Abstract
Background and Objectives
The State Children’s Health Insurance Program (SCHIP) has improved insurance coverage rates. However, children’s enrollment status in SCHIP frequently changes, which can leave families with uncertainty about their children’s coverage status. We examined whether insurance uncertainty was associated with unmet health care needs.
Methods
We compared self-reported survey data from 2,681 low-income Oregon families to state administrative data and identified children with uncertain coverage. We conducted cross-sectional multivariate analyses using a series of logistic regression models to test the association between uncertain coverage and unmet health care needs.
Results
The health insurance status for 13.2% of children was uncertain. After adjustments, children in this uncertain “gray zone” had higher odds of reporting unmet medical (odds ratio [OR] =1.73; 95% confidence interval [CI]=1.07, 2.79), dental (OR=2.41; 95% CI=1.63, 3.56), prescription (OR=1.64, 95% CI=1.08, 2,48), and counseling needs (OR=3.52; 95% CI=1.56, 7.98), when compared with publicly insured children whose parents were certain about their enrollment status.
Conclusions
Uncertain children’s insurance coverage was associated with higher rates of unmet health care needs. Clinicians and educators can play a role in keeping patients out of insurance gray zones by (1) developing practice interventions to assist families in confirming enrollment and maintaining coverage and (2) advocating for policy changes that minimize insurance enrollment and retention barriers.
As the cost of private health insurance outpaces the earnings of American families,1 millions of families now rely on Medicaid and the State Children’s Health Insurance Program (SCHIP) to provide health insurance for their children.2-4 In fact, at least 40% of children in the United States now depend on Medicaid or SCHIP for their coverage, and this rate will likely increase with rising unemployment rates.5-7 Despite expansions in public insurance programs, however, approximately 9 million children are without health insurance at any point in time and nearly double that rate when accounting for children with coverage gaps at some point during the year.8 Children from low-income families are four to five times more likely to experience a lapse in coverage than the children of high earners,3,8-11 and children are much more likely than adults to have repeated uninsured episodes.12,13
Uninsured children are less likely to receive recommended primary care services and more likely to experience delays in the care they do receive. Thus, recent policies have focused on public insurance expansions to increase children’s coverage.7, 14-26 Frequent and cumbersome SCHIP reenrollment processes, however, often create confusion about the enrollment status of eligible children,27 contributing to uncertainty about coverage status or what could be considered a “gray zone” phenomenon. The disadvantages of being uninsured are well-established; less is known about the gray zones of uncertainty—being unaware or misinformed about ones’ current insurance coverage status.
We identified a group of low-income children in Oregon whose parents were uncertain or unaware of their child’s coverage status and examined how this uncertainty was associated with unmet needs. By linking two state databases with household survey data, we found a significant percentage of parents who understood their child’s coverage status to be different from what was reported by the state. Some parents believed their children to be enrolled in public insurance, but the state had no record of enrollment. In other cases, the state showed current enrollment, but the parents reported their children were uninsured. To examine the implications of parental uncertainty about their child’s insurance status among a sample of low-income families, we had two main objectives: (1) to identify factors associated with higher odds of a parent being unaware or uncertain about their child’s insurance status and (2) to determine if children with uncertain coverage had higher odds of experiencing unmet health care needs as compared to publicly insured children with more certain insurance coverage.
Methods
Study Population
We identified all families enrolled in Oregon’s food stamp program in early 2005. At that time, children’s eligibility requirements for food stamps and the Oregon Health Plan (OHP) were essentially the same, including a household income less than 185% of the federal poverty level (FPL) and US citizenship. These two public programs, however, had different applications and enrollment procedures. For the purposes of this study, Oregon children receiving food stamps were presumed eligible for publicly funded health insurance.
Subject Selection
From a total of 84,087 food-stamp households with at least one child over age 1 year, we selected a representative sample of 10,175. Infants under 1 year of age had different insurance eligibility requirements and so we did not include them.
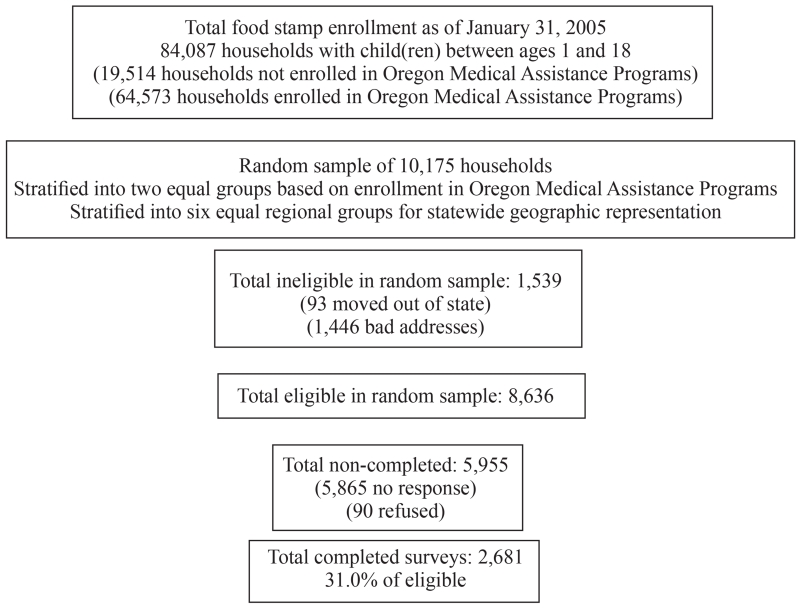
Our sample was selected using a three-step process. Appendix 1 shows a flow chart illustrating sample selection.
First, we cross-referenced state databases to find food stamp families without children enrolled in OHP (approximately 23%). To confirm that children were not merely in the OHP reenrollment process, we considered only those with no record of enrollment in the OHP for 60 days; state experts reported that a health insurance reenrollment window rarely exceeds 45 days. Second, we selected a random, stratified sample of 10,175 households. The sample was divided evenly between families with no children enrolled in OHP and families with at least one OHP-enrolled child. We used the survey selection procedure in SAS 9.1 and over-sampling techniques, aided by PASS software for adequate power calculations, to select a stratified, random sample. Third, we randomly selected a focal child from each household. In the survey described below, we provided instructions with the child’s name in multiple locations throughout the letter and on the survey to direct parents to only provide information about the one child.
Among this sample of 10,175 households, 8,637 were ultimately deemed eligible to participate in a statewide survey (we excluded families who had moved out of state and those whose surveys were returned with no current forwarding address). We received 2,681 completed surveys, for a response rate of approximately 31%. More details about the survey sample have been published elsewhere.28
Comparison of Respondents to Eligible Survey Population
We directly compared respondents to the total eligible survey population, confirming similar characteristics between these two groups, and Appendix 2 shows a comparison of respondents and nonrespondents. We observed slight differences only by geographic region, race, and whether or not the child was enrolled in OHP, so we made statistical adjustments to account for potential nonresponse bias.29,30 We created a weighting variable in a two-step sequence of adjustments. We weighted households back to the original population by assigning base weights depending on the probability of original selection. In a second weighting step, which used a raking ratio estimation process, we multiplied the individual base weights by a nonresponse adjustment factor derived from the difference in response rates by OHP enrollment status, region, and race/ethnicity. This paper reports results weighted back to the overall study population of 84,087 households in the food stamp program.
Statewide Survey
We partnered with state policymakers to design a survey instrument that asked low-income Oregon parents about the focal child’s insurance status and access to health care services during the previous year. Some questions were adapted from validated national surveys,31-34 and others were written by our team to ensure relevance to current state initiatives. We conducted cognitive interviews with six low-income parents and made adjustments based on their insights. Surveys were translated into Spanish and Russian (the two most common non-English languages spoken among this population) and then independently back translated to ensure fidelity of translation. We then conducted cognitive testing with two native Spanish speakers and one native Russian speaker to further refine these surveys.
The instrument was a self-report, mail-return survey written at a fifth-grade reading level. We used a four-wave mailing methodology (two surveys and two reminder postcards). Telephone follow-up was not financially feasible. The study was approved by the Oregon Health and Science University Institutional Review Board.
Variables and Analysis
Unmet Health Care Needs Variables
We measured the following outcome variables: unmet medical needs, unmet prescription needs, skipped medication doses, no doctor visits, delayed urgent care, and reports of big problems obtaining necessary dental care, specialty care, and counseling (Table 1).
Table 1.
Outcome Variables Pertaining to Unmet Health Care Needs for Children
| Unmet Health Care Needs Variable | Corresponding Survey Question(s) |
|---|---|
| Unmet medical need | In the last 12 months, was there any time when YOUR CHILD needed medical care but did NOT get it? (yes/ no) |
| Unmet prescription need | In the last 12 months, was there ever a time YOUR CHILD needed prescription medicines, but you could NOT afford to fill the prescription? (DO NOT count free samples as a filled prescription.) (yes/no) |
| Missed medication doses | In the last 12 months, was there ever a time YOUR CHILD had to skip doses or take less medication because you couldn’t afford the medicine? (yes/no) |
| No doctor visits | In the last 12 months, how many times did you take YOUR CHILD to a doctor’s office or clinic for care? (DO NOT include emergency room or hospital visits. Your best estimate is fine.) (continuous variable, dichotomized as yes doctor visits/no doctor visits) |
| Big problem getting dental care | In the last 12 months, how much of a problem, if any, was it to get dental care for your child? (dichotomized: not a problem/small problem, big problem) |
| Rarely or never got immediate care | In the last 12 months, when YOUR CHILD needed care right away for an illness, injury, or condition, how often did your child get care as soon as you wanted it? INCLUDED OPTION TO OPT OUT IF CHILD DID NOT NEED CARE (dichotomized: always/usually, rarely/never) |
| Big problem getting specialty care | In the last 12 months, did you or a doctor think that YOUR CHILD needed care from a specialist? (Specialists are doctors like surgeons, allergy doctors, skin doctors, and others who specialize in one area of health care.) ONLY THOSE RESPONDING YES were asked: In the last 12 months, how much of a problem, if any, was it to see the specialist that your child needed to see? (dichotomized: not a problem/small problem, big problem) |
| Big problem getting counseling | Does your child have any kind of developmental, emotional, or mental health condition now for which he or she needs treatment or counseling? ONLY THOSE RESPONDING YES were asked: In the last 12 months, how much of a problem, if any, was it for you to get this treatment or counseling for your child? (dichotomized: not a problem/small problem, big problem) |
Health Insurance Enrollment Variables
We constructed two child health insurance enrollment variables incorporating responses to four survey questions and state data. The first question asked, “At this time, what type of health insurance is your child covered by?” Respondents could choose among several check boxes. For validation, we examined three additional questions that included the option: “My child currently has health insurance.” Twenty-four of the 2,681 respondents had inconsistencies, and these were excluded from further analyses. Among the remaining 2,657, we incorporated administrative data and put each child into four groups: (1) Child is OHP insured, aware of status (enrolled in OHP by administrative data and self-report), (2) Child has private insurance, aware of status (not administratively enrolled in OHP and self-reported private), (3) Child has uncertain coverage, not aware of status (mismatch between OHP administrative enrollment status and self-report, “gray zone”), (4) Child is uninsured, aware of status (not administratively enrolled in OHP and self-reported uninsured). We constructed a second variable, further differentiating between the two gray-zone groups with uncertain status: uninsured, unaware of status (not administratively enrolled but self-reported OHP coverage), and OHP-enrolled, unaware of status (administratively OHP-enrolled but self-reported not enrolled in OHP).
Predictor Variables
The conceptual model for predicting access to health care developed by Aday and Andersen was adapted to identify the following nine covariables, which might influence a child’s access to health insurance and health care services: child’s gender, child’s age, child’s race/ethnicity, parental employment, parental insurance status, geographic region, monthly household income, whether or not child has a special health care need (yes/no), and whether or not child has a usual source of care (yes/no).35 According to the Behavioral Model of Health Services Utilization, predisposing factors include sociodemographics known to influence an individual’s health behavior and propensity to seek health care (eg, age, race/ethnicity); enabling resources are personal, family, and community resources that facilitate or impede a person’s ability to seek care (eg, parental employment, parental insurance); and need for care encompasses a perceived need for health care services (eg, whether or not the child has a special health care need).
All of these factors affect a person’s ability to access and use both health insurance (primary predictor) and necessary health care services (primary outcomes). We hypothesized that access to health insurance and awareness of health insurance status would both be associated with access to and utilization of health care services. All independent covariables were significantly associated with at least one outcome in two-tailed, chi-square bivariate analyses (P<.10).
Analysis
We performed all statistical tests using SPSS 16.0 using the complex samples module to account for the complex sampling design. We used chi-square bivariate analyses to indentify demographic characteristics associated with enrollment status (Table 2). We then ran a series of logistic regression models to identify covariates associated with higher odds of being in the two groups of children whose parents were unaware or uncertain of their child’s insurance status: (1) OHP enrolled, unaware and (2) uninsured, unaware, as compared with being in the group who were OHP enrolled, aware (Table 3). To assess whether a child in an insurance gray zone had higher odds of experiencing unmet health care needs, after accounting for all covariates, we conducted another series of multivariable models (Tables 4 and 5).
Table 2.
Demographic Characteristics of Children in Oregon’s Food Stamp Population by Health Insurance Enrollment Status
| Independent Covariables |
Child Has Public
Insurance (OHP) n= 1300 (Weighted %) |
Child Has Private
Insurance n= 554 (Weighted %) |
Child Has Uncertain Health
Insurance Status (in a “Gray Zone”) n= 423 (Weighted %) |
Child Is Uninsured
n=380 (Weighted %) |
|---|---|---|---|---|
|
| ||||
| Child’s gender (n=2,657) $ | ||||
| Female | 50.1 | 44.8 | 44.5 | 49.0 |
| Male | 49.9 | 55.2 | 55.5 | 51.0 |
|
| ||||
| Child’s age** (n=2,657)$ | ||||
| 1–4 years | 31.9 | 22.5 | 25.9 | 18.2 |
| 5–9 years | 29.6 | 32.9 | 27.6 | 32.7 |
| 10–14 years | 23.7 | 28.8 | 30.5 | 28.7 |
| 15–18 years | 14.8 | 15.8 | 16.0 | 20.4 |
|
| ||||
| Race/ethnicity* (n=2,657)$ | ||||
| White, non-Hispanic | 68.3 | 83.4 | 67.0 | 62.9 |
| Hispanic, any race | 20.2 | 8.4 | 21.6 | 29.0 |
| Non-white, non-Hispanic | 11.5 | 8.3 | 11.4 | 8.1 |
|
| ||||
| Parental employmenta* (n=2,596)$$ | ||||
| Not employed | 63.3 | 33.7 | 53.7 | 43.7 |
| Employed | 36.7 | 66.3 | 46.3 | 56.3 |
|
| ||||
| Parental insurance statusb* (n=2,540)$$ | ||||
| Insured | 74.7 | 77.9 | 52.8 | 22.5 |
| Not insured | 25.3 | 22.1 | 47.2 | 77.5 |
|
| ||||
| Geographic region (n=2,657) $ | ||||
| 1 (NW Coastal) | 4.3 | 4.1 | 4.1 | 4.9 |
| 2 (Portland Area) | 37.5 | 33.8 | 34.7 | 38.0 |
| 3 (Central Western) | 28.4 | 34.9 | 26.0 | 24.1 |
| 4 (SW Coastal) | 15.4 | 13.1 | 16.2 | 17.6 |
| 5 (North Central, Columbia Gorge) | 8.9 | 9.3 | 12.4 | 11.4 |
| 6 (Southern and Eastern) | 5.6 | 4.7 | 6.6 | 4.0 |
|
| ||||
| Monthly household income* (n=2,657)$ | ||||
| <$1,000 | 70.7 | 30.3 | 55.7 | 50.1 |
| $1,000–$1,500 | 16.3 | 16.9 | 22.5 | 18.8 |
| $1,501–$2,000 | 8.5 | 27.2 | 12.7 | 17.1 |
| >$2,000 | 4.5 | 25.6 | 9.1 | 14.0 |
|
| ||||
| Child has special health care need(s)c** (n=2,510) $$ | ||||
| No | 85.9 | 92.2 | 85.1 | 92.3 |
| Yes | 14.1 | 7.8 | 14.9 | 7.7 |
|
| ||||
| Child has usual source of care* (n=2,524)$$ | ||||
| Yes usual source of care | 93.1 | 83.6 | 95.8 | 90.4 |
| No usual source of care | 6.9 | 16.4 | 4.2 | 9.6 |
Note: Oregon Health Plan (OHP) is Oregon’s combined Medicaid and State Children’s Health Insurance Program
P<.001 in the χ2 analysis for overall differences between demographic subgroups.
P<.01 in the χ2 analysis for overall differences between demographic subgroups.
Demographic characteristic known from administrative data.
Demographic characteristics known from self report.
(Note: Population number varies for each characteristic depending on the information available. The demographic data gathered from administrative files was more complete than the self-reported data.)
The employment status of the parent who completed the survey (>85% were mothers).
The insurance status of the parent who completed the survey.
Response to the following question: “Does YOUR CHILD have a physical, emotional, or mental health condition now that seriously interferes with your child’s ability to do the things most children his or her age can do?”
Column percentage=100% (may not be exact due to rounding to nearest 10th)
Total in sample with known administrative data and self-reported insurance information = (unweighted n=2,657, weighted n= 83,580).
Four groups: (1) Child Has Public Insurance (Oregon Health Plan—OHP) (enrolled in public insurance by both administrative data and self-report): unweighted n=1,300, weighted n= 57,356 (68.6%); (2) Child Has Private Insurance (private by self-report, not administratively enrolled in OHP): unweighted n=554, weighted n=9,211 (11.0%); (3) Child Has Uncertain Health Insurance Status “Gray Zone” (mismatch between administrative and self-reported data): unweighted n=423, weighted n=11,063 (13.2%); (4) Child Is Uninsured (uninsured by self-report, not administratively enrolled in OHP): unweighted n=380, weighted n=5,950 (7.1%).
Table 3.
Factors Associated With a Child’s Uncertain Health Insurance Status (Mismatch Between Administrative and Self-reported Health Insurance Enrollment Data— the Gray Zones)
| Independent Covariables |
OHP Enrolled, Unaware n= 171 (Weighted n=5,974) (Weighted %) |
OHP Enrolled, Unaware (Versus OHP Enrolled, Aware) Adjusted OR* (95% CI) |
Uninsured, Unaware
n= 252 (Weighted n=3,474) (Weighted %) |
Uninsured, Unaware (Versus OHP Enrolled, Aware) Adjusted OR* (95% CI) |
|---|---|---|---|---|
|
| ||||
| Child’s gender | ||||
| Female | 7.8 | 0.88 (0.55, 1.41) | 4.3 | 0.79 (0.54, 1.17) |
| Male | 9.4 | 1.00 | 4.9 | 1.00 |
|
| ||||
| Child’s age | ||||
| 1–4 years | 6.7 | 0.54 (0.25, 1.15) | 5.1 | 0.88 (0.47, 1.66) |
| 5–9 years | 7.4 | 0.78 (0.39, 1.57) | 4.8 | 0.96 (0.52, 1.75) |
| 10–14 years | 12.1 | 1.12 (0.57, 2.22) | 3.7 | 0.76 (0.39, 1.47) |
| 15–18 years | 9.1 | 1.00 | 4.6 | 1.00 |
|
| ||||
| Race/ethnicity (combined variable) |
||||
| White, non-Hispanic | 8.3 | 1.00 | 4.5 | 1.00 |
| Hispanic, any race | 9.1 | 1.22 (0.65, 2.28) | 5.4 | 1.00 (0.82, 1.22) |
| Non-white, Non-Hispanic | 9.9 | 0.84 (0.32, 2.22) | 4.0 | 1.19 (0.94, 1.50) |
|
| ||||
| Parental employmenta | ||||
| Not employed | 8.2 | 1.00 | 4.4 | 1.00 |
| Employed | 9.6 | 1.39 (0.86, 2.25) | 5.0 | 1.53 (1.03, 2.27) |
|
| ||||
| Parental insurance statusb | ||||
| Insured | 6.3 | 1.00 | 3.7 | 1.00 |
| Not insured | 12.5 | 2.81 (1.68, 4.69) | 6.8 | 2.21 (1.41, 3.46) |
|
| ||||
| Geographic region | ||||
| 1 (NW Coastal) | 8.3 | 0.80 (0.44, 1.46) | 4.3 | 0.94 (0.79, 1.11) |
| 2 (Portland Area) | 8.4 | 0.79 (0.41, 1.52) | 4.2 | 1.05 (0.86, 1.28) |
| 3 (Central Western) | 7.6 | 1.03 (0.53, 2.01) | 4.5 | 1.51 (1.23, 1.87) |
| 4 (SW Coastal) | 9.1 | 0.85 (0.45, 1.60) | 4.8 | 1.27 (1.06, 1.53) |
| 5 (North Central, Columbia Gorge) | 10.7 | 1.03 (0.52, 2.01) | 6.4 | 1.88 (1.59, 2.24) |
| 6 (Southern and Eastern) | 11.3 | 1.00 | 4.6 | 1.00 |
|
| ||||
| Monthly household income | ||||
| <$1,000 | 8.0 | 1.00 | 3.8 | 1.00 |
| $1,000–$1,500 | 12.1 | 1.74 (0.97, 3.13) | 5.1 | 1.40 (0.86, 2.28) |
| $1,501–$2,000 | 6.8 | 1.10 (0.47, 2.55) | 7.5 | 2.50 (1.37, 4.58) |
| >$2,000 | 9.0 | 2.09 (0.82, 5.36) | 5.8 | 2.94 (1.45, 5.96) |
|
| ||||
| Child has special health care need(s)c | ||||
| No | 8.2 | 1.00 | 4.7 | 1.00 |
| Yes | 11.2 | 0.85 (0.41, 1.78) | 3.9 | 0.70 (0.40, 1.23) |
|
| ||||
| Child has usual source of care (USC) | ||||
| Yes USC | 8.0 | 1.00 | 4.3 | 1.00 |
| No USC | 16.2 | 3.27 (1.71, 6.25) | 6.7 | 1.87 (0.99, 3.54) |
OHP—Oregon Health Plan (Oregon’s combined Medicaid and State Children’s Health Insurance Program)
Controlling for all variables listed in the table. (Comparison group in dichotomous outcome variables is OHP-insured children.)
OHP Enrolled, Not Aware: child was administratively OHP enrolled but self-reported not being enrolled. Uninsured, Not Aware: not administratively enrolled in OHP but self-reported OHP enrolled.
see footnotes from Table 2
Table 4.
Associations Between a Child’s Health Insurance Status and Unmet Health Care Needs
| Access Measure |
% Reporting Children’S Health
Care Access Difficulties (Weighted) |
Multivariate
Odds Ratio * |
P Value** |
|---|---|---|---|
|
| |||
| Unmet medical need | |||
| Child has public insurance (OHP), aware | (Total 16.0%) | ||
| Child has private insurance, aware | 12.7 | 1.00 | |
| Child OHP enrolled, unaware | 14.4 | 1.37 (0.88, 2.14) | |
| Child uninsured, unaware | 19.2 | 1.64 (0.87, 3.09) | |
| Child uninsured, aware | 24.6 | 1.91 (1.16, 3.14) | |
| (unweighted n=2,236, weighted n=70,088) | 41.9 | 4.32 (2.78, 6.72) | P<.001 |
|
| |||
| Unmet prescription need | |||
| Child has public insurance (OHP), aware | (Total 22.1%) | ||
| Child has private insurance, aware | 18.4 | 1.00 | |
| Child OHP enrolled, unaware | 29.9 | 1.76 (1.22, 2.56) | |
| Child uninsured, unaware | 28.5 | 1.88 (1.11, 3.19) | |
| Child uninsured, aware | 22.5 | 1.26 (0.80, 1.98) | |
| (unweighted n=2,215, weighted n=69,557) | 37.7 | 2.47 (1.62, 3.79) | P<.001 |
|
| |||
| Missed medication doses | |||
| Child has public pnsurance (OHP), aware | (Total 10.7%) | ||
| Child has private insurance, aware | 8.8 | 1.00 | |
| Child OHP enrolled, unaware | 15.2 | 1.87 (1.09, 3.20) | |
| Child uninsured, unaware | 11.5 | 1.19 (0.62, 2.32) | |
| Child uninsured, aware | 14.5 | 1.74 (0.99, 3.05) | |
| (unweighted n=2,226, weighted n=69,853) | 19.0 | 2.35 (1.33, 4.14) | P<.001 |
|
| |||
| No doctor visits | |||
| Child has public insurance (OHP), aware | (Total 13.8%) | ||
| Child has private insurance, aware | 10.6 | 1.00 | |
| Child OHP enrolled, unaware | 11.0 | 1.02 (0.59, 1.77) | |
| Child uninsured, unaware | 18.4 | 1.04 (0.54, 2.01) | |
| Child uninsured, aware | 16.8 | 1.15 (0.58, 2.29) | |
| (unweighted n=2,259, weighted n=70,903) | 41.3 | 2.67 (1.61, 4.43) | P<.001 |
|
| |||
| Rarely or never got immediate care1 | |||
| Child has public insurance (OHP), aware | (Total 21.6%) | ||
| Child has private insurance, aware | 18.5 | 1.00 | |
| Child OHP enrolled, unaware | 12.8 | 0.68 (0.38, 1.22) | |
| Child uninsured, unaware | 32.6 | 2.28 (1.18, 4.42) | |
| Child uninsured, aware | 30.6 | 1.96 (1.10, 3.50) | |
| (unweighted n=1,522, weighted n=48,389) | 50.3 | 3.92 (2.30, 6.70) | P<.001 |
|
| |||
| Big problem getting dental care | |||
| Child has public insurance (OHP), aware | (Total 25.9%) | ||
| Child has private insurance, aware | 20.5 | 1.00 | |
| Child OHP enrolled, unaware | 21.6 | 0.87 (0.59, 1.29) | |
| Child uninsured, unaware | 41.8 | 2.80 (1.70, 4.62) | |
| Child uninsured, aware | 32.4 | 1.78 (1.15, 2.76) | |
| (unweighted n=2,209, weighted n=69,341) | 61.5 | 5.58 (3.70, 8.43) | P<.001 |
|
| |||
| Big problem getting specialty care2 | |||
| Child has public insurance (OHP), aware | (Total 29.5%) | ||
| Child has private insurance, aware | 27.0 | 1.00 | |
| Child OHP enrolled, unaware | 21.0 | 0.40 (0.18, 0.88) | |
| Child uninsured, unaware | 33.9 | 1.17 (0.49, 2.79) | |
| Child uninsured, aware | 54.9 | 2.12 (0.96, 4.67) | |
| (unweighted n=570, weighted n=18,060) | 45.2 | 1.30 (0.56, 3.01) | P<.05 |
|
| |||
| Big problem getting counseling3 | |||
| Child has public insurance (OHP), aware | (Total 20.7%) | ||
| Child has private insurance, aware | 16.5 | 1.00 | |
| Child OHP enrolled, unaware | 32.9 | 2.27 (1.00, 5.15) | |
| Child uninsured, unaware | 33.0 | 6.06 (1.94, 18.98) | |
| Child uninsured, aware | 18.5 | 1.52 (0.53, 4.39) | |
| (unweighted n=519, weighted n=16,399) | 35.5 | 5.23 (2.06, 13.27) | P<.05 |
Child has Public Insurance (OHP), Aware: child was administratively OHP-enrolled, and self-reported OHP-enrolled.
Child has Private Insurance, Aware: child was not administratively OHP-enrolled, and self-reported having private coverage.
Child OHP-Enrolled, Unaware: child was administratively OHP-enrolled, but self-reported not being enrolled.
Child Uninsured, Unaware: not administratively enrolled in OHP, but self-reported OHP-enrolled.
Child Uninsured, Aware; not administratively enrolled in OHP, and self-reported being uninsured.
P value in the χ2 analysis for overall differences between the four groups.
Adjusted for child’s gender, child’s age, child’s race/ethnicity, parental employment, parental insurance status, geographic region, monthly household income, whether or not child has a special health care need (yes/no), whether or not child has a usual source of care (yes/no).
Only among children who needed immediate care in the previous 12 months;
Only among children who needed specialty care in the previous 12 months;
Only among children who needed counseling in the previous 12 months.
Table 5.
Associations Between Uncertain Health Insurance Coverage (Being in an Insurance Gray Zone) and Children’s Unmet Health Care Needs
| Access Measure |
% Reporting Children’S Health
Care Access Difficulties (Weighted) |
Multivariate
Odds Ratio * |
P Value** |
|---|---|---|---|
|
| |||
| Unmet medical need | (Total 16.0%) | ||
| Child has OHP (public insurance) | 12.7 | 1.00 | P<.001 |
| Child has private insurance | 14.4 | 1.37 (0.88, 2.14) | |
| Child is in health insurance “gray zone” | 21.1 | 1.73 (1.07, 2.79) | |
| Child is uninsured | 41.9 | 4.33 (2.79, 6.73) | |
| (unweighted n=2,236, weighted n=70,088) | |||
|
| |||
| Unmet prescription need | |||
| Child has OHP (public insurance) | (Total 22.1%) | ||
| Child has private insurance | 18.4 | 1.00 | P<.001 |
| Child is in health insurance “gray zone” | 29.9 | 1.77 (1.22, 2.56) | |
| Child is uninsured | 26.4 | 1.64 (1.08, 2.48) | |
| (unweighted n=2,215, weighted n=69,557) | 37.7 | 2.46 (1.61, 3.76) | |
|
| |||
| Missed medication doses | |||
| Child has OHP (public insurance) | (Total 10.7%) | ||
| Child has private insurance | 8.8 | 1.00 | P<.001 |
| Child is in health insurance “gray zone” | 15.2 | 1.87 (1.09, 3.19) | |
| Child is uninsured | 12.5 | 1.38 (0.83, 2.28) | |
| (unweighted n=2,226, weighted n=69,853) | 19.0 | 2.36 (1.34, 4.15) | |
|
| |||
| No doctor visits | |||
| Child has OHP (public insurance) | (Total 13.8%) | ||
| Child has private insurance | 10.6 | 1.00 | P<.001 |
| Child is in health insurance “gray zone” | 11.0 | 1.02 (0.59, 1.77) | |
| Child is uninsured | 17.8 | 1.08 (0.63, 1.84) | |
| (unweighted n=2,259, weighted n=70,902) | 41.3 | 2.68 (1.62, 4.44) | |
|
| |||
| Big problem getting dental care | |||
| Child has OHP (public insurance) | (Total 25%) | ||
| Child has private insurance | 20.5 | 1.00 | P<.001 |
| Child is in health insurance “gray zone” | 21.6 | 0.88 (0.59, 1.30) | |
| Child is uninsured | 38.5 | 2.41 (1.63, 3.56) | |
| (unweighted n=2,209, weighted n=69,341) | 61.5 | 5.58 (3.70, 8.43) | |
|
| |||
| Rarely or never got immediate care1 | |||
| Child has OHP (public insurance) | (Total 21.6%) | ||
| Child has private insurance | 18.5 | 1.00 | P<.001 |
| Child is in health insurance “gray zone” | 12.8 | 0.68 (0.38, 1.22) | |
| Child is uninsured | 31.9 | 2.17 (1.30, 3.63) | |
| (unweighted n=1,522, weighted n=48,389) | 50.3 | 3.92 (2.29, 6.69) | |
|
| |||
| Big problem getting specialty care2 | |||
| Child has OHP (public insurance) | (Total 29.5%) | P<.05 | |
| Child has private insurance | 27.0 | 1.00 | |
| Child is in health insurance “gray zone” | 21.0 | 0.39 (0.18, 0.88) | |
| Child is uninsured | 38.9 | 1.37 (0.67, 2.80) | |
| (unweighted n=570, weighted n=18,060) | 45.2 | 1.30 (0.56, 3.00) | |
|
| |||
| Big problem getting counseling3 | |||
| Child has OHP (public insurance) | (Total 21%) | ||
| Child has private insurance | 16.5 | 1.00 | P<.05 |
| Child is in health insurance “gray zone” | 32.9 | 2.34 (1.03, 5.33) | |
| Child is uninsured | 27.3 | 3.52 (1.56, 7.98) | |
| (unweighted n=519, weighted n=16,399) | 35.5 | 5.07 (2.02, 12.69) | |
OHP—Oregon Health Plan (combined Medicaid and State Children’s Health Insurance Program)
Note: Gray zone group above combines both child OHP enrolled, unaware (child was administratively OHP enrolled but self-reported not being enrolled) and child uninsured, unaware (not administratively enrolled in OHP but self-reported OHP enrolled), which are shown separately in Table 4.
P value in the χ2 analysis for overall differences between the four groups.
Adjusted for child’s gender, child’s age, child’s race/ethnicity, parental employment, parental insurance status, geographic region, monthly household income, whether or not child has a special health care need (yes/no), whether or not child has a usual source of care (yes/no).
Only among children who needed immediate care in the previous 12 months;
Only among children who needed specialty care in the previous 12 months;
Only among children who needed counseling in the previous 12 months.
Results
Children’s Health Insurance Enrollment and Demographic Factors
More than two thirds (68.7%) of the children in the study population were administratively enrolled in OHP and aware of being publicly insured, 11% were not administratively enrolled and reported private insurance, and 7.1% were not administratively enrolled and aware of being uninsured. But, 13.2% of the children were in the gray zone, with parents unaware of their child’s current OHP administrative insurance status. When comparing children with uncertain coverage to those with certain OHP enrollment, a higher percentage had uninsured parents, were from families earning more than $1,000 per month, were of Hispanic origin, and had parents employed outside the home. Uncertainty was also associated with a higher percentage of children with special health care needs and children without a usual source of care (USC) (Table 2).
Among children in the gray zone of uncertainty, approximately one third (n=171) were administratively enrolled but self-reported not being enrolled in OHP (OHP enrolled, unaware), and two thirds (n=252) were not administratively enrolled but reported current OHP enrollment (uninsured, unaware). As predicted by the Aday and Anderson Behavioral Model, certain characteristics predisposed children to having higher odds of an uncertain health insurance status. For, example, having a parent who was uninsured was significantly associated with higher odds of a child being in either of the two gray zones, as compared to those who were aware of their child’s OHP enrollment status (Table 3). Those not aware of being uninsured were more likely to have employed parents and to be living in families earning greater than $1,500 per month. Having no USC was associated with being OHP-enrolled but unaware (Table 3).
Health Insurance Gray Zones and Children’s Access to Health Care
Among children in Oregon’s food stamp population, being in a health insurance gray zone was associated with compromised access to health care (Table 4). Both gray zone subgroups experienced significantly higher odds of delayed care and unmet dental needs, compared to those with certain OHP coverage. Children who were OHP enrolled, but unaware, also had higher odds of unmet prescription and counseling needs. Those uninsured, but unaware, had higher odds of unmet medical needs.
Children in the combined gray zones had almost twice the odds of unmet medical and prescription needs, when compared with those who had more certain OHP coverage. In addition, being in a gray zone was associated with two to three times the odds of experiencing delayed care and encountering big problems getting dental care and counseling (Table 5).
Uninsured children had the highest odds of experiencing unmet needs. Children with private coverage had fewer significant differences than those covered by OHP. When compared to OHP-insured children, those with private coverage had higher odds of unmet prescription and counseling needs, while privately covered children had lower odds of experiencing big problems getting specialty care.
Discussion
Health insurance coverage is essential to the health and well-being of all children in the United States.36 Yet, among a population of children in Oregon presumed eligible for public insurance, one out of five children (20.3%) was either uninsured or in an insurance gray zone. The parents of one out of eight children (13.2%) in this low-income population reported an insurance status that differed from state administrative records. Children with an uncertain health insurance status were more likely to experience unmet health care needs, when compared to children whose parents were certain about their public coverage status. Insured children whose parents were not aware of this status appeared to be slightly more vulnerable, especially for unmet medication and counseling needs. Thus, this study further informs the Aday and Anderson Behavioral Model by demonstrating that an uncertain health insurance status was a hindrance to obtaining necessary health care services, as compared with having more certainty about one’s coverage.
There are likely multiple explanations for uncertainty about the health insurance status of children in our study population. While the administrative insurance status of the child was known at the time of final sample selection, the mailing, re-mailing, completion, and return of household surveys cannot happen instantaneously. We observed an average of 10 to 60 days between the date a survey was mailed and when it was returned, during which time a child’s health insurance status may have changed. At the time of the survey, Oregon required children to reenroll every 6 months. Such frequent reenrollment requirements (ie, 6 months versus 12 months) have been associated with higher rates of coverage gaps;37 therefore, some of our study participants may have fallen into the gray zones due to a lapse in public coverage that occurred during the short study period.
But, while lapsed coverage can explain some cases, it cannot explain all cases. We conducted a post-hoc analysis of the 252 children whose parents believed they were covered by OHP but were not administratively OHP enrolled, and we found 141 whose parents reported their child to be OHP enrolled continuously for the past 12 months. For these confirmed mismatches, the uncertainty might have been due to parental confusion about obtaining or maintaining enrollment in OHP.27,37-43 The parents of the remaining 111 children reported that their child had an insurance gap during the previous year. We did not, however, have self-reported data to determine when they believed this gap to have occurred. Future studies should be designed to enable confirmation of public insurance status on the date surveys are completed (eg, require parents to write a date on the actual survey and cross-reference with administrative files from that exact date). Or, alternatively, policy reform efforts could create a “Medicare for kids” program that would nearly eliminate uncertainty about a child’s eligibility or enrollment status (ie, if the child is under 19 years old, he or she is automatically covered—similar to how Medicare works for individuals aged 65 and older).
Regardless of whether frequent lapses in insurance coverage or confusion about enrollment explain why a particular child had uncertainty surrounding his or her insurance status, in this study, being in a gray zone mattered. This study showed a clear differentiation between children in the gray zones as compared with those who appeared to have more certain and continuous coverage. While not as severely affected as those who were aware of being uninsured, children in gray zones experienced more unmet health care needs when compared to those with certain coverage. Further, the large number of children with an uncertain insurance status challenges the assumption that low-income children have adequate access to continuous insurance simply by meeting eligibility requirements.
Policy and Practice Implications
Our study revealed a significant number of low-income children with uncertainty surrounding their insurance status and that being in these gray zones was associated with higher rates of unmet health care needs. What can be done to minimize coverage lapses and uncertainty surrounding public insurance coverage? Clinicians can develop and test practice-level interventions to improve enrollment and retention in public insurance programs. Our findings suggest socio-demographic factors associated with increased odds that a child will fall into a gray zone. An intervention could be as simple as education provided by a clinician during a well-child visit or a flyer in the waiting room. Primary care practices could also contribute to public insurance retention efforts by developing mechanisms that track a patient’s insurance enrollment date and institute systems to remind parents of upcoming renewal periods while also offering assistance. Some electronic health records might facilitate automated processes. We conducted an extensive literature search and found no reports of studies evaluating these types of interventions; such research needs to be done.
On the policy side, efforts to enroll and retain eligible children in public health insurance programs should continue, and clinicians can be effective advocates. Specifically, clinicians and educators can lobby for elimination of SCHIP waiting periods and other reforms to minimize churning. A unified public benefits application process (sometimes referred to as Express Lane Eligibility) is another way to streamline enrollment in multiple public programs at one time. This process has also proven to be cost-saving.39 Advocacy efforts related to improving SCHIP are excellent opportunities to get students and residents involved in the policy-making process.44,45
Limitations
One limitations of our study is that families enrolled in the food stamp program are already connected to a public benefit and may encounter less uncertainty about how to obtain and maintain insurance coverage compared to a more general low-income population. Our results can only be generalized to Oregon’s food stamp population, so our study may be understating the prevalence of insurance uncertainty in the general population. It does, however, illustrate an association between higher rates of unmet health care needs and being in an insurance gray zone.
A second limitation is that budgetary constraints allowed survey administration in only English, Spanish, and Russian, and telephone follow-up was not possible. A third limitation is that while the 31% response rate is comparable to similar studies of Medicaid-eligible populations,46-49 and we took several steps to achieve weighted adjustments, response bias may have affected the study results.
Fourth, as with any self-reported data, there is potential for recall bias and reporting error. To minimize recall bias, we asked respondents to recall only those events and occurrences from the past 12 months and several questions pertained to similar topics to verify consistency in responses.
Fourth, the cross-sectional nature of our analyses uncovers associations but prevents making any causal inferences, and we may have omitted other potential confounders that could have affected access to care. Finally, as previously mentioned, there are likely multiple explanations for children being in the gray zones, as they are described in this study. We could not confirm each child’s enrollment status on the exact date a survey was completed or received; thus, it is likely that churning on and off coverage accounts for some cases of uncertainty. We were, however, able to conduct a posthoc analysis comparing the full-year self-reported insurance status of all children who were uninsured but unaware. The confirmed insurance status mismatch in a majority of these cases demonstrates that parental uncertainty was a common reason for being in a gray zone.
Conclusions
Some families whose children have health insurance may be unaware of this coverage; other families who believe their children are covered may be mistaken. Regardless of whether these children actually possess or lack coverage, being in a gray zone may put them at risk for experiencing unmet health care needs.
Acknowledgments
Thank you to the Office for Oregon Health Policy and Research (OHPR), the Oregon Department of Children, Adults, and Families (CAF-food stamp office), and the Oregon Division of Medical Assistance Programs. We are grateful for contributions from Janne Boone, Jessica Miller, James Oliver, Rebecca Ramsey, Pooya Naderi, Jeanene Smith, Bruce Goldberg, Ron Taylor, and Jeff Tharpe. A special thank you to Tina Edlund for her survey design expertise. We also wish to acknowledge the parents who completed surveys and the anonymous peer reviewers who shared their insights to improve this manuscript.
The study was partially funded by a grant to the Oregon Office for Health Policy and Research from the Health Resources and Services Administration. Dr DeVoe’s time on this project was partially supported by grant numbers 5-F32-HS014645 and 1-K08-HS16181 from the Agency for Healthcare Research and Quality and by the OHSU Department of Family Medicine Research Division. These funding agencies had no involvement in the design and conduct of the study, analysis and interpretation of the data, and preparation, review, or approval of the manuscript.
Appendix 1 Flow Diagram of Potential Study Participants
Appendix 2 Comparison of Respondent Characteristics to Sample Population
| Demographics |
Overall Sample 10,175 n—unweighted (%—unweighted) |
Eligible Population 8,636 n—unweighted (%—unweighted) |
Survey Respondents 2,681 n—unweighted (%—unweighted) |
Response Rate Percent of Survey Respondents From Eligible Population (unweighted) |
|---|---|---|---|---|
| Overall 31.0% | ||||
| Race/ethnicity* | ||||
| White | 7,528 (74.0%) | 6,369 (73.7%) | 2,026 (75.6%) | 31.8% |
| Black | 270 (2.7%) | 218 (2.5%) | 50 (1.9%) | 22.9% |
| Hispanic | 1,864 (18.3%) | 1,600 (18.5%) | 475 (17.7%) | 29.7% |
| Asian | 110 (1.1%) | 95 (1.1%) | 31 (1.2%) | 32.6% |
| American Indian | 324 (3.2%) | 286 (3.3%) | 74 (2.8%) | 25.9% |
| Pacific Islander | 13 (0.1%) | 12 (0.1%) | 6 (0.2%) | 50.0% |
| Other | 47 (0.5%) | 40 (0.5%) | 16 (0.6%) | 40.0% |
| Unknown | 19 (0.2%) | 16 (0.2%) | 3 (0.1%) | 18.9% |
| Gender (child) | ||||
| Female | 4,983 (49.0%) | 4,227 (48.9%) | 1,295 (48.3%) | 30.6% |
| Male | 5,192 (51.0%) | 4,409 (51.1%) | 1,386 (51.7%) | 31.4% |
| Age | ||||
| 1 to 4 | 2,728 (26.8%) | 2,259 (26.2%) | 687 (25.6%) | 30.4% |
| 5 to 9 | 2,943 (28.9%) | 2,495 (28.9%) | 811 (30.2%) | 32.5% |
| 10 to 14 | 2,520 (24.8%) | 2,192 (25.4%) | 707 (26.4%) | 32.3% |
| 15 and over | 1,984 (19.5%) | 1,690 (19.6%) | 476 (17.8%) | 28.2% |
| Region | ||||
| 1 (NW Coastal) | 1,685 (16.6%) | 1,459 (16.9%) | 504 (18.8%) | 34.5% |
| 2 (Portland Area) | 1,702 (16.7%) | 1,387 (16.1%) | 417 (15.6%) | 30.1% |
| 3 (Central Western) | 1,701 (16.7%) | 1,448 (16.8%) | 427 (15.9%) | 29.5% |
| 4 (SW Coastal) | 1,696 (16.7%) | 1,462 (16.9%) | 435 (16.2%) | 29.8% |
| 5 (North Central, Columbia Gorge) | 1,695 (16.7%) | 1,422 (16.5%) | 409 (15.3%) | 28.8% |
| 6 (Southern and Eastern) | 1,696 (16.7%) | 1,461 (16.9%) | 489 (18.2%) | 33.5% |
| Current enrollment in a program sponsored by the Office for Medical Assistance Programs (OMAP) |
||||
| At least one child enrolled in OMAP | 5,087 (50.0%) | 4,346 (50.3%) | 1,471 (54.9%) | 33.8% |
| No child enrolled in OMAP | 5,088 (50.0%) | 4,290 (49.7%) | 1,210 (45.1%) | 28.2% |
| Monthly Income** | ||||
| <$500 | 3,109 (30.6%) | 2,589 (30.0%) | 770 (28.7%) | 29.7% |
| $501–$1,000 | 2,628 (25.8%) | 2,221 (25.7%) | 711 (26.5%) | 32.0% |
| $1,001–$1,500 | 1,976 (19.4%) | 1,666 (19.3%) | 487 (18.2%) | 29.2% |
| $1,501–$2,000 | 1,434 (14.1%) | 1,249 (14.5%) | 412 (15.4%) | 33.0% |
| >$2,000 | 1,028 (10.1%) | 911 (10.5%) | 301 (11.2%) | 33.0% |
Race and ethnicity are combined into one variable in this table because the administrative data available to us had only one combined variable. For the tables based only on self-reported data, there are two separate variables.
Household income data are reported as monthly income, which was available in the administrative data. Self-reported data about household size and income allowed us to calculate income as a percentage of the federal poverty level.
References
- 1.DeVoe JE, Dodoo MS, Phillips RL, Green LA. Graham Center one-pager: who will have health insurance in 2025. Am Fam Physician. 2005;72:1989. [PubMed] [Google Scholar]
- 2.Cuttler L, Kenney G. State Children’s Health Insurance Program and pediatrics. Arch Pediatr Adolesc Med. 2007;161:630–3. doi: 10.1001/archpedi.161.7.630. [DOI] [PubMed] [Google Scholar]
- 3.Selden T, Hudson J. Access to care and utilization among children: estimating the effects of public and private coverage. Med Care. 2006;44:I-19–I-26. doi: 10.1097/01.mlr.0000208137.46917.3b. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham PJ, Hadley J, Reschovsky J. The effects of SCHIP on children’s health insurance coverage: early evidence from the Community Tracking Study. Med Care Res Rev. 2002;59:359–83. doi: 10.1177/107755802237807. [DOI] [PubMed] [Google Scholar]
- 5.Vistnes JP, Rhoades JA. Changes in children’s health insurance status, 1996-2005: estimates for the US civilian noninstitutionalized population under age 18. Agency for Healthcare Research and Quality; Washington, DC: 2006. Statistical Brief #141. [Google Scholar]
- 6.Vistnes J, Schone B. Pathways to coverage: the changing roles of public and private sources. Health Aff. 2008;27:44–57. doi: 10.1377/hlthaff.27.1.44. [DOI] [PubMed] [Google Scholar]
- 7.DeVoe JE, Graham A, Krois L, Smith J, Fairbrother GL. “Mind the gap” in children’s health insurance coverage: does the length of a child’s coverage gap matter? Ambul Pediatr. 2008;8:19–32. doi: 10.1016/j.ambp.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Satchell M, Pati S. Insurance gaps among vulnerable children in the United States, 1999-2001. Pediatrics. 2005;116:1155–61. doi: 10.1542/peds.2004-2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guendelman S, Angulo V, Oman D. Access to health care for children and adolescents in working poor families. Med Care. 2005;43:68–78. [PubMed] [Google Scholar]
- 10.Shi LY. The convergence of vulnerable characteristics and health insurance in the US. Soc Sci Med. 2001;53:519–29. doi: 10.1016/s0277-9536(00)00357-9. [DOI] [PubMed] [Google Scholar]
- 11.Probst JC, Moore CG, Baxley EG. Update: health insurance and utilization of care among rural adolescents. J Rural Health. 2005;21:279–87. doi: 10.1111/j.1748-0361.2005.tb00096.x. [DOI] [PubMed] [Google Scholar]
- 12.Gilmer T, Kronick R, Rice T. Children welcome, adults need not apply: changes in public program enrollment across states and over time. Med Care Res Rev. 2005;62:56–78. doi: 10.1177/1077558704271723. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell J, Haber S, Hoover S. What happens to children who lose public health insurance coverages? Med Care Res Rev. 2006;63:623–35. doi: 10.1177/1077558706290945. [DOI] [PubMed] [Google Scholar]
- 14.Sommers B. Why millions of children eligible for Medicaid and SCHIP are uninsured: poor retention versus poor take-up. Health Aff. 2007;26:w560–w567. doi: 10.1377/hlthaff.26.5.w560. [DOI] [PubMed] [Google Scholar]
- 15.Raghavan R, Aarons GA, Roesch SC, Leslie LK. Longitudinal patterns of health insurance coverage among a national sample of children in the child welfare system. Am J Public Health. 2008;98:478–84. doi: 10.2105/AJPH.2007.117408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aiken KD, Freed GL, Davis MM. When insurance status is not static: insurance transitions of low-income children and implications for health and health care. Ambul Pediatr. 2004;4:237–43. doi: 10.1367/A03-103R.1. [DOI] [PubMed] [Google Scholar]
- 17.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353:382–91. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 18.Kogan MD, Alexander GR, Teitelbaum MA, Jack BW, Kotelchuck M, Pappas G. The effect of gaps in health insurance on continuity of a regular source of care among preschool-aged children in the United States. JAMA. 1995;274:1429–35. [PubMed] [Google Scholar]
- 19.Smith PJ, Stevenson J, Chu SY. Associations between childhood vaccination coverage, insurance type, and breaks in health insurance coverage. Pediatrics. 2006;117:1972–8. doi: 10.1542/peds.2005-2414. [DOI] [PubMed] [Google Scholar]
- 20.Kane DJ, Zotti ME, Rosenberg D. Factors associated with health care access for Mississippi children with special health care needs. Matern Child Health J. 2005;9:S23–S31. doi: 10.1007/s10995-005-3964-9. [DOI] [PubMed] [Google Scholar]
- 21.Dombkowski K, Lantz P, Freed G. Role of health insurance and a usual source of medical care in age-appropriate vaccination. Am J Public Health. 2004;93:786–91. doi: 10.2105/ajph.94.6.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haas JS, Lee LB, Kaplan CP, Sonneborn D, Phillips KA, Liang SY. The association of race, socioeconomic status, and health insurance status with the prevalence of overweight among children and adolescents. Am J Public Health. 2003;93:2105–10. doi: 10.2105/ajph.93.12.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wood PR, Smith LA, Romero D, Bradshaw P, Wise PH, Chavkin W. Relationships between welfare status, health insurance status, and health and medical care among children with asthma. Am J Public Health. 2002;92:1446–52. doi: 10.2105/ajph.92.9.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens GD, Seid M, Halfon N. Enrolling vulnerable, uninsured but eligible children in public health insurance: association with health status and primary care access. Pediatrics. 2006;117:e751–e759. doi: 10.1542/peds.2005-1558. [DOI] [PubMed] [Google Scholar]
- 25.Flores G, Vega L. Barriers to health care access for Latino children: a review. Fam Med. 1998;30(3):196–205. [PubMed] [Google Scholar]
- 26.DeVoe J, Baez A, Angier H, Krois L, Edlund C, Carney P. Insurance + access does not equal health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;5:511–8. doi: 10.1370/afm.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fairbrother G, Dutton MJ, Bachrach D, Newell K-A, Boozang P, Cooper R. Costs of enrolling children in Medicaid and SCHIP. Health Aff. 2004;23:237–43. doi: 10.1377/hlthaff.23.1.237. [DOI] [PubMed] [Google Scholar]
- 28.DeVoe J, Krois L, Edlund C, Smith J, Carlson N. Uninsurance among children whose parents are losing Medicaid coverage: results from a statewide survey of Oregon families. Health Serv Res. 2008;43:401–18. doi: 10.1111/j.1475-6773.2007.00764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elliot D. Weighting for non-response: a survey’s researcher’s guide. Office of Population Censuses and Surveys, Social Survey Division; London, England: 1991. [Google Scholar]
- 30.Kalton G, Kasprzyk D. The treatment of missing survey data. Survey Methodology. 1986;12:1–16. [Google Scholar]
- 31.Agency for Healthcare Research and Quality . CAHPS 2.0 survey and reporting kit. Agency for Healthcare Research and Quality; Silver Springs, Md: 2002. [Google Scholar]
- 32.Center for Studying Health System Change . Community Tracking Study, Household Survey Instrument 2000-2001, round three. Center for Studying Health System Change; Washington, DC: 2004. Technical publication #54. [Google Scholar]
- 33.Medical Expenditure Panel Survey [Accessed August 20, 2007];Agency for Healthcare Research and Quality. 2004 www.meps.ahrq.gov/mepsweb/
- 34.National Health Interview Survey [Accessed August 20, 2007]; www.cdc.gov/nchs/nhis.htm.
- 35.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–20. [PMC free article] [PubMed] [Google Scholar]
- 36.Children’s health—why insurance matters. Kaiser Family Foundation; [Accessed August 20, 2007]. 2002. www.kff.org/uninsured/4055-index.cfm. [Google Scholar]
- 37.Fairbrother GL, Emerson HP, Partridge L. How stable is Medicaid coverage for children? Health Aff. 2007;26:520–8. doi: 10.1377/hlthaff.26.2.520. [DOI] [PubMed] [Google Scholar]
- 38.Holahan J, Dubay LC, Kenney G. Which children are still uninsured and why. The Future of Children. 2003;13 [PubMed] [Google Scholar]
- 39.Ross DC, Hill IT. Enrolling eligible children and keeping them enrolled. The Future of Children. 2003;13:81–97. [PubMed] [Google Scholar]
- 40.Pati S, Romero D, Chavkin W. Changes in use of health insurance and food assistance programs in medically underserved communities in the era of welfare reform: an urban study. Am J Public Health. 2002;92:1441–5. doi: 10.2105/ajph.92.9.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Remler DK, Glied SA. What other programs can teach us: increasing participation in health insurance programs. Am J Public Health. 2003;93:67–74. doi: 10.2105/ajph.93.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stuber J, Bradley E. Barriers to Medicaid enrollment: who is at risk? Am J Public Health. 2005;95:292–8. doi: 10.2105/AJPH.2002.006254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ullman F, Hill I. Eligibility under State Children’s Health Insurance Programs. Am J Public Health. 2001;91:1449–51. doi: 10.2105/ajph.91.9.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Norris T. Family practice residency programs: agents for positive social change. Fam Med. 1998;30(2):100–2. [PubMed] [Google Scholar]
- 45.Saultz J. Defining basic health benefits: lessons learned from the Oregon Health Plan. Fam Med. 2008;40(6):433–7. [PubMed] [Google Scholar]
- 46.Wright B, Carlson M, Edlund C, DeVoe J, Gallia C, Smith J. The impact of increased cost sharing on Medicaid enrollees. Health Aff. 2005;24:1106–16. doi: 10.1377/hlthaff.24.4.1106. [DOI] [PubMed] [Google Scholar]
- 47.Carlson M, DeVoe J, Wright B. Short-term impacts of coverage loss in a Medicaid population: early results from a prospective cohort study of the Oregon Health Plan. Ann Fam Med. 2006;4:391–8. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Solotaroff R, DeVoe J, Wright B, et al. Medicaid programme changes and the chronically ill: early results from a prospective cohort study of the Oregon Health Plan. Chronic Illness. 2005;1:191–205. doi: 10.1177/17423953050010030301. [DOI] [PubMed] [Google Scholar]
- 49.Annual Report of the National CAHPS Benchmarking Database 2000. US Agency for Healthcare Research and Quality; Rockville, Md: 2003. [Google Scholar]