Abstract
Background:
Myeloperoxidase (MPO) is an enzyme, elevated in the atheroma and serum of a patient with atherosclerotic vessels. The aim of this study is to investigate whether the serum MPO level is related to the presence of plaque in patients without risk factors, such as, diabetes, hypertension, obesity, and hyperlipidemia.
Materials and Methods:
A serum sample was collected from patients who referred for angiography. The MPO level was measured in the serum samples of 40 patients without risk factors for atherosclerosis using the enzyme-linked immunosorbent assay (ELISA).
Results:
The MPO level was 245.5 ± 13.8 (ng/ml) in patients with atherosclerosis and 213.9 ± 8.9 (ng/ml) in patients without atherosclerosis. There was a significant difference between the groups (P = 0.002). The odds ratio was 0.67 (0.95 CI, 0.17 – 2.5) for patients with and without coronary atherosclerosis.
Conclusion:
Although the MPO concentration is higher in patients suffering from atherosclerosis, it is not a predictor of coronary artery disease in patients without diabetes, hypertension, obesity, and hyperlipidemia.
Keywords: Acute coronary syndrome, coronary artery disease, myeloperoxidase
INTRODUCTION
Large numbers of patients with coronary artery disease do not have any classic risk factors.[1,2] As myocardial infarction and death could be the first presentation of atherosclerotic plaque, many researchers study new methods and biomarkers to distinguish patients with atherosclerosis, as also prevention of its adverse effects. Myeloperoxidase is an enzyme stored in the azurophilic granules in immune cells, such as, neutrophils and monocytes, and is secreted during leukocyte activation. It is involved in innate immunity and reacts with hydrogen peroxide and chloride, producing hypochlorous acid (HOCl).[3] It has oxidative and inflammatory effects. Of late, MPO has been known as a measurable risk factor in acute coronary syndrome (ACS) in patients with chest pain.
Oxidative stress and inflammation have important roles in the pathogenesis of coronary artery disease (CAD) and lead to ACS.[4]
It has been implicated as a proinflammatory enzyme found in the culprit plaque and its levels are measurable in patient serum.[5]
Myeloperoxidase is capable of using nitric oxide as a substrate and its circulatory level has reverse correlation with brachial artery vasodilation.[6] It changes the biological effects of proteins and lipids resulting in hallucination, nitration, and oxidative cross-linkage.[7] It changes stable plaque to vulnerable plaque and is involved in atherosclerotic disease.[8,9] It is involved in remodeling and left ventricular dilation after acute myocardial infarction (MI).[10,11] Circulatory neutrophils in patients with acute MI or with unstable angina contain lower amounts of MPO and consequently their levels are higher in blood circulation. MPO is released after neutrophil activation.[4]
Some studies show MPO as an independent prognostic factor in patients with chest pain.
In patients without myocardial necrosis and with negative troponin T, the initial measurement of MPO concentration may help identify high-risk patients. It takes three to six hours for the troponin to reach measurable levels in the serum; however, the MPO increases immediately in the serum when the troponin is negative.[12] As immunohistochemical studies show MPO in atherosclerotic lesions and links between MPO and oxidation of low-density lipoprotein (LDL),[13,14] the serum concentration of MPO can predict coronary atherosclerosis in patients with ischemic disease.
In this study, we evaluate whether the serum level of MPO is associated with the presence of atherosclerosis in coronary arteries in patients without atherosclerotic risk factors, such as, diabetes, hypertension, obesity, and hyperlipidemia.
MATERIALS AND METHODS
This case-control study was approved by the Ethics Committee of the Isfahan University of Medical Sciences. We recruited patients who were less than 55 years old, during 18 months from the Chamran Hospital. All patients had an indication for angiography. The history of present and past medical problems was taken and the presence of CAD risk factors was defined.
History of diabetes was defined as a history of fasting blood sugar obtained twice, with a value higher than 126 mg/dl, or obtained once along with a clinical sign of hyperlipidemia, determined as an LDL higher than 160 or triglyceride higher than 150, and hypertension higher than 140/90.
Patients with CAD (defined as more than 50% stenosis documented by angiography), without a history of diabetes, hypertension, hyperlipidemia, and with a body mass index (BMI) less than 30 were selected as a case group. The control group comprised of patients without any of these risk factors and without atherosclerotic changes in the coronary arteries. The exclusion criteria were: (1) A presence of febrile and inflammatory disease, (2) malignancy, (3) liver dysfunction, (4) acute renal insufficiency, (5) autoimmune disease, (6) any thrombotic disease, and (7) heart failure class 3 and 4.
Blood samples were collected after 10–12 hours fasting for determining serum MPO and were stored at -80°C, in a freezer. Angiography was done with the Judkins standard. First, a Judkins catheter was inserted into the aorta through the femoral artery. Subsequently, an injection was administered into the coronary arteries for obtaining the left and right views, by two specialists who were unaware of the level of the MPO report data, independently.
The myeloperoxidase level was measured simultaneously in all samples in the Physiology Research Center using the enzyme-linked immunosorbent assay (ELISA) method with the ELISA kit (cat. Number: DMYE00B, R and D system). In this sandwich method, two monoclonal antibodies attached to two antigens on an MPO molecule. Then the free antibodies were washed from the wells. A substrate solution was added resulting in change of color. The process was completed by adding a stop solution, and optical density was determined in a 450 nm wave length. MPO concentration was obtained by optical density and standard curve.
Baseline characteristics of patients, MPO concentration, and presence of coronary artery disease in angiographic study were entered in SPSS 17 and analyzed.
RESULTS
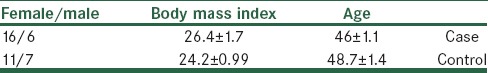
The total number of participants was 40; they had no atherosclerotic risk factors including diabetes, hypertension, obesity, and hyperlipidemia. They were divided into two groups: Case and control. Eighteen patients had coronary atherosclerotic disease. twenty-two patients were cases who had no coronary involvement. Demographic characteristics of patients including age, gender, and BMI are mentioned in Table 1. Age and BMI had no significant difference between groups.
Table 1.
Basic characteristics of patients
The myeloperoxidase level was 213 ± 8.9 ng/ml in the controls and 245.5 ± 13.8 ng/ml in the cases, with a significant difference (P = 0.002) between groups.
A study was done on 604 patients with chest pain, who presented to the Emergency Department, and 115 matched healthy subjects as controls.[15] In that study, the cutoff point was 198 PM, which enabled us to divide the patients into two groups: High MPO level and low. Based on this, in our study, we calculated the odds ratio of 0.67 (0.17–2.5) with a confidence interval of 95%.
DISCUSSION
Myeloperoxidase is an inflammatory factor that is involved in coronary artery disease. Our data suggests that even in patients suffering from CAD, without the mentioned risk factors, the MPO level is higher than in patients without CAD. High levels of MPO show background inflammation; it produces free radicals and leads to oxidative stress. If this prolongs, the high levels cause activation of special pathways. It causes LDL oxidation, binds to LDL in the plasma, and promotes site-specific oxidation of lipoproteins. It uses nitric oxide and causes endothelial dysfunction as well as decreased relaxation of smooth muscle cells because of nitric oxide in the vascular walls.[16] Correlation of MPO levels and atherosclerosis, and cardiovascular events has been proposed in recent studies. This is first done on patients without CAD risk factors. It demonstrates that the MPO level is higher in the CAD group and has a significant difference. However, it is not suggested as a marker for CAD screening.
Similar to our study, Wilson et al. demonstrate a significant correlation between serum MPO and heart failure in patients without cardiovascular disease, without diabetes, and with normal blood pressure showing that there was significant correlation between MPO and heart failure.[17]
Our study shows that regardless of cardiovascular risk factors, an increase in MPO levels is an independent factor for coronary artery disease, but cannot be used as a diagnostic factor.
The MPO concentration and CAD relation are controversial.
In a study on 333 patients, leukocyte and blood MPO concentrations were associated with the presence of CAD.[16]
In another study on 389 patients with unstable angina, without troponin elevation, the MPO levels could help identify patients with a higher risk of significant coronary stenosis; also it could predict a future need for interventions.[18]
Against these, there are studies denying this correlation.
In a study on 1018 patients in the Emergency Department with chest pain, the plasma level of MPO was measured in patients with acute coronary syndrome and noncardiac chest pain. It demonstrates that MPO has insufficient accuracy for decision-making in patients with suspected ACS.[19]
In another study on 51 patients with chest pain, the severity of CAD determined by angiography had no correlation with the MPO level.[20]
There is some dubiety in studies on ACS: Blood MPO shows early elevation in ACS subjects in the first two hours after onset of symptoms and then it decreases rapidly.[15] Blood samples for MPO analysis were collected at different time points. Also the interval of angiography and chest pain is different in patients. On the other hand, as use of statins decrease plaque instability, it is necessary to be justified between groups. The other point is that MPO is higher in eroded plaque compared to ruptured plaque.
Histopathological studies on patients dying of acute MI show two-thirds have plaque rupture, whereas, one-third have plaque erosion.
Studies with optical coherence tomography show that MPO levels are higher in eroded plaque than in ruptured plaque.[21]
This incoordination in elevation of MPO levels shows that it is not an appropriate marker for determining the risk in all patients with chest pain. Our study demonstrates that despite a higher MPO level in patients with CAD, it cannot predict the presence of atherosclerotic involvement of coronary arteries in patients without diabetes, hypertension, hyperlipidemia, and obesity.
CONCLUSION
Although MPO concentration is higher in patients with atherosclerosis, it cannot predict coronary artery disease in patients without diabetes, hypertension, obesity, and hyperlipidemia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Futterman LG, Lemberg L. Fifty percent of patients with coronary artery disease do not have any of the conventional risk factors. Am J Crit Care. 1998;7:240–4. [PubMed] [Google Scholar]
- 2.Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904. doi: 10.1001/jama.290.7.898. [DOI] [PubMed] [Google Scholar]
- 3.Gaut JP, Yeh GC, Tran HD, Byun J, Henderson JP, Richter GM, et al. Neutrophils employ the myeloperoxidase system to generate antimicrobial brominating and chlorinating oxidants during sepsis. Proc Natl Acad Sci U S A. 2001;98:11961–6. doi: 10.1073/pnas.211190298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loria V, Dato I, Graziani F, Biasucci LM. Myeloperoxidase: A new biomarker of inflammation in ischemic heart disease and acute coronary syndromes. Mediators Inflamm 2008. 2008 doi: 10.1155/2008/135625. 135625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullane KM, Kraemer R, Smith B. Myeloperoxidase activity as a quantitative assessment of neutrophil infiltration into ischemic myocardium. J Pharmacol Methods. 1985;14:157–67. doi: 10.1016/0160-5402(85)90029-4. [DOI] [PubMed] [Google Scholar]
- 6.van der Vliet A, Eiserich JP, Shigenaga MK, Cross CE. Reactive nitrogen species and tyrosine nitration in the respiratory tract: Epiphenomena or a pathobiologic mechanism of disease? Am J Respir Crit Care Med. 1999;160:1–9. doi: 10.1164/ajrccm.160.1.9807044. [DOI] [PubMed] [Google Scholar]
- 7.Nicholls SJ, Hazen SL. Myeloperoxidase and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2005;25:1102–11. doi: 10.1161/01.ATV.0000163262.83456.6d. [DOI] [PubMed] [Google Scholar]
- 8.Podrez EA, Schmitt D, Hoff HF, Hazen SL. Myeloperoxidase-generated reactive nitrogen species convert LDL into an atherogenic form in vitro. J Clin Invest. 1999;103:1547–60. doi: 10.1172/JCI5549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu X, Kassim SY, Parks WC, Heinecke JW. Hypochlorous acid oxygenates the cysteine switch domain of pro-matrilysin (MMP-7). A mechanism for matrix metalloproteinase activation and atherosclerotic plaque rupture by myeloperoxidase. J Biol Chem. 2001;276:41279–87. doi: 10.1074/jbc.M106958200. [DOI] [PubMed] [Google Scholar]
- 10.Askari AT, Brennan ML, Zhou X, Drinko J, Morehead A, Thomas JD, et al. Myeloperoxidase and plasminogen activator inhibitor 1 play a central role in ventricular remodeling after myocardial infarction. J Exp Med. 2003;197:615–24. doi: 10.1084/jem.20021426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasilyev N, Williams T, Brennan ML, Unzek S, Zhou X, Heinecke JW, et al. Myeloperoxidase-generated oxidants modulate left ventricular remodeling but not infarct size after myocardial infarction. Circulation. 2005;112:2812–20. doi: 10.1161/CIRCULATIONAHA.105.542340. [DOI] [PubMed] [Google Scholar]
- 12.Daugherty A, Dunn JL, Rateri DL, Heinecke JW. Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. J Clin Invest. 1994;94:437–44. doi: 10.1172/JCI117342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heinecke JW. Mass spectrometric quantification of amino acid oxidation products in proteins: Insights into pathways that promote LDL oxidation in the human artery wall. Faseb J. 1999;13:1113–20. doi: 10.1096/fasebj.13.10.1113. [DOI] [PubMed] [Google Scholar]
- 14.Podrez EA, Abu-Soud HM, Hazen SL. Myeloperoxidase-generated oxidants and atherosclerosis. Free Radic Biol Med. 2000;28:1717–25. doi: 10.1016/s0891-5849(00)00229-x. [DOI] [PubMed] [Google Scholar]
- 15.Brennan ML, Penn MS, Van Lente F, Nambi V, Shishehbor MH, Aviles RJ, et al. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med. 2003;349:1595–604. doi: 10.1056/NEJMoa035003. [DOI] [PubMed] [Google Scholar]
- 16.Zhang R, Brennan ML, Fu X, Aviles RJ, Pearce GL, Penn MS, et al. Association between myeloperoxidase levels and risk of coronary artery disease. JAMA. 2001;286:2136–42. doi: 10.1001/jama.286.17.2136. [DOI] [PubMed] [Google Scholar]
- 17.Tang WH, Katz R, Brennan ML, Aviles RJ, Tracy RP, Psaty BM, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol. 2009;103:1269–74. doi: 10.1016/j.amjcard.2009.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rebeiz AG, Tamim HM, Sleiman RM, Abchee AG, Ibrahim Z, Khoury MY, et al. Plasma myeloperoxidase concentration predicts the presence and severity of coronary disease in patients with chest pain and negative troponin-T. Coron Artery Dis. 2011;22:553–8. doi: 10.1097/MCA.0b013e32834c5e98. [DOI] [PubMed] [Google Scholar]
- 19.Peacock WF, Nagurney J, Birkhahn R, Singer A, Shapiro N, Hollander J, et al. Myeloperoxidase in the diagnosis of acute coronary syndromes: The importance of spectrum. Am Heart J. 2011;162:893–9. doi: 10.1016/j.ahj.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 20.de Azevedo Lucio E, Gonçalves SC, Ribeiro JP, Nunes GL, de Oliveira JR, Araujo GN, et al. Lack of association between plasma myeloperoxidase levels and angiographic severity of coronary artery disease in patients with acute coronary syndrome. Inflamm Res. 2011;60:137–42. doi: 10.1007/s00011-010-0247-8. [DOI] [PubMed] [Google Scholar]
- 21.Ferrante G, Nakano M, Prati F, Niccoli G, Mallus MT, Ramazzotti V, et al. High levels of systemic myeloperoxidase are associated with coronary plaque erosion in patients with acute coronary syndromes: A clinicopathological study. Circulation. 2010;122:2505–13. doi: 10.1161/CIRCULATIONAHA.110.955302. [DOI] [PubMed] [Google Scholar]


