reviewed the manuscript. AAK participated in sample collection, data interpretation and reviewed the manuscript. DI participated in data analysis and revised the manuscript. CR and MA participated in overall study design, data analysis and interpretation, and in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge Dr. Aliphaxard Manjurano, Dr. Jackline Mosha and Mr. Akili Kalinga from NIMR Mwnza and Tukuyu, respectively, for providing part of the study samples. This work was supported by the Training Health Researchers into Vocational Excellence in East Africa (THRiVE) consortium funded by the Wellcome Trust Grant Number 087540.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this paper are included within the paper. Raw data may be obtained from the corresponding author on request.
Consent for publication
This study reports no individual data. Data reported in this study are solely based on Plasmodium falciparum genetics and bears no individual participant information.
Ethics approval and consent to participate
The study was reviewed and approved by the Kilimanjaro Christian Medical University College Research Ethics Review Committee (CRERC no. 446). Samples used in this study were collected in previous studies in which informed consent was obtained from participants (or parents/guardians of children under 18 years) to voluntarily participate.
Abbreviations
- ACT
artemisinin-based combinational therapy
- CQ
chloroquine
- SMC
seasonal malaria chemoprevention
- ELISA
enzyme-linked immunosorbent assay
- IPTi
intermittent preventive treatment of malaria in infancy
- IPTp
intermittent preventive treatment of malaria in pregnancy
- NIMR
National Institute of Medical Research
- PCR–RFLP
polymerase chain reaction-restriction fragment length polymorphisms
- Pdhfr
Plasmodium falciparum dihydrofolate reductase
- Pfdhps
Plasmodium falciparum dihydropteroate synthetase
- SP
sulfadoxine–pyrimethamine
- SPSS
statistical package for social sciences
- SSOP
single-strand oligonucleotide probes
- THRiVE
Training Health Researchers into Vocational Excellence in East Africa
- WHO
World Health Organization
Contributor Information
Reginald A. Kavishe, Email: rekavishe@yahoo.com
Robert D. Kaaya, Email: robertkaaya@yahoo.com
Sidsel Nag, Email: sidselnag@sund.ku.dk.
Camilla Krogsgaard, Email: cakro@dtu.dk.
Jakob Ginsbak Notland, Email: j_akob@hotmail.com.
Adellaida A. Kavishe, Email: adellakavishe@yahoo.com
Deus Ishengoma, Email: deusishe@yahoo.com.
Cally Roper, Email: Cally.Roper@lshtm.ac.uk.
Michael Alifrangis, Email: micali@sund.ku.dk.
References
- 1.WHO . World Malaria Report, 2008. Geneva: World Health Organization; 2008. [Google Scholar]
- 2.Cairns M, Roca-Feltrer A, Garske T, Wilson AL, Diallo D, Milligan PJ, et al. Estimating the potential public health impact of seasonal malaria chemoprevention in African children. Nat Commun. 2012;3:881. doi: 10.1038/ncomms1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crawley J, Sismanidis C, Goodman T, Milligan P. Effect of intermittent preventive treatment for malaria during infancy on serological responses to measles and other vaccines used in the expanded programme on immunization: results from five randomised controlled trials. Lancet. 2012;380:1001–1010. doi: 10.1016/S0140-6736(12)60775-2. [DOI] [PubMed] [Google Scholar]
- 4.Tine RC, Ndiaye P, Ndour CT, Faye B, Ndiaye JL, Sylla K, et al. Acceptability by community health workers in Senegal of combining community case management of malaria and seasonal malaria chemoprevention. Malar J. 2013;12:467. doi: 10.1186/1475-2875-12-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . World Malaria Report. Geneva: World Health Organization; 2015. [Google Scholar]
- 6.Conteh L, Patouillard E, Kweku M, Legood R, Greenwood B, Chandramohan D. Cost effectiveness of seasonal intermittent preventive treatment using amodiaquine & artesunate or sulphadoxine-pyrimethamine in Ghanaian children. PLoS ONE. 2010;5:e12223. doi: 10.1371/journal.pone.0012223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Triglia T, Wang P, Sims PF, Hyde JE, Cowman AF. Allelic exchange at the endogenous genomic locus in Plasmodium falciparum proves the role of dihydropteroate synthase in sulfadoxine-resistant malaria. EMBO J. 1998;17:3807–3815. doi: 10.1093/emboj/17.14.3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zolg JW, Plitt JR, Chen GX, Palmer S. Point mutations in the dihydrofolate reductase-thymidylate synthase gene as the molecular basis for pyrimethamine resistance in Plasmodium falciparum. Mol Biochem Parasitol. 1989;36:253–262. doi: 10.1016/0166-6851(89)90173-4. [DOI] [PubMed] [Google Scholar]
- 9.Cowman AF, Morry MJ, Biggs BA, Cross GA, Foote SJ. Amino acid changes linked to pyrimethamine resistance in the dihydrofolate reductase-thymidylate synthase gene of Plasmodium falciparum. Proc Natl Acad Sci USA. 1988;85:9109–9113. doi: 10.1073/pnas.85.23.9109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterson DS, Walliker D, Wellems TE. Evidence that a point mutation in dihydrofolate reductase-thymidylate synthase confers resistance to pyrimethamine in falciparum malaria. Proc Natl Acad Sci USA. 1988;85:9114–9118. doi: 10.1073/pnas.85.23.9114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naidoo I, Roper C. Drug resistance maps to guide intermittent preventive treatment of malaria in African infants. Parasitology. 2011;138:1469–1479. doi: 10.1017/S0031182011000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naidoo I, Roper C. Mapping ‘partially resistant’, ‘fully resistant’, and ‘super resistant’ malaria. Trends Parasitol. 2013;29:505–515. doi: 10.1016/j.pt.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Brooks DR, Wang P, Read M, Watkins WM, Sims PF, Hyde JE. Sequence variation of the hydroxymethyldihydropterin pyrophosphokinase: dihydropteroate synthase gene in lines of the human malaria parasite, Plasmodium falciparum, with differing resistance to sulfadoxine. Eur J Biochem. 1994;224:397–405. doi: 10.1111/j.1432-1033.1994.00397.x. [DOI] [PubMed] [Google Scholar]
- 14.Triglia T, Cowman AF. Primary structure and expression of the dihydropteroate synthetase gene of Plasmodium falciparum. Proc Natl Acad Sci USA. 1994;91:7149–7153. doi: 10.1073/pnas.91.15.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang P, Read M, Sims PF, Hyde JE. Sulfadoxine resistance in the human malaria parasite Plasmodium falciparum is determined by mutations in dihydropteroate synthetase and an additional factor associated with folate utilization. Mol Microbiol. 1997;23:979–986. doi: 10.1046/j.1365-2958.1997.2821646.x. [DOI] [PubMed] [Google Scholar]
- 16.Kublin JG, Dzinjalamala FK, Kamwendo DD, Malkin EM, Cortese JF, Martino LM, Mukadam RA, Rogerson SJ, Lescano AG, Molyneux ME, Winstanley PA, Chimpeni P, et al. Molecular markers for failure of sulfadoxine-pyrimethamine and chlorproguanil-dapsone treatment of Plasmodium falciparum malaria. J Infect Dis. 2002;185:380–388. doi: 10.1086/338566. [DOI] [PubMed] [Google Scholar]
- 17.Omar SA, Adagu IS, Warhurst DC. Can pretreatment screening for dhps and dhfr point mutations in Plasmodium falciparum infections be used to predict sulfadoxine-pyrimethamine treatment failure? Trans R Soc Trop Med Hyg. 2001;95:315–319. doi: 10.1016/S0035-9203(01)90250-0. [DOI] [PubMed] [Google Scholar]
- 18.Staedke SG, Sendagire H, Lamola S, Kamya MR, Dorsey G, Rosenthal PJ. Relationship between age, molecular markers, and response to sulphadoxine-pyrimethamine treatment in Kampala, Uganda. Trop Med Int Health. 2004;9:624–629. doi: 10.1111/j.1365-3156.2004.01239.x. [DOI] [PubMed] [Google Scholar]
- 19.Alifrangis M, Lemnge MM, Ronn AM, Segeja MD, Magesa SM, Khalil IF, et al. Increasing prevalence of wildtypes in the dihydrofolate reductase gene of Plasmodium falciparum in an area with high levels of sulfadoxine/pyrimethamine resistance after introduction of treated bed nets. Am J Trop Med Hyg. 2003;69:238–243. [PubMed] [Google Scholar]
- 20.Matondo SI, Temba GS, Kavishe AA, Kauki JS, Kalinga A, van Zwetselaar M, et al. High levels of sulphadoxine-pyrimethamine resistance Pfdhfr-Pfdhps quintuple mutations: a cross sectional survey of six regions in Tanzania. Malar J. 2014;13:152. doi: 10.1186/1475-2875-13-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO . Policy recommendation on Intermittent Preventive Treatment during infancy with sulphadoxine-pyrimethamine (SP-IPTi) for Plasmodium falciparum malaria control in Africa. Geneva: World Health Organization; 2010. [Google Scholar]
- 22.Arinaitwe E, Ades V, Walakira A, Ninsiima B, Mugagga O, Patil TS, et al. Intermittent preventive therapy with sulfadoxine-pyrimethamine for malaria in pregnancy: a cross-sectional study from Tororo, Uganda. PLoS ONE. 2013;8:e73073. doi: 10.1371/journal.pone.0073073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrington WE, Mutabingwa TK, Muehlenbachs A, Sorensen B, Bolla MC, Fried M, et al. Competitive facilitation of drug-resistant Plasmodium falciparum malaria parasites in pregnant women who receive preventive treatment. Proc Natl Acad Sci USA. 2009;106:9027–9032. doi: 10.1073/pnas.0901415106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harrington WE, Mutabingwa TK, Kabyemela E, Fried M, Duffy PE. Intermittent treatment to prevent pregnancy malaria does not confer benefit in an area of widespread drug resistance. Clin Infect Dis. 2011;53:224–230. doi: 10.1093/cid/cir376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin JT, Mbewe B, Taylor SM, Luntamo M, Meshnick SR, Ashorn P. Increased prevalence of dhfr and dhps mutants at delivery in Malawian pregnant women receiving intermittent preventive treatment for malaria. Trop Med Int Health. 2013;18:175–178. doi: 10.1111/tmi.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO-MPAC Malaria Policy Advisory Committee to the WHO: conclusions and recommendations of, March 2013 meeting. Malar J. 2013;2013(12):213. doi: 10.1186/1475-2875-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alifrangis M, Lusingu JP, Mmbando B, Dalgaard MB, Vestergaard LS, Ishengoma D, et al. Five-year surveillance of molecular markers of Plasmodium falciparum antimalarial drug resistance in Korogwe District, Tanzania: accumulation of the 581G mutation in the P. falciparum dihydropteroate synthase gene. Am J Trop Med Hyg. 2009;80:523–527. [PubMed] [Google Scholar]
- 28.Braun V, Rempis E, Schnack A, Decker S, Rubaihayo J, Tumwesigye NM, et al. Lack of effect of intermittent preventive treatment for malaria in pregnancy and intense drug resistance in western Uganda. Malar J. 2015;14:372. doi: 10.1186/s12936-015-0909-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gutman J, Kalilani L, Taylor S, Zhou Z, Wiegand RE, Thwai KL, et al. The A581G Mutation in the gene encoding Plasmodium falciparum dihydropteroate synthetase reduces the effectiveness of sulfadoxine-pyrimethamine preventive therapy in malawian pregnant women. J Infect Dis. 2015;211:1997–2005. doi: 10.1093/infdis/jiu836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrington WE, Morrison R, Fried M, Duffy PE. Intermittent preventive treatment in pregnant women is associated with increased risk of severe malaria in their offspring. PLoS ONE. 2013;8:e56183. doi: 10.1371/journal.pone.0056183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Minja DT, Schmiegelow C, Mmbando B, Bostrom S, Oesterholt M, Magistrado P, et al. Plasmodium falciparum mutant haplotype infection during pregnancy associated with reduced birthweight, Tanzania. Emerg Infect Dis. 2013;19:9. doi: 10.3201/eid1909.130133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chico RM, Cano J, Ariti C, Collier TJ, Chandramohan D, Roper C, et al. Influence of malaria transmission intensity and the 581G mutation on the efficacy of intermittent preventive treatment in pregnancy: systematic review and meta-analysis. Trop Med Int Health. 2015;20:1621–1633. doi: 10.1111/tmi.12595. [DOI] [PubMed] [Google Scholar]
- 33.Mohammed A, Ndaro A, Kalinga A, Manjurano A, Mosha JF, Mosha DF, et al. Trends in chloroquine resistance marker, Pfcrt-K76T mutation ten years after chloroquine withdrawal in Tanzania. Malar J. 2013;12:415. doi: 10.1186/1475-2875-12-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Polski JM, Kimzey S, Percival RW, Grosso LE. Rapid and effective processing of blood specimens for diagnostic PCR using filter paper and Chelex-100. Mol Pathol. 1998;51:215–217. doi: 10.1136/mp.51.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alifrangis M, Enosse S, Pearce R, Drakeley C, Roper C, Khalil IF, et al. A simple, high-throughput method to detect Plasmodium falciparum single nucleotide polymorphisms in the dihydrofolate reductase, dihydropteroate synthase, and P. falciparum chloroquine resistance transporter genes using polymerase chain reaction- and enzyme-linked immunosorbent assay-based technology. Am J Trop Med Hyg. 2005;72:155–162. [PubMed] [Google Scholar]
- 36.Jelinek T, Ronn AM, Curtis J, Duraisingh MT, Lemnge MM, Mhina J, et al. High prevalence of mutations in the dihydrofolate reductase gene of Plasmodium falciparum in isolates from Tanzania without evidence of an association to clinical sulfadoxine/pyrimethamine resistance. Trop Med Int Health. 1997;2:1075–1079. doi: 10.1046/j.1365-3156.1997.d01-189.x. [DOI] [PubMed] [Google Scholar]
- 37.University of Mayland School of Medicine. PCR-allele-specific restriction analysis (ASRA): Protocols for Plasmodium falciparum drug resistance mutation analyses. University of Mayland 2002. Accessed 5 Oct 2013.
- 38.Ronn AM, Msangeni HA, Mhina J, Wernsdorfer WH, Bygbjerg IC. High level of resistance of Plasmodium falciparum to sulfadoxine-pyrimethamine in children in Tanzania. Trans R Soc Trop Med Hyg. 1996;90:179–181. doi: 10.1016/S0035-9203(96)90129-7. [DOI] [PubMed] [Google Scholar]
- 39.Clyde DF, Shute GT. Resistance of Plasmodium falciparum in Tanganyika to pyrimethamine administered at weekly intervals. Trans R Soc Trop Med Hyg. 1957;51:505–513. doi: 10.1016/0035-9203(57)90039-1. [DOI] [PubMed] [Google Scholar]
- 40.Taverne J. Tanzania phases out chloroquine for the treatment of malaria. Trends Parasitol. 2001;17:360. doi: 10.1016/S1471-4922(01)02067-0. [DOI] [PubMed] [Google Scholar]
- 41.Mugittu K, Ndejembi M, Malisa A, Lemnge M, Premji Z, Mwita A, et al. Therapeutic efficacy of sulfadoxine-pyrimethamine and prevalence of resistance markers in Tanzania prior to revision of malaria treatment policy: Plasmodium falciparum dihydrofolate reductase and dihydropteroate synthase mutations in monitoring in vivo resistance. Am J Trop Med Hyg. 2004;71:696–702. [PubMed] [Google Scholar]
- 42.Njau JD, Goodman CA, Kachur SP, Mulligan J, Munkondya JS, McHomvu N, et al. The costs of introducing artemisinin-based combination therapy: evidence from district-wide implementation in rural Tanzania. Malar J. 2008;7:4. doi: 10.1186/1475-2875-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iriemenam NC, Shah M, Gatei W, van Eijk AM, Ayisi J, Kariuki S, et al. Temporal trends of sulphadoxine-pyrimethamine (SP) drug-resistance molecular markers in Plasmodium falciparum parasites from pregnant women in western Kenya. Malar J. 2012;11:134. doi: 10.1186/1475-2875-11-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raman J, Little F, Roper C, Kleinschmidt I, Cassam Y, Maharaj R, et al. Five years of large-scale dhfr and dhps mutation surveillance following the phased implementation of artesunate plus sulfadoxine-pyrimethamine in Maputo Province, Southern Mozambique. Am J Trop Med Hyg. 2010;82:788–794. doi: 10.4269/ajtmh.2010.09-0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vinetz JM. Intermittent preventive treatment for malaria in sub-Saharan Africa: a halfway technology or a critical intervention? Am J Trop Med Hyg. 2010;82:755–756. doi: 10.4269/ajtmh.2010.825editorial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schönfeld M, Barreto MI, Schunk M, Maduhu I, Maboko L, Hoelscher M, et al. Molecular surveillance of drug-resistance associated mutations of Plasmodium falciparum in south-west Tanzania. Malar J. 2007;6:2. doi: 10.1186/1475-2875-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gesase S, Gosling RD, Hashim R, Ord R, Naidoo I, Madebe R, et al. High resistance of Plasmodium falciparum to sulphadoxine/pyrimethamine in northern Tanzania and the emergence of dhps resistance mutation at Codon 581. PLoS ONE. 2009;4:e4569. doi: 10.1371/journal.pone.0004569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kavishe RA, Paulo P, Kaaya RD, Kalinga A, van Zwetselaar M, Chilongola J, et al. Surveillance of artemether-lumefantrine associated Plasmodium falciparum multidrug resistance protein-1 gene polymorphisms in Tanzania. Malar J. 2014;13:264. doi: 10.1186/1475-2875-13-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alifrangis M, Dalgaard MB, Lusingu JP, Vestergaard LS, Staalsoe T, Jensen AT, et al. Occurrence of the Southeast Asian/South American SVMNT haplotype of the chloroquine-resistance transporter gene in Plasmodium falciparum in Tanzania. J Infect Dis. 2006;193:1738–1741. doi: 10.1086/504269. [DOI] [PubMed] [Google Scholar]
- 50.Pindolia DK, Garcia AJ, Huang Z, Smith DL, Alegana VA, Noor AM, et al. The demographics of human and malaria movement and migration patterns in East Africa. Malar J. 2013;12:397. doi: 10.1186/1475-2875-12-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Juma DW, Omondi AA, Ingasia L, Opot B, Cheruiyot A, Yeda R, et al. Trends in drug resistance codons in Plasmodium falciparum dihydrofolate reductase and dihydropteroate synthase genes in Kenyan parasites from 2008 to 2012. Malar J. 2014;13:250. doi: 10.1186/1475-2875-13-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mbonye AK, Birungi J, Yanow SK, Shokoples S, Malamba S, Alifrangis M, et al. Prevalence of Plasmodium falciparum resistance markers to sulfadoxine-pyrimethamine among pregnant women receiving intermittent preventive treatment for malaria in Uganda. Antimicrob Agents Chemother. 2015;59:5475–5482. doi: 10.1128/AAC.00507-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vinayak S, Alam MT, Mixson-Hayden T, McCollum AM, Sem R, Shah NK, et al. Origin and evolution of sulfadoxine resistant Plasmodium falciparum. PLoS Pathog. 2010;6:e1000830. doi: 10.1371/journal.ppat.1000830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chipwaza B, Mugasa JP, Mayumana I, Amuri M, Makungu C, Gwakisa PS. Self-medication with anti-malarials is a common practice in rural communities of Kilosa district in Tanzania despite the reported decline of malaria. Malar J. 2014;13:252. doi: 10.1186/1475-2875-13-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ringsted FM, Massawe IS, Lemnge MM, Bygbjerg IC. Saleability of anti-malarials in private drug shops in Muheza, Tanzania: a baseline study in an era of assumed artemisinin combination therapy (ACT) Malar J. 2011;10:238. doi: 10.1186/1475-2875-10-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this paper are included within the paper. Raw data may be obtained from the corresponding author on request.


