Abstract
OBJECTIVE
Health insurance options are changing. Electronic health record (EHR) databases present new opportunities for providers to track the insurance coverage status of their patients. This study demonstrates the use of EHR data for this purpose.
METHODS
Using EHR data from the OCHIN Network of community health centers, we conducted a retrospective cohort study of data from children presenting to a community health center in 2010–2011 (N = 185 959). We described coverage patterns for children, used generalized estimating equation logistic regression to compare uninsured children with those with insurance, and assessed insurance status at subsequent visits.
RESULTS
At their first visit during the study period, 21% of children had no insurance. Among children uninsured at a first visit, 30% were uninsured at all subsequent visits. In multivariable analyses (including gender, age, race, ethnicity, language, income, location, and type of clinic), we observed significant differences in the characteristics of children who were uninsured as compared with those with insurance coverage. For example, compared with white, non-Hispanic children, nonwhite and/or Hispanic children had lower odds of being uninsured than having Medicaid/Medicare (adjusted odds ratio, 0.73; 95% confidence interval: 0.71–0.75) but had higher odds of being uninsured than having commercial insurance (adjusted odds ratio, 1.50; 95% confidence interval: 1.44–1.56).
CONCLUSIONS
Nearly one-third of children uninsured at their first visit remained uninsured at all subsequent visits, which suggests a need for clinics to conduct insurance surveillance and develop mechanisms to assist patients with obtaining coverage. EHRs can facilitate insurance surveillance and inform interventions aimed at helping patients obtain and retain coverage.
Keywords: electronic health records, insurance, health, children
Stable health insurance coverage facilitates access to health care.1–7 Policies implemented under the Children’s Health Insurance Program (CHIP) expanded coverage options for children in the United States,8–14 yet millions of US children remain uninsured or experience frequent gaps in coverage.15–19 Parents report barriers to accessing public insurance programs for their children, including uncertainty about a child’s coverage eligibility and status.19,20 The same barriers may be faced by other populations who become eligible for new coverage under the 2009 Patient Protection and Affordable Care Act, known as the Affordable Care Act (ACA).21 Thus, it will be important to track coverage for these populations and to identify new data sources that can provide the information needed for tracking insurance status and coverage patterns. Many persons who will be affected by CHIP and ACA insurance expansions are patients of community health centers (CHCs).22,23 In this article, we demonstrate secondary usage of electronic health records (EHRs) as an emerging data source for health insurance surveillance by CHCs and other primary care providers to track patients’ insurance coverage status and to identify patients most likely to benefit from outreach and support to obtain and maintain coverage.
We conducted a retrospective cohort study to describe the population of children served by 44 CHCs in 7 states during a 2-year period (January 1, 2010–December 31, 2011), and to assess characteristics associated with children presenting to a CHC with no insurance. We then used a nested cohort design to identify trends in insurance status over time for children with more than 1 visit during the study period.
METHODS
Data Source
In 2001, a group of Oregon CHCs partnered to form a member-based, nonprofit collaborative. This unique organization, originally called the Oregon Community Health Information Network (renamed “OCHIN” as other states joined), was created to facilitate the implementation of EHRs in CHCs. OCHIN now has CHC members in 13 states with >300 primary care clinics, and >3300 clinicians caring for >1 500 000 patients. All member clinics share OCHIN’s fully integrated EHR, which is built on EpicCare Systems software (Epic, Verona,Wisconsin), with a practice management data system (claims, billing, scheduling) and a full electronic medical record.
Using EHR data from the OCHIN, we identified a retrospective cohort of all children (ages 0–18 years) who visited an OCHIN site during the 2-year study period. For this cohort, we obtained EHR data from visits occurring during the study period, including the following: (1) self-reported demographic characteristics routinely collected on patient registration forms at most CHCs (age, gender, household income, race, ethnicity, and preferred language); (2) health center information such as location and clinical setting; and (3) patient insurance status. For patient-level variables, we used information from each individual’s first visit to a CHC in the OCHIN network during the study period. Because we had visit-level data from each visit at an OCHIN site, we were also able to represent summative total visits, per person, throughout the study period. We created the EHR research data set by using structured query language to extract all relevant data out of EpicCare’s Clarity data warehouse. We then imported this aggregate data set into Stata IC 11.0; all analyses were performed by using Stata (Stata Corp, College Station, TX).
Variables
Health insurance status was the primary dependent variable. Health insurance status was based on information from each visit and categorized as uninsured, Medicaid/Medicare, and “commercial” (non-Medicaid, non-Medicare insurance). If a child had more than 1 payer at a visit, only the primary payer was assessed. Based on the Aday and Andersen behavioral model of health care utilization,24–27 we selected the following covariates that were conceptualized as potentially influencing insurance coverage and utilization of CHC services: gender, age, race, ethnicity, language, income, rural/urban health center location, and whether the visit took place at a school-based health center (SBHC).
Study Population and Inclusion Criteria
There were 185 989 children seen within the OCHIN system during the study period. To maximize inclusion and provide reliable measures of association, our criteria excluded as few children as possible. We excluded 14 children who had >100 visits recorded, another 14 with missing information on gender, and 2 with missing information on health center location. In total, we excluded only 30 children (0.2%) from our analyses (remaining study population n = 185 959 children). If covariates were missing data for >1% of the population (race/ethnicity, language, and income), we included a “missing data” category in the multivariable analyses.
Analyses
We described characteristics for all children in the study population and assessed participant-specific data from each child’s first visit within the OCHIN system during the study period. We evaluated the distribution and descriptive statistics of the number of CHC visits made by children in the study population during the study period. We analyzed the relationship between insurance status and the covariates of interest by using univariable and multivariable generalized estimating equation logistic regression models to account for the total number of visits nested in the 185 959 children. An exchangeable correlation structure was assumed where visits were clustered within subjects and subjects within clinics. A robust sandwich estimator was applied to account for possible misspecification of the correlation structure. Finally, we examined changes in children’s insurance over time by using graphical methods. This study was approved by the institutional review board at our academic institution.
RESULTS
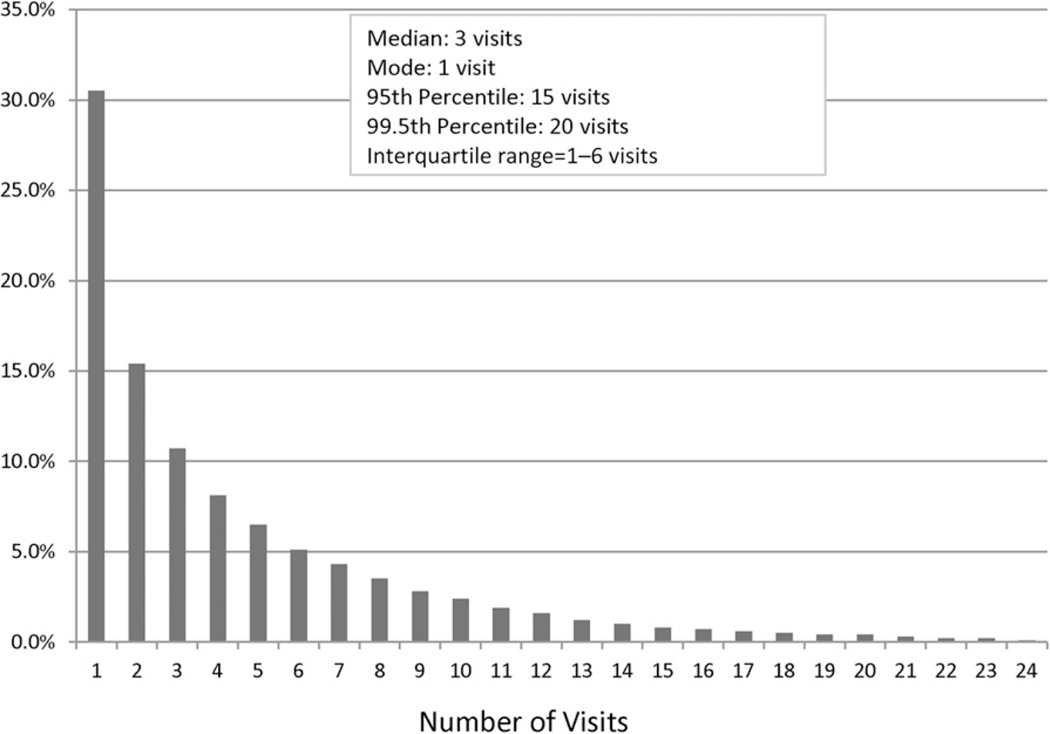
Table 1 illustrates demographic information for the 185 959 children in the study population, based on data collected at each child’s first visit to a health center in the OCHIN Network in the 2-year study period. Children were evenly distributed across age strata. Approximately 71% identified as white, 41% identified as Hispanic, and 31% identified Spanish as their primary language. Over half had household incomes below the federal poverty level. Over three-fourths (78%) were seen in urban areas. Most visits were in community primary care clinics (88%), as compared with SBHCs (12%). More visits occurred among children who were <5 years old, Hispanic, from non-English speaking households, and receiving Medicaid (data not shown). During the 2-year study period, the population had a total of 880 268 visits. The study cohort of children had a median of 3 visits and an interquartile range of 1 to 6 with a negative logarithmic pattern of distribution (Fig 1). Most children (95%) had between 1 and 15 visits over the 2-year period.
TABLE 1.
Characteristics of Children at Their First Visit to a CHC in the OCHIN Network During the Study Period (January 1, 2010–December 31, 2011)
| No. (n = 185 959) | Percentage | |
|---|---|---|
| Gender | ||
| Boy | 90 227 | 48.52 |
| Girl | 95 732 | 51.48 |
| Age | ||
| <1 | 24 593 | 13.22 |
| 1–4 | 40 426 | 21.74 |
| 5–9 | 39 690 | 21.34 |
| 10–14 | 41 412 | 22.27 |
| 15–18 | 39 838 | 21.42 |
| Race | ||
| White | 132 778 | 71.40 |
| Black/African American | 12 358 | 6.65 |
| Asian/Pacific Islander/Hawaiian Native | 6554 | 3.52 |
| Native American/Alaska Native | 1548 | 0.83 |
| More than 1 race | 2644 | 1.42 |
| Missing | 30 077 | 16.17 |
| Ethnicity | ||
| Hispanic | 76 871 | 41.34 |
| Non-Hispanic | 108 708 | 58.46 |
| Missing | 380 | 0.20 |
| Language | ||
| English | 108 807 | 58.51 |
| Spanish | 56 721 | 30.50 |
| Other | 7008 | 3.77 |
| Missing | 13 423 | 7.22 |
| Income | ||
| <100% federal poverty level | 96 015 | 51.63 |
| 101%–150% federal poverty level | 14 074 | 7.57 |
| 151%–200% federal poverty level | 5592 | 3.01 |
| >200% federal poverty level | 16 214 | 8.72 |
| Missing | 54 064 | 29.07 |
| Clinic type | ||
| School-based health center | 22 767 | 12.24 |
| Primary care clinic | 163 192 | 87.76 |
| Health center location | ||
| Rural | 39 993 | 21.51 |
| Urban | 145 966 | 78.49 |
| Insurance status | ||
| Uninsured | 38 726 | 20.83 |
| Medicaid/Medicare | 124 113 | 66.74 |
| Commercial | 23 120 | 12.43 |
FIGURE 1.
Number of visits, per child, to a CHC clinic in the OCHIN Network during the study period (January 1, 2010–December 31, 2011). Total number of visits for study population = 880 268.
As shown in Table 2, uninsured children seen in this network of CHCs were demographically different from children with Medicaid/Medicare and commercial insurance. An estimated 19% of 0 to 14 year olds were uninsured; 29% of children aged 15 to 18 years of age were uninsured. Approximately 18% nonwhite and/or Hispanic children were uninsured, compared with 24% of white, non-Hispanic children; and 17% of children who spoke a language other than English were uninsured, compared with 20% who spoke English.
TABLE 2.
Characteristics of Being Uninsured, Having Medicaid/Medicare, or Commercial Insurance at First Visit for Children Seen at a CHC in the OCHIN Network (January 1, 2010–December 31, 2011)
| Covariates | Characteristics at First Visit, % | ||
|---|---|---|---|
| Uninsured, n = 38 726 |
Medicaid/Medicare, n = 124 113 |
Commercial, n = 23 120 |
|
| Gender | |||
| Boy | 20.56 | 67.31 | 12.13 |
| Girl | 21.07 | 66.21 | 12.72 |
| Age, y | |||
| 0–14 | 18.60 | 70.54 | 10.86 |
| 15–18 | 28.98 | 52.80 | 18.22 |
| Race/ethnicity | |||
| White, Non-Hispanic | 24.24 | 55.50 | 20.25 |
| Nonwhite and/or Hispanic | 17.90 | 75.91 | 6.18 |
| Missing | 23.09 | 63.83 | 13.08 |
| Language | |||
| English | 19.94 | 63.63 | 16.44 |
| Other than English | 16.50 | 79.15 | 4.35 |
| Missing | 48.54 | 33.08 | 18.39 |
| Income | |||
| >100% federal poverty level | 22.27 | 55.44 | 22.30 |
| At or below 100% federal poverty level | 24.27 | 67.91 | 7.82 |
| Missing | 13.74 | 72.17 | 14.09 |
| Location | |||
| Urban | 22.19 | 70.37 | 7.44 |
| Rural | 15.85 | 53.49 | 30.66 |
| Clinic type | |||
| Primary care clinic | 17.36 | 71.56 | 11.07 |
| School-based health center | 45.64 | 32.19 | 22.17 |
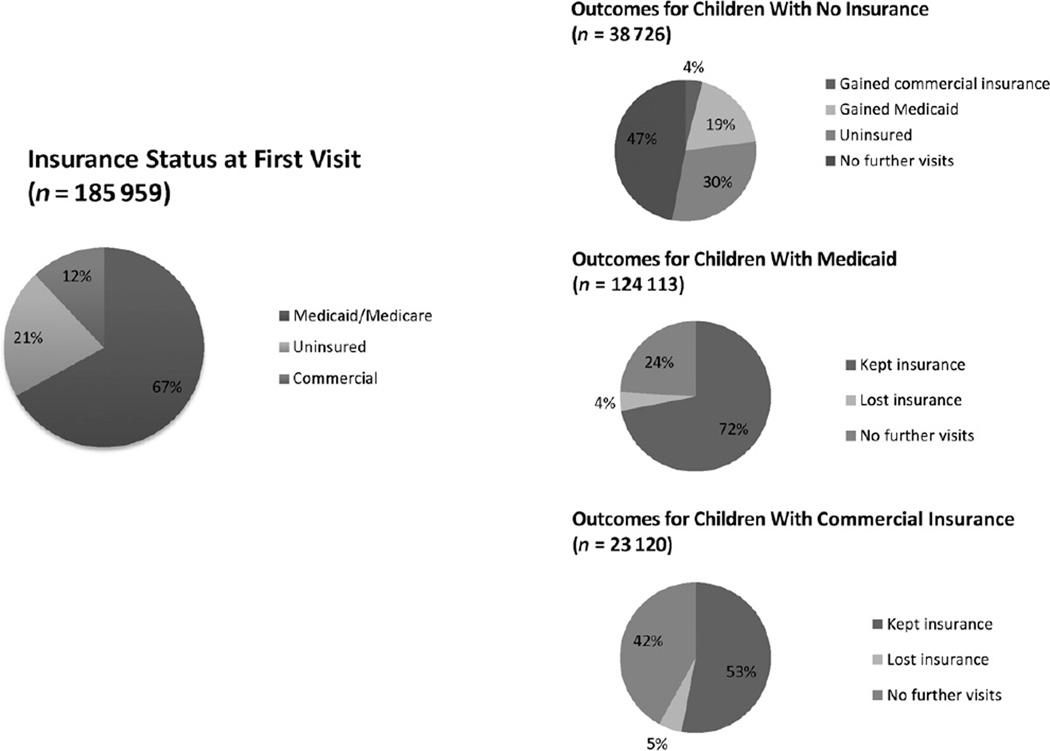
At their first visit, 21% of children were uninsured, 12% had commercial insurance, and 67% had Medicaid (Table 1, Fig 2). Of the 38 726 children with no insurance at their first visit, 30% were uninsured at all subsequent visits during the study period, 19% gained Medicaid for at least 1 subsequent visit, 4% gained commercial insurance for at least 1 subsequent visit, and 47% had no further visits within the OCHIN system. Of the 124 113 children with Medicaid at their first visit, 72% had insurance (any type) for every subsequent visit, 4% were uninsured for at least 1 subsequent visit, and 24% had no further visits within the OCHIN system. Of the 23 120 children with commercial insurance at their first visit, 53% had insurance (any type) for every subsequent visit, 5% were uninsured at a subsequent visit, and 42% had no further visits within the OCHIN system (Fig 2).
FIGURE 2.
Longitudinal assessment of insurance status over time, among children seen in CHCs in the OCHIN Network.
In multivariable analyses (including gender, age, race, ethnicity, language, income, location, and type of clinic), we observed significant differences in the characteristics of children who were uninsured as compared with those with insurance coverage (Table 3). Compared with younger kids, children 15 to 18 years of age had higher odds of being uninsured than having Medicaid/Medicare coverage (adjusted odds ratio [aOR], 1.87; 95% confidence interval [CI]: 1.82–1.92), but they had lower odds of being uninsured than having commercial coverage (aOR, 0.81; 95% CI: 0.78–0.84). Compared with white/non-Hispanic children, those who identified as nonwhite and/or Hispanic had lower odds of being uninsured than having Medicaid/Medicare coverage (aOR, 0.73; 95% CI: 0.71–0.75), but they had higher odds of being uninsured than having commercial insurance (aOR, 1.50; 95% CI: 1.44–1.56). Compared with children from urban areas, those from rural areas had lower odds of being uninsured than having either Medicaid/Medicare coverage (aOR, 0.89; 95% CI: 0.87–0.92) or commercial insurance (aOR, 0.22; 95% CI: 0.21–0.23). Compared with children seen at non-SBHCs, children seen at SBHCs had higher odds of being uninsured than having either Medicaid/Medicare (aOR, 3.39; 95% CI: 3.28–3.50) or commercial insurance (aOR, 1.06; 95% CI: 1.01–1.10).
TABLE 3.
Factors Associated With Being Uninsured Compared With Medicaid/Medicare and Commercial Insurance, Among Children Seen at a CHC in the OCHIN Network (January 1, 2010–December 31, 2011)
| Covariates | Medicaid/Medicare | Commercial | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted Odds of Being Uninsured |
P | Adjusted Odds of Being Uninsured |
P | Unadjusted Odds of Being Uninsured |
P | Adjusted Odds of Being Uninsured |
P | |
| Gender | ||||||||
| Boy | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| Girl | 1.07 (1.05–1.09) | <.001 | 0.98 (0.96–1.00) | .073 | 0.97 (0.94–1.00) | .088 | 0.98 (0.95–1.01) | .201 |
| Age, y | ||||||||
| 0–14 | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| 15–18 | 2.21 (2.16–2.26) | <.001 | 1.87 (1.82–1.92) | <.001 | 0.82 (0.79–0.84) | <.001 | 0.81 (0.78–0.84) | <.001 |
| Race/ethnicity | ||||||||
| White, Non-Hispanic | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| Nonwhite and/or Hispanic | 0.57 (0.55–0.58) | <.001 | 0.73 (0.71–0.75) | <.001 | 3.00 (2.90–3.09) | <.001 | 1.50 (1.44–1.56) | <.001 |
| Missing | 0.83 (0.79–0.87) | <.001 | 0.84 (0.80–0.89) | <.001 | 1.54 (1.44–1.65) | <.001 | 1.19 (1.11–1.28) | <.001 |
| Language | ||||||||
| English | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| Other than English | 0.66 (0.65–0.68) | <.001 | 0.96 (0.93–0.99) | .003 | 3.75 (3.61–3.90) | <.001 | 1.87 (1.78–1.96) | <.001 |
| Missing | 4.37 (4.20–4.55) | <.001 | 4.04 (3.86–4.22) | <.001 | 1.94 (1.85–2.04) | <.001 | 1.22 (1.16–1.28) | <.001 |
| Income | ||||||||
| >100% federal poverty level | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| At or below 100% federal poverty level | 0.94 (0.92–0.96) | <.001 | 0.87 (0.85–0.89) | <.001 | 1.60 (1.55–1.66) | <.001 | 1.62 (1.56–1.68) | <.001 |
| Missing | 0.69 (0.67–0.71) | <.001 | 0.84 (0.82–0.86) | <.001 | 1.06 (1.02–1.10) | .002 | 1.08 (1.04–1.12) | <.001 |
| Location | ||||||||
| Urban | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| Rural | 0.93 (0.90–0.95) | <.001 | 0.89 (0.87 –0.92) | <.001 | 0.16 (0.16–0.17) | <.001 | 0.22 (0.21–0.23) | <.001 |
| Clinic type | ||||||||
| Primary care clinic | 1.00 | — | 1.00 | — | 1.00 | — | 1.00 | — |
| School-based health center | 3.91 (3.80–4.04) | <.001 | 3.39 (3.28–3.50) | <.001 | 1.23 (1.19–1.29) | <.001 | 1.06 (1.01–1.10) | .011 |
Adjusted odds ratios are based on multivariable generalized estimating equation logistic regression models accounting for visits nested in children and children nested in clinics. Multivariable models were adjusted for gender, age, race, ethnicity, language, income, rural/urban health center location, and clinic type.
DISCUSSION
Health insurance status facilitates or hinders access to care for patients. This study demonstrates how health care systems can use their EHR data to better understand insurance coverage patterns among their patient populations. Certain patient characteristics were significantly associated with whether a child had insurance coverage at a CHC visit. Such information can help CHCs and other clinics providing health care to vulnerable populations better focus their insurance outreach efforts on patients most at risk for uninsurance. Conducting this type of surveillance will become increasingly important as insurance coverage options expand with health care reform legislation, such as the CHIP and the ACA. Further, the Health Information Technology for Economic and Clinical Health Act, which incentivizes increased adoption and use of EHRs in health care systems across the country, will increase the impetus for CHCs to conduct this type of surveillance.28
In this study population, several patient characteristics were significantly associated with being uninsured, as compared with having Medicaid/Medicare coverage or commercial insurance, at a given CHC visit. Some of our findings confirm previous research (eg, the higher odds of being uninsured versus publicly insured at a visit among children aged 15 to 18 years, compared with children <15 years).29 Other findings reported here differed from previous reports; for example, we found racial and ethnic minorities had lower odds of being uninsured at a visit than being publicly insured.30,31 This may be due to CHC’s outreach efforts to get minority children public coverage, or because some populations were more likely to access health care services despite being uninsured. Children seeking care in SBHCs also had higher odds of being uninsured than being insured by private or public coverage, compared with those seeking care in other settings. This may reflect the fact that SBHCs provide critical access to uninsured kids, or in some cases, because an insured child or adolescent is considered uninsured for an SBHC visit to maintain confidentiality.
The differences in the strength and direction of associations with being uninsured compared with having public versus commercial coverage highlight the benefits of public health insurance programs. This might suggest that public insurance programs help reduce health insurance disparities for racial/ethnic minorities and low-income families. In contrast, these disparities persist in private programs.29
Policy and Practice Implications
As the first study of this scale, this article demonstrates a novel methodology: using EHR data to conduct health insurance surveillance in CHCs. These methods could be used in primary care clinics to inform system-level interventions seeking to facilitate health insurance enrollment and retention for patients, especially those who become eligible for new insurance programs through the ACA. These methods could also be used by policy makers wishing to partner with CHCs and other health care systems to better understand patterns of insurance among certain populations or geographic communities. Importantly, our longitudinal assessment of children over a 2-year time period demonstrates a methodology for using EHR data to track how a patient’s insurance status changes (or does not change) over time. Notably, we found that nearly one-third of the children uninsured at their first visit remained uninsured at all subsequent visits. This speaks to the need for clinics to conduct insurance surveillance and develop mechanisms to intervene and assist patients with obtaining coverage that may be available to them.
This article also demonstrates the need to develop better systems for capturing the data needed for conducting such analyses in the future. For example, we were missing information on race/ethnicity, language, and/or income for a moderate percentage of the children in the study population (7%–29%); even without complete data, we demonstrated that these demographic characteristics are associated with different patterns of insurance coverage. Further, these social determinants of health have been reported in multiple studies to be associated with patients’ ability to access health care services, comprehend health care advice, and improve health status and outcomes.32–35 Thus, it is imperative that information on patients’ social determinants of health be included in EHR data. This could be accomplished through policies requiring that EHRs facilitate the collection of these data, and that health care systems develop workflows to collect related data.
Limitations
The method for monitoring insurance status employed here requires regular health care visits. We may have under-estimated the percentage of patients without health insurance, as it is likely that some uninsured children in the communities served by these CHCs did not come in for a visit during the study period. Further, children insured at a first visit may not have returned to the clinics if they lost coverage subsequent to the first visit. We also acknowledge the potential for misclassification of insurance status, especially in settings where there may be concerns about confidentiality (eg, SBHCs). We used missing data categories in our statistical analyses to minimize exclusions, which may have limited our understanding of the true relationship between the study covariates and their effect on insurance outcomes. For example, some of the missing demographic categories were associated with higher or lower odds of being uninsured (Table 2). Imputation methods were considered36 to address this “missingness”; however, the use of such methods with EHR data needs further development and evaluation. Finally, our EHR data set did not allow for identification of siblings, so we could not account for clustering within families. We did, however, adjust for number of visits and clinic variation in our multivariable analyses to account for the fact that visits were clustered within subjects and subjects within clinics.
Conclusions
EHRs provide new opportunities for identifying uninsured populations and tracking insurance coverage in populations at risk for discontinuous coverage. EHRs can facilitate insurance surveillance and inform clinic-based interventions aimed at helping patients obtain and retain insurance coverage.
WHAT’S KNOWN ON THIS SUBJECT
Stable health insurance coverage facilitates access to health care. Despite expanded coverage options for children, parents report barriers to accessing insurance programs for their children, including uncertainty about a child’s coverage status and eligibility.
WHAT THIS STUDY ADDS
Electronic health records can be used as an emerging data source for conducting health insurance surveillance to track trends in patients’ insurance coverage status, and to identify patients who may benefit from outreach and support to obtain and maintain coverage.
Acknowledgments
FUNDING: Supported by the Agency for Healthcare Research and Quality (AHRQ) (1 R01 HS018569), the Patient-Centered Outcomes Research Institute (PCORI), and the Oregon Health & Science University, Department of Family Medicine.
We thank OCHIN, Inc, and all clinics in the network for participating in this research.
ABBREVIATIONS
- aOR
adjusted odds ratio
- ACA
Affordable Care Act
- CHC
community health center
- CHIP
Children’s Health Insurance Program
- CI
confidence interval
- EHR
electronic health record
- SBHC
school-based health center
Footnotes
Dr Hatch conducted all analyses and wrote the first draft; Ms Angier assisted with analysis planning and contributed substantial edits; Dr Marino oversaw the statistical analyses and contributed substantial edits; Drs Heintzman and Nelson contributed substantial edits; Dr Gold helped conceive of the study and contributed substantial edits; Ms Vakarcs pulled the data set from the electronic health record; Dr DeVoe conceived of the study, assisted with analysis planning, and contributed substantial edits; and all authors approved the final manuscript as submitted.
The funding agencies had no involvement in the preparation, review, or approval of the article.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
- 1.Federico SG, Steiner JF, Beaty B, Crane L, Kempe A. Disruptions in insurance coverage: patterns and relationship to health care access, unmet need, and utilization before enrollment in the State Children’s Health Insurance Program. Pediatrics. 2007;120(4) doi: 10.1542/peds.2006-3094. Available at: www.pediatrics.org/cgi/content/full/120/4/e1009. [DOI] [PubMed] [Google Scholar]
- 2.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027–1037. doi: 10.1542/peds.2012-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110(6) doi: 10.1542/peds.110.6.e73. Available at: www.pediatrics.org/cgi/content/full/110/6/e73. [DOI] [PubMed] [Google Scholar]
- 4.Cassedy A, Fairbrother G, Newacheck PW. The impact of insurance instability on children’s access, utilization, and satisfaction with health care. Ambul Pediatr. 2008;8(5):321–328. doi: 10.1016/j.ambp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman C, Paradise J. Health insurance and access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–160. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 6.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 7.DeVoe JE, Ray M, Krois L, Carlson MJ. Uncertain health insurance coverage and unmet children’s health care needs. Fam Med. 2010;42(2):121–132. [PMC free article] [PubMed] [Google Scholar]
- 8.111th Congress. Compilation of Patient Protection and Affordable Care Act. [Accessed December 16, 2011]; Available at: http://docs.house.gov/energycommerce/ppacacon.pdf.
- 9.US Department of Health and Human Services. [Accessed October 11, 2012];SCHIP evaluation. 2001 Available at: http://aspe.hhs.gov/health/schip/pl105-33.htm.
- 10.Fairbrother G, Dutton MJ, Bachrach D, Newell K-A, Boozang P, Cooper R. Costs of enrolling children in Medicaid and SCHIP. Health Aff (Millwood) 2004;23(1):237–243. doi: 10.1377/hlthaff.23.1.237. [DOI] [PubMed] [Google Scholar]
- 11.Sommers AS, Dubay L, Blumberg LJ, Blavin FE, Czajka JL. Dynamics in Medicaid and SCHIP eligibility among children in SCHIP’s early years: implications for reauthorization. Health Aff (Millwood) 2007;26(5):w598–w607. doi: 10.1377/hlthaff.26.5.w598. [DOI] [PubMed] [Google Scholar]
- 12.Musumeci M. Implementing the ACA’s Medicaid-Related Health Reform Provisions After the Supreme Court’s Decision. Washington, DC: The Henry J. Kaiser Family Foundation; 2012. [Google Scholar]
- 13.Cuttler L, Kenney GM. State Children’s Health Insurance Program and Pediatrics: background, policy challenges, and role in child health care delivery. Arch Pediatr Adolesc Med. 2007;161(7):630–633. doi: 10.1001/archpedi.161.7.630. [DOI] [PubMed] [Google Scholar]
- 14.Kaiser Commission on Medicaid and the Uninsured. [Accessed January 14, 2011];Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA) 2009 Available at: www.kff.org/medicaid/upload/7863.pdf. [Google Scholar]
- 15.DeVoe JE, Graham A, Krois L, Smith J, Fairbrother GL. “Mind the Gap” in children’s health insurance coverage: does the length of a child’s coverage gap matter? Ambul Pediatr. 2008;8(2):129–134. doi: 10.1016/j.ambp.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Short PF, Graefe DR, Schoen C. Churn, Churn, Churn: How Instability of Health Insurance Shapes America’s Uninsured Problem. Washington, DC: The Commonwealth Fund; 2003. [PubMed] [Google Scholar]
- 17.Fairbrother G, Jain A, Park HL, Massoudi MS, Haidery A, Gray BH. Churning in Medicaid managed care and its effect on accountability. J Health Care Poor Underserved. 2004;15(1):30–41. doi: 10.1353/hpu.2004.0003. [DOI] [PubMed] [Google Scholar]
- 18.DeVoe JE, Krois L, Edlund C, Smith J, Carlson NE. Uninsured but eligible children: are their parents insured? Recent findings from Oregon. Med Care. 2008;46(1):3–8. doi: 10.1097/MLR.0b013e31815b97ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeVoe JE, Ray M, Graham A. Public health insurance in Oregon: underenrollment of eligible children and parental confusion about children’s enrollment status. Am J Public Health. 2011;101(5):891–898. doi: 10.2105/AJPH.2010.196345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;5(6):511–518. doi: 10.1370/afm.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collins SR, Robertson R, Garber T, Doty MM. Gaps in Health Insurance: Why So Many Americans Experience Breaks in Coverage and How the Affordable Care Act Will Help: Findings From the Commonwealth Fund Health Insurance Tracking Survey of US Adults, 2011. Washington, DC: The Commonwealth Fund; 2012. [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services. [Accessed July 20, 2012];Community health centers and the Affordable Care Act in 2011: increasing access to affordable, cost effective, high quality care. 2011 Available at: www.healthcare.gov/news/factsheets/2011/08/communityhealthcenters08092011a.html.
- 23.Morgan D. Health Centers for Poor, Uninsured See Ranks Swell. Washington, DC: The White House; 2012. [Google Scholar]
- 24.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen R, Aday LA. Access to medical care in the U.S.: realized and potential. Med Care. 1978;16(7):533–546. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18(1):49–74. [PMC free article] [PubMed] [Google Scholar]
- 27.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 28.111th Congress. American Recovery and Reinvestment Act of 2009. [Accessed October 31, 2012];2009 Available at: www.gpo.gov/fdsys/pkg/PLAW-111publ5/pdf/PLAW-111publ5.pdf.
- 29.DeNavas C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2010. Washington, DC: US Census Bureau; 2011. [Google Scholar]
- 30.Shone LP, Dick AW, Brach C, et al. The role of race and ethnicity in the State Children’s Health Insurance Program (SCHIP) in four states: are there baseline disparities, and what do they mean for SCHIP? Pediatrics. 2003;112(6 pt 2) Available at: www.pediatrics.org/cgi/content/full/112/6/e521. [PubMed] [Google Scholar]
- 31.Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2) doi: 10.1542/peds.2004-1474. Available at: www.pediatrics.org/cgi/content/full/115/2/e183. [DOI] [PubMed] [Google Scholar]
- 32.Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh GK, Yu SM. Infant mortality in the United States: trends, differentials, and projections, 1950 through 2010. Am J Public Health. 1995;85(7):957–964. doi: 10.2105/ajph.85.7.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85(7):949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329(2):103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 36.Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]