Abstract
Recently, the role of 18F-choline in the detection of parathyroid adenomas has been reported. At our institution, we are currently studying the role of this tracer in comparison to the standard methoxy-isobutyl-isonitrile.(MIBI) scan with single photon emission tomography/computed tomography. Our initial results show that 18F-choline is at least as good as 99mTc-MIBI scan. We present here a representative case of a 45-year-old woman with multiple skeletal lytic lesions and a high parathyroid hormone.(PTH) who underwent both these imaging techniques with concordant results, further confirmed by histopathology and postoperative fall in serum PTH levels.
Keywords: 18F-choline positron emission tomography/computed tomography, methoxy-isobutyl-isonitrile scan, parathyroid adenoma
INTRODUCTION
Surgical excision of abnormal parathyroid tissue whether adenoma, carcinoma, or hyperplasia is considered as the definitive treatment of hyperparathyroidism. Surgery is the standard of care due to potential long-term skeletal, cardiovascular, and neuropsychiatric effects of even mild hyperparathyroidism.[1] Nuclear medicine imaging techniques have played an important role in the detection and localization of parathyroid adenomas, with 99mTc-methoxy-isobutyl-isonitrile (MIBI) scan currently being the standard test used. The addition of single photon emission computed tomography/computed tomography (SPECT/CT) has had an incremental benefit in exact localization of the adenomas.
Although 18F-choline has been used as a photon emission tomography (PET) tracer for some years now, its utility in the detection of parathyroid adenomas has only recently been explored.
We are currently studying the role of this modality vis-a-vis 99mTc-MIBI scan with early SPECT/CT in patients with primary hyperparathyroidism.
CASE REPORT
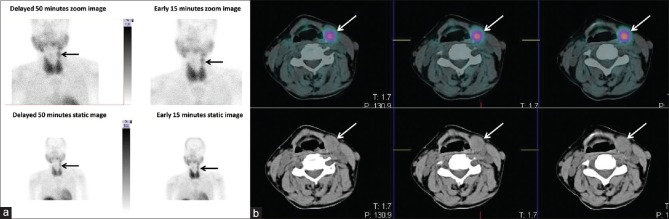
A 45-year-old female patient presented with complaints of bone pain and difficulty in walking for last 3 months. A plain radiograph of bilateral hip joints ordered by a local practitioner showed multiple lytic areas in the pelvis and femora. A workup for multiple myeloma returned negative. She was referred to a tertiary care institute for a fluorodeoxyglucose (FDG) PET/CT, in which multiple poorly FDG avid skeletal lesions were reported with no evidence of primary malignant pathology. The patient was referred to our institution for further management. A review of the FDG PET/CT revealed a rounded lesion measuring 2.2 cm with mild FDG uptake superior to the upper pole of the left lobe of thyroid just inferior to the left submandibular gland lateral to and abutting the left lamina of thyroid cartilage. Her renal function was deranged for at least last 1 year, and last serum creatinine was 1.9 mg%. She was also having celiac disease. In view of clinical history, we ordered a parathyroid hormone (PTH) assay which showed a value of more than 3000 pg/ml from two different laboratories. Her serum calcium was 10.4 mg/dl (laboratory normal 8.80–10.60) and serum phosphorus was 3.60 mg/dl (2.40–4.40), and Vitamin D levels were consistently in deficient range. We proceeded with a 99mTc-MIBI scan and early, delayed and early SPECT/CT images were taken which revealed high uptake in the above lesion. This was interpreted as an ectopic left superior parathyroid adenoma [Figure 1a and b]. No other adenoma was localized. As part of our ongoing study, she underwent a 18F-choline PET/CT study post 3 mCi intravenous injection of the tracer, which showed intense uptake in the above lesion [Figure 2a and b]. We found the lesion to thyroid ratio much higher than that seen in the MIBI scan, making the images easier to interpret. A diagnosis of ectopic left superior parathyroid adenoma arising in the probable setting of tertiary hyperparathyroidism was made. The patient underwent focused parathyroidectomy with a 70% reduction in iPTH levels intraoperatively. Frozen and permanent section histopathology returned as parathyroid adenoma. One month after surgery, the patient reported a significant improvement in her symptoms and PTH levels have returned to near normal.
Figure 1.
(a) Planar early and delayed images of 99mTc-methoxy-isobutyl-isonitrile scan showing a focus of increased tracer uptake superior to the left lobe of thyroid (black arrow). (b) Single photon emission computed tomography/computed tomography done after the early image reveals the same lesion (white arrow) measuring 2.2 cm × 1.5 cm × 2.3 cm inferior to the left submandibular gland, closely abutting the left lamina of thyroid cartilage
Figure 2.
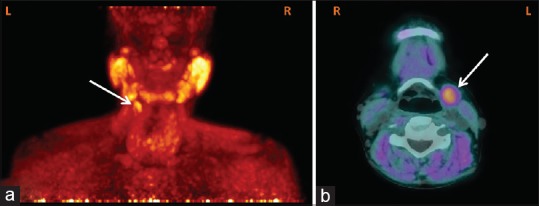
(a and b) Maximum intensity projection (posterior view) and transaxial images of 18F-choline photon emission tomography/computed tomography image showing the ectopic left superior parathyroid adenoma with intense uptake (white arrow)
DISCUSSION
In the era of PET/CT, various tracers have been tried for accurate localization of parathyroid adenomas. However, the efficacy of FDG, fluorodopa, and 11C-methionine has not been established so far. A search for a PET-based tracer is ongoing that can be as good as MIBI scan or better. 18F-choline has recently been reported as a possible novel PET agent for parathyroid localization preoperatively.[2,3,4,5,6] The possible mechanism for choline uptake is its conversion into phosphatidylcholine by the enzyme choline kinase and subsequent incorporation into the cell membrane.
A recent study by Lezaic et al. in 24 patients revealed that the sensitivity and specificity of 18F-choline PET/CT were 92% and 100%, and sensitivity was much higher than any of the conventional scintigraphic techniques.[2] Cazaentre et al. reported incidental uptake of 18F-choline in parathyroid hyperplasia in a case of prostate cancer.[4] In a study of 12 patients by Michaud et al., the authors found a detection rate of 92% for 18F-choline PET/CT and it also solved discrepant results between MIBI scan and ultrasound.[6]
Few authors have also demonstrated choline uptake in parathyroid adenomas using 11C-choline.[7,8] Kluijfhout et al. reported a case where 18F-choline PET/CT enabled a minimally invasive surgery for parathyroid adenoma in a patient with negative ultrasound and MIBI scan.[9]
No larger studies have been performed in this regard yet. At our institution, we do not have 11C-choline, and synthesis of 18F-choline has only recently started. In this particular case, the diagnosis was reliably made on MIBI scan, but 18F-choline PET/CT proved to be as good as MIBI scan. There are emerging reports of the superiority of 18F-choline over MIBI scan.[9] This investigation offers high sensitivity comparable to already established nuclear medicine techniques. Furthermore, unlike MIBI scan, the choline PET/CT in our case showed a very high lesion to thyroid ratio. Thus, it may be easier to report smaller lesions very close to the thyroid with this modality. It appears to provide additional hope specially in cases of low gland mass and multi-gland involvement due to better resolution of PET/CT as compared to SPECT/CT coupled with good image contrast. We feel that 18F-choline is, therefore, a promising tracer requiring further investigation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of clinical endocrinologists and the American Association of endocrine surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49–54. doi: 10.4158/EP.11.1.49. [DOI] [PubMed] [Google Scholar]
- 2.Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: A pilot study. Eur J Nucl Med Mol Imaging. 2014;41:2083–9. doi: 10.1007/s00259-014-2837-0. [DOI] [PubMed] [Google Scholar]
- 3.Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab. 2013;98:3111–2. doi: 10.1210/jc.2013-2084. [DOI] [PubMed] [Google Scholar]
- 4.Cazaentre T, Clivaz F, Triponez F. False-positive result in 18F-fluorocholine PET/CT due to incidental and ectopic parathyroid hyperplasia. Clin Nucl Med. 2014;39:e328–30. doi: 10.1097/RLU.0b013e3182a77b62. [DOI] [PubMed] [Google Scholar]
- 5.Hodolic M, Huchet V, Balogova S, Michaud L, Kerrou K, Nataf V, et al. Incidental uptake of (18) F-fluorocholine (FCH) in the head or in the neck of patients with prostate cancer. Radiol Oncol. 2014;48:228–34. doi: 10.2478/raon-2013-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michaud L, Burgess A, Huchet V, Lefèvre M, Tassart M, Ohnona J, et al. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab. 2014;99:4531–6. doi: 10.1210/jc.2014-2821. [DOI] [PubMed] [Google Scholar]
- 7.Mapelli P, Busnardo E, Magnani P, Freschi M, Picchio M, Gianolli L, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med. 2012;37:593–5. doi: 10.1097/RLU.0b013e31824c5ffc. [DOI] [PubMed] [Google Scholar]
- 8.Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-choline PET/CT: Preliminary results. Clin Nucl Med. 2014;39:1033–8. doi: 10.1097/RLU.0000000000000607. [DOI] [PubMed] [Google Scholar]
- 9.Kluijfhout WP, Vriens MR, Valk GD, Barth RE, Borel Rinkes IH, de Keizer B. (18) F-Fluorocholine PET-CT enables minimal invasive parathyroidectomy in patients with negative sestamibi SPECT-CT and ultrasound: A case report. Int J Surg Case Rep. 2015;13:73–5. doi: 10.1016/j.ijscr.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]