Abstract
Background and Objectives:
The mediastinum is a relatively uncommon site of distant metastases, which typically appear as peripheral lung nodules. We chose to assess the utility of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) for the diagnosis of distant metastases to the mediastinum.
Materials and Methods:
Over the period 2008–2013, a total of 446 patients with concurrent or previously diagnosed and treated extrathoracic malignancies were evaluated.
Results:
Surgical treatment was carried out in 414 patients (156 women and 237 men aged 26–68 years, mean age of 56.5 years) presenting with distant metastases to the lungs: Thoracoscopic wedge resection was completed in 393 patients and lobectomy and segmentectomy were performed in 7 and 14 patients, respectively. The median time from primary tumor resection was 6.5 years (range: 4.5 months to 17 years). Thirty-two of these patients underwent EBUS-TBNA for mediastinal manifestation of the underlying disease. EBUS-TBNA specimens were aspirated from the subcarinal or right paratracheal lymph node stations in 26 (81%) patients and from the hilar lymph nodes in 6 (18.8%) patients only. Metastases to lymph nodes were confirmed in 14 of these patients (43.8%). Primary lung cancer was diagnosed in seven patients. Mediastinoscopy was performed in two patients to reveal either lymph node metastasis or sarcoidosis. Thoracotomy for pulmonary metastases resection and mediastinal lymph node biopsy was performed in nine patients. Lymph node metastasis was confirmed in five patients (15.6%). The diagnostic efficacy, sensitivity, specificity, and negative predictive value (NPV) of EBUS-TBNA were 78.8%, 93.3%, 100%, and 87.5%, respectively.
Conclusion:
EBUS-TBNA is a valuable diagnostic tool in a selected group of patients with secondary tumors in the mediastinum and lungs.
Keywords: Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), mediastinal, metastases
INTRODUCTION
Pulmonary metastases from distant primary tumors are indicative of late-stage cancer. In isolated cases, in around 20% of patients, metastasectomy is the treatment of choice delivering better long-term outcomes.[1] Preoperative imaging [computed tomography (CT), positron emission tomography-computed tomography (PET-CT)] is highly useful; however, in 37% of surgical patients, the actual number of neoplastic lesions present during surgery is reported to be higher than the one detected with radiological imaging.[2] Moreover, the incidence of metastases to lymph nodes in the pulmonary hilum or mediastinum can be as high as 42.4% in some types of cancer.[3] There is considerable evidence that the presence of mediastinal metastases at the time of metastasectomy is usually associated with shorter survival.[4] Some authors actually believe that operative treatment is contraindicated in patients who present with lymph node metastases.[5] The issue still remains controversial, which highlights the importance of preoperative diagnostic tests of mediastinal lymph nodes. For many years, mediastinoscopy has been the standard investigation of choice. Over the last decade, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) and other endoscopic procedures have grown in importance and have been successfully used for the diagnosis of primary lung cancer. However, only few studies have demonstrated the diagnostic efficacy of this tool.[6] In this paper, we chose to assess the diagnostic utility of EBUS-TBNA for distant metastases to the mediastinum.
MATERIALS AND METHODS
Lymph node sampling
The EBUS-TBNA procedure was performed with Pentax EB-1970UK ultrasound video bronchoscope, EPK-1,000 digital video processor, Hitachi Hi Vision 5,500 processor, and a convex-probe linear array endobronchial ultrasound bronchoscope (Olympus XBF-UC260F-OL8; Olympus Ltd., Tokyo, Japan). A dedicated 22-gauge needle was used for lymph node sampling. Needle aspiration of the largest accessible lymph nodes was ultrasound-guided. An internal stylet was removed after the initial puncture and negative pressure was applied with a syringe to obtain histological cores and cytological specimens. The aspirated material was smeared onto glass slides; smears were fixed in 95% alcohol. Papanicolaou staining and light microscopy were also performed by an independent cytopathologist. Histological cores were fixed with formalin and stained with hematoxylin and eosin. Immunohistochemistry was also performed when necessary.
Mediastinoscopy
Standard cervical mediastinoscopy was performed in two patients who were previously tumor-negative by EBUS-TBNA. The procedure was performed in an operating room under general anesthesia. Biopsies from stations 4R, 7, and 4L were routinely obtained. Four patients underwent surgical resection of the peripheral tumor and dissection of lymph nodes. The results of the surgical pathology specimens' evaluation were subsequently correlated with EBUS-TBNA results.
Statistical methods
Sensitivity, specificity, and accuracy were calculated using standard definitions. Negative predictive value (NPV) was calculated with the following formula: Number of true negatives/(number of true negatives — Number of false negatives). NPV was calculated for a 95% confidence interval.
RESULTS
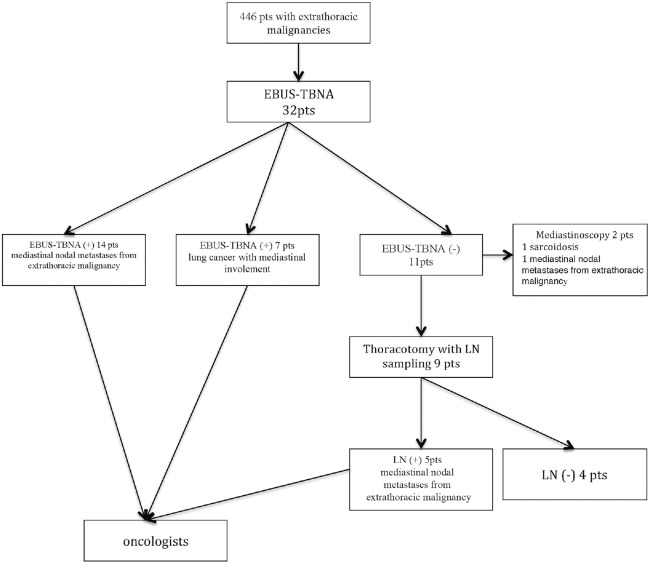
Over the period 2008-2013, a total of 446 patients (188 women and 237 men aged 26-68 years, mean age of 56.5 years) diagnosed with distant metastases to the lungs were operated upon. The median time from primary tumor resection was 6.5 years (range: 4.5 months to 17 years). CT and PET-CT revealed the presence of peripheral lung tumors in 414 patients (93%). Thoracoscopic wedge resection was performed in 393 (95%) patients with peripheral lesions; lobectomy and segmentectomy were performed in 7 (1.7%) and 14 (3.4%) of these patients, respectively. Lesions within the mediastinum were detected with diagnostic imaging in 32 (7%) patients. Additionally, 32 out of 446 patients underwent EBUS-TBNA due to mediastinal manifestation of the underlying disease. The median size of sampled lymph nodes was 16 mm (range: 12-32 mm). The mean number of lymph node stations biopsied per patient was 1.9 (range: 1.0-2.6). Patients were suspected to have intrathoracic lymph node metastases based on enlargement (short axis >10 mm) visualized by CT or F-18 fluorodeoxyglucose (FDG) uptake ≥standard uptake value (SUV) 2.5 on PET scans. Mean FDG uptake was 4.7 (range: 2.8-9.6) [Table 1]. Before EBUS-TBNA, each patient was examined by a pulmonologist using a flexible bronchoscopy procedure. No endobronchial mucosal abnormality was found in any patient. All EBUS-TBNA procedures were performed under moderate sedation with intravenous midazolam alone or midazolam and fentanyl by the same interventional pulmonologist. Each node underwent a median of four passes (range: 2-6). Kidney cancer (n = 9), breast cancer (n = 7), and colon cancer (n = 4) were most common in patients with mediastinal manifestations of the underlying disease. Overall, EBUS-TBNA procedures were performed in the study population. The subcarinal or right paratracheal lymph node stations were the site of aspiration in 26 (81%) patients. Six (18.8%) patients had only hilar lymph nodes sampled. In the majority of patients, biopsy specimens were collected from lymph node stations 7 (n = 21) and 4R (n = 15). Metastases to the lymph nodes were confirmed in 14 patients (21.9%). Primary lung cancer was diagnosed in seven patients (21.2%). Mediastinoscopy was performed in two patients to reveal either lymph node metastasis (kidney cancer) or sarcoidosis. Thoracotomy for resection of lung metastases and mediastinal lymph nodes biopsy was performed in nine patients. Lymph node metastases were confirmed in five patients (15.6%). Metastatic lymph nodes at stations 7 and 4R were found in three and two patients, respectively. Four (12.5%) patients were negative [Table 2]. All patients with positive EBUS-TBNA mediastinal lymph nodes were disqualified from surgery [Figure 1]. The diagnostic efficacy, sensitivity, specificity, and NPV of EBUS-TBNA were 78.8%, 93.3%, 100%, and 87.5%, respectively.
Table 1.
Patient characteristics (N = 446)
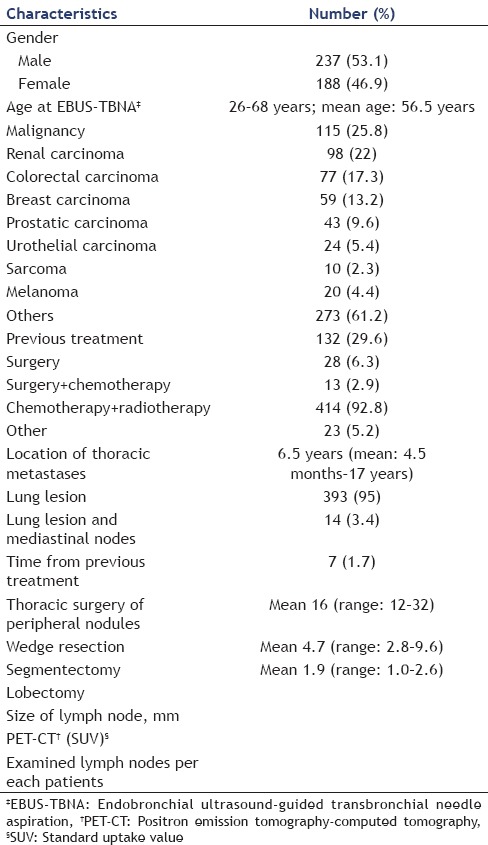
Table 2.
Histological and clinical data
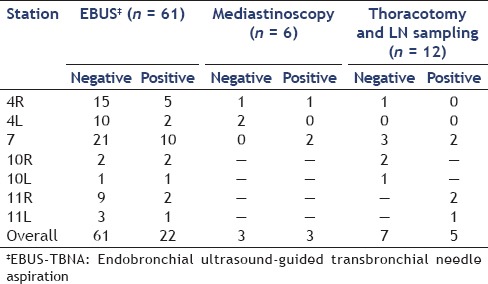
Figure 1.
Distribution of patients by EBUS-TBNA findings, follow-up, and final diagnosis. EBUS-TBNA: Endobronchial ultrasound-guided transbronchial needle aspiration; LN: Lymph node
DISCUSSION
Distant metastases to the lungs are observed in 25%-30% of cancer patients.[7] Removal of all metastatic foci by surgery is an established therapeutic method used for many years. Almost 50% of all patients with kidney cancer present with pulmonary metastases at diagnosis.[8] Late results of conservative treatment are poor; 5-year survival is observed only in 15%-20% of these patients.[9] Postmetastasectomy late results are significantly better, with 5-year survival of 60%.[10] On the other hand, 5-year survival of 3%-11% was reported for nonoperated patients. In a study by Pastorino et al.,[11] the 5-, 10- and 15-year survival statistics reported for a group of 5,206 patients with different cancer types were 36%, 26%, and 22%, respectively, with a mean survival of 36 months. The presence of metastases to the mediastinal lymph nodes is a controversial problem. In studies by Pfannschmidt et al.,[12] mediastinal involvement was observed in 16.1% of the patients with colon cancer and in 15.7% of the patients with kidney cancer. In other studies, the incidence of mediastinal lymph node metastases was significantly higher, up to 28.6%.[13] There is considerable evidence that the presence of mediastinal lymph node metastases is typically associated with a poor prognosis; some authors claim it to be an independent prognostic factor.[14] It is worth noting that mediastinal lymph node sampling during thoracotomy and lymphadenectomy are performed by only 55.5% and 13% of surgeons, respectively.[15] Controversies surrounding the presence of metastases to the mediastinal lymph nodes are important from the perspective of eligibility assessment for surgical treatment. Some authors believe that the presence of metastases to the mediastinal lymph nodes is a contraindication to surgical treatment in some types of cancer.[12] Other surgeons claim that this group of patients should not be considered ineligible for surgical treatment despite significantly poorer late results (mean survival in patients with LN- and LN+ is 107 and 37 months, respectively).[4] This controversy highlights the importance of preoperative diagnostic tests of mediastinal lymph nodes. A mediastinoscopy stills remains a recognized standard, with serious complications rates of 1%.[16] Therefore, EBUS-TBNA has grown in importance in recent years as the first-stage diagnostic procedure of mediastinal lymph nodes. In terms of primary lung cancer, the role of EBUS-TBNA is well-known, and the diagnostic efficacy, sensitivity, specificity, and NPV of EBUS-TBNA are 99.1%, 100%, 98.7%, and 97%, respectively.[17] Regarding distant metastases to the lungs, the outcomes for EBUS-TBNA are slightly poorer and range from 85% to 92% for sensitivity, 88% to 100% for specificity, and 73% to 76% for NPV.[18,19,20] Diagnostic efficacy, sensitivity, specificity, and NPV of EBUS-TBNA obtained in this study were 78.8%, 93.3%, 100%, and 87.5%, respectively. These results are similar to previous reports in the literature. A significant limitation of this study is that it was a retrospective analysis involving a small sample size. However, the obtained results allow the conclusion that EBUS-TBNA is a valuable diagnostic tool in a selected group of patients with secondary tumors of the mediastinum and lungs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Younes RN, Gross JL, Taira AM, et al. Surgical resection of Lung metastases: Results from 529 patients. Clinics (Sao Paulo) 2009;64:535–41. doi: 10.1590/S1807-59322009000600008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cerfolio RJ, Bryant AS. Is palpation of the nonresected pulmonary lobe(s) required for patients with non-small cell lung cancer. A prospective study? J Thorac Cardiovasc Surg. 2008;131:261–8. doi: 10.1016/j.jtcvs.2007.08.062. [DOI] [PubMed] [Google Scholar]
- 3.Pfannschmidt J, Klode J, Muley T, et al. Nodal involvement at the time of pulmonary metastasectomy: Experiences in 245 Patients. Ann Thorac Surg. 2006;81:448–54. doi: 10.1016/j.athoracsur.2005.08.049. [DOI] [PubMed] [Google Scholar]
- 4.Renaud S, Falcoz PE, Alifano M, et al. Systematic lymph node dissection in lung metastasectomy of renal cell carcinoma: An 18 years of experience. J Surg Oncol. 2014;109:823–9. doi: 10.1002/jso.23593. [DOI] [PubMed] [Google Scholar]
- 5.Meimarakis G, Angele MK, Schneider C, et al. Impact of systematic lymph node dissection in the resection of pulmonary metastases of solid extrapulmonary tumours. Zentralbl Chir. 2010;135:556–63. doi: 10.1055/s-0030-1247314. [DOI] [PubMed] [Google Scholar]
- 6.Nakajima T, Yasufuku K, Iyoda A, et al. The evaluation of lymph node metastasis by endobronchial ultrasound-guided transbronchial needle aspiration: Crucial for selection of surgical candidates with metastatic lung tumors. J Thorac Cardiovasc Surg. 2007;134:1485–90. doi: 10.1016/j.jtcvs.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 7.Kudelin N, Bölükbas S, Eberlein M, et al. Metastasectomy with standardized lymph node dissection for metastatic renal cell carcinoma: An 11-year single-center experience. Ann Thorac Surg. 2013;96:265–71. doi: 10.1016/j.athoracsur.2013.04.047. [DOI] [PubMed] [Google Scholar]
- 8.Dekernion JB, Ramming KP, Smith RB. The natural history of metastatic renal cell carcinoma: A computer analysis. J Urol. 1978;120:148–52. doi: 10.1016/s0022-5347(17)57082-2. [DOI] [PubMed] [Google Scholar]
- 9.Ravaud A, Audhuy B, Gomez F, et al. Subcutaneous interleukin-2, interferon alfa-2a, and continuous infusion of fluorouracil in metastatic renal cell carcinoma: A multicenter phase II trial. Groupe Français d'Immunothérapie. J Clin Oncol. 1998;16:2728–32. doi: 10.1200/JCO.1998.16.8.2728. [DOI] [PubMed] [Google Scholar]
- 10.Kavolius JP, Mastorakos DP, Pavlovich C, et al. Resection of metastatic renal cell carcinoma. J Clin Oncol. 1998;16:2261–6. doi: 10.1200/JCO.1998.16.6.2261. [DOI] [PubMed] [Google Scholar]
- 11.Pastorino U, Buyse M, Friedel G, et al. The International Registry of Lung Metastases. Long-term results of lung metastasectomy: Prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg. 1997;113:37–49. doi: 10.1016/s0022-5223(97)70397-0. [DOI] [PubMed] [Google Scholar]
- 12.Pfannschmidt J, Egerer G, Bischof M, et al. Surgical intervention for pulmonary metastases. Dtsch Arztebl Int. 2012;109:645–51. doi: 10.3238/arztebl.2012.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ercan S, Nichols FC, 3rd, Trastek VF, et al. Prognostic significance of lymph node metastasis found during pulmonary metastasectomy for extrapulmonary carcinoma. Ann Thorac Surg. 2004;77:1786–91. doi: 10.1016/S0003-4975(03)01200-1. [DOI] [PubMed] [Google Scholar]
- 14.Iizasa T, Suzuki M, Yoshida S, et al. Prediction of prognosis and surgical indications for pulmonary metastasectomy from colorectal cancer. Ann Thorac Surg. 2006;82:254–60. doi: 10.1016/j.athoracsur.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Yuste M, Cassivi S, Paleru C. Thoracic lymphatic involvement in patients having pulmonary metastasectomy: Incidence and the effect on prognosis. J Thorac Oncol. 2010;5(Suppl 2):S166–9. doi: 10.1097/JTO.0b013e3181dcf920. [DOI] [PubMed] [Google Scholar]
- 16.Navani N, Nankivell M, Woolhouse I, et al. Endobronchial ultrasound-Guided transbronchial needle aspiration for the diagnosis of intrathoracic lymphadenopathy in patients with extrathoracic malignancy: A multicenter study. J Thorac Oncol. 2011;6:1505–9. doi: 10.1097/JTO.0b013e318223c3fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vincent BD, El-Bayoumi E, Hoffman B, et al. Real-time endobronchial ultrasound-guided transbronchial lymph node aspiration. Ann Thorac Surg. 2008;85:224–30. doi: 10.1016/j.athoracsur.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 18.Tournoy KG, Govaerts E, Malfait T, et al. Endobronchial ultrasound-guided transbronchial needle biopsy for M1 staging of extrathoracic malignancies. Ann Oncol. 2011;22:127–31. doi: 10.1093/annonc/mdq311. [DOI] [PubMed] [Google Scholar]
- 19.Chen F, Miyahara R, Sato T, et al. Usefulness of endobronchial ultrasound in patients with previously treated thoracic malignancy. Interact Cardiovasc Thorac Surg. 2012;14:34–7. doi: 10.1093/icvts/ivr043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanz-Santos J, Cirauqui B, Sanchez E, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of intrathoracic lymph node metastases from extrathoracic malignancies. Clin Exp Metastasis. 2013;30:521–8. doi: 10.1007/s10585-012-9556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]