Abstract
To determine if aircraft noise exposure causes an increased incidence of hypertension among residents near airports. We conducted a meta-analysis of observational studies to evaluate the association between aircraft noise exposure and the incidence of hypertension. PubMed, Embase, Web of Science, the Cochrane Library, and the Chinese Biomedical Literature Database were searched without any restrictions. Odds ratios (ORs) with 95% confidence intervals (CIs) were extracted. The pooled ORs were calculated using both the fixed effects model and random effects model. All analyses were performed using STATA version 12.0 software (Stata Corporation, College Station, TX, USA). We examined five studies, comprising a total of 16,784 residents. The overall OR for hypertension in residents with aircraft noise exposure was 1.63 (95% CI, 1.14-2.33), and one of our included studies showed that there was no evidence that aircraft noise is a risk factor for hypertension in women. According to our subgroup analysis, the summary OR for the incidence was 1.31 (95% CI, 0.85-2.02) with I2 of 80.7% in women and 1.36 (95% CI, 1.15-1.60) with moderate heterogeneity in men. The pooled OR for the incidence of hypertension in residents aged over 55 years and under 55 years was 1.66 (95% CI, 1.21-2.27) with no heterogeneity and 1.78 (95% CI, 1.33-2.39) with I2 of 29.4%, respectively. The present meta-analysis suggests that aircraft noise could contribute to the prevalence of hypertension, but the evidence for a relationship between aircraft noise exposure and hypertension is still inconclusive because of limitations in study populations, exposure characterization, and adjustment for important confounders.
Keywords: Aircraft noise exposure, hypertension, meta-analysis
Introduction
Aircraft noise is an important environment health issue associated with sleep disturbance, annoyance, hearing loss, and cardiovascular diseases.[1,2,3,4,5,6,7,8] Correia[5] found that the aircraft noise was statistically associated with a higher relative rate of hospitalization for cardiovascular diseases among older people residing near airports. Hypertension is a major risk factor for cardiovascular disease, and the first survey in which it was reported that the exposure to aircraft noise may cause hypertension in humans was published in the 1970s.
Noise is a ubiquitous part of human life and a major public health problem of modern times. Experimental studies have indicated that noise has the potential to trigger a physiological stress response by activating the sympathetic nervous system and causing arousal of the neuroendocrine system.[9] The release of stress hormones results in various acute hemodynamic and metabolic effects such as elevated blood pressure, aggregation of thrombocytes, and release of free fatty acids into the bloodstream.[10,11] Further, long-term noise exposure may lead to chronic dysregulation in the stress mechanism and increase the risk of hypertension.[12]
This suggestion has been explored in both epidemiologic and experimental studies. However, there are differences among the findings. Knipschild[13,14,15] and Rosenlund[6] reported the association between exposure to aircraft noise and hypertension, and implied that aircraft noise might be a risk factor for hypertension. In contrast, Goto's[16] study on the incidence of hypertension around airports reported no significant difference in areas with different levels of aircraft noise, while Eriksson[17] found significant differences between men and women in terms of the relationship between aircraft noise and the cumulative incidence of hypertension, noting an increased risk of hypertension in men but not in women. Therefore, we performed a meta-analysis on observational studies investigating the relationship between aircraft noise and hypertension.
Materials and Methods
Our meta-analysis was conducted following the checklist of items in the Meta-analysis Of Observational Studies in Epidemiology (MOOSE)[18] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements.[19] Methodological reviews were as follows.
Search strategy
A comprehensive literature search of the following databases was conducted: PubMed, Embase, the Cochrane Library, Web of Science, and the Chinese Biomedical Literature Database, all of which were searched without year or language restrictions. We used combinations of the following keywords and corresponding medical subject headings (MeSH) terms for the literature search: “aircraft noise,” “hypertension,” “high blood pressure,” etc. There were no restrictions on the language of publication during the document retrieval, and there was also no restriction placed on the geographical location of studies. The reference lists of the retrieved articles were also searched and relevant studies were checked manually to identify other literature related to our article topic.
Criteria for study selection
We first screened the identified abstracts or titles. For this meta-analysis, we included original studies that reported the causal link between aircraft noise exposure and hypertension, while studies on noise exposure from other sources (occupational, railway, industry, and road or neighborhood noise) were not included. The second screen was based on full-text review. Studies were considered eligible if they met the following criteria:
Cross-sectional, cohort, or case-control design;
The exposure of interest was aircraft noise;
-
The outcome of interest was hypertension, as defined by the following criteria:
- Diagnosis by a physician;
- Being under active treatment with a specific drug;
- Evidence from physical examination of the subjects and electrocardiographic, echocardiographic, or blood pressure laboratory measurements, or
- Through self-report;
Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were reported for the groups exposed versus the groups not exposed to aircraft noise. Ecological studies, editorials, case reports, and reviews were not considered eligible.
Data extraction and quality assessment
Two independent reviewers (Huang and Song) screened the resulting titles, abstracts, and even full texts to identify studies that met our inclusion criteria. Any disagreement was resolved by a third reviewer (Yang). The following variables were extracted from all studies: data about study characteristics (authors, year of publication, study design, and country), study population (number of cases, sex, and age), exposure level, and adjusted factors. Extracted data were entered into Microsoft Office Excel 2007 SP3 (Microsoft Corporation, WA, USA) and were checked by the third reviewer (Yang). The study quality was assessed by publication type (3 = peer-reviewed article, 0 = not peer reviewed), study design (1 = cross-sectional, 2 = case-control, 3 = cohort), validity of outcome assessment (0 = self-report, 3 = diagnosis by a physician or physical examination), control of confounding variables (0 = no control, 1 = age and sex only, 2 = age and sex with one or more major hypertension risk factors, 3 = age, sex, one or more major hypertension risk factors, as well as other factors), and response rate (0 = <80%, 3 = ≥80%). The total score was assessed as follows: very good = 10 points and above, good = 6-9 points, and fair = 5 points or below.[20]
Statistical analysis
The pooled estimates for dichotomous variables are reported as ORs with 95% CI. If ORs with 95% CI were not available, we calculated these from the raw data. Heterogeneity of effect sizes was assessed by Cochran's Q statistic (significance level set at P < 0.10) and the I2 statistic, which is a quantitative measure of consistency across studies.[21] If heterogeneity was present (i.e., Q test result significant or I2 ≥ 50%), a random effects method was used to estimate a pooled effect size; otherwise, the fixed effects model with inverse variance method was applied. Subgroup analysis was performed according to gender, age, and adjusted factors. All analyses were performed using STATA version 12.0. Also, P < 0.05 (two-tailed) was considered statistically significant except for the heterogeneity test, for which P < 0.10 (one-tailed) was used.
Results
Figure 1 summarizes the literature search process used in the present meta-analysis, which included five studies with data collected from a total of 16,784 subjects. Of these, four studies were cross-sectional[6,13,16,22] and one was a cohort study.[17] Two[6,17] studies were conducted in Europe, two[13,22] in Oceania, and one[16] in Asia. One study[13] was published before 2000 and the other four[6,16,17,22] after 2000. Characteristics of these included studies are summarized in Table 1. The evaluation of a risk bias in the included studies is shown in Table 2.
Figure 1.
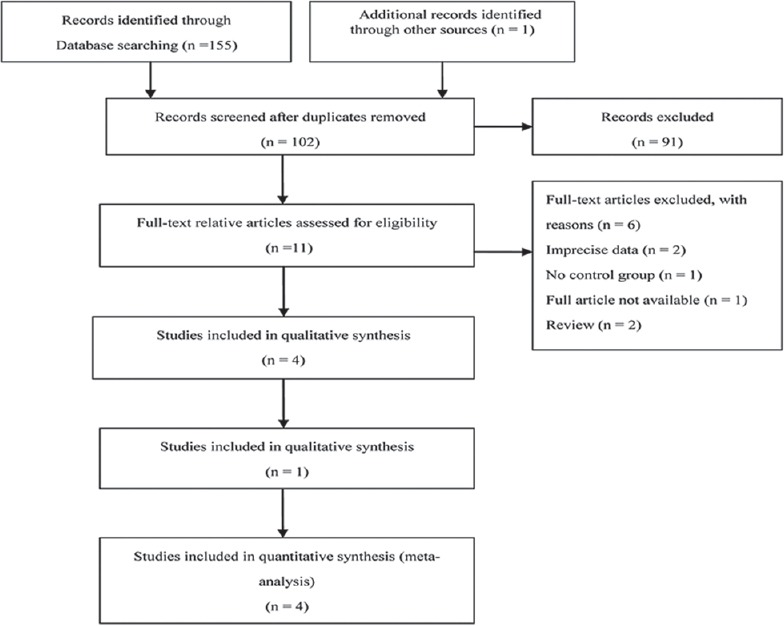
PRISMA diagram showing selection of articles for review
Table 1.
Characteristics of the included studies
| First author | Year | Country | Study design | Population age (years) | Number of cases of hypertension | Exposure levels (dBA) | Adjustments | OR |
|---|---|---|---|---|---|---|---|---|
| Rosenlund et al.[6] | 2001 | Sweden | cross-sectional | 19-80 | 2959 | <55; ≥55 | Age, sex, smoking, education, physical activity, fruit consumption and house type | Multivariable adjusted |
| Knipschild[13] | 1977 | Netherlands | cross-sectional | 35-64 | 5828 | 20-40; 40-60 | Not reported | Unadjusted |
| GOTO[16] | 2002 | Japan | cross-sectional | NA | 1646 | Unexposed; ≥75; | Anti-hypertension treatment, diet, alcohol consumption and smoking | Multivariable adjusted |
| Eriksson et al.[17] | 2010 | Sweden | cohort | 35-56 | 4721 | <50; ≥50 | Age, socioeconomic status, smoking and body mass index, sex (total population only) | Multivariable adjusted |
| Black[22] | 2007 | Sydney | cross-sectional | 15-87 | 1500 | unexposed; ≥70; | Noise sensitivity, annoyance of traffic and aircraft noise, interaction between aircraft and traffic noise annoyance | Multivariable adjusted |
Table 2.
Assessment of the methodological quality of studies included in the meta-analysis on aircraft noise exposure and hypertension
Figure 2 presents our combined meta-analysis of four studies.[6,13,17,22] The OR of hypertension in residents with aircraft noise exposure was 1.63 (95% CI, 1.14-2.33), with the aggregate results showing that significant heterogeneity existed in the included studies (I2 = 81.2%, P = 0.001). To assess the influence of the individual studies on the overall outcome, they were removed one by one and the substantial heterogeneity in the aircraft noise and hypertension association was attributed to one study,[17] as omitting this study resulted in a homogenous outcome whereby the pooled OR was 1.84 (95% CI, 1.51-2.24) with low heterogeneity (I2 = 13.5%, P = 0.315).
Figure 2.
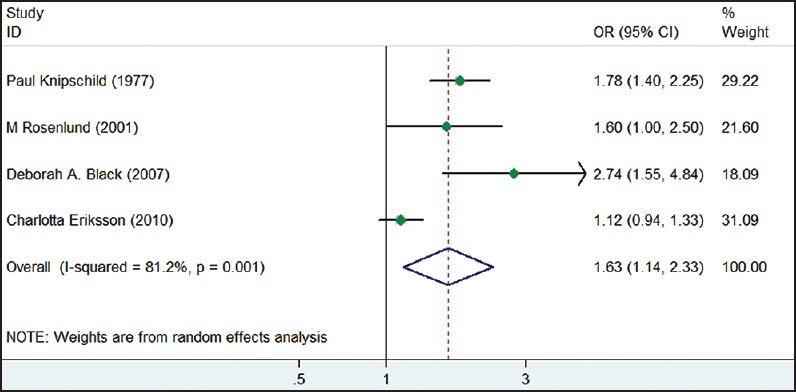
Forest plot of meta-analysis of hypertension in residents with aircraft noise exposure. Individual studies represented by OR and 95% CI
Only one study[16] reported the results with mean ± standard deviation (SD). The authors compared the blood pressure data of women (N = 469) living around an airport with women living in areas with no aircraft noise (N = 1177), controlling of variables such as antihypertension treatment, diet, alcohol consumption, and smoking. The study found no evidence of aircraft noise as a risk factor for hypertension in women.
Subgroup analysis
Subgroup analysis of gender
A subgroup analysis was performed according to gender. The pooled OR for the incidence of hypertension in men was 1.36 (95% CI, 1.15-1.60) with moderate heterogeneity (P = 0.175, I2 = 42.7%) [Figure 3]. The studies that reported women's OR for the incidence of hypertension had an overall OR of 1.31 (95% CI, 0.85-2.02), and substantial heterogeneity was observed (P = 0.006, I2 = 80.7%) [Figure 4]. The analysis of sensitivity was done through exclusion, one by one, of the individual studies and the substantial heterogeneity in the aircraft noise and hypertension association was attributed to one study;[17] the aggregated OR was 1.81 (95% CI, 1.28-2.54) with I2 of 0%.
Figure 3.
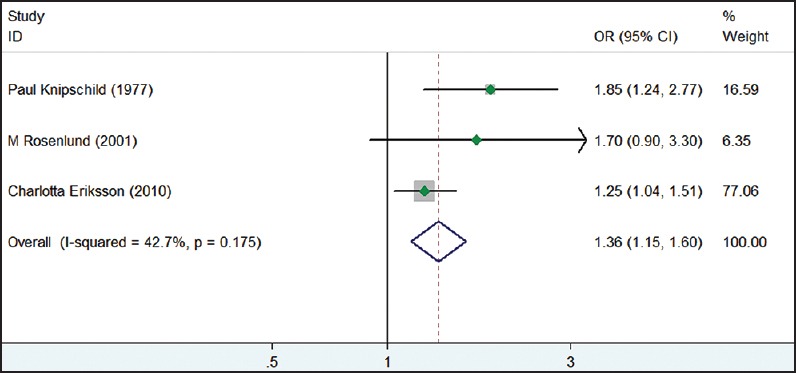
Forest plot of meta-analysis of hypertension in men with aircraft noise exposure. Individual studies represented by OR and 95% CI
Figure 4.
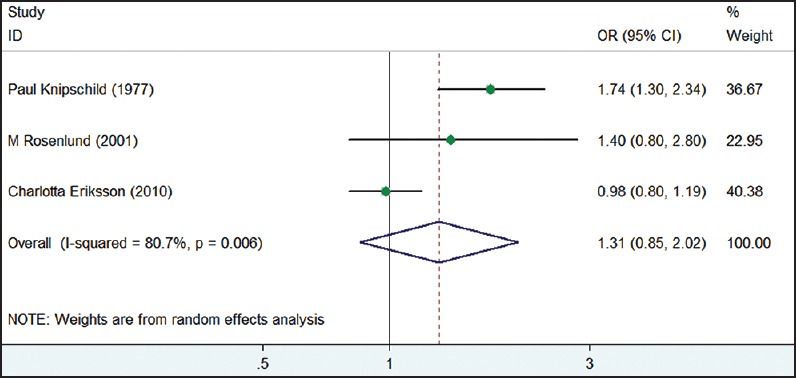
Forest plot of meta-analysis of hypertension in women with aircraft noise exposure. Individual studies represented by OR and 95% CI
Subgroup analysis of age
This subgroup analysis explored the impact of age with subjects grouped into those aged over and under 55 years. The pooled OR for the incidence of hypertension in residents aged over 55 years and those aged under 55 years were 1.66 (95% CI, 1.21-2.27) with I2 of 0%, and 1.78 (95% CI, 1.33-2.39) with I2 of 29.4%, respectively, [Table 3].
Table 3.
Subgroup analysis
| Group | Hypertension | |||
|---|---|---|---|---|
| No. of studies | OR (95%CI) | Pheterogeneity | I2(%) | |
| Total | 4 | 1.63 (1.14, 2.33) | 0.001 | 81.2 |
| Sex | ||||
| Men | 3 | 1.36 (1.15, 1.60) | 0.175 | 42.7 |
| Women | 3 | 1.31 (0.85, 2.02) | 0.006 | 80.7 |
| Age | ||||
| <55 years | 2 | 1.78 (1.33, 2.39) | 0.234 | 29.4 |
| ≥55 years | 2 | 1.66 (1.21, 2.27) | 0.64 | 0 |
| Adjustment for ORs | ||||
| Unadjusted | 3 | 1.56 (1.35, 1.79) | 0.386 | 0 |
| Adjusted | 3 | 1.56 (0.88, 2.78) | 0.001 | 85.6 |
Subgroup analysis of unadjusted and multivariable adjusted OR
A subgroup analysis was conducted for unadjusted and multivariable adjusted ORs. Three studies[6,13,17] that reported unadjusted ORs for the incidence of hypertension had an overall OR of 1.56 (95% CI, 1.35-1.79) with no evidence of heterogeneity (P = 0.386, I2 = 0%). The pooled OR for the incidence of hypertension in studies[6,17,22] with multivariable adjusted factors was 1.56 (95% CI, 0.88-2.78) with substantial heterogeneity (P = 0.001, I2 = 85.6%). The high heterogeneity could be explained by the inconsistent adjustment factors [Table 3].
Discussion
This meta-analysis showed that there is a relationship between aircraft noise exposure and the prevalence of hypertension, and the results are consistent with a previous meta-analysis that found an increased risk of hypertension among populations with aircraft noise exposure.[23] One of our included studies[16] concluded that there was no obvious difference in blood pressure caused by aircraft noise in women in Fukuoka, Japan. Our gender-specific subgroup analysis also suggested that there is a relationship between aircraft noise exposure and the incidence of hypertension in men, but the relationship was not significant in women. A recent cohort study[17] reported an increased risk of hypertension in men but not in women, following long-term exposure to aircraft noise. This difference may be explained by the differing epidemiology and progression of cardiovascular diseases in men and women, and there is evidence of gender differences in the pathogenesis of cardiovascular diseases.[24,25,26] The risk of hypertension in residents was significantly associated with exposed aircraft noise according to age, with subjects aged under 55 years showing a slighter higher association than those over 55 years. One study[6] reported that hearing loss might protect against aircraft noise and that people who have an auditory deficiency are less sensitive to noise, which could partly explain the diverging results presented in this study. The overall unadjusted OR showed an increased risk of hypertension among people with aircraft noise exposure. The pooled OR in studies with multivariable adjusted factors showed a slightly weaker relationship between hypertension and aircraft noise exposure, with the high heterogeneity mainly attributed to the differing adjustment factors. In fact, it is hard to detect the health impact of noise from a single source, such as aircraft, because there are many noise sources presented in our daily life such as life events, shift work, and hypertension in parent(s), which may also be potential factors substantially influencing the noise effect. Therefore, we should be cautious in determining the adjustment factors in future studies.
The strength of this study is mainly related to the large number of subjects. In addition, many previous meta-analyses were focused on investigating the relationship between community noise and cardiovascular disease, while our paper aimed to study the association between aircraft noise and hypertension.
However, the limitations in the present meta-analysis should be acknowledged. Some factors added to the difficulty in interpreting the results of this review and high heterogeneity existed in several pooled results. First, the studies included in our meta-analysis used different study populations and different sampling methods to define airport noise levels. For instance, several studies had no clear-cut noise range, e.g., people exposed to <55 dB (A), for noise exposed groups or unexposed groups. Second, most data were abstracted without adjusting for confounding effects and inconsistent adjustment confounders; thus, the pooled results might be prone to bias.
Conclusion
This meta-analysis suggests that aircraft noise exposure may be associated with an increased risk of hypertension. However, the relationship was significant in men but not in women, and there was no significant difference in ages.
Acknowledgments
The authors wish to thank Pin Yang and Chunhu Shi for their helpful comments.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Basner M, Griefahn B, Berg Mv. Aircraft noise effects on sleep: Mechanisms, mitigation and research needs. Noise Health. 2010;12:95–109. doi: 10.4103/1463-1741.63210. [DOI] [PubMed] [Google Scholar]
- 2.Morrell S, Taylor R, Lyle D. A review of health effects of aircraft noise. Aust N Z J Public Health. 1997;21:221–36. doi: 10.1111/j.1467-842x.1997.tb01690.x. [DOI] [PubMed] [Google Scholar]
- 3.Passchier-Vermeer W, Passchier WF. Noise exposure and public health. Environ Health Perspect. 2000;108(Suppl 1):123–31. doi: 10.1289/ehp.00108s1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Passchier W, Knottnerus A, Albering H, Walda I. Publlic health impact of large airports. Rev Environ Health. 2000;15:83–96. doi: 10.1515/reveh.2000.15.1-2.83. [DOI] [PubMed] [Google Scholar]
- 5.Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: Multi-airport retrospective study. BMJ. 2013;347:f5561. doi: 10.1136/bmj.f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenlund M, Berglind N, Pershagen G, Järup L, Bluhm G. Increased prevalence of hypertension in a population exposed to aircraft noise. Occup Environ Med. 2001;58:769–73. doi: 10.1136/oem.58.12.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stansfeld S, Haines M, Brown B. Noise and health in the urban environment. Rev Environ Health. 2000;15:43–82. doi: 10.1515/reveh.2000.15.1-2.43. [DOI] [PubMed] [Google Scholar]
- 8.Franssen EA, van Wiechen CM, Nagelkerke NJ, Lebret E. Aircraft noise around a large international airport and its impact on general health and medication use. Occup Environ Med. 2004;61:405–13. doi: 10.1136/oem.2002.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ising H, Braun C. Acute and chronic endocrine effects of noise: Review of the research conducted at the Institute for Water, Soil and Air Hygiene. Noise Health. 2000;2:7–24. [PubMed] [Google Scholar]
- 10.Spreng M. Possible health effects of noise induced cortisol increase. Noise Health. 2000;2:59–64. [PubMed] [Google Scholar]
- 11.Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise Health. 2003;5:1–11. [PubMed] [Google Scholar]
- 12.Babisch W, Kamp Iv. Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health. 2009;11:161–8. doi: 10.4103/1463-1741.53363. [DOI] [PubMed] [Google Scholar]
- 13.Knipschild P. V. Medical effects of aircraft noise: Community cardiovascular survey. Int Arch Occup Environ Health. 1977;40:185–90. doi: 10.1007/BF01842081. [DOI] [PubMed] [Google Scholar]
- 14.Knipschild P, Oudshoorn N. VII. Medical effects of aircraft noise: Drug survey. Int Arch Occup Environ Health. 1977;40:197–200. doi: 10.1007/BF01842083. [DOI] [PubMed] [Google Scholar]
- 15.Knipschild P. VI. Medical effects of aircraft noise: General practice survey. Int Arch Occup Environ Health. 1977;40:191–6. doi: 10.1007/BF01842082. [DOI] [PubMed] [Google Scholar]
- 16.Goto K, Kaneko T. Distribution of blood pressure data from people living near an airport. J Sound Vib. 2002;250:145–9. [Google Scholar]
- 17.Eriksson C, Bluhm G, Hilding A, Ostenson CG, Pershagen G. Aircraft noise and incidence of hypertension — gender specific effects. Environ Res. 2010;110:764–72. doi: 10.1016/j.envres.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observation studies in epidemiology: A proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 20.Ndrepepa A, Twardella D. Relationship between noise annoyance from road traffic noise and cardiovascular diseases: A meta-analysis. Noise Health. 2011;13:251–9. doi: 10.4103/1463-1741.80163. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Black DA, Black JA, Issarayangyun T, Samuels SE. Aircraft noise exposure and resident's stress and hypertension: A public health perspective for airport environmental management. J Air Transp Manag. 2007;13:264–76. [Google Scholar]
- 23.van Kempen EE, Kruize H, Boshuizen HC, Ameling CB, Staatsen BA, de Hollander AE. The association between noise exposure and blood pressure and ischemic heart disease: A meta-analysis. Environ Health Perspect. 2002;110:307–17. doi: 10.1289/ehp.02110307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oparil S, Miller AP. Gender and blood pressure. J Clin Hypertens (Greenwich) 2005;7:300–9. doi: 10.1111/j.1524-6175.2005.04087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer MR, Haas E, Barton M. Gender differences of cardiovascular disease new perspectives for estrogen receptor signaling. Hypertension. 2006;47:1019–26. doi: 10.1161/01.HYP.0000223064.62762.0b. [DOI] [PubMed] [Google Scholar]
- 26.Vitale C, Miceli M, Rosano GM. Gender-specific characteristics of atherosclerosis in menopausal women: Risk factors, clinical course and strategies for prevention. Climacteric. 2007;10(Suppl 2):16–20. doi: 10.1080/13697130701602712. [DOI] [PubMed] [Google Scholar]


