Abstract
Background:
Stroke is an important cause of disability in children. Pediatric stroke may be due to significant permanent cognitive and motor handicap in children. In this study, we evaluated long-term outcomes of stroke in pediatric patients who have been discharged with definite diagnosis of stroke in Tehran Mofid children’s Hospital and Imam Hossein children’s Hospital located in Isfahan, Iran, from 2005 to 2012.
Materials and Methods:
A total of 53 children with stroke were included in the study. Stroke outcomes as motor disability, seizures, and cognitive dysfunctions were assessed.
Results:
After a median follow-up of 4 years, 15 (29%) patients experienced full recovery. Thirty-eight (71%) patients had some degree of neurological handicap.
Conclusion:
Approximately 70% of children with arterial ischemic stroke suffer from long-term neurological disabilities including motor deficits, cognitive impairment, and late seizures. Stroke recurrence is the most important risk factor responsible for severe adverse neurological outcomes in pediatric stroke.
Keywords: Ischemic stroke, neurological, outcome
INTRODUCTION
Ischemic stroke is defined as focal neurological deficit in the territory of specific cerebral arteries. Stroke is rare in children though it is one of the most important causes of significant and long-term disability.[1,2]
Etiology of stroke in pediatric age is quite different from that in adult age.
Various conditions in children may predispose them to stroke. In most children with stroke, more than one risk factor could be found.[3]
The most common presentation of stroke in children is focal neurologic deficit such as hemiplegia, hemiparesis, facial palsy, seizure, and loss of consciousness.[2,3] Stroke can leave the affected patient with significant motor and mental disability.[4,5,6] Studies on pediatric stroke had increased during recent years, but clinical study of pediatric stroke outcome is rare with contradictory results. Full recovery has been observed in 25–30% of pediatric patients with stroke, but unfortunately despite expected neuronal plasticity, 70–80% of patients suffer from long-term disabilities which persist in adulthood.[5,7,8]
Results of a cross-sectional retrospectively recruited study of stroke outcome showed that children with arterial ischemic stroke display significantly poorer cognitive functioning as worse performance on verbal and nonverbal intellectual function on many cognitive measurements in comparison to normal children.[9]
Seizures are common in acute phase of childhood stroke. Childhood stroke may present with seizures. In any child with acute focal deficit and seizure, stroke should be considered as a differential diagnosis. Rate of seizure in the early period after stroke is significantly higher than adults and has been reported to be 25–58% in different studies. Secondary epilepsy after childhood stroke has been reported to be 20–25%. Early seizure was the main predictor of secondary epilepsy.[2,10,11,12]
Recurrence of stroke occurred in 20% of the patients with childhood stroke. Patients with underlying disease particularly arteriopathy, congenital heart disease, and hereditary hypercoagulable state are at increased risk of recurrence, which is the most important risk factor for severe neurological disability.[13,14]
Recently various studies have been performed on subject of pediatric ischemic stroke, while investigation of stroke outcome in children is rare. The aim of our study was to assess long-term neurological outcomes in patients with stroke.
MATERIALS AND METHODS
In this retrospective study, we assessed long-term neurological outcome of patients with stroke who have been admitted in pediatric neurology subspecialty service in Tehran Mofid children’s hospital and Isfahan Imam Hossein children’s hospital from 2005 to 2013.
Inclusion criteria were definitive diagnosis of arterial ischemic stroke and availability of data.
The patients with neurometabolic or neurodegenerative disorder, neuromuscular disorder, past history of the central nervous system damage due to other etiologies were excluded from the study.
Patients
Sixty-nine patients with arterial ischemic stroke were identified. Forty-one cases were from Mofid children’s hospital in Tehran, and the rest were from Imam Hossein children’s hospital in Isfahan. Data of 14 patients were not available or were lost to follow-up. Two patients had died. A total of 53 patients with definite diagnosis of stroke were included in this study. Out of these 53 patients, 34 patients were male and 19 patients were female. All data including age, sex, presenting signs and symptoms, initial neuroimaging, and neurological state on discharge were abstracted.
All data regarding physical examination and evolution of disease in serial outpatient clinical examination were recorded.
The patient’s last neurological condition was evaluated by physical examination and parent's interview.
For evaluation of the long-term outcome following stroke, a clinical investigation (physical examination, patients, and their parents’ interview), assessment of school performance, limitation in daily activities, and health-related quality of life questionnaires were used.
All data collected from physical examination and interviews were analyzed statistical Package for Social Science (SPSS) version 20, using t and Chi-squared tests.
RESULTS
A total of 53 patients with definite diagnosis of stroke whose data were available were included. Age at first stroke was 10 months to 12 years (mean age was 5.2 years).
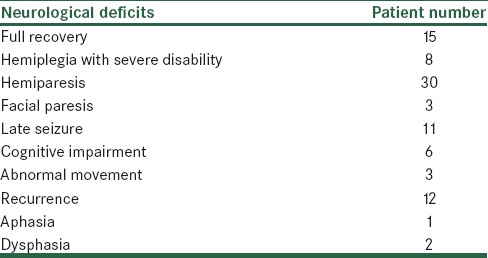
In 53% of the patients, at least one risk factor was recognized for stroke. Arteriopathy other than moyamoya,[6] congenital heart disease,[6] and hereditary hypercoagulable state[5] were the most common risk factors for stroke. In 80% of the patients with stroke recurrence, a definite risk factor was identified. After a median follow-up of 4 years, 15 patients (29%) found full recovery. Thirty-eight patients (71%) had some degrees of neurological handicap. Nineteen patients (35%) got partial recovery and suffered from mild hemiparesis. Most of the patients with full recovery had presented mild motor disability. Eight of 11 patients with mild presenting symptom had full recovery comparing to 7 of 42 patients with more severe initial motor disability. Severity of initial functional disability was significantly related with poor functional outcome (P < 0.05).
Eleven (20%) patients with hemiparesis needed some supports but were able to walk independently. Hemiplegia with severe disability was observed in 8 (15%) patients.
Facial paresis was observed in 3 patients (5%). Eight patients (15%) had significant cognitive impairments. Two of these patients had Down syndrome. Out of the remaining 6 patients with cognitive problems affecting school performance and daily life, 3 patients had recurrence of stroke. Recurrence of stroke occurred in 12 patients (22%). Recurrence of stroke was a major risk factor for cognitive impairment (P < 0.05). Three patients (5%) had dysphasia (2 patients) or aphasia (1 patient). In 3 patients (5%), abnormal movement (chorea-dystonia) was observed. Eleven patients (20%) had secondary epilepsy and were treated with anticonvulsant. The worst functional outcome was observed in patients with recurrent stroke, moyamoya disease, and hereditary hypercoagulable state.
Five of 8 patients with severe neurological deficits had experienced stroke recurrence (P < 0.05).
Nearly all the patients (10 of 11) with secondary epilepsy experienced seizure as a presenting symptom or during hospitalization (P < 0.05).
The results are available in Tables 1 and 2.
Table 1.
Demographic and characterization of patients
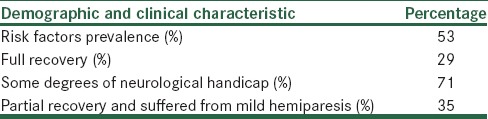
Table 2.
Distribution of neurological outcome after arterial ischemic stroke in children
DISCUSSION
The incidence of pediatric stroke has been reported as 1.2–13 case per 100,000 children in different studies.[15] Clinical manifestations of stroke include hemiparesis, hemiplegia, facial palsy, seizure, and loss of consciousness. Long-term neurological outcome of stroke varies from lack of any presentation full recovery to severe neurological disability. Sequels of stroke, such as focal neurological deficit, cognitive impairment, speech problem, seizure, and movement disorder, may impact daily life.[4,5,8,9] Mortality of stroke is 0.2–15%. Stroke recurrence in different studies has been reported as 14–22%. Full recovery has been reported in 20–30% of the patients. Despite predictable neuronal plasticity in children, most of the children with stroke suffer from neurological sequels of stroke.[4]
In a study on 33 children with stroke who had been followed for 2 years, residual neurological problems were observed in in two-thirds of children.[16]
A study performed in London on functional outcomes after stroke demonstrated that more than half of the patients present no activity restriction and the rest of the patients displayed mild to moderate limitation, primarily in domains of motor, cognitive, and self-care abilities. Moreover, severity of disabilities was well associated with the extent of brain damage.[17]
A large prospective study of childhood stroke outcome on 123 patients with arterial ischemic stroke in Canada indicated full recovery in 45% of the patients. Associated neurologic disorders and need to rehabilitation were predictors of poorer prognosis.[18]
In a study of consequences of childhood stroke in adolescence in 26 patients in Canada, 80% of cases found complete recovery or experienced mild disabilities. In this multimodal assessment of stroke outcome, arteriopathy, need to rehabilitation services, modified ranking scale more than or equal to 1 were predictors of poorer outcome.[5]
In a retrospective study in Turkey of 98 children with AIS, 66% of patients had focal deficit, 52 patients had seizure, and 18 patients died.[15]
Our study demonstrated full recovery in 15 (29%) of the patients.
Most of the patients with full recovery had presented mild motor disability. In our study, 8 of 11 cases with mild presenting symptom had full recovery compared to 7 of 42 patients with more severe initial motor disability.
Focal neurological deficits are the most common long-term sequel of stroke in children. In a few studies on stroke outcome in children, 30–70% of the patients had focal deficits as hemiplegia, hemiparesis, and facial palsy.[9,10,11]
In our study, 38 patients (71%) had some degrees of neurological handicap. Severity of initial functional disability was significantly related with poor functional outcome.
Cognitive impairment after stroke has been reported in different studies. While, in our study, cognitive function was not evaluated with exact quantitatively organized methods, based on qualitative evaluations some degree of cognitive impairment influencing the school performance was observed in 6 patients (11%).
Recurrence of stroke was a major risk factor for cognitive impairment in our study.
Mortality was 2–15% in different studies. Loss of consciousness, hematologic dysfunctions, and hemorrhagic transformation were associated with higher mortality rate.[15,19]
In our study, mortality was observed in 2 patients. One of them had moyamoya and had experienced four episodes of stroke.
Incidence of secondary epilepsy has been reported to be 15–20% in previous studies.[8,19,20] In our study, 11 patients (20%) had secondary epilepsy and needed anticonvulsant therapy for seizure control. Seizure in the 1st day after stroke was a major risk factor for secondary epilepsy in our patients.
In our study, stroke recurrence and severity of presenting symptoms were the most important risk factors for severe neurological handicap. Five of 8 patients with severe neurological deficits had experienced stroke recurrence.
CONCLUSION
Stroke recurrence and severity of presenting symptoms are the most important risk factors in final prognosis of stroke in children. Recurrence of stroke was observed in patients with multiple risk factors for stroke. Therefore, extensive evaluation of any patient with stroke is highly recommended for discovering probable risk factor and appropriate treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Professor Mohammad Ghofrani for his invaluable guidance and encouragement. Also, we would like to appreciate patients and their parents for their participation in this study.
REFERENCES
- 1.Deng Y, Wang Y, Yang W, Yu Y, Xu J, Wang Y, et al. Risk factors and imaging characteristics of childhood stroke in China. J Child Neurol. 2015;30:339–43. doi: 10.1177/0883073814538667. [DOI] [PubMed] [Google Scholar]
- 2.Mallick AA, Ganesan V, Kirkham FJ, Fallon P, Hedderly T, McShane T, et al. Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: A prospective population-based study. Lancet Neurol. 2014;13:35–43. doi: 10.1016/S1474-4422(13)70290-4. [DOI] [PubMed] [Google Scholar]
- 3.Giroud M, Lemesle M, Gouyon JB, Nivelon JL, Milan C, Dumas R. Cerebrovascular disease in children under 16 years of age in the city of Dijon, France: A study of incidence and clinical features from 1985 to 1993. J Clin Epidemiol. 1995;48:1343–8. doi: 10.1016/0895-4356(95)00039-9. [DOI] [PubMed] [Google Scholar]
- 4.Gomes A, Rinehart N, Greenham M, Anderson V. A critical review of psychosocial outcomes following childhood stroke (1995-2012) Dev Neuropsychol. 2014;39:9–24. doi: 10.1080/87565641.2013.827197. [DOI] [PubMed] [Google Scholar]
- 5.Elbers J, deVeber G, Pontigon AM, Moharir M. Long-term outcomes of pediatric ischemic stroke in adulthood. J Child Neurol. 2014;29:782–8. doi: 10.1177/0883073813484358. [DOI] [PubMed] [Google Scholar]
- 6.Lee EH, Yum MS, Ko TS. Risk factors and clinical outcomes of childhood ischemic stroke in a single Korean tertiary care center. J Child Neurol. 2012;27:485–91. doi: 10.1177/0883073811420297. [DOI] [PubMed] [Google Scholar]
- 7.Lo W, Gordon AL, Hajek C, Gomes A, Greenham M, Anderson V, et al. Pediatric stroke outcome measure: Predictor of multiple impairments in childhood stroke. J Child Neurol. 2014;29:1524–30. doi: 10.1177/0883073813503186. [DOI] [PubMed] [Google Scholar]
- 8.Mallick AA, O’Callaghan FJ. Risk factors and treatment outcomes of childhood stroke. Expert Rev Neurother. 2010;10:1331–46. doi: 10.1586/ern.10.106. [DOI] [PubMed] [Google Scholar]
- 9.Hajek CA, Yeates KO, Anderson V, Mackay M, Greenham M, Gomes A, et al. Cognitive outcomes following arterial ischemic stroke in infants and children. J Child Neurol. 2014;29:887–94. doi: 10.1177/0883073813491828. [DOI] [PubMed] [Google Scholar]
- 10.Fox CK, Glass HC, Sidney S, Lowenstein DH, Fullerton HJ. Acute seizures predict epilepsy after childhood stroke. Ann Neurol. 2013;74:249–56. doi: 10.1002/ana.23916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abend NS, Beslow LA, Smith SE, Kessler SK, Vossough A, Mason S, et al. Seizures as a presenting symptom of acute arterial ischemic stroke in childhood. J Pediatr. 2011;159:479–83. doi: 10.1016/j.jpeds.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chadehumbe MA, Khatri P, Khoury JC, Alwell K, Szaflarski JP, Broderick JP, et al. Seizures are common in the acute setting of childhood stroke: A population-based study. J Child Neurol. 2009;24:9–12. doi: 10.1177/0883073808320756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sträter R, Becker S, von Eckardstein A, Heinecke A, Gutsche S, Junker R, et al. Prospective assessment of risk factors for recurrent stroke during childhood – A 5-year follow-up study. Lancet. 2002;360:1540–5. doi: 10.1016/S0140-6736(02)11520-0. [DOI] [PubMed] [Google Scholar]
- 14.Rodan L, McCrindle BW, Manlhiot C, MacGregor DL, Askalan R, Moharir M, et al. Stroke recurrence in children with congenital heart disease. Ann Neurol. 2012;72:103–11. doi: 10.1002/ana.23574. [DOI] [PubMed] [Google Scholar]
- 15.Per H, Unal E, Poyrazoglu HG, Ozdemir MA, Donmez H, Gumus H, et al. Childhood stroke: Results of 130 children from a reference center in Central Anatolia, Turkey. Pediatr Neurol. 2014;50:595–600. doi: 10.1016/j.pediatrneurol.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 16.Pavlovic J, Kaufmann F, Boltshauser E, Capone Mori A, Gubser Mercati D, Haenggeli CE, et al. Neuropsychological problems after paediatric stroke: Two year follow-up of Swiss children. Neuropediatrics. 2006;37:13–9. doi: 10.1055/s-2006-923932. [DOI] [PubMed] [Google Scholar]
- 17.deVeber GA, MacGregor D, Curtis R, Mayank S. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol. 2000;15:316–24. doi: 10.1177/088307380001500508. [DOI] [PubMed] [Google Scholar]
- 18.Emam AT, Ali AM, Babikr MA. Childhood stroke in Eastern Province, KSA: Pattern, risk factors, diagnosis and outcome. Acta Paediatr. 2009;98:1613–9. doi: 10.1111/j.1651-2227.2009.01421.x. [DOI] [PubMed] [Google Scholar]
- 19.Salih MA, Abdel-Gader AG, Al-Jarallah AA, Kentab AY, Al-Nasser MN. Outcome of stroke in Saudi children. Saudi Med J. 2006;27(Suppl 1):S91–6. [PubMed] [Google Scholar]
- 20.Naess H, Waje-Andreassen U, Thomassen L, Nyland H, Myhr KM. Do all young ischemic stroke patients need Long-term secondary preventive medication? Neurology. 2005;65:609–11. doi: 10.1212/01.wnl.0000173029.89752.7b. [DOI] [PubMed] [Google Scholar]


