Abstract
Hospitals have complex soundscapes that create challenges to patient care. Extraneous noise and high reverberation rates impair speech intelligibility, which leads to raised voices. In an unintended spiral, the increasing noise may result in diminished speech privacy, as people speak loudly to be heard over the din. The products available to improve hospital soundscapes include construction materials that absorb sound (acoustic ceiling tiles, carpet, wall insulation) and reduce reverberation rates. Enhanced privacy curtains are now available and offer potential for a relatively simple way to improve speech privacy and speech intelligibility by absorbing sound at the hospital patient's bedside. Acoustic assessments were performed over 2 days on two nursing units with a similar design in the same hospital. One unit was built with the 1970s’ standard hospital construction and the other was newly refurbished (2013) with sound-absorbing features. In addition, we determined the effect of an enhanced privacy curtain versus standard privacy curtains using acoustic measures of speech privacy and speech intelligibility indexes. Privacy curtains provided auditory protection for the patients. In general, that protection was increased by the use of enhanced privacy curtains. On an average, the enhanced curtain improved sound absorption from 20% to 30%; however, there was considerable variability, depending on the configuration of the rooms tested. Enhanced privacy curtains provide measureable improvement to the acoustics of patient rooms but cannot overcome larger acoustic design issues. To shorten reverberation time, additional absorption, and compact and more fragmented nursing unit floor plate shapes should be considered.
Keywords: Acoustics, hospital design, noise, speech intelligibility
Introduction
The acoustic environment of a health care facility can substantially impact the quality of care a patient receives and the potential benefit a patient derives from that care.[1,2,3,4,5,6] Despite this well-established relationship, there are no existing methods that allow specific predictions to be made about the impact of specific acoustic metrics on patient care or health care outcomes.
Most hospital-based research related to noise focuses on overall decibel levels, which, while important, miss several crucial parameters that can be used to characterize noise. The chief among these are sound pressure (decibel) level fluctuations over time, frequency spectrum, speech intelligibility, speech privacy, and reverberation times.
Acoustic perception
Okcu et al. demonstrated that decibel levels alone are inadequate for describing the lived experience of the acoustic environment.[7] By comparing two intensive care units, the research showed that the proportion of time that the sound levels were at maximum and peak levels correlated positively with nurses’ annoyance with the noise. Hagerman, et al. found that patients considered the staff attitude to be better after additional sound absorption was installed in the space, providing evidence that acoustics plays a significant role in influencing our perception and influences everyone in the space — Patients and staff.[3]
In 2007, the Center for Health Design and the Robert Wood Johnson Foundation published a white paper that reviewed “how different aspects of sound — Noise, speech privacy, speech intelligibility, and music — Impact patient and staff outcomes in healthcare settings and the specific environmental design strategies that can be used to improve the acoustical environment of healthcare settings” p.2.[4] The authors concluded that the most important negative impacts of hospital noise on patients were physiological effects, reduced patient confidentiality, and impaired speech intelligibility and communication.
Prior findings in the same setting
Noise has been acknowledged as an issue at this medical center, and a variety of steps have been taken to increase awareness and reduce the impact of noises that were identified as problematic by the staff. Studies were conducted that were designed to measure decibel levels, describe what generated the noise, and in some cases included simple interventions to reduce the levels.[8,9,10] One study demonstrated the value of closing a patient's room door in reducing the noise level to more acceptable levels. That same study illustrated that turning the alarm volume up to high did not increase audibility for the staff outside the room, providing evidence that localized alarms within patient rooms should be adjusted for patient exposure and not to notify the staff.[8] Another study conducted in a chemotherapy unit, revealed that a squeaky chair and the main entrance door to the chemo unit generated the most noise and both could be repaired to remediate the noise.[10]
Research focused on speech intelligibility in hospitals indicates it may be a significant and potentially hazardous problem.[11,12] A recent acoustical assessment of multiple patient care areas concluded that not one of the areas had acoustic attributes that indicated optimum conditions for speech intelligibility.[11] At this medical center, a study was designed to measure the impact of noise typical of the nursing units on inpatients’ ability to hear, understand, and recall what was said to them.[12] The study demonstrated that the study participants averaged 10 years younger than the typical inpatient population had significant difficulty in identifying and recalling key words in the speech-in-noise test masked by hospital noise recorded in our nursing units. The background noise levels had an even greater impact on recall than key word identification, a finding that may have clinical significance — Patient education is not of much use if patients comprehend the information during the consultation but cannot remember the information later. The study also demonstrated that identifying key words was more difficult when hospital noise included extraneous voices.
Perhaps more importantly, the study illustrated that lower decibel levels resulted in improved performance, as did testing in “plain” hospital noise versus hospital noise with voices. Pope's 2010 study of noise levels on four nursing units reported that at least one person's voice could be heard speaking during every 5-min interval of sound measurement (68/68 measures made over 12 h on each unit — A total of 48 h) and that more than one voice could be heard 91% of the time.[9] Therefore, the determination that extraneous voices made it even more difficult to identify and recall words in noise was deemed particularly important in our hospital environment.
Speech privacy and speech intelligibility
Speech privacy measures are generally focused on sound transmission between spaces, across curtains, for example. Measurements deemed with “no privacy” generally means that over 90% of the sentences can be understood and conversations are easily overheard between these locations. “Marginal” speech privacy means that 40-80% of the sentences can be understood and conversations can be overheard by someone trying to listen in. “Normal” speech privacy means that 10-30% of the sentences can be understood and conversations can be overheard by careful listeners. “Confidential” speech privacy means that less than 10% of the sentences can be understood and conversations are not understood but a listener will be able hear the speaker's voice.[13,14] These categories can be seen, with the corresponding Speech Intelligibility Index (SII) and Articulation Index (AI) cut-off points in Table 1.
Table 1.
Categories of speech privacy and speech intelligibility determined by Speech Intelligibility Index (SII) and Articulation Index (AI)
| Speech privacy “Confidential” | Speech privacy “Normal” to “marginal” | Speech privacy “No privacy” |
|---|---|---|
| SII <0.10 | 0.10 <SII <0.45 | 0.45 <SII |
| AI <0.05 | 0.05 <AI <0.35 | 0.35 <AI |
| Speech intelligibility “Poor” | Speech intelligibility “Fair/Normal” | Speech intelligibility “Excellent” |
Speech intelligibility measures are generally focused on sound transmission within a space, as within a curtained area. These measures often improve from interventions designed to improve speech privacy. This occurs when more sound is absorbed, reducing the overall sound level and reducing reverberation rates resulting in improved clarity of words and ability to locate the speaker.
Sound absorption
Increasing sound absorption reduces the reflected sound energy and makes the space quieter and feels more intimate. The reduced reverberation improves the localization of sounds and speech to aid nurses and patients in better identifying the direction of sound sources.
Opportunity to evaluate a product designed to improve speech privacy
The medical center had the opportunity to evaluate the effectiveness of an enhanced acoustic privacy curtain within the standard and a newly refurbished care area. The Hush Curtain® was designed to absorb sound for improved speech privacy. The vendor, Chinook Acoustics, was interested in obtaining “real life” data and willing to pay for the services of an acoustical engineer. The focus of the investigation was to understand:
Whether the SII and sound transmission differed significantly between usual fabric privacy curtains and the enhanced acoustic privacy curtains; and
To determine whether the effect was significant in a nursing unit that already had improved average sound absorption, i.e., was there still an additional acoustic benefit in using the enhanced privacy curtains?
Methods
The study protocol was submitted to the medical center's research and development committee and it was approved as nonhuman subjects’ research. In addition, the medical center's Deputy Director for Patient Care Services gave her approval to conduct the study in a patient care area.
Setting
The standard nursing unit was designed with one nurse station at the center of the unit. The walls were painted gypsum board for the patient rooms and corridors; the walls did not extend to the structure above the acoustical ceiling tile. The ceilings were of mineral fiber ceiling tiles. The floors were of tile. The standard privacy curtains were semi-translucent fabric.
The newly refurbished nursing unit was opened in 2013. The staff and design team integrated more sound absorptive ceiling tiles, improved the wall assemblies, designated a “quiet room” for private conversations, and split the central nurses’ station into two small stations reducing the number of staff congregating throughout the day. One station was located at the unit entrance, designed to greet and direct visitors when they first arrived on the unit with the intention of reducing traffic flow in the areas where patient care took place. The second station was designed to accommodate the staff focused on the work of the unit, providing spaces for providers to sit at work stations to review and enter medical records. The empirical response from the staff was that the new nursing unit was quieter and more comfortable but no acoustical measurements were completed to document and define these perceived improvements.
Nurse managers and staff from both nursing units discussed the logistics of the study with the principal investigator and acoustical engineer. The engineer described what equipment he would be using and what kind of noise he would have to generate to perform the testing. It was decided that the vendor would participate on the initial day of testing to ensure that housekeeping staff were given appropriate instructions on how to correctly hang the enhanced acoustic privacy curtains. The testing dates were scheduled based on availability of the engineer in combination with housekeepers’ schedules to ensure that the greatest number is available on the day of training.
Room selection
The criteria for room selection were based on representativeness of typical patient rooms and the existence a “mirror” room in case some rooms were not available on the testing day due to patient factors beyond our control. Three rooms on the refurbished unit and five on the standard nursing unit were selected. The measures of sound transmission and reverberation time were planned for three conditions:
With the standard privacy curtain pushed against the walls,
With the standard privacy curtains deployed, and
And with the Hush Curtains® (enhanced acoustical privacy curtain) deployed.
The 1/3-octave band sound levels were measured with a Larson Davis 2900 Type 1 real time spectrum analyzer (Larson Davis - a PCB Piezotronics division 3425 Walden Avenue Depew, NY 14043-2495 USA) that recorded the statistical value of sound with respect to amplitude (measured in decibels) and frequency but did not record it in audio for later listening. A 150-W Behringer Eurolive ultra-compact speaker on a 1.2 meters tripod was placed near the head of the bed for each tested room. The speaker played pink noise between 125 Hz and 16,000 Hz, which covers the frequency range associated with human speech from 160 Hz to 8,000 Hz, and at a decibel level that did not disturb normal operations and was usually 10 dB louder than the background decibel level at the nurses’ station. This ensured that the measurements provided an adequate signal-to-noise ratio to accurately document the sound transmitted from the speaker source in the patient room compared to other incidental activities or conversations in the units. The source and signal measurements with the pink noise were measured for 30 s, and were repeated if background noise sources were audible during the testing. Background sound levels were measured for 2-3 min at the receiver locations. The testing was completed over 2 consecutive days, beginning in the refurbished unit where fewer rooms were being tested and finishing on the standard unit. The reverberation time (RT60) was measured within each patient room with the standard curtain and with the enhanced acoustical privacy curtain.
On the days of testing, when a patient or patients occupied a room where testing was performed, the patients were given ear muff hearing protection during the testing to ensure that they were not at risk and to minimize the disruption by the sounds generated in the course of testing. Unit staff and other patients were also made aware of the testing.
Measurements
The measured sound transmission and reverberation time were completed in eight rooms. Five rooms on the standard unit and three on the refurbished unit were evaluated.
Sound absorption
The average sound absorption coefficient for speech frequencies was calculated based on the measured RT60 for each room, which is dependent on the room volume and total room surface area. The measured results were compared to the 2010 Facility Guidelines Institute Guidelines for Design and Construction of Health Care Facilities standard of 0.15 for private patient room and multibed patient rooms.[15] The results represent the average absorption coefficient between 250 Hz, 500 Hz, 1 kHz, and 2 kHz for each room with a standard curtain in a closed position (visually obscuring patient from door) and Hush Curtain® for the rooms with these installed. The number of standard privacy curtains was the number found hanging on the day of testing and was assumed to be the normal number for a particular room. The number of Hush Curtains® hung on the days of testing was determined by the vendor to be optimum. The average sound absorption coefficient and number of each type of curtain hanging during the assessment can be found in Table 2.
Table 2.
Average* sound absorption coefficient (ᾱ) for patient rooms in standard and refurbished nursing units with standard and Hush Curtains® in place
| Rooms | Standard curtain | Hush Curtain® | |
|---|---|---|---|
| Standard unit | |||
| Room A — four-bed | 0.24 (eight curtains) | 0.30 (12 curtains) | |
| Room B — one-bed | 0.23 (one curtain) | 0.28 (two curtains) | |
| Room C — one-bed | 0.24 (one curtain) | Not tested | |
| Room D — two-bed | 0.27 (four curtains) | 0.34 (five curtains) | |
| Room E — four-bed | 0.31 (eight curtains) | Not tested | |
| Refurbished unit | |||
| Room F — two-bed | 0.24 (four curtains) | Not tested | |
| Room G — two-bed | 0.17 ( four curtains) | 0.28 (eight curtains) | |
| Room H — one-bed | 0.23 (one curtain) | 0.28 (two curtains) | |
*FGI Design value of 0.15 is considered to be an average, acceptable sound absorption for patient rooms[13], A larger number indicates that the room more efficiently absorbs reflected sound and will generally be perceived as being quieter
Speech privacy
Speech privacy, defined by the SII and AI, was calculated from the sound transmission measurements using “normal speech levels” completed per ASTM E1130 Standard Test Method for Objective Measurement of Speech Privacy in Open Offices Using Articulation Index[13] and ANSI S3.5-1997 Methods for Calculation of the Speech Intelligibility Index[14] (1/3-octave band procedure). For each room the sound source speaker was placed on a tripod with the center of the speaker at 1.2 meters to 1.3 meters above the floor (depending on the bed height) to capture the sound path from the bedridden patient hearing and speech location. The sound transmission was measured at a variety of locations: Inside patient rooms, at the patient room doorway, in the hallway, and at the nurse stations. Measures were made at a height of 1.37 meters above the floor; the sound source speaker played amplified pink noise at 85-87 dB(A) when measured from 1 meter between 125 Hz and16000 Hz. The measured source level at the nurse station condition was 10 dB above the background sound level for rooms within 10.5 meters of the nurse station but was less than 10 dB above the background level for rooms further from the nurse station. Higher source levels were not an option because the adjacent patient rooms and corridors were occupied during testing. Therefore, the impact of the background sound on the predicted levels was considered to be part of the standard deviation for the data.
The speech privacy level was calculated from the position of the patient to the nearest nurse station or alcove, and from the nearest nurse station with the patient room door open––The norm on each nursing unit. These two measures were Expected to differ because the background noise level was generally higher at the nurse workstation and quieter in the patient room with the door open.
Results
Two rooms that were planned to be tested in the standard configuration were not tested because the rooms were occupied by patients with isolation precautions and could not be disturbed during the testing period. These rooms were mirrors of adjacent rooms that were tested in the standard configuration and with the Hush Curtain®. The speech privacy metrics are noted in the following tables, and the potential improvements in speech privacy extrapolated from them.
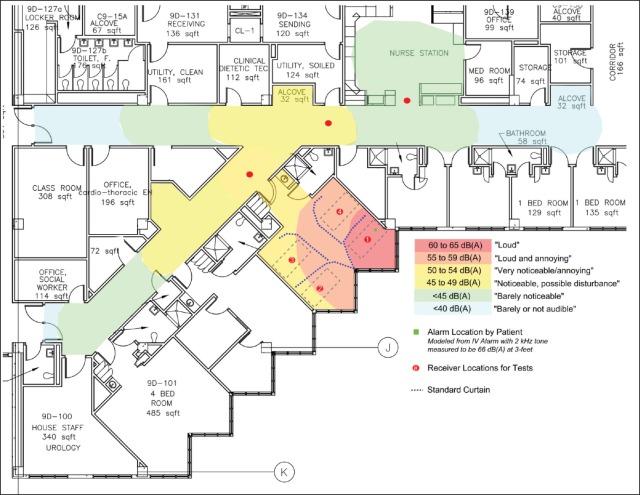
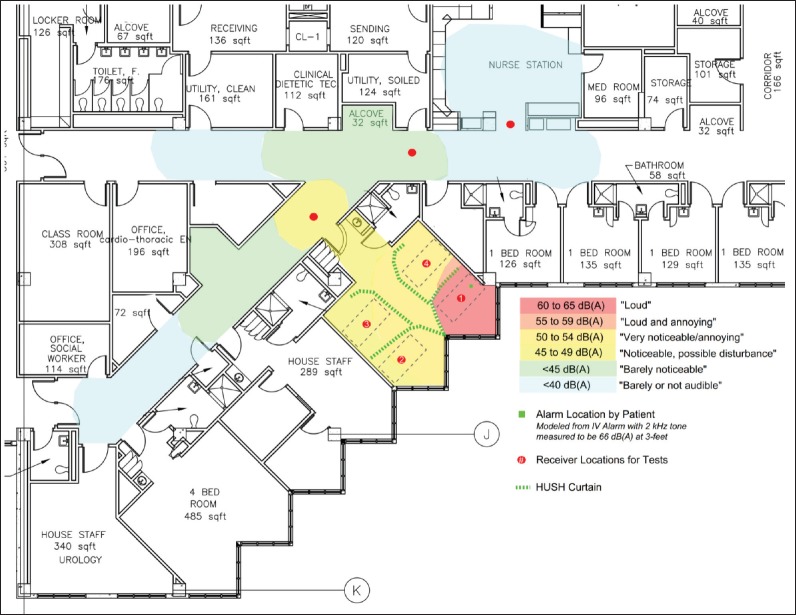
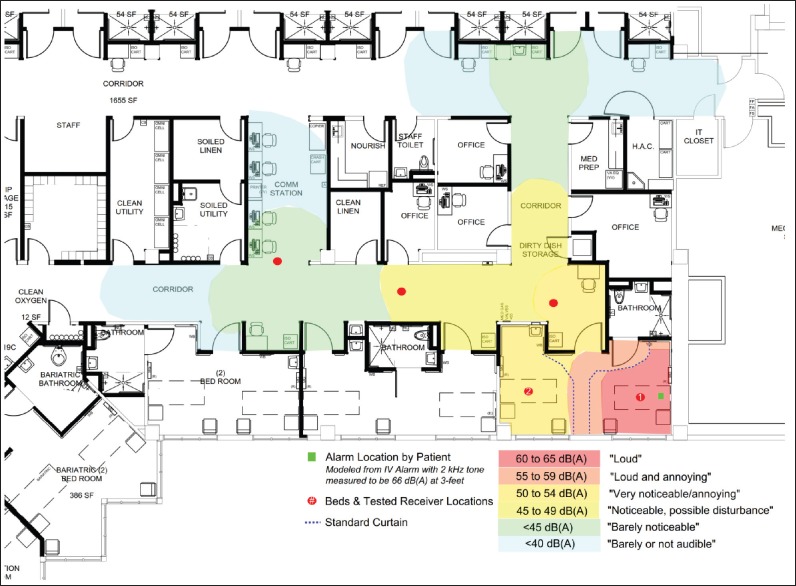
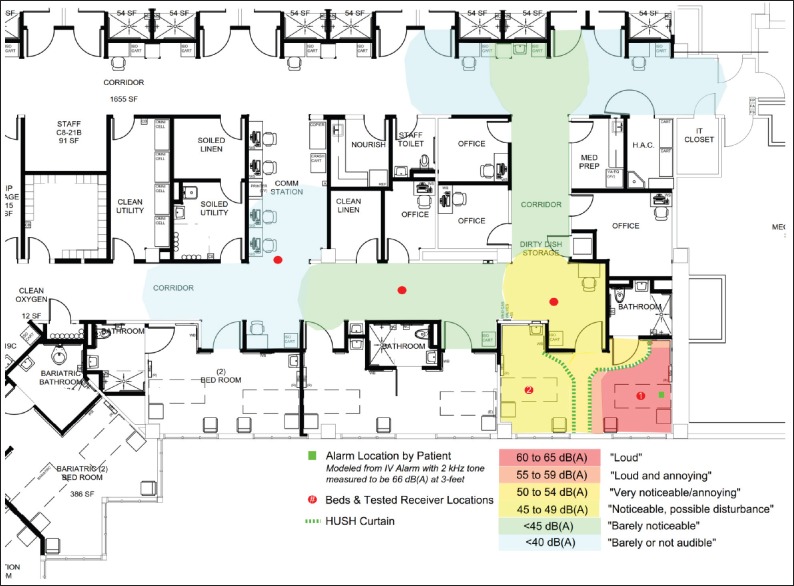
The figures denote the estimated levels of perception of a bedside medical alarm that is 65 dB(A) at 1 meter with a dominant tone at 2 kHz. The predicted levels are based on the measured sound reduction due to architectural design, material finishes, and the acoustic effect of the standard privacy curtain compared to the enhanced acoustical curtain.
Rooms: Standard nursing unit
In room A, a four-bed room, speech privacy measures improved 7-14% between the patient beds when comparing no curtain to the standard curtain, and 18-40% between the standard curtain and Hush Curtain® [See Table 3], which is a 2-4 dBA sound reduction.
Table 3.
Speech Intelligibility Index (SII) and Articulation Index (AI) measures made in five patient rooms on the standard unit in three acoustic conditions: No curtain, standard curtain, and Hush Curtain®
| Standard unit Four-bed-occupied Room “A” | No curtain | Standard curtain | Hush Curtain® | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SII | AI | SII | AI | SII | AI | |||||
| Patient in room | 0.640 | 0.564 | 0.607 | 0.521 | 0.524 | 0.426 | ||||
| Patient in room | 0.472 | 0.357 | 0.415 | 0.310 | 0.347 | 0.211 | ||||
| Patient in room | 0.520 | 0.413 | 0.442 | 0.332 | 0.305 | 0.196 | ||||
| Door | 0.288 | 0.182 | 0.262 | 0.157 | 0.158 | 0.082 | ||||
| Patient to nurse station | 0.025 | 0.006 | 0.000 | 0.000 | 0.000 | 0.000 | ||||
| Nurse station to patient | 0.089 | 0.043 | 0.025 | 0.006 | 0.032 | 0.006 | ||||
| One-bed “mirror” rooms — unoccupied | ||||||||||
| Room “B” | ||||||||||
| Doorway | 0.669 | 0.587 | 0.663 | 0.579 | 0.583 | 0.481 | ||||
| Hallway | 0.489 | 0.376 | 0.471 | 0.359 | 0.372 | 0.248 | ||||
| Patient to nurse station | 0.158 | 0.044 | 0.149 | 0.046 | 0.098 | 0.022 | ||||
| Nurse station to patient | 0.145 | 0.039 | 0.137 | 0.042 | 0.100 | 0.029 | ||||
| Room “C” | ||||||||||
| Doorway | 0.673 | 0.595 | 0.664 | 0.583 | ||||||
| Hallway | 0.507 | 0.395 | 0.503 | 0.394 | ||||||
| Patient to nurse station | 0.282 | 0.158 | 0.248 | 0.123 | ||||||
| Nurse station to patient | 0.262 | 0.139 | 0.229 | 0.105 | ||||||
| (Two-bed-occupied) | ||||||||||
| Room “D” | ||||||||||
| Patient in room | 0.722 | 0.655 | 0.677 | 0.597 | 0.620 | 0.536 | ||||
| Entry | 0.634 | 0.537 | 0.590 | 0.488 | 0.376 | 0.257 | ||||
| Door | 0.506 | 0.391 | 0.438 | 0.317 | 0.192 | 0.095 | ||||
| Patient to nurse station | 0.206 | 0.090 | 0.131 | 0.041 | 0.100 | 0.041 | ||||
| Nurse station to patient | 0.321 | 0.190 | 0.246 | 0.123 | 0.163 | 0.079 | ||||
| Four-bed-occupied | ||||||||||
| Room “E” | ||||||||||
| Patient in room | 0.604 | 0.511 | ||||||||
| Patient in room | 0.484 | 0.371 | ||||||||
| Patient in room | 0.444 | 0.327 | ||||||||
| Door | 0.291 | 0.187 | ||||||||
| Patient to nurse station | 0.011 | 0.001 | ||||||||
| Nurse station to patient | 0.086 | 0.023 | ||||||||
With this four-bed configuration the low background noise level resulted in insufficient masking of voices for beds situated side by side; thus, there was limited speech privacy even with the Hush Curtain® . However, even with the low background level, results for measures made at the beds across the room, through two curtains, showed significant improvement. This resulted in a 32-41% improvement in speech privacy, which improved the perceived speech privacy from “marginal” to “normal” range; this is equivalent to a 4-dBA sound reduction. A visual depiction of how the acoustical performance impacts the perception of a bedside medical alarm is shown in Figures 1 and 2.
Figure 1.
Standard unit_Room A_standard curtain with alarm
Figure 2.
Standard unit_Room A_Hush Curtain with alarm
In rooms B and C, mirror one-bed rooms, there was less than 5% improvement in speech privacy between the direct path (no curtain) and the standard curtain. The comparison between standard and Hush Curtain® revealed a 17-30% improvement in speech privacy, which is a 2-3 dBA sound reduction.
The measured differences between the mirror rooms were due to the location of the patient bed relative to the nurse station. Room B had a more direct line of sight path to the nurse station while Room C had a reflected sound path from the bed to the nurse station. There was additional noise reduction contributed by the barrier created by a doorway and a wall.
In Room D, a two-bed room, the change between the direct path (no curtain) and the standard curtain was between 6% and 9% improved speech privacy, and the change between the standard curtain and Hush Curtain® was 10-70% improved speech privacy, which is a 2-8 dBA sound reduction. The most significant improvement was found from the far bed to the door because the sound was transmitted through two layers of Hush Curtain®, one layer separating the patient beds and one layer separating the foot of the beds from the walkway into the room.
Room E, a four-bed room, was occupied by three patients; so testing was only completed on the standard curtain condition as a point of comparison to Room A. These results corresponded closely to the four-bed condition in Room A though these rooms were configured differently.
Rooms: Refurbished nursing unit
As a baseline the speech privacy and sound transmission were measured in Room F, a two-bed room. The difference between the standard curtain and no curtain was less than 10%. The results are shown in Table 4 and correspond well with the other two-bed rooms for the standard curtain configuration. The negligible improvement is attributed to the thin privacy curtain, which is the dominant condition for speech privacy and sound transmission.
Table 4.
Speech Intelligibility Index (SII) and Articulation Index (AI) measures made in three patient rooms on the standard unit in three acoustic conditions: No curtain, standard curtain, and Hush Curtain®
| Refurbished unit two -bed-occupied room “F” |
No curtain | Standard curtain | Hush Curtain® | |||
|---|---|---|---|---|---|---|
| SII | AI | SII | AI | SII | AI | |
| Doorway | 0.581 | 0.487 | 0.553 | 0.454 | ||
| 2nd patient bed | 0.536 | 0.428 | 0.503 | 0.389 | ||
| Hallway | 0.357 | 0.241 | 0.442 | 0.333 | ||
| Patient to nurse station | 0.009 | 0.000 | 0.010 | 0.000 | ||
| Nurse station to patient | 0.146 | 0.039 | 0.131 | 0.034 | ||
| Two-bed-unoccupied | ||||||
| Room “G” | ||||||
| Doorway | 0.706 | 0.639 | 0.674 | 0.597 | 0.511 | 0.404 |
| 2nd patient bed | 0.592 | 0.492 | 0.570 | 0.470 | 0.375 | 0.264 |
| Hallway | 0.501 | 0.408 | 0.468 | 0.366 | 0.378 | 0.263 |
| Patient to nurse station | 0.020 | 0.003 | 0.019 | 0.001 | 0.010 | 0.000 |
| Nurse station to patient | 0.193 | 0.075 | 0.172 | 0.061 | 0.115 | 0.033 |
| One-bed-unoccupied | ||||||
| Room “H” | ||||||
| Doorway | 0.644 | 0.559 | 0.614 | 0.523 | 0.612 | 0.521 |
| Hallway | 0.449 | 0.328 | 0.403 | 0.278 | 0.394 | 0.266 |
| Patient to nurse station | 0.262 | 0.149 | 0.249 | 0.136 | 0.203 | 0.092 |
| Nurse station to patient | 0.274 | 0.150 | 0.261 | 0.135 | 0.215 | 0.096 |
In Room G, a two-bed room, there was a 5-10% improvement in speech privacy measures between the no curtain and standard curtain conditions. The improvement in speech privacy between the standard curtain and the Hush Curtain® was 30-45%, which is a 2-6 dBA sound reduction. A visual depiction of how the acoustical performance impacts the perception of a bedside medical alarm is shown in Figures 3 and 4.
Figure 3.
Refurbished unit_Room G_standard curtain with alarm
Figure 4.
Refurbished unit_Room G_Hush Curtain with alarm
In Room H, a one-bed room, there was a 5-10% improvement in speech privacy between the direct path (no curtain) and the standard curtain condition. The speech privacy improvement between the standard curtain and Hush Curtain® was less than 10% just outside the curtain but increased to 25% to the nurse's station, which is a 1-2 dBA sound reduction. The small difference between the two curtain types was likely due to the architectural design that included a short hall within the single patient room, and most of the acoustic improvement was due to the plenum effect and barrier effect of the room and doorway.
Discussion
The acoustic assessment performed on two nursing units demonstrated that acoustically enhanced privacy curtains can provide additional auditory protection for patients though the overall speech privacy and sound reduction performance with the Hush Curtains® were limited by the architectural and overall acoustical design of the patient rooms and facility.
On average the Hush Curtains® improved the average sound absorption by 20-30% for rooms that already had relatively low reverberation times with acoustical ceiling tile, hospital bed mattresses, and furnishings. However, there was considerable variability in their effectiveness, depending on the orientation, configuration, and location of the rooms being tested. This was specifically noted in the comparison of one-bed room Room H with a long vestibule, and Rooms B and C with no vestibule. Room H had “marginal” improved to “normal” speech privacy levels in the hallway adjacent to the room with the addition of the Hush Curtain® while Rooms B and C had “no privacy” improved to “marginal” speech privacy levels in the hallway adjacent to the room with the addition of the Hush Curtain® . This shows that while the enhanced acoustic curtain reduces the sound transmission, this system cannot ameliorate fundamental acoustical design issues.
The SII and AI results revealed that the low background noise levels inside the rooms limited the speech privacy effectiveness for both standard curtains and Hush Curtains® between the patient beds although with the improved sound reduction of the Hush Curtains® the speech privacy was improved. The elevated background sound levels in the corridors provided better overall speech privacy for all conditions from patient rooms, and the Hush Curtains® provided a speech privacy improvement of 15–60% depending on the architectural layout, room orientation-floor plate shape, and the sound absorptive performance of the room finishes and ceiling tiles.
Auditory cues allow nurses to determine a patient's need for assistance or assessment even when a patient is not in the direct line of sight. A hospital's acoustic characteristics play a critical role in how quickly a nurse hears an acoustic cue — An alarm, a patient's voice — And accurately place it so that the nurse knows exactly where to go to address the need.[16] The figures visually depicting the audibility of bedside medical alarms shows that for most conditions, alarm systems near patients are not clearly audible above background noise outside of the patient room. This means that alarms may be active for longer periods of time before the staff hear and respond.
Ryherd and Oku's research has expanded our understanding beyond the impact of surface materials on reverberation. Their work illustrates the impact of floor plate shapes on corridor reverberation rates. Specifically, their simulations identified “visual fragmentation” and “relative grid distance” as significantly correlated with increased reverberation time. The increased reverberation time would result in nurses’ reduced ability to accurately locate a sound source.[16]
Limitations
This study has several important limitations. The study was conducted on clinical nursing units while patient care was ongoing; therefore, some accommodations had to be made while performing the various acoustic measures. For that reason, not every measure was made in every room. However, because we also selected “mirror” rooms, we can reasonably extrapolate what most of the measures would be. On the other hand, a strength of the study is that the measures were made in “real” conditions — with patients in some rooms and not in others. Acoustic guidelines for health care settings are currently published at levels recommended for unoccupied buildings. Rarely are newly constructed or refurbished patient care units tested when they are in use. This study has provided valuable evidence related to the performance of the metrics recommended by standard guidelines in a functional inpatient medical care environment.
This study was conducted on nursing units with the same overall footprint but from different eras of construction. These differences in construction had the most significant impact on the sound absorptive performance of the ceiling tiles, and the layout of the rooms in relation to the nurses’ stations. This made the study useful in providing a context for the effective differences between the two types of privacy curtains: Standard fabric and Hush Curtains® for 1970s era building compared to the 2010s construction. To provide a more generalizing conclusion about the results a more in-depth study in the future of the effects of the floor plate, room configurations, and material finishes is needed.
The AI measures used in this study may not be an exact reflection of speech privacy. This metric is the current standard that is noted in the Facility Guidelines Institute but speech privacy and intelligibility metrics are still being reevaluated and improved to more closely match with ongoing research in psychoacoustics. For example, although current metrics incorporate speech frequencies, they do not reveal whether or not extraneous voices contributed to the background decibel measurements. More testing designed to directly compare human experience is encouraged to better determine the accuracy of this and other metrics in calculating speech privacy. That being said, we did follow the AI recommendation to compare the relative privacy measured between different locations within open plan spaces. We also followed the recommendation to evaluate how environmental variables such as barriers, furniture, ceilings, masking sound, or wall panels in open plan components influenced speech privacy metrics.[13]
This study was conducted over 2 days that were selected based on factors related to availability of the acoustical engineer, the Hush Curtain® vendor, housekeepers, and nurse managers of the nursing units. We have no way of knowing whether the noise on the nursing units was typical. The variance in background noise has a direct impact on the predicted speech privacy and intelligibility metrics. The background noise levels were usually within 5 dB of the measured sound transmission source for some of the rooms that were more than 10.5 meters from the nurse stations, which reinforces the “confidential” rating that was measured but does impact the standard deviation of the measurements to this location. The background sound levels were measured in mostly unoccupied rooms, and in all cases the patients and staff were asked to refrain from talking and common background noise sources (televisions, radios, etc.) were muted during the ambient measurement. This provided a prediction that is the “worst case scenario” in the context of speech privacy when other patients in a multiple patient room are sleeping, and one patient is interacting with a health care provider. This scenario was observed in both four-bed patient rooms during the 2-two day testing. If additional ambient noise conditions were measured from some staff and patient activity in the rooms, then the sound privacy ratings would all improve. Based on our measurements and observations, it is not likely that the background noise levels would be much lower than the levels used in this study.
What is missing from our results is the perception of speech privacy and speech intelligibility from the hospital staff and patients. The ultimate goal of refining acoustic metrics for health care settings is to improve the safety, comfort, privacy, and care provided in these environments. That is only possible with the collection of the human experience of the environment in addition to the building materials, layout, and acoustic measures. Unfortunately, that was not possible within the time and financial constraints of this study.
Our study results suggest that room and floor layout configuration plays a large role in the acoustics of hospital patient rooms, and alterations to the privacy curtain provides measurable improvement but cannot overcome larger acoustic design issues. Overall, to provide sound environments with shorter reverberation time, designers should integrate sound absorptive finishes, and take into consideration how the room and facility layout will impact and how the nursing staff will interact with one another and with patients. Locating staff near patient doors with beds oriented so that the nurse can see the head of the bed will improve response time but will reduce speech privacy. To improve the speech privacy for patients, more fragmented nursing unit floor-plate shapes could be created in conjunction with the use of remote calls and monitoring.[16]
Financial support and sponsorship
This material is the result of work supported with resources and the use of facilities at the VA Portland Health Care System. Chinook Acoustics, Inc. paid Erik Miller-Klein for acoustical assessment. The contents of this publication do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We extend our thanks to the nurse managers, and nursing and housekeeping staff of the two nursing units for their enthusiastic cooperation with this research. In addition, we want to acknowledge the interest and support of the veteran inpatients whose hospital rooms were evaluated.
References
- 1.Fife D, Rappaport E. Noise and hospital stay. Am J Pub Health. 1976;66:680–1. doi: 10.2105/ajph.66.7.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker CF, Garvin BJ, Kennedy CW, Polivka BJ. The effect of environmental sound on communication on CCU patients’ heart rate and blood pressure. Res Nurs Health. 1993;16:415–21. doi: 10.1002/nur.4770160605. [DOI] [PubMed] [Google Scholar]
- 3.Hagerman J, Rasmanis G, Blomkvist V, Ulrich R, Eriksen CA, Therorell T. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. Int J Cardiol. 2005;98:267–70. doi: 10.1016/j.ijcard.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Joseph A, Ulrich R. Concord, CA: The Center for Health Design; 2007. Sound Control for Improved Outcomes in Healthcare Settings; pp. 1–15. [Google Scholar]
- 5.Hsu T, Ryherd E, Persson Waye K, Ackerman J. Noise pollution in hospitals: Impact on patients. J Clin Outcomes Manag. 2012;19:301–9. [Google Scholar]
- 6.Ryherd E, Ackerman J, Zimring C, Okcu S, Persson Waye K. Noise pollution in hospitals: Impact on staff. J Clin Outcomes Manag. 2012;19:491–500. [Google Scholar]
- 7.Okcu S, Ryherd E, Zimring C, Samuels O. Soundscape evaluations in two critical healthcare settings with different designs. J Acoust Soc Am. 2011;130:1348–58. doi: 10.1121/1.3607418. [DOI] [PubMed] [Google Scholar]
- 8.Lawson N, Thompson K, Saunders G, Saiz J, Richardson J, Brown D, et al. Sound intensity and noise evaluation in a critical care unit. Am J Crit Care. 2010;19:e88–99. doi: 10.4037/ajcc2010180. [DOI] [PubMed] [Google Scholar]
- 9.Pope D. Decibel levels and noise generators on four medical/surgical nursing units. J Clin Nurs. 2010;19:2463–70. doi: 10.1111/j.1365-2702.2010.03263.x. [DOI] [PubMed] [Google Scholar]
- 10.Gladd DK, Saunders GH. Ambient noise levels in the chemotherapy clinic. Noise Health. 2011;13:444–51. doi: 10.4103/1463-1741.90322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryherd EE, Moeller M, Jr, Hsu T. Speech intelligibility in hospitals. J Acoust Soc Am. 2013;134:586–95. doi: 10.1121/1.4807034. [DOI] [PubMed] [Google Scholar]
- 12.Pope DS, Gallun FJ, Kampel S. Effect of hospital noise on patients’ ability to hear, understand, and recall speech. Res Nurs Health. 2013;36:228–41. doi: 10.1002/nur.21540. [DOI] [PubMed] [Google Scholar]
- 13.West Conshohocken, PA: ASTM International; 2008. [Last accessed on 2015 Dec 13]. ASTM E1130-08. Standard Test Method for Objective Measurement of Speech Privacy in Open Plan Spaces Using Articulation Index. Available from: http://www.astm.org . [Google Scholar]
- 14.New York, USA: Acoustical Society of America; 1997. ANSI S3.5-1997. Methods for Calculation of the Speech Intelligibility Index. American National Standard, Standards Secretariat. [Google Scholar]
- 15.Chicago, IL: The American Society for Healthcare Engineering of the American Hospital Association; 2010. Facility Guidelines Institute Guidelines for Design and Construction of Healthcare Facilities; pp. 24–37. [Google Scholar]
- 16.Okcu S, Shpuza E, Ryherd R, Zimring C. Linking acoustics and floor-plate shape qualities of healthcare settings. Arch Sc Rev. 2013;56:315–32. [Google Scholar]