Abstract
IMPORTANCE
In the United States, health insurance is not universal. Observational studies show an association between uninsured parents and children. This association persisted even after expansions in child-only public health insurance. Oregon’s randomized Medicaid expansion for adults, known as the Oregon Experiment, created a rare opportunity to assess causality between parent and child coverage.
OBJECTIVE
To estimate the effect on a child’s health insurance coverage status when (1) a parent randomly gains access to health insurance and (2) a parent obtains coverage.
DESIGN, SETTING, AND PARTICIPANTS
Oregon Experiment randomized natural experiment assessing the results of Oregon’s 2008 Medicaid expansion. We used generalized estimating equation models to examine the longitudinal effect of a parent randomly selected to apply for Medicaid on their child’s Medicaid or Children’s Health Insurance Program (CHIP) coverage (intent-to-treat analyses). We used per-protocol analyses to understand the impact on children’s coverage when a parent was randomly selected to apply for and obtained Medicaid. Participants included 14 409 children aged 2 to 18 years whose parents participated in the Oregon Experiment.
EXPOSURES
For intent-to-treat analyses, the date a parent was selected to apply for Medicaid was considered the date the child was exposed to the intervention. In per-protocol analyses, exposure was defined as whether a selected parent obtained Medicaid.
MAIN OUTCOMES AND MEASURES
Children’s Medicaid or CHIP coverage, assessed monthly and in 6-month intervals relative to their parent’s selection date.
RESULTS
In the immediate period after selection, children whose parents were selected to apply significantly increased from 3830 (61.4%) to 4152 (66.6%) compared with a nonsignificant change from 5049 (61.8%) to 5044 (61.7%) for children whose parents were not selected to apply. Children whose parents were randomly selected to apply for Medicaid had 18% higher odds of being covered in the first 6 months after parent’s selection compared with children whose parents were not selected (adjusted odds ratio [AOR] = 1.18; 95% CI, 1.10–1.27). The effect remained significant during months 7 to 12 (AOR = 1.11; 95% CI, 1.03–1.19); months 13 to 18 showed a positive but not significant effect (AOR = 1.07; 95% CI, 0.99–1.14). Children whose parents were selected and obtained coverage had more than double the odds of having coverage compared with children whose parents were not selected and did not gain coverage (AOR = 2.37; 95% CI, 2.14–2.64).
CONCLUSIONS AND RELEVANCE
Children’s odds of having Medicaid or CHIP coverage increased when their parents were randomly selected to apply for Medicaid. Children whose parents were selected and subsequently obtained coverage benefited most. This study demonstrates a causal link between parents’ access to Medicaid coverage and their children’s coverage.
Millions of people in the United States lack health insurance coverage. Being uninsured is associated with reduced access to health care services and poorer health outcomes as compared with being insured.1–4 After the 1997 passage of the Children’s Health Insurance Program (CHIP) and its 2009 reauthorization, coverage rates for US children increased dramatically5,6; the number of children insured by CHIP programs rose from 2.2 million in 2000 to 5.3 million in 2011.7 Despite these opportunities to gain insurance, an estimated 7.2 million US children did not have continuous coverage in 2012, many of whom likely qualified for Medicaid or CHIP.8
During the past decade, income thresholds for Medicaid eligibility were more stringent for adults than for children in most US states, making it difficult for adults to qualify for Medicaid coverage.8 Thus, one explanation for children’s lack of coverage despite CHIP expansions may be found in cross-sectional analyses showing that at a given time, when a parent lacks health insurance, his or her child is more likely to be without insurance.9,10 This association has also been reported in many longitudinal studies; however, past research has relied on observational data that limited conclusions about causality.11–14 Oregon’s 2008 randomized Medicaid expansion provides a rare opportunity to investigate a potential causal relationship between insurance coverage for parents and their children. This expansion, often referred to as the Oregon Experiment, is described in detail elsewhere.15–18 Briefly, this unique natural policy experiment gave a subset of uninsured, low-income adults access to Medicaid through a randomized selection process. In 2008, Oregon’s Medicaid program, the Oregon Health Plan (OHP), sought to enroll 10 000 non–categorically eligible (ie, not meeting federally mandated Medicaid eligibility criteria) low-income adults into its expansion program (OHP Standard), which had been closed to new enrollment since 2004. Uninsured, low-income adults were encouraged to put their names on a reservation list. From this list, there were 8 random drawings; individuals selected in these drawings were invited to apply for OHP coverage. The reservation list included more than 90 000 registrants; of these, approximately 30 000 were randomly selected to apply and about 10 000 were ultimately enrolled in OHP.19 Not everyone selected to apply completed an application, and not all applicants met enrollment eligibility criteria.
The opportunity to apply for Medicaid offered by random selection in the Oregon Experiment occurred independent of changes to the family’s socioeconomic status (eg, income or employment). This allowed us to evaluate the effect of a parent’s access to Medicaid on his or her child’s Medicaid or CHIP status independent of the potential for confounding inherent in such a socioeconomic status change. To our knowledge, this is the first study that examines a causal link between a parent gaining access to coverage and a child’s coverage status. We assessed the following: (1) how longitudinal Medicaid or CHIP coverage differed between children whose parents were randomly selected to apply vs children whose parents were registrants on the reservation list but were not selected to apply (intent-to-treat analyses); and (2) differences between coverage for children whose parents were randomly selected to apply and obtained coverage vs those whose parents were not selected and did not obtain coverage (per-protocol analyses).
Methods
This study was approved by the Oregon Health & Science University Institutional Review Board. Consent and authorization were formally waived by the Oregon Health & Science University Institutional Review Board, as the study included no more than minimal risk, the study did not adversely affect the rights or welfare of the participants, and the research could not be practically conducted without the waiver.
Data Sources
The Oregon Experiment’s reservation list includes the registrant’s name, birth date, sex, and address for adults who sought the chance to obtain coverage. It also includes the individual’s randomization status (ie, whether he or she was selected to apply for OHP).19 For some registrants, it also includes a Medicaid unique client identification (ID) number.
The OHP administrative data include individuals’ coverage start and end dates as well as client and house hold ID numbers. Oregon’s Medicaid and CHIP programs are administered jointly through the OHP. These data were used to confirm OHP coverage status over time and to link parents and their children within the study data sets. We used OHP administrative data from adults and children who were enrolled at any time between January 1, 2002, and December 31, 2010. These data were also used to confirm the subpopulation of individuals selected to apply from the reservation list who successfully obtained OHP coverage.
OCHIN is a collaboration of health systems with more than 300 ambulatory care clinics. Originally the Oregon Community Health Information Network, it was renamed OCHIN, Inc when it expanded beyond Oregon (now in >20 states). Member clinics share a centrally hosted EpicCare electronic health record (EHR) with an enterprise-wide master patient index.20 The OCHIN network clinics serve a large portion of the OHP population.20,21 We used OCHIN EHR data from patients seen in an Oregon clinic between January 1, 2002, and December 31, 2010, to identify adults in the Oregon Experiment who did not gain OHP coverage during the study period as well as adults and children who were not in the OHP records.
Data Matching, Linkages, and Study Population
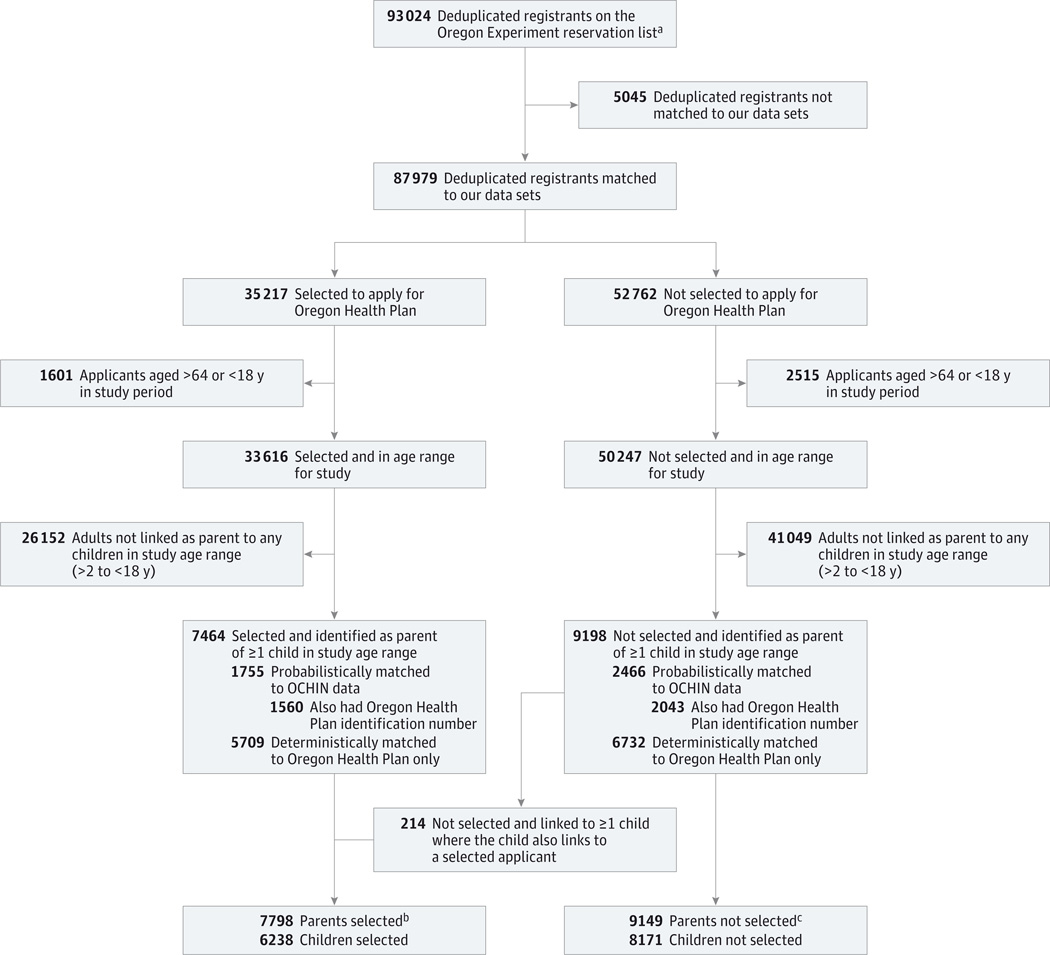
Of the 93 024 deduplicated registrants from the reservation list (Figure 1), 48 872 were deterministically matched to OHP administrative data only (not found in the OCHIN data set) and 39 107 were probabilistically matched to the OCHIN EHR (of whom 34 084 were also matched to the OHP data). We used Link Plus (Centers for Disease Control and Prevention) to probabilistically match reservation list registrants to the OCHIN EHR through demographic variables common to both data sets. Two research staff members (H.A. and S.R.B.) independently performed case-by-case review of uncertain matches. Of the 87 979 matched registrants, 35 217 were selected to apply for coverage and 52 762 were not selected to apply. We created parent-child linkage algorithms to determine which of these adults could be linked with children (aged 2–18 years) in the OHP and/or OCHIN data sets. Parents were linked to children using household case ID numbers (OHP administrative data set) as well as emergency contact information and financial guarantor data (OCHIN EHR data set). Information on creation and validation of our linkage algorithms can be found elsewhere.22 Through this process, we linked 16 662 parents with children (n = 7464 selected; n = 9198 not selected). From these parents, we randomly selected 1 child per household for our analyses (n = 14 409), as the high intraclass correlation of coverage status among siblings within a family (intraclass correlation ≥0.90 in all study months) would produce unstable models.
Figure 1.
Study Population Flow Diagram
aWe deduplicated the list as people could register for the lottery multiple times.
bMore than 1 applicant per household could be included. Households were defined by the mother, and 120 fathers were in more than 1 household.
cMore than 1 applicant per household could be included. Households were defined by the mother, and 165 fathers were in more than 1 household.
All adults in the household of a registrant selected in the randomization process were allowed to apply for Medicaid. For this reason, in the intent-to-treat analyses, children were put into 2 categories: (1) at least 1 parent randomly selected to apply for OHP (n = 7798 adults; n = 6238 children); and (2) no parent randomly selected to apply for OHP (n = 9149 adults; n = 8171 children). Per-protocol analyses included the following subpopulations: (1) at least 1 parent selected to apply and obtained OHP coverage (n = 3354 adults; n = 2577 children); and (2) no parent randomly selected to apply for OHP and no parent obtained coverage (n = 7436 adults; n = 6675 children).
Study Variables
The primary independent variable for intent-to-treat analyses was whether a parent was randomly selected to apply for OHP coverage. The parental selection date was considered the date the child was exposed to the intervention. Based on the distribution of these dates, we randomly assigned a selection date to children whose parents were not selected (non-exposed controls). In per-protocol analyses, comparison groups were selected parents who obtained OHP coverage vs parents who were not selected and did not obtain OHP coverage.
The primary outcome was children’s OHP coverage, assessed monthly and in 6-month intervals relative to the Oregon Experiment selection date of their parent(s). These 6-month intervals were chosen because adults who received OHP insurance were covered for 6 months before they were required to reapply. The distribution of coverage was strongly bimodal, with more than 80% of children having either 0% or 100% coverage in any given period. For both parent and child, those with 50% or more coverage during a given interval were considered insured; those with less than 50% coverage were considered uninsured. We considered as potential covariates those previously shown to affect coverage: age of the child and parent at selection date, race/ethnicity of the parent and child, number of children in the household, child’s sex, number of linked parents, percentage of the population in the child’s zip code taking part in the food stamp program, and Rural-Urban Continuum Code for the zip code.10,23–27 We also considered as a covariate whether the parent registrant was probabilistically or deterministically matched to the reservation list.
Statistical Analysis
We compared baseline characteristics between the selected and nonselected groups using Pearson χ2 tests for categorical variables and Wilcoxon tests of differences for continuous variables. To examine the longitudinal effect of parental selection on child’s insurance, we used a generalized estimating equation (GEE) model with a logit link and robust sandwich variance estimator to account for the temporal correlation of children’s coverage during the study period. This model used child’s insurance status in a given month as the outcome and was evaluated in each of the 18 months before and after the parental selection date. To estimate the effect parental selection status had on children’s coverage after the selection date (intent-to-treat analyses), we used GEE models (as described earlier) limited to the 18 months after selection and summarizing the child’s insurance for three 6-month intervals (0–6 months, 7–12 months, and 13–18 months after the parental selection date). We conducted per-protocol analyses using GEE models limited to children whose parents were selected and obtained OHP coverage (covered ≥50% of the time) in the first 6 months after the selection date (intervention group) and children whose parents were not selected and did not have OHP coverage in the first 6 months after selection (controls). In both the intent-to-treat and per-protocol models, we adjusted for covariates that significantly differed between the 2 groups at baseline. We report odds ratios (ORs) in this study, and these estimates do not approximate relative risk because coverage is not rare in this study population.28
Analyses were conducted using SAS version 9.4 (SAS Institute, Inc) and R version 2.15.2 (R Foundation for Statistical Computing) statistical software. P < .05 was considered statistically significant for all analyses.
Results
There were no significant differences at baseline between the selected and unselected groups in parent’s age or in child’s age, race/ethnicity, and sex. The groups differed on parent’s race/ethnicity (P = .004), number of children in the household (P < .001), number of parent registrants in the household on the reservation list (P < .001), Rural-Urban Continuum Code for the child’s zip code (P = .006), and whether at least 1 parent registrant from the reservation list was probabilistically matched to OCHIN EHR data (P < .001) (Table 1).
Table 1.
Study Population Characteristics With Parents Selected to Apply vs Not Selected to Apply for OHP Coverage
| Characteristic | Parent Selecteda | Parent Not Selectedb |
P Valuec |
|---|---|---|---|
| Parent registrants, No. | 7798 | 9149 | |
| Children, No. | 6238 | 8171 | |
| Age, mean (SD), y | |||
| Parent | 36.2 (8.3) | 36.4 (8.3) | .09 |
| Child | 9.7 (4.2) | 9.9 (4.1) | .51 |
| Ethnicity/race, No. (%) | |||
| Parent | |||
| Hispanic, any race | 513 (6.6) | 656 (7.2) | .004 |
| Non-Hispanic, white | 5297 (67.9) | 6370 (69.6) | |
| Non-Hispanic, nonwhite | 834 (10.7) | 914 (10.0) | |
| Not collected or unknown | 1154 (14.8) | 1209 (13.2) | |
| Child | |||
| Hispanic, any race | 518 (8.3) | 669 (8.2) | .62 |
| Non-Hispanic, white | 3619 (58.0) | 4760 (58.2) | |
| Non-Hispanic, nonwhite | 662 (10.6) | 817 (10.0) | |
| Not collected or unknown | 1439 (23.1) | 1925 (23.6) | |
| Children per household, No. (%) | |||
| 1 | 1554 (24.9) | 2284 (27.9) | <.001 |
| 2 | 2179 (34.9) | 2917 (35.7) | |
| ≥3 | 2505 (40.2) | 2907 (36.4) | |
| Sex of child, No. (%) | |||
| Male | 3231 (51.8) | 4233 (51.8) | .98 |
| Female | 3004 (48.2) | 3933 (48.2) | |
| Parent registrants on Oregon Experiment reservation list, No. (%) | |||
| 1-Parent families | 2885 (46.3) | 4385 (53.6) | <.001 |
| 2-Parent families | |||
| 1 Parent registrant | 1793 (28.7) | 2811 (34.4) | |
| 2 Parent registrants | 1560 (25.0) | 978 (12.0) | |
| Rural-Urban Continuum Code, No. (%) | |||
| Metropolitan population, >1 000 000 | 2508 (40.2) | 3426 (41.9) | .006 |
| Metropolitan population, 250 000–1 000 000 | 1236 (19.8) | 1710 (20.9) | |
| Metropolitan population, 2500–250 000 | 777 (12.5) | 927 (11.4) | |
| Rural population, <2500 | 1717 (27.5) | 2108 (25.8) | |
| Data source for parental match to reservation list, No. (%) | |||
| Deterministically matched to OHP | 3148 (50.5) | 3682 (45.1) | <.001 |
| Probabilistically matched to OCHIN EHRd | 3090 (49.5) | 4489 (54.9) | |
| Duration of child’s OHP coverage in month prior to Oregon Experiment selection date of parent(s) to apply for OHP coverage, No. (%) |
|||
| ≥50% | 3809 (61.1) | 4934 (60.4) | .38 |
| <50% | 2429 (38.9) | 3240 (39.6) |
Abbreviations: EHR, electronic health record; OHP, Oregon Health Plan.
At least 1 parent randomly selected to apply for OHP.
No parent randomly selected to apply for OHP.
From χ2 test for categorical variables and Wilcoxon rank sum test for continuous variables.
Includes those who also had an OHP identification number.
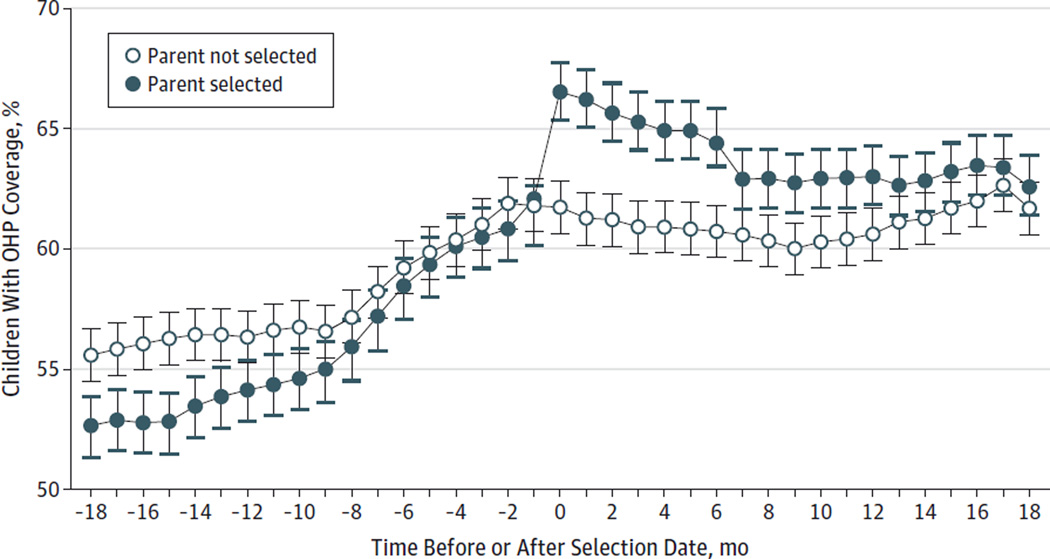
Figure 2 demonstrates the percentage of children covered by OHP for 50% of days or more in a given month, adjusted for covariates significantly different between the 2 groups. In most of the 18-month period before the parental selection date, there was no significant difference in coverage between the 2 groups. In the immediate period after selection, there was a significant increase in OHP coverage rates among children whose parents were selected to apply (from 61.4% [n = 3830] to 66.6% [n = 4152]) compared with children with no parent selected (from 61.8% [n = 5049] to 61.7% [n = 5044]) (P < .001). The percentage of children with OHP coverage remained significantly higher in the selected group for the first 12 months of the period after selection (63.1% [n = 3937] with parent selected vs 60.6% [n = 4952] with no parent selected at month 12; P < .001).
Figure 2.
Percentage of Children With Oregon Health Plan (OHP) Coverage 18 Months Before and After Random Selection of Parents to Apply for OHP Coverage
For the parent selected group, the selection date was the date on which a parent was randomly selected to apply for OHP coverage (the date a child was exposed to the intervention). Based on this distribution of selection dates for the intervention group, a selection date was randomly assigned to children whose parents were not selected (nonexposed controls). Predicted percentages are based on a logit generalized estimating equation model adjusted for covariates found to be significantly different between selected and unselected groups, including parent’s race/ethnicity, number of children in the household, number of parents in the household on the reservation list, Rural-Urban Continuum Code for the child’s zip code, and whether either parent registrant from the reservation list was probabilistically matched to OCHIN electronic health record data. Error bars indicate 95% CIs for the percentage of children with OHP coverage at each time point.
In intent-to-treat analyses (Table 2), children whose parents were randomly selected to apply for OHP had higher odds of coverage in the first 6-month period after selection compared with those whose parents were not selected (unadjusted OR = 1.26; 95% CI, 1.18–1.35; adjusted OR = 1.18; 95% CI, 1.10–1.27). The effect of parent selection remained significant during months 7 to 12 in both unadjusted (OR = 1.19; 95% CI, 1.11–1.27) and adjusted (OR = 1.11; 95% CI, 1.03–1.19) analyses. Unadjusted analyses show a continued positive effect of parent selection in months 13 to 18 (OR = 1.14; 95% CI, 1.06–1.22); the effect was not significant in adjusted analyses (OR = 1.07; 95% CI, 0.99–1.14). In adjusted per-protocol analyses, children whose parents were selected and obtained OHP coverage had more than double the odds of being insured in the first 6-month period after selection compared with children whose parents were not selected (OR = 2.37; 95% CI, 2.14–2.64); this positive effect remained significant across the study period in all models. Results were similar when GEE analyses were stratified by number of parent registrants (eTable in the Supplement).
Table 2.
Effects of Parent Selection to Apply for OHP Coverage and of Selected Parent(s) Obtaining Coverage on Children Obtaining OHP Coverage
| Children With OHP Coverage by Time After Parent Selectiona | ||||||
|---|---|---|---|---|---|---|
| 1–6 mo | 7–12 mo | 13–18 mo | ||||
| Model | %b | OR (95% CI) | %b | OR (95% CI) | %b | OR (95% CI) |
| Intent-to-treat analysesc | ||||||
| Unadjusted | ||||||
| Parent selectedd | 65.8 | 1.26 (1.18–1.35) | 63.1 | 1.19 (1.11–1.27) | 63.2 | 1.14 (1.06–1.22) |
| Parent not selectede | 60.5 | 1 [Reference] | 59.0 | 1 [Reference] | 60.2 | 1 [Reference] |
| Adjustedf | ||||||
| Parent selectedd | 65.5 | 1.18 (1.10–1.27) | 62.6 | 1.11 (1.03–1.19) | 62.8 | 1.07 (0.99–1.14) |
| Parent not selectede | 61.6 | 1 [Reference] | 60.1 | 1 [Reference] | 61.3 | 1 [Reference] |
| Per-protocol analysesg | ||||||
| Unadjusted | ||||||
| Parent selected and obtained OHP coverageh |
76.5 | 2.55 (2.30–2.82) | 70.6 | 1.92 (1.75–2.21) | 69.4 | 1.67 (1.52–1.84) |
| Parent not selected and did not obtain OHP coveragei |
56.0 | 1 [Reference] | 55.5 | 1 [Reference] | 57.6 | 1 [Reference] |
| Adjustedf | ||||||
| Parent selected and obtained OHP coverageh |
75.9 | 2.37 (2.14–2.64) | 69.7 | 1.77 (1.60–1.96) | 68.4 | 1.53 (1.38–1.69) |
| Parent not selected and did not obtain OHP coveragei |
57.0 | 1 [Reference] | 56.5 | 1 [Reference] | 58.6 | 1 [Reference] |
Abbreviations: OHP, Oregon Health Plan; OR, odds ratio.
A child was classified as covered if there was evidence of OHP coverage for more than 50% of the period.
The unadjusted percentages are the observed percentage; the adjusted percentages are estimated from predicted probability of coverage from the models.
To estimate the effect parental selection status had on children’s coverage, we used generalized estimating equation modeling limited to 18 months after a parent was selected to apply for OHP (those not selected were randomly assigned a selection date based on the distribution of selection dates for the selected group).
At least 1 parent was randomly selected to apply for OHP (n = 7798 adults; n = 6238 children).
No parent was randomly selected to apply for OHP (n = 9149 adults; n = 8171 children).
Adjusted for covariates found to be significantly different between selected and unselected groups, including parent’s race/ethnicity, number of children in the household, number of parents in the household on the reservation list, Rural-Urban Continuum Code for the child’s zip code, and whether either parent registrant from the reservation list was probabilistically matched to OCHIN electronic health record data. Missing parental race/ethnicity was included in the models as a separate category with the parental race/ethnicity variable.
To estimate the effect of a parent being selected and obtaining coverage, we used generalized estimating equation modeling limited to children whose parents were selected and received OHP coverage in the first 6 months after the selection date (intervention group) and children whose parents were not selected and did not get OHP coverage in the first 6 months after selection (controls).
At least 1 parent selected to apply ultimately obtained OHP coverage after selection (n = 3354 adults; n = 2577 children).
No parent was randomly selected to apply for OHP and no parent obtained coverage (n = 7436 adults; n = 6675 children).
Discussion
Past studies of the Oregon Experiment examined the impact of expanded OHP coverage on adults’ health care use, financial strain, and health outcomes.15–18 We assessed how increased parental access to Medicaid in the Oregon Experiment affected children’s coverage. We found higher OHP coverage rates among children whose parents were randomly selected to apply for OHP vs those not selected. There was an even stronger positive effect on children’s OHP coverage when parents were selected and obtained OHP coverage. This suggests that expanding parental access to Medicaid coverage will have a positive impact on children’s public health insurance rates.
Our findings confirm previous studies showing significantly higher rates of children’s coverage when a parent is covered,9–14 and they strengthen this knowledge by demonstrating a causal link between access to Medicaid for parents and their children. In the Oregon Experiment, parents’ access to coverage was not due to a family’s changed socioeconomic status or changed insurance eligibility (eg, new job, increased pay) that would have directly affected their child’s coverage. Additionally, all children in the study (those with selected and nonselected parents) had equal access to Medicaid or CHIP available during the study period; thus, the higher OHP coverage rates among children whose parents were selected cannot be explained by these children having preferential access to this coverage.
One plausible explanation for our findings is that when an adult in the household was selected to apply for OHP coverage, it created an impetus to submit an application for everyone in the family. Qualitative studies found that some parents without their own OHP coverage were unaware that their children were eligible for coverage.9,10 Similarly, many parents who lost coverage when OHP scaled back its program for non–categorically eligible adults believed their children were no longer eligible.29,30 Involvement in the Oregon Experiment may have alerted such participants to their children’s eligibility.
Additionally, 6 months after adults obtained coverage, they were required to reenroll, which led to the loss of coverage for many adults.25 For children, the OHP reenrollment period is 12 months. This eventual loss of coverage among many adults who obtained coverage in the Oregon Experiment might explain why the parental selection effect on children’s coverage was not significant 13 to 18 months after selection in the adjusted intent-to-treat models and why the OR decreased over time in the per-protocol models.
Policy Implications
The Oregon Experiment, which intended to give adults access to Medicaid, also had a positive impact on children’s coverage. In other words, a policy with the “intent to treat” adults also increased children’s coverage. The positive effect of parental selection on children’s coverage was magnified when a selected parent obtained coverage. Findings from this study suggest that one way to maximize Medicaid insurance for children is to ensure parents have the ability to obtain coverage. The Patient Protection and Affordable Care Act of 2010 has provided adults with new coverage opportunities. As more parents gain coverage, it is likely that children’s rates will also improve. To ensure that eligible children obtain coverage, states should participate in Medicaid expansions and other programs created by the Patient Protection and Affordable Care Act of 2010 to increase insurance options for parents and children.31–34 There is a need for additional research to closely monitor whether parents are churning on and off available programs due to income fluctuations and how these parental gains and losses affect families.35–37
Limitations
Using OCHIN EHR data, we captured more households than would have been possible using OHP administrative data alone. The OCHIN data allowed identification of parental linkages without requiring that both parent and child be insured by Medicaid at some point. It also allowed the capture of registrants who had OHP ID numbers but did not list them on their registration forms and of patients who did not receive OHP ID numbers because they did not apply for insurance (because they either were not selected or chose not to apply). Although we do not expect the capture of children linked to lottery applicants afforded by the use of OCHIN EHR data to create bias, the linkage source differed between the intervention groups, which means there could be confounding associated with parental OCHIN patient status. We included the data source for parental match as a covariate in our modeling to control for this, but potential bias may still be present. To avoid model instability, we randomly selected 1 child from each household, which limited our sample size; however, the high intraclass correlation in insurance coverage between siblings suggests this approach would not create bias. Missing values in the race/ethnicity variable were considered as a category instead of being removed in our analyses; no other values in the study population characteristics were missing as the data systems we used have strong data collection mechanisms on the included covariates. The percentage of racial and ethnic minority participants in our study was lower than national population estimates but similar to Oregon’s.38
It is possible, but not likely, that parents not selected in the Oregon Experiment sought private coverage for themselves and their children; rates of private coverage have declined for American families in the past decade,39,40 and a very small percentage (<7%) of the OCHIN parents and children in our study population ever had private coverage. This study was conducted in 1 state; results may differ in other states with different Medicaid policies.
Conclusions
Children whose parents were randomly selected to apply for coverage through the Oregon Experiment had higher rates of OHP coverage than children whose parents were not selected. Among children whose parents were selected, those whose parents obtained coverage benefited the most. This study demonstrates a causal link between Medicaid coverage for parents and their children. To maximize children’s health insurance coverage rates, parents must also have opportunities to obtain coverage.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported by grant 1 R01 HS018569 from the Agency for Healthcare Research and Quality and by the Department of Family Medicine, Oregon Health & Science University.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Drs DeVoe and Marino had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: DeVoe, Marino, Angier, O’Malley, Bailey, Gallia, Gold.
Acquisition, analysis, or interpretation of data: DeVoe, Marino, Angier, O’Malley, Crawford, Nelson, Tillotson, Gold.
Drafting of the manuscript: Marino, Angier, O’Malley.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Marino, O’Malley, Crawford.
Obtained funding: DeVoe, Gold.
Administrative, technical, or material support: Angier, Nelson, Gallia.
Study supervision: DeVoe, Angier, Gold.
Conflict of Interest Disclosures: None reported.
REFERENCES
- 1.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 2.Hadley J. Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. JAMA. 2007;297(10):1073–1084. doi: 10.1001/jama.297.10.1073. [DOI] [PubMed] [Google Scholar]
- 3.Kaiser Commission on Medicaid and the Uninsured. The uninsured and the difference health insurance makes. [Accessed August 9, 2013]; http://kff.org/health-reform/fact-sheet/the-uninsured-and-the-difference-health-insurance/ [Google Scholar]
- 4.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027–1037. doi: 10.1542/peds.2012-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dubay L, Guyer J, Mann C, Odeh M. Medicaid at the ten-year anniversary of SCHIP: looking back and moving forward. Health Aff (Millwood) 2007;26(2):370–381. doi: 10.1377/hlthaff.26.2.370. [DOI] [PubMed] [Google Scholar]
- 6.Kenney G, Yee J. SCHIP at a crossroads: experiences to date and challenges ahead. Health Aff (Millwood) 2007;26(2):356–369. doi: 10.1377/hlthaff.26.2.356. [DOI] [PubMed] [Google Scholar]
- 7.Smith V, Snyder L, Rudowitz R. CHIP Enrollment: June 2011 Data Snapshot. Washington, DC: Kaiser Family Foundation; 2012. [Google Scholar]
- 8.Kaiser Commission on Medicaid and the Uninsured. The uninsured: a primer—key facts about health insurance on the eve of coverage expansions. [Accessed January 10, 2014]; http://kff.org/report-section/the-uninsured-a-primer-2013-2-who-are-the-uninsured/ [Google Scholar]
- 9.DeVoe JE, Krois L, Edlund T, Smith J, Carlson NE. Uninsurance among children whose parents are losing Medicaid coverage: results from a statewide survey of Oregon families. Health Serv Res. 2008;43(1, pt 2):401–418. doi: 10.1111/j.1475-6773.2007.00764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeVoe JE, Krois L, Edlund C, Smith J, Carlson NE. Uninsured but eligible children: are their parents insured? recent findings from Oregon. Med Care. 2008;46(1):3–8. doi: 10.1097/MLR.0b013e31815b97ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeVoe JE, Tillotson CJ, Angier H, Wallace LS. Recent health insurance trends for US families: children gain while parents lose. Matern Child Health J. 2014;18(4):1007–1016. doi: 10.1007/s10995-013-1329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angier H, DeVoe JE, Tillotson C, Wallace L, Gold R. Trends in health insurance status of US children and their parents, 1998–2008. Matern Child Health J. 2013;17(9):1550–1558. doi: 10.1007/s10995-012-1142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubay L, Kenney G. Expanding public health insurance to parents: effects on children’s coverage under Medicaid. Health Serv Res. 2003;38(5):1283–1301. doi: 10.1111/1475-6773.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sommers BD. Insuring children or insuring families: do parental and sibling coverage lead to improved retention of children in Medicaid and CHIP? J Health Econ. 2006;25(6):1154–1169. doi: 10.1016/j.jhealeco.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Baicker K, Finkelstein A. The effects of Medicaid coverage: learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen H, Baicker K, Finkelstein A, Taubman S, Wright BJ Oregon Health Study Group. What the Oregon Health Study can tell us about expanding Medicaid. Health Aff (Millwood) 2010;29(8):1498–1506. doi: 10.1377/hlthaff.2010.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Finkelstein A, Taubman S, Wright B Oregon Health Study Group. The Oregon Health Insurance Experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–268. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oregon Division of Medical Assistance Programs. OHP standard reservation list final report, March through October 2008. [Accessed May 31, 2013]; http://www.oregon.egov.com/oha/healthplan/DataReportsDocs/OHP%20Standard%20Reservation%20List%20Final%20Report.pdf.
- 20.Devoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-Based Research Network (SNW-PBRN) J Am Board Fam Med. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hatch B, Angier H, Marino M. Using electronic health records to conduct children’s health insurance surveillance. Pediatrics. 2013;132(6):e1584–e1591. doi: 10.1542/peds.2013-1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Angier H, Gold R, Crawford C, et al. Linkage methods for connecting children with parents in electronic health record and state public health insurance data. Matern Child Health J. 2014;18(9):2025–2033. doi: 10.1007/s10995-014-1453-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fairbrother G, Madhavan G, Goudie A, et al. Reporting on continuity of coverage for children in Medicaid and CHIP: what states can learn from monitoring continuity and duration of coverage. Acad Pediatr. 2011;11(4):318–325. doi: 10.1016/j.acap.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 24.DeVoe JE, Graham A, Krois L, Smith J, Fairbrother GL. “Mind the gap” in children’s health insurance coverage: does the length of a child’s coverage gap matter? Ambul Pediatr. 2008;8(2):129–134. doi: 10.1016/j.ambp.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Department of Agriculture. Rural-Urban Continuum Codes. [Accessed August 22, 2013]; http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.aspx.
- 26.US Department of Agriculture. Supplemental Nutrition Assistance Program (SNAP) data system. [Accessed August 22, 2013]; http://www.ers.usda.gov/data-products/supplemental-nutrition-assistance-program-(snap)-data-system.aspx.
- 27.Hill HD, Shaefer HL. Covered today, sick tomorrow? trends and correlates of children’s health insurance instability. Med Care Res Rev. 2011;68(5):523–536. doi: 10.1177/1077558711398877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cummings P. The relative merits of risk ratios and odds ratios. Arch Pediatr Adolesc Med. 2009;163(5):438–445. doi: 10.1001/archpediatrics.2009.31. [DOI] [PubMed] [Google Scholar]
- 29.DeVoe JE, Ray M, Graham A. Public health insurance in Oregon: underenrollment of eligible children and parental confusion about children’s enrollment status. Am J Public Health. 2011;101(5):891–898. doi: 10.2105/AJPH.2010.196345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeVoe JE, Westfall N, Crocker S, et al. Why do some eligible families forego public insurance for their children? a qualitative analysis. Fam Med. 2012;44(1):39–46. [PMC free article] [PubMed] [Google Scholar]
- 31.Office of the Legislative Counsel. Compilation of Patient Protection and Affordable Care Act. [Accessed December 16, 2011];111th Congress, 2nd Sess. 2010 http://housedocs.house.gov/energycommerce/ppacacon.pdf.
- 32.Kenney G, Dubay L, Zuckerman S, Huntress M. Making the Medicaid expansion an ACA option: how many low-income Americans could remain uninsured. [Accessed May 31, 2013]; http://www.urban.org/publications/412606.html. [Google Scholar]
- 33.Kaiser Family Foundation. The Coverage Gap: Uninsured Poor Adults in States That Do Not Expand Medicaid. Washington, DC: Kaiser Family Foundation; 2013. [Google Scholar]
- 34.Rasmussen PW, Collins SR, Doty MM, Garber T. In states’ hands: how the decision to expand Medicaid will affect the most financially vulnerable Americans: findings from the Commonwealth Fund Health Insurance Tracking Surveys of US Adults, 2011 and 2012. Issue Brief (Commonw Fund) 2013;23:1–8. [PubMed] [Google Scholar]
- 35.Sommers BD, Rosenbaum S. Issues in health reform: how changes in eligibility may move millions back and forth between Medicaid and insurance exchanges. Health Aff (Millwood) 2011;30(2):228–236. doi: 10.1377/hlthaff.2010.1000. [DOI] [PubMed] [Google Scholar]
- 36.Short PF, Graefe DR, Swartz K, Uberoi N. New estimates of gaps and transitions in health insurance. Med Care Res Rev. 2012;69(6):721–736. doi: 10.1177/1077558712454195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Collins SR, Robertson R, Garber T, Doty MM. Gaps in health insurance: why so many Americans experience breaks in coverage and how the Affordable Care Act will help: findings from the Commonwealth Fund Health Insurance Tracking Survey of US Adults, 2011. Issue Brief (Commonw Fund) 2012;9:1–22. [PubMed] [Google Scholar]
- 38.US Census Bureau. US Census Bureau fact finder. [Accessed July 8, 2014]; http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- 39.Gould E. Employer-sponsored health insurance erosion continues in 2008 and is expected to worsen. Int J Health Serv. 2010;40(4):743–776. doi: 10.2190/HS.40.4.j. [DOI] [PubMed] [Google Scholar]
- 40.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2012 Current Population Survey. EBRI Issue Brief. 2012;(376):1–34. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.