Abstract
Background
Cataract surgery is associated with the development of late-onset age-related macular degeneration (AMD). The pathogenic mechanism is still not fully established. The purpose of this study was to evaluate the possible changes in central macula thickness (CMT) and subfoveal choroid thickness (SCT) after uneventful cataract surgery.
Material/Methods
A total of 65 eyes of 65 patients who underwent phacoemulsification and intracapsular lens implantation were included in this prospective study. Patients had not undergone previous ocular surgery and had no other ocular abnormality. CMT and SCT were measured at baseline and postoperatively at week 1 and months 1, 3, 6 and 12 via spectral domain optical cohorence tomography (SD-OCT).
Results
CMT was 252.4±27.6 μm (mean ±SD) preoperatively, then 253.5±29.8, 256.1±28.7, 257.4±27.2, 253.18±23.7, and 252.8±21.7 μm at postoperative week 1 and postoperative months 1, 3, 6, and 12, respectively. There were insignificant changes in CMT, and it returned to baseline at six months after surgery (all p>0.05). SCT was 237.4±21.6 μm preoperatively, and 240.5±24.8, 241.2±25.7, 242.7±26.3, 243.1±24.2, and 244.2±21.4 μm at postoperative week 1 and postoperative months 1, 3, 6, and 12, respectively. Although there was an increase in SCT during follow-up, the difference between preoperative and postoperative values was not significant (p>0.05).
Conclusions
Uncomplicated phacoemulsification induces subclinical changes in CMT, probably due to the inflammatory insult of surgery, and CMT returns to baseline value. There were slight, insignificant increases in choroid thickness during follow-up, and this did not return to baseline during follow-up. Changes in the choroid after cataract surgery may provide clues to the development of late-onset AMD.
MeSH Keywords: Cataract Extraction; Choroidal Neovascularization; Macular Degeneration; Tomography, Optical Coherence
Background
The choroid is the vascular structure between the retinal pigment epithelium (RPE) and lamina fusca layers of the sclera. It is one of the regions with the highest blood circulation ratio in the human body [1], and structurally and functionally normal choroidal vessels are essential for retinal physiology. Abnormal choroidal blood volume may cause photoreceptor dysfunction and/or death of the retina [2]. Detailed examination of the choroidal structure is important for a clear understanding of important disorders that are a threat to vision, such as choroidal neovascularization, polypoidal choroidal vasculopathy, central serous chorioretinopathy and high myopia chorioretinal atrophy. Enhanced depth imaging (EDI) optical coherence tomography (OCT) is a novel method for choroidal imaging with improved depth perception [3]. In studies that have used EDI-OCT, choroidal thickness was found to be decreased in disorders such as myopic fundus, diabetic macula edema, and retinitis pigmentosa, and increased in disorders such as central serous chorioretinopathy, polypoidal choroidal vasculopathy, and neovascular age-related macular degeneration (AMD) [4–8].
Cataract surgery with phacoemulsification has become the most extensively used intraocular surgery, with very successful visual outcomes, particularly in elderly patients. Subclinical changes are reported in retinal layers, even after uncomplicated surgery [9]. Animal studies and histological research have shown that pro-inflammatory molecules released during and after surgery are active not only in the retina, but also in the choroidal tissues [10,11]. Epidemiologic studies have reported an increase in frequency of age-related macular degeneration (AMD) after cataract surgery [12,13]. This may be a result of both induction of pro-inflammatory molecules as a result of surgery and activation of reactions caused by excessive light entering the eye. Changes that occur in the choroid after cataract surgery may provide clues to the development of late-onset AMD.
Our aim in this study was to analyze changes in central macular thickness and subfoveal choroidal thickness by SD-OCT after uneventful cataract surgery. To our knowledge, there are no previous studies examining changes in choroidal thickness during a follow-up period of one year after cataract surgery.
Material and Methods
In this prospective study, we examined 65 eyes of 65 patients (30 female, 35 male) who had senile cataract in their eyes. We also examined the contralateral eye of patients which did not have any problem and had not had any ophthalmic surgery during follow-up. Prior to the cataract surgery, the possible complications were explained to the patients, and all patients signed a consent form. All research and measurements followed the principles of the World Medical Association Declaration of Helsinki. The study was approved by the Kocaeli University ethics committee.
Patients were excluded if they had glaucoma, retinal disease, uveitis, diabetes mellitus, or other systemic diseases that could affect the retina and choroid, or if they were taking anti-inflammatory drugs. Patients with abnormal macular morphology preoperatively or opacification that could interfere with OCT were also excluded.
All patients underwent measurement of best corrected visual acuity, measurement of intraocular pressure (IOP) with applanation tonometry (Nidek ND 2000), biomicroscopy, fundus examination, and OCT before cataract surgery, and postoperatively at week 1 and months 1, 3, 6, and 12. CMT measurements were performed with SD-OCT (Spectralis HRA OCT; Heidelberg Engineering, Heidelberg, Germany). Central 1 mm thickness was measured by the fast macular thickness map composed of 16 parallel scans. SCT was recorded from the subfoveal area using EDI with the same OCT. Because choroidal thickness demonstrates diurnal variation, measurement was made at the same time each day (between 09.30 and 11.00 hours) [14]. All subjects were imaged by the same experienced technician.
Cataract surgeries were performed between May 2014 and December 2014 under topical anesthesia, using a standard technique. The white-colored, blue-light-filtering, hydrophobic, aspheric intraocular lens was implanted “in the bag” in all cases, and then the viscoelastic material was carefully washed out from the anterior chamber. The duration of phacoemulsification varied between 61 seconds and 171 seconds, and the mean phaco energy was between 20% and 35%. Postoperative medication was the same for all patients, consisting of dexamethasone, nepafenac, and moxifloxacin eye drops applied five times daily for three weeks.
Statistical analysis
All statistical analyses were performed using SPSS for Windows software (version 18.0, IBM SPSS, Armonk, NY, USA). All values were given as mean±SD. Changes in CMT, SCT, and IOP after surgery were analyzed by repeated-measures ANOVA and Bonferroni post hoc test. Peak postoperative values were compared with baseline by paired t-test. Values of p<0.05 were considered statistically significant.
Results
The 65 patients comprised 35 (53.8%) women and 30 (46.2%) men, aged 66.8±9.3 years (range: 45–75 years). CME was not observed by OCT in any of our patients during follow-up. Mean CMT was 252.4±27.6 μm before surgery; postoperative measurements were 253.5±29.8 μm at week 1, and 256.1±28.7 μm, 257.4±27.2 μm, 253.1±23.7 μm, and 252.8±21.7 μm at months 1, 3, 6, and 12, respectively. (Figure 1) There were insignificant slight changes in CMT and these had returned to baseline by six months after surgery (all p > 0.05) The mean CMT of contralateral eyes was 251.2±28.6 μm before surgery; postoperative measurements were 251.5±27.8 μm at week 1, and 251.1±31.7 μm, 251.9±27.2 μm, 251.6±24.7 μm, and 251.5±22.8 μm at months 1, 3, 6, and 12, respectively. There were no changes in CMT during the follow-up (all p>0.05)
Figure 1.
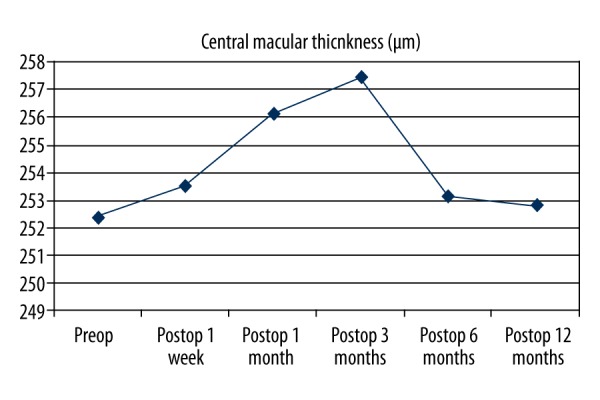
Time course of central macula thickness before (i.e., baseline) and after surgery.
Mean SCT before surgery was 237.4±21.6 μm; postoperative measurements were 240.5±24.8 μm at week 1, and 241.2±25.7 μm, 242.7±26.3, 243.1±24.2 μm, and 244.2±21.4 μm at months 1, 3, 6, and 12, respectively (Figure 2). Although there was a small increase in SCT during follow-up, the difference between preoperative and postoperative values was not significant (p>0.05). The mean SCT of contralateral eyes was 238.4±22.7 μm before surgery; postoperative measurements were 237.9±23.9 μm at week 1, and 238.1±21.6 μm, 238.4±24.2 μm, 238.2±21.9 μm, and 238.9±23.8 μm at months 1, 3, 6, and 12, respectively. There were no changes in SCT during the follow-up (all p>0.05)
Figure 2.
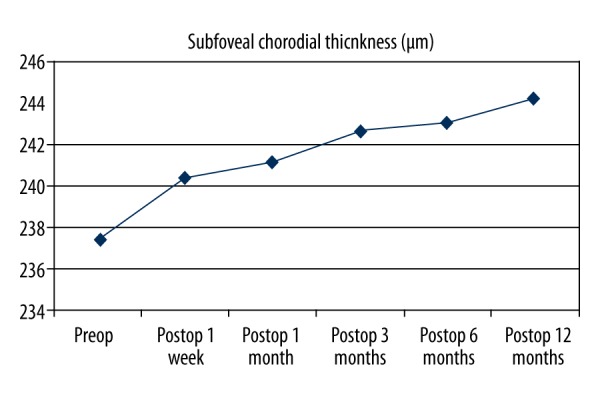
Time course of subfoveal choroidal thickness before (i.e., baseline) and after surgery.
Mean IOP was 17.6±2.1 mmHg before surgery; postoperative measurements were 16.9±2.8 mmHg at week 1, and 14.7±2.6 mmHg, 13.8±2.8 mmHg, 13.4±2.4 mmHg, and 13.1±3.4 mmHg at months 1, 3, 6, and 12, respectively. Postoperative IOP significantly decreased during follow-up, with a significant difference in IOP rates before and after surgery (p<0.05)
Discussion
The main finding of our study is that a continuous increase in choroidal thickness was observed during the follow-up period of 12 months, in comparison with measurements before surgery, but without a statistically significant difference. In terms of macular thickness, CMT increased very slightly in the first three months in comparison with measurements before surgery, and showed a regression back to pre-surgery baseline values in month six. Cystoid macular edema (CME) was not observed in any cases during follow-up.
Falavarjani et al. have argued that cataract types and grades are important in measuring retinal thickness, and similarly, choroidal thickness measurement is also affected by the cataract [15]; however, they used time domain OCT, whereas we used SD-OCT. In addition, we excluded patients with dense cataracts in order to catch straight images, and we minimized the effect of the cataract on the macular and choroidal thickness measurements.
In our study, macular thickness was found to increase to some degree in the three months after surgery, confirming other published reports, but it had returned to preoperative values at the six-month follow-up. This change in macular thickness seems to be due to inflammation caused by surgery. Prostaglandins and cytokines released during surgery play an important role in the development of postoperative cystoid edema and contribute to the increase in macular thickness detected by OCT [16]. Lobo et al. found localized fluorescein leakage from the retina to the vitreous as a result of disruption to the blood-retina barrier, and this increased macular thickness [17]. In animal studies, both the inner and outer blood-retina barriers were shown to be disrupted with the surgery [10,11]. Clinical studies have shown that the frequency of macular edema increases with an increasing number of complications during surgery, such as iris trauma, posterior capsule rupture, loss of vitreous, or intra-ocular lens dislocation [18,19]. Nagy et al. reported lower increases in macular thickness in their series of femtosecond cataract surgery, which was attributed to reduced anterior segment manipulation and consequent reduction in release of prostaglandins [20].
A number of publications have examined changes in choroid thickness after cataract surgery, and generally in these studies SCT was evaluated, because the choroidal vascular structure was most dense at the fovea, which possesses high photoreceptor density and metabolic activity at the macula center [21]. Noda et al. found a statistically significant increase in subfoveal choroidal thickness in the first month after surgery and noted nearly the same values until the six-month follow-up [22]. In a study by Pierru et al., statistically significant increases in choroidal thickness occurred from the first day, which did not regress to preoperative values during follow-up for three months [23]. Ohsugi et al. noted statistically significant increases at subfoveal and inferior perifoveal points during choroid thickness measurements at different reference points in the macula, and non-significant increases at other points [24]. Falcao et al. noted insignificant increases in peripapillary and subfoveal choroidal thickness at follow-up one month after cataract surgery [25]. In our study, no patient developed AMD in the study eye or contralateral healthy eye during follow-up, but the increase in subfoveal choroidal thickness starting in week one continued to progress for the 12 months of follow-up in the eyes operated upon. In the present study, a significant decrease was found in IOP, especially after the third week following cataract surgery. A relatively negative correlation was found between IOP and choroidal thickness; as IOP was lower and ocular perfusion pressure was higher in the early postoperative period, the increase in choroidal thickness was relatively high.
The mean ultrasound phaco energy during surgery and phacoemulsification time may have an influence on macular and choroidal thickness after surgery. There were no complications in our surgeries, we used low-energy ultrasound, and our phacoemulsification time was very short. Thus, we do not consider there to have been an extra effect due to surgery. In our institution, anti-inflammatory eye drops are used as a routine procedure for suppression of inflammation after surgery. For this reason, the effect of cataract surgery on choroidal thickness cannot be evaluated exactly. The effect of phacoemulsification surgery on macular and choroidal thickness could be assessed in some patients without providing treatment with anti-inflammatory eye drops, but this would increase the risks for CME and endophthalmitis. In patients that develop CME in spite of anti-inflammatory therapy, examination of choroidal thickness may help to increase understanding of the effects of cataract surgery on the choroid. Pierru et al. found higher values of SCT in patients that developed CME after cataract surgery, in comparison with eyes of other patients who did not develop this complication [23]. Odrobina et al. examined choroidal thickness in patients that developed CmE after cataract, and found that such patients had a thinner subfoveal choroid. They reported a decrease in choroidal blood flow at the level of the choriocapillaris in eyes in which macular edema developed as the cause of this [26]. More studies are needed on this issue, as there are conflicting results between existing studies. Inflammation by itself cannot explain why the increase in choroidal thickness persists for so long. Another speculation is that more light enters the eye during and after cataract surgery, and therefore the retina and choroid are exposed to higher levels of light, and that this event induces angiogenesis by inducing metabolic activation. If choroidal thickness is assumed to reflect the vascularized state of the choroid, then the increase in thickness in the choroidea after cataract surgery may be associated with AMD progression. Increases in the incidence of late-onset AMD and especially neovascular AMD after cataract surgery were reported in the Beaver Dam and Blue Mountains studies [12,13]. Our results may shed light on the controversial issue of why the frequency of late-onset AMD increases after cataract surgery.
There are some limitations in the present study. The intraocular lenses used for the operations were all hydrophobic, aspheric, white in color, and filtered blue light. If different lenses are used, different results may occur. Eyes with axial lengths of between 21.50 and 24.00 at IOL measurement were included in this study; different results could be obtained if shorter or longer axial lengths are selected. A longer time period may be required for light to trigger intraocular reactions and cause certain changes, which is why studies with longer follow-up periods are needed. Various publications have reported decreases in SCT of between 1.4 μm and 1.6 μm every year in healthy individuals [4,27,28]. Therefore, during a follow-up period of one year, a decrease in choroidal thickness would be expected over time.
Conclusions
During the one-year follow-up in this study, the effect on macular thickness of cataract surgery without complications was observed to be at a subclinical level, and was also transient, declining to preoperative values by postoperative month six. SCT was seen to increase continually during the one-year follow-up after surgery, but the sample size would need to be enlarged to confirm our conclusion in further studies. The choroid may be involved in the pathogenesis of various ocular disorders. The vascular structure of the choroid is affected after cataract surgery, and this may be associated with initiation of late-onset AMD.
Footnotes
Conflict of interest
The authors declare that there are no conflicts of interest.
Source of support: Departmental sources
References
- 1.Cioffi GA, Granstam E, Alm A. Adler’s Physiology of the Eye: Clinical Application. 10th ed. Mosby; St Louis: 2003. Ocular circulation; pp. 747–84. [Google Scholar]
- 2.Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. 2010;29:144–68. doi: 10.1016/j.preteyeres.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500. doi: 10.1016/j.ajo.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 4.Nishida Y, Fujiwara T, Imamura Y, et al. Choroidal thickness and visual acuity in highly myopic eyes. Retina. 2012;32:1229–36. doi: 10.1097/IAE.0b013e318242b990. [DOI] [PubMed] [Google Scholar]
- 5.Unsal E, Eltutar K, Zirtiloglu S, et al. Choroidal thickness in patients with diabetic retinopathy. Clin Ophthalmol. 2014;8:637–42. doi: 10.2147/OPTH.S59395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhoot DS, Huo S, Yuan A, et al. Evaluation of choroidal thickness in retinitis pigmentosa using enhanced depth imaging optical coherence tomography. Br J Ophthalmol. 2013;97:66–69. doi: 10.1136/bjophthalmol-2012-301917. [DOI] [PubMed] [Google Scholar]
- 7.Hamzah F, Shinojima A, Mori R, Yuzawa M. Choroidal thickness measurement by enhanced depth imaging and swept-source optical coherence tomography in central serous chorioretinopathy. BMC Ophthalmol. 2014;14:145. doi: 10.1186/1471-2415-14-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung SE, Kang SW, Lee JH, Kim YT. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology. 2011;118:840–45. doi: 10.1016/j.ophtha.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Jagow B, Ohrloff C, Kohnen T. Macular thickness after uneventful cataract surgery determined by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2007;245:1765–71. doi: 10.1007/s00417-007-0605-6. [DOI] [PubMed] [Google Scholar]
- 10.Tso MO, Shih CY. Experimental macular edema after lens extraction. Invest Ophthalmol Vis Sci. 1977;16:381–92. [PubMed] [Google Scholar]
- 11.Liu H, Demetriades AM, Xiao WH, et al. Mouse model of post-surgical breakdown of the blood-retinal barrier. Curr Eye Res. 2004;28:421–26. doi: 10.1080/02713680490503769. [DOI] [PubMed] [Google Scholar]
- 12.Cugati S, Mitchell P, Rochtchina E, et al. Cataract surgery and the 10-year incidence of age-related maculopathy: the Blue Mountains Eye Study. Ophthalmology. 2006;113:2020–25. doi: 10.1016/j.ophtha.2006.05.047. [DOI] [PubMed] [Google Scholar]
- 13.Wang JJ, Klein R, Smith W, et al. Cataract surgery and the 5-year incidence of late-stage age-related maculopathy: Pooled findings from the Beaver Dam and Blue Mountains eye studies. Ophthalmology. 2003;110:1960–67. doi: 10.1016/s0161-6420(03)00816-9. [DOI] [PubMed] [Google Scholar]
- 14.Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:261–66. doi: 10.1167/iovs.11-8782. [DOI] [PubMed] [Google Scholar]
- 15.Falavarjani KG, Modarres M, Nikeghbali A. OCT and cataract. Ophthalmology. 2010;117:849. doi: 10.1016/j.ophtha.2009.12.020. author reply 849–50. [DOI] [PubMed] [Google Scholar]
- 16.Miyake K, Ibaraki N. Prostaglandins and cystoid macular edema. Surv Ophthalmol. 2002;47(Suppl 1):S203–18. doi: 10.1016/s0039-6257(02)00294-1. [DOI] [PubMed] [Google Scholar]
- 17.Lobo CL, Faria PM, Soares MA, et al. Macularalterations after small-incision cataract surgery. J Cataract Refract Surg. 2004;30:752–60. doi: 10.1016/S0886-3350(03)00582-0. [DOI] [PubMed] [Google Scholar]
- 18.Gulkilik G, Kocabora S, Taskapili M, Engin G. Cystoid macular edema after phacoemulsification: risk factors and effect on visual acuity. Can J Ophthalmol. 2006;41:699–703. doi: 10.3129/i06-062. [DOI] [PubMed] [Google Scholar]
- 19.Powe NR, Schein OD, Gieser SC, et al. Synthesis of the literature on visualacuity and complications following cataract extraction with intraocularlens implantation; The Cataract Patient Outcome Research Team. Arch Ophthalmol. 1994;112:239–52. doi: 10.1001/archopht.1994.01090140115033. [DOI] [PubMed] [Google Scholar]
- 20.Nagy ZZ, Ecsedy M, Kovacs I, et al. Macular morphology assessed by optical coherence tomography image segmentation after femtosecond laser-assisted and standard cataract surgery. J Cataract Refract Surg. 2012;38:941–46. doi: 10.1016/j.jcrs.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 21.Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;47:811–15. doi: 10.1016/j.ajo.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Noda Y, Ogawa A, Toyama T, Ueta T. Long-term increase in subfoveal choroidal thickness after surgery for senile cataracts. Am J Ophthalmol. 2014;158:455–59. doi: 10.1016/j.ajo.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Pierru A, Carles M, Gastaud P, Baillif S. Measurement of subfoveal choroidal thickness after cataract surgery in enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55:4967–74. doi: 10.1167/iovs.14-14172. [DOI] [PubMed] [Google Scholar]
- 24.Ohsugi H, Ikuno Y, Ohara Z, et al. Changes in choroidal thickness after cataract surgery. J Cataract Refract Surg. 2014;40:184–91. doi: 10.1016/j.jcrs.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 25.Falcao MS, Goncalves NM, Freitas-Costa P, et al. Choroidal and macular thickness changes induced by cataract surgery. Clin Ophthalmol. 2014;8:55–60. doi: 10.2147/OPTH.S53989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Odrobina D, Laudanska-Olszewska I. Choroidal thickness in clinically significant pseudophakic cystoid macular edema. Retina. 2015;35:136–40. doi: 10.1097/IAE.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 27.Ikuno Y, Kawaguchi K, Nouchi T, Yasuno Y. Choroidal thickness in healthy Japanese subjects. Invest Ophthalmol Vis Sci. 2010;51:2173–76. doi: 10.1167/iovs.09-4383. [DOI] [PubMed] [Google Scholar]
- 28.Ho M, Liu DT, Chan VC, Lam DS. Choroidal thickness measurement in myopic eyes by enhanced. depth optical coherence tomography. Ophthalmology. 2013;120:1909–14. doi: 10.1016/j.ophtha.2013.02.005. [DOI] [PubMed] [Google Scholar]


