Abstract
BACKGROUND AND OBJECTIVES
Recent policy changes have affected access to health insurance for families in the United States. Private health insurance premiums have increased, and state Medicaid programs have cut back coverage for adults. Concurrently, the Children’s Health Insurance Program has made public insurance available to more children. We aimed to better understand how child and parent health insurance coverage patterns may have changed as a result of these policies.
METHODS
We analyzed data from the nationally representative Medical Expenditure Panel Survey, comparing cohorts from 2003 and 2008. We assessed cross-sectional and full-year coverage patterns for child/parent pairs, stratified by income. We conducted chi-square tests to assess significant differences in coverage over time.
RESULTS
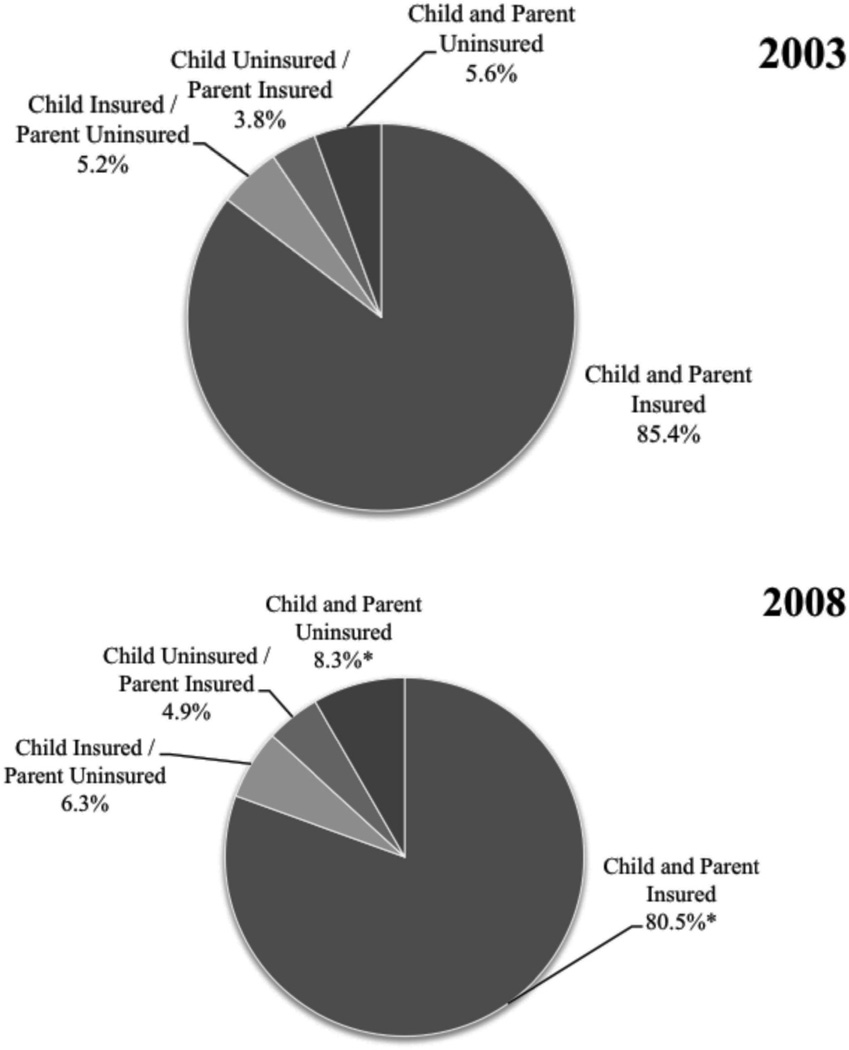
Middle-income child/parent pairs had the most significant changes in their coverage patterns. For example, those with full-year health insurance coverage significantly decreased from 85.4% in 2003 to 80.6% in 2008. There was also an increase in uninsured middle-income child/parent pairs for the full year (5.6% in 2003 to 8.3% in 2008) and an increase in pairs who had a gap in coverage (9.7% in 2003 to 13.0% in 2008).
CONCLUSIONS
The percentage of middle-income child/parent pairs who were lacking insurance, for part or all of the year, has risen, suggesting that these families may be caught between affording private coverage and being eligible for public coverage. Unless private coverage becomes more affordable, insurance instability among middle-income families may persist despite the passage of the Patient Protection and Affordable Care Act.
The current structure of the health insurance system in the United States makes it difficult for millions of families to obtain stable health insurance coverage.1–4 Rising health insurance costs have made private coverage unaffordable for some families, and cutbacks in state Medicaid programs have limited access to public coverage for others.5–7 Concurrently, expansions in the Children’s Health Insurance Program (CHIP) have made public insurance available to more children.8 As a result of these changes in affordability of and access to coverage, it is likely that family patterns of health insurance coverage have shifted in recent years.
Having health insurance is associated with better health outcomes for children.9–13 Parental health insurance coverage status impacts their children’s coverage status,1,14–16 making it essential to understand trends in coverage for children and their parents over time. Previous research has focused on shifts in coverage patterns for adults or children separately; few studies have linked children with their parents or stratified findings by income.3,17–21 For this study, we investigated changes in health insurance coverage patterns for US children and their parents between 2003 and 2008, stratified by income.
Methods
We analyzed data from the nationally representative Medical Expenditure Panel Survey-Household Component (MEPS-HC), maintained by the Agency for Healthcare Research and Quality.22 Details about the MEPS-HC are available elsewhere.22–24 We selected the years 2003 and 2008 for two reasons: (1) nationwide cost-containment measures were implemented in state Medicaid programs in 2003,7 and (2) 2008 was the most recent MEPS-HC data available at the time of this study.22
This analysis was limited to children ages 0–17 years, with responses to 1 full year of the survey (n=19,142). We linked each child with one or both parents and then constructed variables pairing parent and child health insurance status and type. We excluded children for whom no identifiable parent records could be linked (n=558) and for whom self or parental insurance information for the full year was not available (n=3), resulting in a final sample size of 18,581, weighted to a yearly average of 72 million US children.
Study Variables
We created several health insurance coverage variables to represent both cross-sectional (date of interview) and full-year insurance status. MEPS-HC assesses insurance coverage status monthly. We utilized each person’s monthly coverage status to create full-year insurance variables. Parent(s) were considered insured if at least one parent was insured. We categorized type of health insurance for the full year as any private, public only, or no coverage (uninsured). (Detailed algorithms are available from the corresponding author). To stratify by household income, we defined low income as <200% of the federal poverty level (FPL), middle income as 200%–<400% FPL, and high income as ≥400% FPL. These distinctions were based on MEPS poverty categories, which include negative or poor (less than 100% FPL), near poor (100% to less than 125% FPL), low income (125% to less than 200% FPL), middle income (200% to less than 400% FPL), and high income (greater than or equal to 400% FPL). We combined the poor, near poor, and low-income groups together to represent low income for this study as many public insurance programs and other charitable programs consider households earning less than 200% FPL eligible for free or reduced-cost services.23 The FPL for a family of four was $18,100 in 2003 and $21,200 in 2008.25,26
We identified the following demographic variables from the MEPS-HC as conceptually relevant to insurance status: child age and race/ethnicity, parent age and race/ethnicity, family composition, parent employment and education, geographic region of residence, metropolitan statistical area (MSA), child usual source of care (USC) status, parent USC status, child health status, and whether or not the child had special health care needs.23
Analysis
We assessed differences in frequency distributions for cross-sectional and full-year child/parent health insurance coverage status and coverage type using PROC CROSSTAB in SUDAAN version 10.0.1 software (Research Triangle Institute, Research Triangle Park, NC). We used sampling stratification variables and weights to account for the complex sample design of the survey. We conducted chi-square tests of association to assess significant differences over time. We considered statistical significance to be P≤.05. This study was deemed exempt by the Oregon Health & Science University Institutional Review Board.
Results
Health Insurance Status
When comparing 2003 to 2008, the cross-sectional percentage of insured middle income (200%–<400% FPL) child/parent pairs significantly decreased from 85.4% to 80.6% (P=.01); the percentage of full-year insured middle-income child/parent pairs decreased from 78.8% to 72.8% (P<.01) (see Table 1). Low-income child/parent pairs experienced nonsignificant declines, while those in the high-income group saw little change.
Table 1.
Percentage of Child/Parent Pairs Who Have Health Insurance Coverage (Any Type): Differences by Income Level Between 2003 and 2008 (Cross-Sectional and Full Year)
| Child and Parent(s) Insured in 2003 % |
Child and Parent(s) Insured in 2008 % |
|
|---|---|---|
| Cross-sectional* | ||
| Low income (<200% FPL) | 62.5 | 59.3 |
| Middle income (200%–<400% FPL)** | 85.4 | 80.6 |
| High income (≥400% FPL) | 91.2 | 91.3 |
| Full year** | ||
| Low income (<200% FPL) | 51.6 | 48.6 |
| Middle income (200%–<400% FPL)*** | 78.8 | 72.8 |
| High income (≥400% FPL) | 88.3 | 87.6 |
n=18,581
Cross-sectional assessed on day of second interview round in each year
Child and parent had full-year insurance without any gaps in coverage
Statistically significant difference between 2003 and 2008 at P<.01
Federal Poverty Level (FPL) for a family of four in 2003 was $18,100.
FPL for a family of four in 2008 was $21,200.
Cross-sectionally, there was a significant increase in the percentage of uninsured middle-income child/parent pairs (from 5.6% in 2003 to 8.3% in 2008, P=.05) (see Figure 1).
Figure 1.
Patterns of Coverage Change for Middle-income Child/Parent Pairs: Differences Between 2003 and 2008 (Cross-Sectional)
Note: Middle income = 200%–<400% of the Federal Poverty Level
* Comparison between 2003–2008 P≤.05
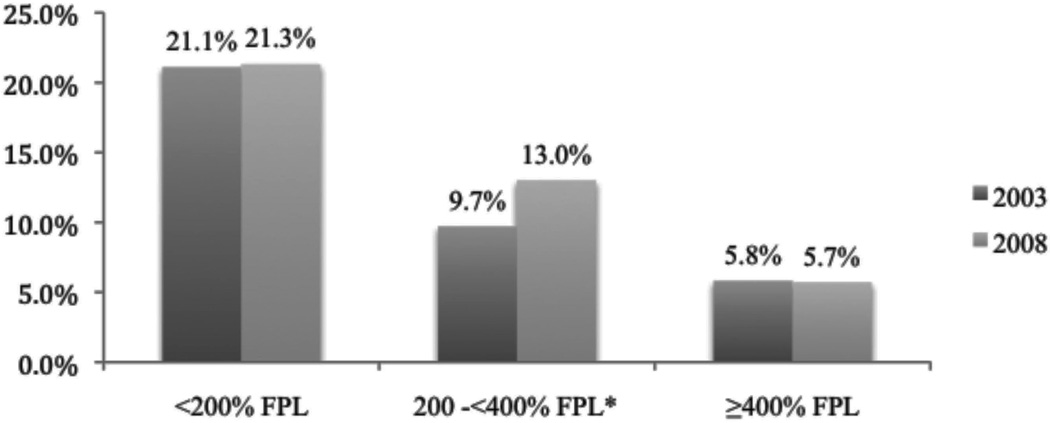
In addition, the percentage of middle-income child/parent pairs who were lacking insurance at some point during the year significantly increased from 9.7% in 2003 to 13.0% in 2008 (P=.04) (see Figure 2). No significant changes were seen for the low- or high-income groups.
Figure 2.
Percentage of Child/Parent Pairs Who Were Lacking Insurance for any Part of or for All of the Year: Differences by Income Level Between 2003 and 2008 (Full Year)
Child/parent pair were lacking insurance for any part of, or for all of the year
* P=.01
Health Insurance Type
Low- and middle-income child/parent pairs saw a significant decrease in private coverage when comparing 2003 to 2008 (Table 2). Specifically, the cross-sectional percentage of middle-income child/parent pairs with private coverage dropped from 75.7% in 2003 to 70.2% in 2008 (P=.01); full-year private coverage for both child/parent pairs decreased from 80.5% in 2003 to 76.4% in 2008 (P=.05).
Table 2.
Trends in Patterns of Health Insurance Coverage Type for Child/Parent Pairs: Differences by Income Level Between 2003 and 2008 (Cross-Sectional and Full Year)
| Low Income (<200% FPL) |
Middle Income (200% to 400% FPL) |
|||||
|---|---|---|---|---|---|---|
| 2003 | 2008 | P Value | 2003 | 2008 | P Value | |
| Unweighted n (%) | Unweighted n (%) | |||||
| Cross-sectional* | ||||||
| Child and parent private | 1,001 (24.7) | 864 (21.5) | 0.11 | 1,742 (75.7) | 1,552 (70.2) | .01 |
| Child private/parent public | # | # | N/A | # | # | N/A |
| Child public/parent private | 486 (9.1) | 418 (8.4) | .50 | 174 (6.1) | 160 (5.1) | .37 |
| Child and parent public | 1752 (28.2) | 1580 (28.8) | .77 | 121 (3.6) | 137 (5.1) | .13 |
| Full year** | ||||||
| Child and parent any private | 1244 (30.8) | 1110 (27.5) | .11 | 1,868 (80.5) | 1,701 (76.4) | .05 |
| Child any private/parent public only | # | # | N/A | # | # | N/A |
| Child public only/parent any private | 675 (12.8) | 579 (11.6) | .34 | 207 (6.9) | 204 (6.9) | .99 |
| Child and parent public only | 1927 (30.5) | 1767 (31.6) | .62 | 121 (3.3) | 121 (4.2) | .23 |
Note: Percentages are not shown for groups where either child and /or parent(s) were uninsured. P values assess for differences in the proportion of each category of child/parent insurance between 2003 and 2008 compared to all other categories combined (including the uninsured groups).
Cross-sectional assessed on day of second interview round in each year.
Child and parent had full-year insurance without gaps. If they had a mix of insurance types, we categorized them into having any private if the mix included private insurance.
Cell sizes <30; estimates not reliable
Private health insurance was defined as coverage provided by employer/union groups, non-group coverage, other group coverage, or coverage through an unknown private category that provided benefits for hospital and physician services.
Public health insurance was defined as coverage under TRICARE, Medicare, Medicaid or SCHIP, or other public hospital/physician programs.
The demographic characteristics of insured middle-income child/parent pairs remained almost the same between 2003 and 2008 with one exception: the percentage of those with parents who had less than 12 years of education dropped significantly from 5.0% to 2.9% (P=.01). Similarly, the only demographic difference among privately insured middle-income child/parent pairs was a significant change in the distribution of parental age; for example, those in this group with a parent over 45 increased from 14.2% in 2003 to 19.2% in 2008, P=.03) (Table 3).
Table 3.
Demographic Characteristics by Insurance Status for Middle-Income Child/Parent Pairs: Differences Between 2003 and 2008 (Cross-Sectional)
| Child and Parent Insured 200% to <400% FPL |
Child and Parent Private Insurance 200% to <400% FPL |
|||
|---|---|---|---|---|
| 2003 (%) | 2008 (%) | 2003 (%) | 2008 (%) | |
| Child age, in years | ||||
| 0–4 | 24.7 | 27.1 | 24.9 | 26.7 |
| 5–9 | 26.6 | 28.1 | 26.7 | 27.7 |
| 10–13 | 25.4 | 22.0 | 25.4 | 22.5 |
| 14–17 | 23.4 | 22.8 | 23.0 | 23.1 |
| Parent age, in years | * | * | ||
| < 24 | 3.4 | 2.7 | 2.7 | 1.6 |
| 25–44 | 82.0 | 78.4 | 83.1 | 79.2 |
| 45+ | 14.7 | 19.0 | 14.2 | 19.2 |
| Child race/ethnicity | ||||
| White, non-Hispanic | 69.0 | 67.5 | 72.4 | 70.7 |
| Hispanic, any race | 12.6 | 13.8 | 11.5 | 12.4 |
| Non-white, non-Hispanic | 18.4 | 18.7 | 16.1 | 16.9 |
| Parent race/ethnicity | ||||
| White, non-Hispanic | 67.5 | 67.1 | 70.7 | 69.9 |
| Hispanic, any race | 14.3 | 14.7 | 13.3 | 13.6 |
| Non-white, non-Hispanic | 18.2 | 18.3 | 15.9 | 16.6 |
| Family composition | ||||
| One parent in household | 18.5 | 16.6 | 15.8 | 14.3 |
| Two parents in household | 81.5 | 83.4 | 84.2 | 85.7 |
| Parent employment | ||||
| Employed | 98.3 | 98.0 | # | # |
| Not employed | 1.7 | 2.0 | # | # |
| Parent education | * | * | ||
| ≥ 12 years | 95.0 | 97.1 | 96.4 | 97.9 |
| < 12 years | 5.0 | 2.9 | 3.6 | 2.1 |
| Geographic residence | ||||
| Northeast | 17.2 | 16.4 | 17.5 | 16.2 |
| Midwest | 27.5 | 24.4 | 28.5 | 25.5 |
| South | 32.6 | 37.7 | 31.1 | 38.6 |
| West | 22.8 | 21.5 | 23.0 | 19.7 |
| Metropolitan Statistical Area (MSA) | ||||
| MSA | 80.7 | 81.7 | 80.8 | 81.7 |
| Non-MSA | 19.3 | 18.3 | 19.2 | 18.3 |
| Child usual source of care (USC) status | ||||
| Yes USC | 93.7 | 91.7 | 94.0 | 91.3 |
| No USC | 6.4 | 8.3 | 6.0 | 8.7 |
| Parent USC status | ||||
| Yes USC | 88.7 | 88.4 | 89.4 | 89.3 |
| No USC | 11.3 | 11.6 | 10.6 | 10.7 |
| Child health status | ||||
| Excellent/very good/good | 98.5 | 98.1 | # | # |
| Fair/poor | 1.5 | 1.9 | # | # |
| Child has special health care needs | ||||
| Yes | 18.8 | 19.5 | 17.7 | 19.0 |
| No | 81.2 | 80.5 | 82.4 | 81.0 |
FPL—Federal Poverty Level
P≤0.05;
Cell sizes <30, estimates not reliable
Race/ethnicity variables were created by combining the race and ethnicity variables.
Family composition refers to whether the child could be linked to one parent or two parents residing in the same family (it does not account for biological relationships between parent and child or the marriage status between the two parents).
Geographic information included four regional categories in the MEPS-HC, which are based on US census regions.
MSA designated place of residence as either an urban or a non-urban area.
USC was defined as whether there was a particular doctor’s office, clinic, health center, or other place that the individual usually goes to when sick or needing advice about health.
The special health care needs identifies children with activity limitations or who need or use more health care or other services than is usual for most children of the same age group.
Discussion
A smaller percentage of US middle-income child and parent pairs had health insurance coverage in 2008, as compared to 2003, while low- and high-income pairs experienced little or no change. Further, the percentage of middle-income child/parent pairs with private health insurance coverage decreased during this time period. There are likely several explanations for why patterns of private coverage changed for middle-income pairs, while low-and high-income coverage patterns remained more stable, including: (1) middle-income families are less able to afford private health insurance,27 (2) the percentage of low-income child/parent pairs with private coverage was already fairly low in 2003 so there were few families who could lose it in 2008, and (3) high-income families continue to be able to afford private insurance despite increased cost.
Unaffordable employer-sponsored insurance costs have put low and middle earners at a distinct disadvantage;27 as workers lose employer insurance options, families must look elsewhere for coverage.5 Public health insurance programs are more accessible to low-income families; however, these programs are not currently accessible to middle-income families.28 As shown in this study, the percentage of uninsured middle-income child/parent pairs has increased. It appears that these families may be caught between being able to afford private insurance and being eligible for public health insurance. Further, the significant drop in insured parent/child pairs with coverage among less educated families suggests that these families may be the most vulnerable. Interestingly, there were no other significant changes in the demographics of families with health insurance in this study, suggesting that longstanding disparities in health insurance coverage have remained constant.
The Patient Protection and Affordable Care Act (PPACA) of 2010 may reduce the number of uninsured child/parent pairs. Since it was passed, the PPACA has been responsible for improved access to health insurance coverage for about one million young adults through their parent’s health insurance, and about 30,000 have gained coverage because of the pre-existing condition insurance plan.29 However, a recent Gallup poll suggests that despite these gains, the overall number of uninsured Americans continues to climb, outpacing coverage expansions of the PPACA.30
By 2014, the PPACA will also require the creation of health insurance exchanges to allow those without insurance offered through their employers to buy it directly, Medicaid expansions to Americans making less than 133% FPL, and tax credits to help the middle class afford insurance.31 Current estimates, however, project that 8% of the population will still remain uninsured after implementation of the full PPACA, including those whose income is too high to receive a subsidy but too low to pay for coverage,32 thus the findings of this study may persist even after implementation of the full PPACA.
Limitations
Our analyses were limited by the existing data and, as with all studies that rely on self-report, response bias remains a possibility. We describe changes in health insurance coverage, but MEPS data do not provide explanations about why these changes have occurred. In Table 3, we looked for demographic differences that might explain these changes but found that nearly none had changed significantly. Thus, we concluded that controlling for demographic covariables would likely not have significantly changed the results. Lastly, this study does not account for state-level differences stemming from individual state policies, which have expanded and contracted public health insurance to the uninsured.
Conclusions
A smaller percentage of US middle-income child/parent pairs had private health insurance coverage in 2008, as compared with 2003. A larger percentage of middle-income child/parent pairs were uninsured. These families may be caught between affording private coverage and being eligible for public coverage. Unless private coverage becomes more affordable or public coverage more widely available, this problem may persist despite the passage of the PPACA.
Acknowledgments
This study was financially supported by the Agency for Healthcare Research and Quality (1 K08 HS16181) and (1 R01 HS018569), the Oregon Health & Science University Department of Family Medicine, and the Ohio State University Department of Family Medicine. The funding agencies had no involvement in the design and conduct of the study, analysis and interpretation of the data, or preparation, review, or approval of the manuscript. AHRQ collects and manages the Medical Expenditure Panel Survey.
Footnotes
This study was presented at the 2011 Agency for Healthcare Research and Quality Annual Meeting, the 2011 Annual Meeting of the North American Primary Care Research Group in Banff, Alberta, Canada, and the 2012 Society of Teachers of Family Medicine Annual Spring Conference in Seattle.
References
- 1.DeVoe JE, Krois L, Edlund C, Smith J, Carlson N. Uninsured but eligible children: are their parents insured? Recent findings from Oregon. Med Care. 2007;46(1):3–8. doi: 10.1097/MLR.0b013e31815b97ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeVoe JE, Tillotson C, Wallace L. Uninsured children with insured parents. JAMA. 2008;300(16):1904–1913. doi: 10.1001/jama.2008.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vistnes J, Schone B. Pathways to coverage: the changing roles of public and private sources. Health Aff. 2008;27(1):44–57. doi: 10.1377/hlthaff.27.1.44. [DOI] [PubMed] [Google Scholar]
- 4.Fairbrother G. Commentary on IOM report: health insurance is a family matter. Amb Pediatr. 2003;3(2):66–67. doi: 10.1367/1539-4409(2003)003<0066:coirhi>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 5.Kaiser Family Foundation and Health Research and Educational Trust. Employer health benefits: 2008 annual survey. [Accessed February 22, 2009]; http://ehbs.kff.org/pdf/7790.pdf. [Google Scholar]
- 6.Banthin JS, Cunningham P, Bernard DM. Finacial burden of health care, 2001–2004. Health Aff. 2008;27(1):188–195. doi: 10.1377/hlthaff.27.1.188. [DOI] [PubMed] [Google Scholar]
- 7.Kaiser Commission on Medicaid and the Uninsured. States respond to fiscal pressure: state Medicaid spending growth and cost containment in fiscal years 2003 and 2004. [Accessed August 3, 2011];Results from a 50-state survey. www.kff.org/medicaid/upload/States-Respond-to-Fiscal-Pressure-State-Medicaid-Spending-Growth-and-Cost-Containment.pdf. [Google Scholar]
- 8.Kenney G, Yee J. SCHIP at a crossroads: experiences to date and challenges ahead. Health Aff. 2007;26(2):356–369. doi: 10.1377/hlthaff.26.2.356. [DOI] [PubMed] [Google Scholar]
- 9.Weissman JS, Stern RS, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, consequences. Ann Intern Med. 1991;114(4):325–331. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- 10.Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Loss of health insurance and the risk for a decline in self-repoted health and physician functioning. Med Care. 2002;40:1126–1131. doi: 10.1097/00005650-200211000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110:73. doi: 10.1542/peds.110.6.e73. [DOI] [PubMed] [Google Scholar]
- 12.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338:513–519. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 13.Hadley J. Sicker and poorer: the consequences of being uninsured. Med Care Res Rev. 2003;60(2 Suppl):3S–75S. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- 14.DeVoe JE, Ray M, Graham A. Public health insurance in Oregon: underenrollment of eligible children and parental confusion about children’s enrollment status. Am J Public Health. 2011;101(5):891–898. doi: 10.2105/AJPH.2010.196345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeVoe JE, Tillotson CJ, Wallace LS. Children’s receipt of health care services and family health insurance patterns. Ann Fam Med. 2009;7(5):406–413. doi: 10.1370/afm.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeVoe J, Krois L, Edlund C, Smith J, Carlson N. Uninsurance among children whose parents are losing Medicaid coverage: results from a statewide survey of Oregon families. Health Serv Res. 2008;43(1 Part II):401–418. doi: 10.1111/j.1475-6773.2007.00764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen RA, Makuc DM, Bernstein AB, et al. Health insurance coverage trends, 1959–2007: estimates from the National Health Interview Survey. National Health Statistics Reports. 2009;(17):1–25. [PubMed] [Google Scholar]
- 18.Pizer SD, Frakt AB, Iezzoni LI. Uninsured adults with chronic conditions or disabilities: gaps in public insurance programs. Health Aff. 2009;28(6):1141–1150. doi: 10.1377/hlthaff.28.6.w1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newacheck PW, Park MJ, Brindis CD, et al. Trends in private and public health insurance for adolescents. JAMA. 2004;291(10):1231–1237. doi: 10.1001/jama.291.10.1231. [DOI] [PubMed] [Google Scholar]
- 20.Ziegenfuss JY, Davern ME. Twenty years of coverage: an enhanced current population survey—1989–2008. Health Serv Res. 2010;46(1 Pt 1):199–209. doi: 10.1111/j.1475-6773.2010.01171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holahan J. The 2007–09 recession and health insurance coverage. Health Aff. 2011;30(1):145–152. doi: 10.1377/hlthaff.2010.1003. [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. [Accessed February 22, 2009]; www.meps.ahrq.gov/mepsweb/
- 23.Agency for Healthcare Research and Quality. MEPS HC-089: 2004 full year consolidated data file. [Accessed January 10, 2008]; www.meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h89/h89doc.pdf.
- 24.Cohen J, Monheit A, Beauregard K, et al. The Medical Expenditure Panel Survey: a national health information resource. Inquiry. 1996 winter;:373–389. [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services. 2003 HHS Poverty Guidelines. Federal Register. 2003;68(7):6456–6458. [Google Scholar]
- 26.US Department of Health and Human Services. Annual update of the HHS Poverty Guidelines. Federal Register. 2008;73(15):3971–3972. [Google Scholar]
- 27.Blakely S. Employers, workers, and the future of employment-based health benefits. EBRI Issue Brief. 2010;(339):1–23. [PubMed] [Google Scholar]
- 28.Choi M, Sommers BD, McWilliams JM. Children’s health insurance and access to care during and after the CHIP expansion period. J Health Care Poor Underserved. 2011;22(2):576–589. doi: 10.1353/hpu.2011.0041. [DOI] [PubMed] [Google Scholar]
- 29.Sebelius K. ACA is helping millions: Americans experiencing better health, lower costs. Modern Healthcare. 2011;41(46):18. [PubMed] [Google Scholar]
- 30.Mendes E. More Americans uninsured in 2011. [Accessed January 25, 2012]; www.gallup.com/poll/152162/Americans-Uninsured-2011.aspx. [Google Scholar]
- 31.US Department of Health and Human Services. The health care law & you: what’s changing and when. [Accessed January 11, 2012]; www.healthcare.gov/law/timeline/index.html.
- 32.Hall MA. Getting to universal coverage with better safety-net programs for the uninsured. J Health Polit Policy Law. 2011;36(3):521–526. doi: 10.1215/03616878-1271198. [DOI] [PubMed] [Google Scholar]