Abstract
Previous research indicates that exposure to noise during sleep can cause sleep disturbance. Seamen on board vessels are frequently exposed to noise also during sleep periods, and studies have reported sleep disturbance in this occupational group. However, studies of noise and sleep in maritime settings are few. This study's aim was to examine the associations between noise exposure during sleep, and sleep variables derived from actigraphy among seamen on board vessels in the Royal Norwegian Navy (RNoN). Data were collected on board 21 RNoN vessels, where navy seamen participated by wearing an actiwatch (actigraph), and by completing a questionnaire comprising information on gender, age, coffee drinking, nicotine use, use of medication, and workload. Noise dose meters were used to assess noise exposure inside the seamen's cabin during sleep. Eighty-three sleep periods from 68 seamen were included in the statistical analysis. Linear mixed-effects models were used to examine the association between noise exposure and the sleep variables percentage mobility during sleep and sleep efficiency, respectively. Noise exposure variables, coffee drinking status, nicotine use status, and sleeping hours explained 24.9% of the total variance in percentage mobility during sleep, and noise exposure variables explained 12.0% of the total variance in sleep efficiency. Equivalent noise level and number of noise events per hour were both associated with increased percentage mobility during sleep, and the number of noise events was associated with decreased sleep efficiency.
Keywords: Navy, noise exposure, seamen, sleep, vessel
Introduction
It is well recognized that exposure to noise may cause adverse health effects, such as sleep disturbance.[1] Relationships between environmental noise and sleep have been thoroughly studied,[2,3,4] but little emphasis has been put on noise and sleep in occupational settings. For seamen, assessing sleep and stressors affecting sleep is pertinent, as sleep is considered essential for quality of life, health, and daytime performance.[3] Several studies have shown that obtaining adequate sleep may be a challenge for seamen,[5,6,7,8,9,10] and accidents at sea have been related to fatigue or sleepiness, which is closely linked to insufficient sleep.[11,12] Noise is one of the main physical stressors on board vessels,[13] and questionnaire surveys among seamen have indicated noise as an important cause for sleep disturbance at sea.[14,15] A recent study in the Royal Norwegian Navy (RNoN) reported mean noise levels in cabins during typical operating modes to range from 44 to 78 dB(A) depending on vessel type.[16] According to the WHO guidelines (i.e., Leq,night,outside of 40 dB(A)), these levels are expected to disturb sleep.[3]
Although noise can be expected to affect seamen's sleep, the authors have been able to identify only two laboratory studies and two field studies with objective measurements of noise and sleep on vessels.[17,18,19,20,21] In addition to noise level, individuals’ sensitivity and noise characteristics such as number of noise events have implications for sleep disturbance from noise.[2,3] However, we are not aware of any studies investigating number of noise events on board vessels. More knowledge on how noise influence seamen's sleep is warranted. The aim of this study was to determine noise exposure (based on noise dose meters) during sleep and to study the associations between noise exposure (equivalent noise level and noise events) and objectively monitored sleep (based on actigraphic recordings) on board RNoN vessels.
Methods
As part of a larger study of noise and health in the RNoN, data were collected on board 21 RNoN surface vessels during April 2012 to June 2013. Data collection was carried out by two trained researchers who stayed on board each vessel for one to three consecutive days. The vessels operated mainly in sheltered waters along the Norwegian coast with an inclusion criterion for maximum sea state during data collection set to 3, which indicates a maximum wave height of about 1.25 m. The reason for this exclusion criterion was that high seas may influence the actigraphs used in the study. The study was approved by the RNoN and by the Regional Committee of Medical and Health Research Ethics, South East Norway. Results were treated anonymously, and individual data were not accessible to the RNoN.
Participants
When the researchers entered a vessel, the management was asked to identify 2-5 potential participants from different job categories on board (engineers, navigators, chefs, etc.), ensuring that the sample of seamen was representative for different kinds of work on board navy vessels. The selected seamen were then informed about the study and those who agreed to participate signed an informed consent. Only one person did not agree to participate. A total of 72 officers and sailors (no conscripts) from 21 RNoN vessels participated in the study, having both noise exposure and sleep monitored during at least one sleep period. All personnel working on board RNoN vessels need to fulfill a set of physical and psychological requirements; thus, the health status of the participating seamen was considered to be good.
Design
Upon the researchers’ arrival, usually around noon or in the afternoon, the enrolled seamen completed a questionnaire comprising information on gender, age, coffee drinking (yes/no), nicotine use (yes/no), medication use, workload before sleep (visual analog scale: 0-10), and position on board. Then, an actiwatch (actigraph) was mounted on their nondominant wrist, and the participants were instructed to press an event button on the actiwatch when they went to bed with the intention to sleep (bedtime), and again upon final awakening (rise time). Noise dose meters were placed in the seamen's cabins, preferably close to the head position during sleep. The actiwatch and the noise dose meter logged continuously for 1-3 days during the sampling period.
Instruments and measures
To monitor noise exposure, Brüel and Kjaer noise dose meter Type 4445 were used. The dose meters were calibrated before placement in the cabins and checked after the end of the measurement period. The dose meters measurement range was set to 30-100 or 50-120 dB depending on the expected noise level in the cabin. The noise dose meter logged the following parameters each minute: Equivalent continuous A-weighted noise level using a 3 dB exchange rate, and maximum A-weighted noise level (LAmax). Noise measurement data was processed using the software, Protector Type 7825 Version 5.0.0 (Brüel & Kjær Sound & Vibration Measurement A/S, Nærum, Denmark). For each sleep period measured by the actiwatch, the corresponding time interval from the noise dose meter was selected for identification of LAmax for each minute and for calculation of the equivalent noise level for the total sleep period. To identify noise events, the following definition was used; a noise event occurred if the LAmax level for a measured minute was at least 9 dB higher than the LAmax level in the preceding minute. The number of noise events during a sleep period were counted and coded manually into a “noise events” variable. The noise events variable was transformed into “noise events per hour” to be able to conduct statistical analysis adjusted for variation in duration of the sleep periods. To obtain a measure of the intensity of the noise events in a sleep period, the mean LAmax level of the identified noise events was calculated. For identification and counting of noise events, Microsoft Excel 2010 was used.
Actigraphs were used to monitor the seamen's sleep. The actigraphs measure body movements during sleep, and actigraphy is a validated method for sleep monitoring.[22] Two similar types of actiwatch models were used: AW4, produced by Cambridge Neurotechnology Ltd. (http://www.camntech.com/), and the newer actiwatch 2, produced by Philips, Respironics (http://actigraphy.respironics.com/). Both actiwatch models contain a piezoelectric accelerometer with a sampling rate of 32 Hz. The two similar models have been compared, and equivalent activity, and sleep statistics have been indicated.[23] In the current study, independent samples t-tests showed no significant differences between the sleep variables obtained with AW4 as compared with actiwatch 2. The participants used the event button on the actiwatch to indicate bed time and rise time. The software, Respironics Actiware Version 5.61 (Philips Respironics, Inc. Murrysville, PA, USA), was used to preprocess the data from the actiwatch. The epoch length was set to 1 min, and the sensitivity was set to medium. The sleep periods were identified and sleep variables within these intervals were extracted [Table 1].
Table 1.
Explanation of sleep variables extracted from the actiwatch
| Sleep variable | Explanation | Measure |
|---|---|---|
| Bedtime | The time participant went to bed with the intent to sleep | Time |
| Rise time | The time participant got up and started the day | Time |
| Sleep onset latency | Period of time between bedtime and sleep initiation | Minutes |
| Time in bed (sleep period) | Time between bed time and rise time | Hours |
| Sleep interval duration | Time between sleep start and sleep end | Hours |
| Awakenings | Number of awakenings during the sleep interval | Number |
| Average duration of awakenings | Average duration of blocks scored as wake (awakenings) | Minutes |
| WASO | Wake after sleep onset — the number of waking minutes between sleep start and sleep end | Minutes |
| Percentage mobility | Percentage of time scored as mobile in the sleep interval | Percentage |
| Sleep efficiency | Percentage of time in bed actually spent sleeping | Percentage |
As for the noise events variable, the sleep variables awakenings and wake after sleep onset (WASO) were transformed to their measurement unit “per hour,” to adjust for variation in duration of the sleep periods. The variables “bed time” and “rise time” were transformed into the variable “sleeping hours” with the categories nighttime (sleep period between 9 p.m. and 9 a.m.) and daytime (sleep period fully or partly between 9 a.m. and 9 p.m.). The “sleeping hours” variable was used as an independent variable while the other sleep variables were used as dependent variables in the analysis.
Selection
A total of 95 sleep periods were measured among the 72 seamen. Nineteen of the seamen had 2-4 sleep periods measured while 53 had one sleep period measured. For five sleep periods, the sleep interval duration (time between sleep start and sleep end) were shorter than 90 min and were excluded as this was considered to be too short to ensure that the sleep period was representative in terms of different sleep stages.[24] Furthermore, three noise measurements were excluded since they did not record noise during the whole sleep period, and four actiwatch recordings were excluded due to sea state >3 and high speed compromising the reliability of the actiwatch on board one vessel. Thus, a total of 83 sleep periods from 68 seamen were included in analysis [Figure 1].
Figure 1.
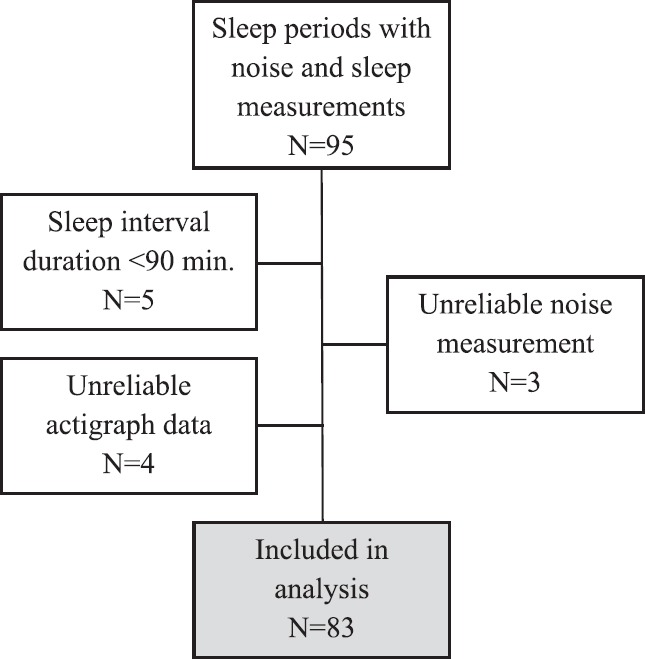
Flowchart describing exclusions from the data material
Among the 83 included sleep periods, 41 were monitored on board, 11 coast guard vessels, 12 on two frigates, 13 on three mine vessels, eight on two supply vessels, four on one coastal corvette, and five on the Royal Yacht. Of the included participants, 13 were engine room workers, 14 sailors, eight navigators, seven chefs, seven electricians, seven office workers, five operation room workers, and seven belonged to miscellaneous job categories.
Data analysis
The residuals of sleep onset latency were not normally distributed; therefore, sleep onset latency was log-transformed (LN) before analysis. The residuals of the LN-transformed variable were normally distributed. The noise events variable were categorized into three equal groups; more than 1.1 events per hour (Group 1), 0.5-1.1 events per hour (Group 2), and <0.5 events per hour (Group 3).
As preparatory analysis, correlations between the equivalent noise levels, the mean LAmax of noise events, age, workload, and sleep variables were calculated using Pearson's product-moment correlation test. Independent samples t-tests were used to compare the sleep variables between different categorical variables (male vs. female, coffee drinker vs. no coffee drinker, nicotine use vs. no use, night vs. day sleep). One-way analysis of variance was conducted to compare the different sleep variables between the three noise events groups, and also to check if the equivalent noise levels and mean LAmax of noise events, differed with the three noise events groups.
Linear mixed-effects models were used to examine the association between noise exposure and sleep. The sleep variables associated (P ≤ 0.2) with at least one of the noise exposure variables in preparatory analysis were included as dependent variables in separate mixed-effects models. The individual participants and vessels were entered as random factors in the random- and the mixed-effects models. The fixed factors were entered in the mixed-effects models in two stages. Possible confounders (gender, age, coffee consumption, nicotine use, workload, sleeping hours) associated (P ≤ 0.2) with at least one of the sleep variables in preparatory analysis were entered as fixed factors in model 1. The fixed factors with significance value P ≤ 0.2 were retained before entering the noise exposure variables (equivalent noise level, noise events per hour, and mean LAmax of the noise events) as fixed factors in model 2. In the final model, the fixed factors with significance value P ≤ 0.2 were retained. To test if the fixed factors in the mixed-effects models explained significantly more variance in the different sleep parameters than the random-effects model, comparison of 2 times the restricted log likelihood to the Chi-square distribution with 6 degrees of freedom were made.
The Statistical Products of Service Solution package (SPSS) version 22 (IBM Corporation, Armonk, NY, USA) was used for statistical analysis.
Results
Table 2 shows the descriptive statistics for the sleep periods, including noise exposure and sleep variables. The majority of the participants were male seamen. Nine (11%) of the sleep periods were from female participants. About 40% reported the use of nicotine, which includes both use of cigarettes and/or moist snuff. Almost 80% of the sleep periods was categorized as night sleep (sleep period between 9 p.m. and 9 a.m.). None of the participants reported the use of medication. There was considerable variation in noise exposure during sleep, and 17 of the sleep periods had equivalent noise level >60 dB(A), thus exceeding applicable maritime regulations recommended maximum for cabin noise.[25] In addition, the sleep variables varied substantially [Table 2].
Table 2.
Descriptives of 83 sleep periods among 68 seamen on board 20 Royal Norwegian Navy vessels
| Variables | n (%) | Mean (SD) | Median (minimum-maximum) |
|---|---|---|---|
| Gender | |||
| Male | 74 (89) | ||
| Age (years) | 30 (8) | 29 (18-61) | |
| Coffee drinker | |||
| Yes | 38 (46) | ||
| Nicotine user | |||
| Yes | 30 (36) | ||
| Workload before sleepa | 3.5 (2.0) | 3.5 (0.0-8.3) | |
| Sleeping hours | |||
| Night | 65 (78) | ||
| Noise exposure during sleep | |||
| Equivalent noise level (dB(A)) | 55.5 (5.9) | 54.2 (43.1-71.2) | |
| Noise events per hour | 1.2 (1.3) | 0.8 (0.0-6.6) | |
| ≥1.1 (Group 1) | 29 (35.0) | 2.4 (1.6)b | 1.6 (1.1-6.6) |
| 0.5-1.1 (Group 2) | 27 (32.5) | 0.8 (0.2) | 0.8 (0.5-1.1) |
| <0.5 (Group 3) | 27 (32.5) | 0.3 (0.2) | 0.3 (0.0-0.5) |
| Mean LAmax (dB(A)) of noise events | 71.9 (7.6)c | 71.6 (53.2-92.4)c | |
| Sleep | |||
| Sleep onset latency (min) | 6.8 (7.8) | 4.0 (0.0-43.0) | |
| Time in bed (h) | 6.6 (2.0) | 6.9 (1.9-11.5) | |
| Sleep interval duration (h) | 6.4 (1.9) | 6.7 (1.8-11.4) | |
| Awakenings (/h) | 3.3 (1.0) | 3.3 (1.0-5.4) | |
| Average duration of awakenings (min) | 1.9 (0.6) | 1.8 (1.0-3.6) | |
| Wake after sleep onset (min/h) | 6.3 (2.6) | 6.3 (1.3-15.9) | |
| Mobility during sleep (percentage) | 13.7 (5.1) | 12.7 (5.0-29.2) | |
| Sleep efficiency (%) | 86.5 (5.2) | 86.7 (70.2-94.9) |
aMarking on a visual analogous scale of 10 cm indicating workload. Missing: n = 4, bOne-way analysis of variance indicated differences at the P < 0.01 level between Groups 1 and 2, and Groups 1 and 3, cMean and median of the mean LAmax level of the identified noise events for each sleep period. SD = Standard deviation
Preparatory analysis
There were significant correlations (P < 0.05) between equivalent noise level and the sleep variables time in bed (r = −0.32), sleep interval duration (r = −0.32), average duration of awakenings (r = 0.23), percentage mobility (r = 0.32) and sleep efficiency (r = −0.24). In addition equivalent noise level correlated with age (r = −0.25). Equivalent noise level and the mean LAmax of noise events were intercorrelated with each other (r = 0.65). Sleep onset latency and sleep efficiency, time in bed and sleep interval duration, awakenings and WASO, percentage mobility and sleep efficiency, and the variables average duration of awakenings, WASO, percentage mobility, and sleep efficiency, were significantly intercorrelated (P < 0.01) with each other.
There was significant difference (P < 0.05) in percentage mobility during sleep between males (mean = 14.2, standard deviation [SD] = 5.1) and females (mean = 9.5, SD = 1.9). There were also significant differences (P < 0.05) in awakenings per hour and percentage mobility between sleep periods at night (mean awakenings per hour = 3.2, SD = 0.8, mean percentage mobility = 13.0, SD = 4.5) and sleep periods during the day (mean awakenings per hour = 3.8, SD = 1.2, mean percentage mobility = 16.1, SD = 6.1). There were no significant differences in any of the other sleep variables when analyzed for gender, age, coffee consumption, nicotine use, workload, and sleeping hours (night vs. day).
Between the three noise events groups, there were significant differences (P < 0.05) in the average duration of awakenings, WASO per hour, percentage mobility during sleep and sleep efficiency. There were no significant differences in equivalent noise levels and mean LAmax of the noise events for the three different noise events groups.
Variables in mixed-effects models
The sleep variables, “time in bed,” “sleep interval duration,” “awakenings per hour,” “average duration of awakenings,” “WASO per hour,” “percentage mobility during sleep,” and “sleep efficiency” were associated (P ≤ 0.2) with at least one of the noise exposure variables and were consequently entered as dependent variables in separate random- and mixed-effects models. In addition to the noise exposure variables, gender, coffee drinking status, nicotine use status, and sleeping hours were associated with at least one of the sleep variables (P ≤ 0.2), and were thus entered as fixed factors in the mixed-effects models.
Mixed-effects models
The mixed-effects model with percentage mobility during sleep and sleep efficiency as dependent variables differed significantly (P < 0.05) from the corresponding random-effects model. Thus, only results from these two models are presented [Table 3].
Table 3.
Linear random- and mixed-effects models of percentage mobility during sleep and sleep efficiency. Analysis of 83 sleep periods among 68 seamen on board 20 Royal Norwegian Navy vessels
| Model components | Percentage mobility during sleep (%) | Sleep efficiency (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Random-effects model | Mixed-effects model 1 | Mixed-effects model 2a | Random-effects model | Mixed-effects model 1 | Mixed-effects model 2a | |||||||
| β | SE | β | SE | β | SE | β | SE | β | SE | β | SE | |
| Fixed effects | ||||||||||||
| Intercept | 13.59* | 0.82 | 13.13* | 1.02 | −0.93 | 5.57 | 86.63* | 0.77 | 86.89* | 1.14 | 98.93* | 5.77 |
| Gender (0=male, 1=female) | −2.80b | 1.63 | −1.08 | 1.98 | ||||||||
| Coffee drinker (0=no, 1=yes) | 3.04* | 1.15 | 3.89* | 1.11 | −0.91 | 1.41 | ||||||
| Nicotine user (0=no, 1=yes) | −2.77* | 1.13 | −2.75* | 1.09 | 1.60 | 1.39 | ||||||
| Sleeping hours (0=night, 1=day) | 1.70b | 1.16 | 1.81b | 1.12 | −1.59 | 1.44 | ||||||
| Equivalent noise level | 0.21* | 0.10 | −0.19b | 0.10 | ||||||||
| Noise events per hour | ||||||||||||
| 1.1 or more | 3.05* | 1.12 | −3.45* | 1.33 | ||||||||
| 0.5-1.1 | 2.94* | 1.12 | −2.75* | 1.34 | ||||||||
| <0.5 | Reference | Reference | ||||||||||
| Random effectsc | ||||||||||||
| Within-worker variance | 15.10 | 2.63 | 16.66 | 2.46 | 13.32 | 2.42 | 21.41 | 3.79 | 21.83 | 4.00 | 21.95 | 3.98 |
| Between-vessel variance | 9.30 | 4.06 | 7.42 | 5.06 | 2.77 | 6.12 | 3.87 | 5.77 | 3.97 | 2.29 | 2.87 | |
| Percentage of variance explained by the fixed effects | 1.3 | 24.9 | −0.3 | 12.0 | ||||||||
*P < 0.05, aThe variable “mean LAmax of noise events” was also entered in the mixed-effects model 2, but were not retained (P > 0.2) in the final model, bP ≤ 0.2: The variable was retained in the model, cBetween-worker variance could not be calculated. SE = Standard error
For percentage mobility during sleep, the final mixed-effects model including the fixed factors coffee drinking status, nicotine use status, sleeping hours, equivalent noise level, and noise events per hour, explained one-fourth of the total variance in percentage mobility [Table 3]. Four of the five-fixed factors in the final model were significant determinants (P < 0.05). The final model 2 indicates that higher noise exposure, having the sleep period during daytime, and being a coffee drinker, increases percentage mobility during sleep, while being a nicotine user was associated with less mobility during sleep. Within the range of the measured equivalent noise levels (43-71 dB(A)), a 5.9% difference in mobility during sleep can be expected, while exposure to more than 1.1 noise events per hour increases mobility by 3.1% compared to <0.5 events per hour. Moreover, being a coffee drinker suggests 3.9% more mobility compared to not being a coffee drinker, and using nicotine suggests 2.8% less mobility compared to not using nicotine in the final model.
For sleep efficiency, the final mixed-effects model 2 included equivalent noise level and noise events per hour, but the number of noise events per hour was the only significant determinant (P < 0.05). Exposure to more than 1.1 events per hour was associated with 3.5% decrease in sleep efficiency as compared to less than 0.5 events per hour.
For both percentage mobility during sleep and sleep efficiency, the mixed-effects models showed a relatively high within-worker variance as compared to between-vessel variance [Table 3]. The fixed factors were associated with decreased between-vessel variances, and for percentage mobility, the noise exposure variables were associated with decreased within-worker variance. The between-worker variance could not be calculated.
Discussion
Noise exposure during seamen's sleep on board RNoN vessels was found to be associated with increased percentage mobility during sleep and reduced sleep efficiency. The equivalent noise level, the number of noise events and coffee drinking status were significantly associated with increased percentage mobility during sleep while nicotine use status was associated with decreased mobility during sleep. The number of noise events was the only variable significantly associated with reduced sleep efficiency. Noise exposure was not related to the other sleep variables such as sleep onset and number of awakenings.
In prior studies among seamen, sleep disturbance, and poor sleep quality on board vessels have frequently been reported,[5,6,8] and in a questionnaire survey of offshore fleet workers, noise was reported to be the most important cause of sleep problems at sea.[14] However, in the few previous field studies with objectively monitored noise and sleep on board vessels, results were ambiguous regarding the relationship between noise and sleep.[19,20,21] In the first phase of a research program on seafarer's fatigue, investigating noise (dose meter) and sleep (actigraphy) on board supply vessels for the oil industry, there were significant correlations between noise level, sleep efficiency (r = −0.32), and sleep latency (r = 0.26).[19] However, in a second phase of the program, using similar methods on board vessels in the short sea shipping industry (small tankers and ferries), no associations between noise and sleep were found.[19] Moreover, on board a U.S. Navy vessel (HSV-2 SWIFT), no associations between objectively monitored noise exposure and sleep were found.[20] The mean equivalent noise level on board the supply vessels was 63 dB(A); range 55-72 dB(A), and similar noise levels (mean ≈ 65 dB(A)) were found on board the ferries and tankers.[19] The noise levels on board the vessels in the seafarer's fatigue program cannot be directly compared to the levels in the current study as the dose meters in the fatigue program were placed in locations across the vessels and not merely in the cabins. The seamen on board the supply vessels had an average percentage immobility during sleep of 91.0% (i.e., mean percentage mobility = 9.0%), and the mean sleep efficiency was 88.6% (SD = 4.6).[21] Thus, the seamen on board the supply vessels had markedly lower mean percentage mobility, and slightly higher mean sleep efficiency, than the RNoN seamen who had mean percentage mobility and mean sleep efficiency of 13.7% and 86.5%, respectively. Details on percentage mobility and sleep efficiency in the study on board the ferries and tankers were not available. On board the U.S. Navy vessel, the average background noise levels were reported to be 55.5 dB(A), similar to the RNoN vessels; however, the sleep efficiency among 14 U.S. Navy crew members were lower than for the RNoN seamen with an average of 78.9%.[20]
In the seafarer's fatigue program the ambiguous findings in the two phases of the project were suggested to be related to the difference in the character of the noise on board the vessel types.[19] On the ferries and tankers, the noise was reported to be of a more continuous character than on board the supply vessels where intermittent noise such as alarms and doors closing were common.[19] Furthermore, in the U.S. Navy study, the lack of significant associations between noise and sleep were related to the limited range and the generally consistent noise levels on board HSV-2 SWIFT.[20] There were also few participants (N = 16) limiting the statistical power.[20] The current study differs from the previous field studies as our study had larger variability in noise exposure levels (e.g., equivalent noise level: 43-71 dB(A)), and more participants (N = 68) than in the U.S. Navy study. In addition, the current study measured noise exposure also in terms of the number of noise events. To the author's knowledge, no previous studies of sleep among seamen have considered the number of noise events’ effects on sleep.
In a sleep laboratory, study exposing three men to a steady ship noise level, and comparing sleep parameters for exposed nights (65 dB(A)) with control nights (35-40 dB(A)), no difference in percentage movement time, or sleep efficiency was found.[17] However, the study did find effects of noise on other sleep variables as measured by polysomnography, and suggested adverse effects of noise on night sleep through decreased percentage rapid eye movement sleep and increased shallow sleep.[17] The mean sleep efficiency for the exposed nights in the laboratory study was 88.7%,[17] which is slightly higher than in the current field study. The lower sleep efficiency in the current study as compared to the laboratory study was expected, as the laboratory rule out other factors which may influence sleep.
Although few participants had repeated measurements in the current study, the relatively high within-worker variance indicate that individuals’ sleep quality vary between sleep periods. For percentage mobility during sleep, noise exposure was associated with a decreased within-worker variance, thus explaining some of the variation between individuals’ sleep periods. However, also, other factors such as watch systems and day-to-day variation in operational requirements and activities are likely to cause variation between seamen's sleep periods on board the RNoN vessels. Variation between sleep periods have been reported among watch keepers (4 h on and 8 h off) on board a research vessel sailing from the United Kingdom to Antarctica, where the seamen's sleep efficiency in the second sleep period was poorer as compared to the main sleep period.[5] In a study of fishermen's sleep, the activities on board varied substantially from day-to-day, causing large variability in the amount of obtained sleep.[6]
While previous research on noise and sleep in maritime settings is limited, prior research has established relationships between environmental noise and sleep, such as increased body movements.[3] An increase in body movements during sleep can be regarded as a marker of arousal and shallower sleep stages, but the relationship is complex as body movements during sleep is normal.[3,4] Nevertheless, our findings of increased percentage mobility during sleep with increased noise exposure, suggest that noise exposure may cause shallower sleep among the RNoN seamen, and shallow sleep is considered less restorative and may become detrimental if chronic.[2] Although noise exposure also had an impact on sleep efficiency among the RNoN seamen, the mean sleep efficiency (86.5%) was higher than the normal cut-off value (85%) suggesting sleep impairment.[26] Also compared to several other field studies using actigraphy on board vessels,[5,6,8] the mean sleep efficiency was relatively high. On board the research vessel sailing to Antarctica, the mean sleep efficiency among the participants ranged from 74.2% to 81.7%,[5] among fishermen a mean sleep efficiency of 78.4% have been reported,[6] and on board Swedish cargo vessels, the mean sleep efficiency was 76.4% and 74.2% depending on watch-systems.[8] Thus, the mean sleep efficiency of 86.5% indicates that RNoN seamen sleep reasonably well.
In the current study, the mean LAmax level of the noise events did not have a significant impact on any of the sleep variables. Thus, the number of noise events, as defined by a contrast of +9 dB in LAmax between adjacent 1-min intervals, rather than the LAmax level of these events, seems to be important for explaining sleep disturbance on board the RNoN vessels. The mean LAmax level of the noise events ranged from 53.2 to 92.4 dB, which is substantially higher than the threshold levels expected to evoke sleep responses, i.e., LAmax levels of 32-42 dB.[3] This may explain why the mean LAmax level of noise events did not explain variation in the sleep variables as all noise events had sufficient LAmax level to disturb sleep. The fact that the LAmax level was unrelated to sleep parameters might also be explained by the process of habituation.[27] It was somewhat surprising that noise exposure was not associated with other sleep variables such as awakenings and duration of awakenings since both have been reported to increase with higher noise exposure.[3,4] However, it has been emphasized that the actigraphs have limited ability to detect awakenings,[22] which may explain the lack of associations. The fact that noise events per hour were related to both mobility during sleep and sleep efficiency probably reflects startle responses and is in accord with studies showing that presentation of new stimuli in the sleep situation typically cause sleep impairment.[28] In the preparatory analysis, a significant correlation between equivalent noise level and age was found. This correlation is probably related to conscripts’ and enlisted personnel's cabins being situated closer to continuous noise sources such as engine rooms and above the shafts compared to higher ranking personnel. Thus, younger seamen's cabins have a higher equivalent noise levels as compared to the officer's cabins normally placed further away from such noise sources.[16]
The strength of the current study was the assessment of noise exposure both in terms of equivalent noise level and noise events. To our knowledge, this is the first study to assess the number of noise events on board vessels, and there is currently no standard for defining a noise event. However, it has been indicated that for inducing awakenings the LAmax threshold level is about 35 dB(A) at background levels of 27 dB(A), i.e., a 8 dB difference.[3] When choosing the definition used in this study (i.e., contrast of +9 dB in LAmax between adjacent 1-min intervals), both consideration of previous research and visual inspection of the noise measurements were made. A challenge was that the noise dose meters used only logged noise exposure in 1-min interval; thus, what happened in terms of variation within that minute is unknown. Moreover, the current definition required a 9 dB change in LAmax between adjacent 1-minute intervals, and a noise event occurring with a continuous change toward higher noise level may not have been registered as a noise event.
Noise exposure is merely one factor influencing sleep, and seamen are also exposed to other stressors on board vessels.[13] Although we adjusted for night versus day sleep and workload before sleep in our study, it is a limitation that we did not get sufficient information to thoroughly adjust for watch systems or shift-work schedules, which have been linked to variation in sleep in previous studies among seamen.[7,8,9] We also lacked information on the seamen's length of period at sea, which may have had an impact on the results, as studies have found that sleep may improve further into tour due to habituation to noise.[29] However, in a study of habituation of sleep to a ships noise, habituation was found to some extent in subjective sleep parameters, but no habituation was observed in sleep parameters measured by actigraphy.[18] As the current study primarily investigated instantaneous effects on sleep for single sleep periods, the impact of watch systems and shift-work may be of less importance. On board vessels at sea, there are also constant vibrations and motions caused by running engines and the sea state, which have been associated with sleep problems for seamen.[30] We did not measure vibration or motion, but data collection was primarily carried out in sheltered waters with low sea state. However, four of our measurements on board one of the coastal corvettes were compromised and excluded due to heavy vibrations. Similar problems were reported on board HSV-2 SWIFT,[10] vibrations seems to challenge the use of actigraphy, especially on board high-speed vessels.
In future studies of noise and sleep on board vessels, we would suggest repetitive monitoring of noise and sleep for longer periods to investigate variations and changes throughout a tour. To be able to better relate sleep effects such as awakenings to noise exposure, studies should also synchronize measures of noise and sleep in order to assess the relationship between these variables on a micro-level, instead of looking at the relationships at an aggregated level as in the present and former studies. As the present study merely investigates noise exposure and sleep variables for single sleep periods, one can only speculate on after or long-term effects. In future studies, measures of parameters such as daytime sleepiness, fatigue, mood, and performance should be considered to explore the possible consequences of sleep disturbance on board vessels. Future studies should also account for other important exposures such as shift-work, watch-systems, vibration, and motion. An interesting topic for future research would also be to identify individual differences in regard of the sleep-impairing effect of noise.
The current study showed that noise exposure in terms of equivalent noise level and number of noise events had a negative impact on seamen's sleep on board vessels in the RNoN. Our findings suggest that noise events should be considered when dealing with noise and sleep on board vessels. As this is one of few studies assessing noise and sleep on board vessels, more studies are needed.
Financial support and sponsorship
The Royal Norwegian Navy.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Camilla Hauge for invaluable contribution in the data collection, Kaja Irgens-Hansen and Kari Vagnes for involvement in data collection, Valborg Baste for advice concerning statistics, Gunhild Koldal for the management of the study, the RNoN and especially Hjalmar Johansen and Vilhelm Koefoed for good collaboration during the project. We would also like to show our gratitude to the seamen participating in the study.
References
- 1.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–32. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11:135–42. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Copenhagen: World Health Organization Regional Office for Europe; 2009. WHO. Night Noise Guidelines for Europe. [Google Scholar]
- 4.Pirrera S, De Valck E, Cluydts R. Nocturnal road traffic noise: A review on its assessment and consequences on sleep and health. Environ Int. 2010;36:492–8. doi: 10.1016/j.envint.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Arendt J, Middleton B, Williams P, Francis G, Luke C. Sleep and circadian phase in a ship's crew. J Biol Rhythms. 2006;21:214–21. doi: 10.1177/0748730405285278. [DOI] [PubMed] [Google Scholar]
- 6.Gander P, van den Berg M, Signal L. Sleep and sleepiness of fishermen on rotating schedules. Chronobiol Int. 2008;25:389–98. doi: 10.1080/07420520802106728. [DOI] [PubMed] [Google Scholar]
- 7.Härmä M, Partinen M, Repo R, Sorsa M, Siivonen P. Effects of 6/6 and 4/8 watch systems on sleepiness among bridge officers. Chronobiol Int. 2008;25:413–23. doi: 10.1080/07420520802106769. [DOI] [PubMed] [Google Scholar]
- 8.Lützhöft M, Dahlgren A, Kircher A, Thorslund B, Gillberg M. Fatigue at sea in Swedish shipping-a field study. Am J Ind Med. 2010;53:733–40. doi: 10.1002/ajim.20814. [DOI] [PubMed] [Google Scholar]
- 9.Kongsvik T, Størkersen K, Hansen JH. The possible impact of different watch keeping regimes at sea on sleep, fatigue and safety. In: Bérenguer C, Grall A, Guedes Soares C, editors. Advances in Safety, Reliability and Risk Management. London: CRC Press; 2011. pp. 2910–8. [Google Scholar]
- 10.Miller NL, Matsangas P, Kenney A. The role of sleep in the military: Implications for training and operational effectiveness. In: Laurence JH, Matthews MD, editors. The Oxford Handbook of Military Psychology. New York: Oxford University Press; 2012. pp. 262–81. [Google Scholar]
- 11.Southampton: Marine Accident Investigation Branch; 2004. MAIB. Bridge Watchkeeping Safety Study. [Google Scholar]
- 12.Bal E, Arslan O, Tavacioglu L. Prioritization of the causal factors of fatigue in seafarers and measurement of fatigue with the application of the lactate test. Saf Sci. 2015;72:46–54. [Google Scholar]
- 13.Oldenburg M, Jensen HJ, Latza U, Baur X. Seafaring stressors aboard merchant and passenger ships. Int J Public Health. 2009;54:96–105. doi: 10.1007/s00038-009-7067-z. [DOI] [PubMed] [Google Scholar]
- 14.Hansen JH, Holmen IM. Sleep disturbances among offshore fleet workers: A questionnaire-based survey. Int Marit Health. 2011;62:123–30. [PubMed] [Google Scholar]
- 15.Salyga J, Kušleikaite M. Factors influencing psychoemotional strain and fatigue, and relationship of these factors with health complaints at sea among Lithuanian seafarers. Medicina (Kaunas) 2011;47:675–81. [PubMed] [Google Scholar]
- 16.Sunde E, Irgens-Hansen K, Moen BE, Gjestland T, Koefoed VF, Oftedal G, et al. Noise and exposure of personnel aboard vessels in the Royal Norwegian Navy. Ann Occup Hyg. 2015;59:182–99. doi: 10.1093/annhyg/meu075. [DOI] [PubMed] [Google Scholar]
- 17.Tamura Y, Kawada T, Sasazawa Y. Effect of ship noise on sleep. J Sound Vib. 1997;205:417–25. [Google Scholar]
- 18.Tamura Y, Horiyasu T, Sano Y, Chonan K, Kawada T, Sasazawa Y, et al. Habituation of sleep to a ship's noise as determined by actigraphy and a sleep questionnaire. J Sound Vib. 2002;250:107–13. [Google Scholar]
- 19.Smith AP, Lane A, Bloor MJ, Allen PH, Burke A, Ellis N. Cardiff: Seafarers International Research Centre, Cardiff University; 2003. Fatigue offshore: Phase 2. The short sea and coastal shipping industry. [Google Scholar]
- 20.Archibald K. Monterey, CA: Naval Postgraduate School; 2005. Effects of noise, temperature, humidity, motion and light on the sleep patterns of the crew of HSV-2 SWIFT. [Google Scholar]
- 21.Smith A, Allen P, Wadsworth E. Cardiff: Centre for Occupational and Health Psychology, Cardiff University; 2006. Seafarer Fatigue: The Cardiff Research Programme. [Google Scholar]
- 22.Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med Rev. 2011;15:259–67. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Philips, Respironics. Equivalence of Activity Recordings and Derived Sleep Statistics. 2009. [Last accessed on 2015 Dec 28]. Available from: http://www.actigraphy.respironics.com/documents/AWDataEquivalenceReport_0309-g00inal.pdf .
- 24.Porkka-Heiskanen T, Zitting KM, Wigren HK. Sleep, its regulation and possible mechanisms of sleep disturbances. Acta Physiol (Oxf) 2013;208:311–28. doi: 10.1111/apha.12134. [DOI] [PubMed] [Google Scholar]
- 25.Brussels: Military Agency for Standardization; 1987. NATO. Guidelines for the Acoustical Environment in NATO Surface Ships. Stanag 4293. [Google Scholar]
- 26.Walsleben JA, Kapur VK, Newman AB, Shahar E, Bootzin RR, Rosenberg CE, et al. Sleep and reported daytime sleepiness in normal subjects: The Sleep Heart Health Study. Sleep. 2004;27:293–8. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 27.Pinsker H, Kupfermann I, Castellucci V, Kandel E. Habituation and dishabituation of the gill-withdrawal reflex in Aplysia. Science. 1970;167:1740–2. doi: 10.1126/science.167.3926.1740. [DOI] [PubMed] [Google Scholar]
- 28.Kawada T, Xin P, Kuroiwa M, Sasazawa Y, Suzuki S, Tamura Y. Habituation of sleep to road traffic noise as determined by polysomnography and an accelerometer. J Sound Vib. 2001;242:169–78. [Google Scholar]
- 29.Burke A, Ellis N, Allen P. The impact of work patterns on stress and fatigue among offshore worker populations. In: McCabe P, editor. Contemporary Ergonomics. London: Taylor & Francis; 2003. pp. 131–6. [Google Scholar]
- 30.Haward BM, Lewis CH, Griffin MJ. Motions and crew responses on an offshore oil production and storage vessel. Appl Ergon. 2009;40:904–14. doi: 10.1016/j.apergo.2009.01.001. [DOI] [PubMed] [Google Scholar]


