Depression ranks second in terms of global burden of disease (Ferrari et al., 2013) and world-wide depression is the most commonly encountered mental health problem among women (Piccinelli & Wilkinson, 2000). Globally, the prevalence of depression among adults with chronic conditions is significantly higher than among those without chronic conditions (Moussavi et al., 2007). Specifically, the study of depression and hypertension is an emerging area of research. Coexisting depression with hypertension is related to decrements in health. Although there is evidence of improved health due to depression treatment, there is very little research on whether depression is treated and on patterns of depression treatment when depression co-exists with chronic conditions. Research is warranted on depression treatment patterns among women with hypertension and depression because both conditions are highly prevalent among women and differences in the pharmacokinetic disposition of antidepressants, a main mode of treatment for depression may lead to differential patterns of depression treatment. Therefore, in our current study, we examine factors associated with depression treatment among non-pregnant women with hypertension based on the Andersen Behavioral Model (ABM) for Health Services Utilization. We believe that our study makes an important contribution regarding the emerging literature on depression treatment in the presence of chronic medical illnesses, specifically hypertension.
High prevalence of depression in individuals with hypertension and the relationship between the two conditions is an emerging area of research. Those with hypertension are more likely to develop depression and those with depression may be more likely to develop hypertension (Scalco, Scalco, Azul, & Lotufo, 2005). While depression is reported as a risk factor for incident hypertension (Meyer, Armenian, Eaton, & Ford, 2004), the relationship between depression and incident hypertension is inconsistent with positive, negative and borderline associations being detected (Goldberg, 2010). Whatever the direction of the relationship may be, when depression and hypertension co-exist, depression negatively affects health outcomes, incidence of stroke, and management of hypertension through non-adherence to antihypertensive medications. Among men and women enrolled in a randomized placebo-controlled double-blind clinical trial of antihypertensive therapy, an increase in depressive symptoms overtime was associated with increased mortality, risk of stroke or myocardial infarction (Wassertheil-Smoller et al., 1996). In another study conducted in the United States, the investigators reported that depressive symptoms were associated with lower rate of blood pressure control only among women in one state (Simonsick, Wallace, Blazer, & Beckman, 1995). Compared to elderly with hypertension and no depression, those with hypertension and depression were significantly more likely to have a stroke (Simonsick et al., 1995). In addition, Wang et al. (2002) reported that an increase in depressive symptoms was significantly associated with lower odds of medication adherence to antihypertensive medications.
Although depression is a highly prevalent mental health condition worldwide (World Health Organization [WHO], 2014), there is no investigation specific to the prevalence of co-occurring hypertension and depression. For example, Moussavi et al. (2007) conducted a study utilizing the World Health Survey and found that a one-year prevalence of depression was only reported for four chronic physical conditions and did not include hypertension. While not specific to hypertension, there is great unmet need in terms of depression treatment across different countries of the world. Depression treatment varies from 30-50% in developed countries and 76%-80% in low and middle income countries (LAMIC) (Saxena, Thornicroft, Knapp, & Whiteford, 2007). For example, Wang et al. (2007) reported that the percentage of adequate depression treatment ranged from 10% in Nigeria to 42% in France. In an international study conducted at six locations around the world [Barcelona (Spain), Be'er Sheva (Israel), Melbourne (Australia), Porto Alegre (Brazil), St. Petersburg (Russia), and Seattle (United States)], Simon et al. (2004) reported that even after being diagnosed with depression, individuals were less likely to get depression treatment; again the percentage of adequate depression treatment did not exceed 40% in any of the sites.
Depression treatment among women with hypertension and depression is especially important because of the following reasons. Women are more likely to be diagnosed with depression (20.2% vs. 8.2%) than men possibly due to biological, life cycle, hormonal and psychosocial factors unique to women (Centers for Disease Control & Prevention, 2011). The pharmacokinetic disposition of antidepressants vary between men and women, and women taking antidepressants may exhibit a different adverse event profile, which may result in treatment differences found among women (Frackiewicz, Sramek, & Cutler, 2006). Among women with hypertension, increased depressive symptoms were the strongest risk factor for stroke (Wassertheil-Smoller et al., 1996).
Improvements in depression may occur more rapidly with brief interpersonal psychotherapy than with sertraline (Swartz, et al., 2004). This may result in women using psychotherapy more rather than antidepressants. In addition, there may be subgroup variations in depression treatment that are specific to women. For example, treatment patterns by race in women may be distinctive because of differences in stigmatization between men and women (Hobfall et al., 1995). While there may be the greater mental health stigma among African Americans in general (Copper-Patrick et al., 1997), it is more so in African American women compared to White women (Menke & Flynn, 2009). Factors such as those mentioned above may lead to depression treatment patterns that may be unique to women.
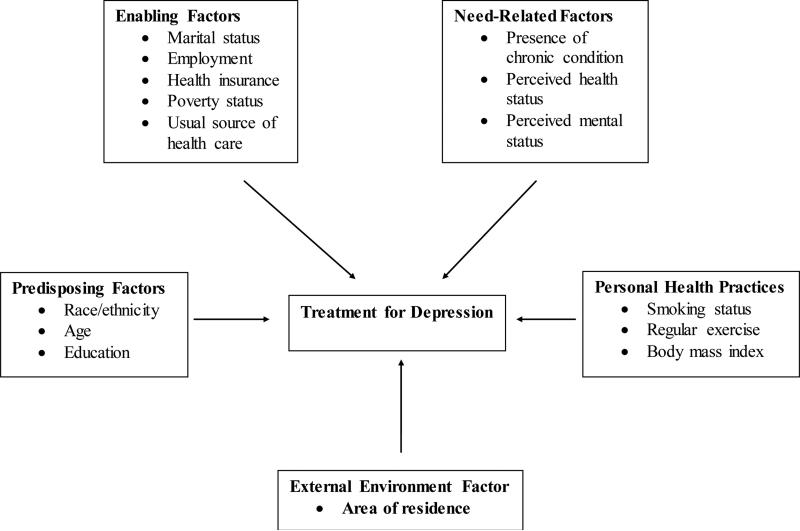
Examination of depression treatment among women may lead to a better understanding of treatment related issues that are specific to women when the two diseases co-occur. Therefore, we examined the rates of depression treatment and variations in depression treatment by a host of factors based on the Andersen Behavioral Model (ABM) for Health Services Utilization (predisposing, enabling, need-related, personal health practices, and external factors) among non-pregnant women with hypertension. The ABM posits that individual's use of health services can be determined by predisposition to use services, factors which enable or impede use, and the need for care (Andersen, 1995; Andersen & Newman, 1973).
METHODS
We used a cross-sectional design to examine depression treatment patterns among women with co-existing depression and hypertension. We included women aged 22 and older with hypertension and depression (N=1,304), using data derived from 2006 and 2007 Medical Expenditure Panel Survey (MEPS). We pooled two years of the MEPS to gain an ample sample size.
MEPS is a nationally representative survey of families and individuals, their medical providers, and employers across the United States (Agency for Healthcare Research & Quality [AHRQ], 2011a). MEPS collects data on the specific health services that Americans use, how frequently they use them, the cost of these services, and how they are paid for, as well as data on the cost, scope, and breadth of health insurance held by and available to US workers, and it is the most complete source of data on the cost and use of health care and health insurance coverage (AHRQ, 2011a).
Women with hypertension were identified from the medical conditions file and the household file. Within MEPS, medical conditions of household members were derived from the medical condition file as well as the full-year population characteristics file. In the full-year population characteristics file, individual's responses to queries on ever having hypertension were recorded. The medical condition file was used to identify depression during the year.
In the MEPS, verbatim text was transformed to corresponding International Classification of Diseases, 9th Edition (ICD-9) and procedure codes by professional coders. Specific guidelines were followed to ensure that conditions were coded as accurately as possible and that missing values were handled properly. Due to confidentiality reasons, only 3-digit ICD-9 codes were made available to the researchers. However, MEPS also converted 5-digit ICD-9 codes to 3-digit clinical classification codes. Details of this conversion are described elsewhere (AHRQ, 2011a). We used both 3-digit ICD-9 codes and clinical classification codes to identify women with hypertension and depression.
We restricted our sample to age 22 and older because the study sample may have included women in college but depression in student population was beyond the scope of the study. We also excluded women who were pregnant during the year because of special considerations of antidepressant treatment during pregnancy (Yonkers et al., 2009). Pregnant women were identified using an algorithm published in prior research (Chatterjee, Kotelchuck, & Sambamoorthi, 2008) and were excluded.
Dependent Variable
The dependent variable was treatment for depression. Treatment for depression consisted of antidepressant use and/or psychotherapy (Bostwick, 2010). For antidepressant use, antidepressant medications were identified from prescription drug files using therapeutic sub-classification categories assigned to each drug using Multum Lexicon variables from Cerner Multum, Inc. We used the therapeutic sub-classification code “249” which represented antidepressants (AHRQ, 2011b). Individuals who reported any use of antidepressants were considered as receiving antidepressants for depression. Psychotherapy visits were identified using the outpatient visits and office-based provider visits files. These files contain information on whether the visit was for “psychotherapy or mental health counseling”. We classified individuals as having psychotherapy, if any of their visits indicated “psychotherapy”. Such procedures have been used in earlier research using MEPS 2000 data (Harman, Edlund, & Fortney, 2004).
Using antidepressants and psychotherapy, we defined depression treatment in two ways. The first measure of depression treatment consisted of any treatment with antidepressants and/or psychotherapy versus no treatment. In the second measure, we combined antidepressant and psychotherapy use to categorize depression treatment variable into four classes: (1) no depression treatment, (2) antidepressant use only, (3) psychotherapy use only, and (4) both antidepressants and psychotherapy. Due to very small number of women using psychotherapy only, we combined groups 3 and 4 (psychotherapy with or without antidepressant use) and analyzed depression treatment with three categories.
Independent Variables
Independent variables comprising of predisposing, enabling, need-related, personal health practices, and external environment factors were assessed. Predisposing factors included race/ethnicity (White, African American, Latina, and those identified as Others), age (22-39, 40-49, 50-64, 65 and above), and education (less than high school, high school, and above high school). Enabling factors included marital status (married, widowed, divorced/separated, and never married), employment (yes/no), health insurance (private, public, and uninsured), poverty status (poor, near poor, middle income, and high income), and having a usual source of health care (yes/no). Need-related factors were perceived physical health status (excellent/very good, good, fair/poor), mental health status (excellent/very good, good, and fair/poor), and presence of any chronic condition (i.e. diabetes or heart disease or arthritis or osteoporosis). Personal health practices included current smoker (yes/no), regular exercise (yes/no), and body mass index (BMI) (underweight/normal, overweight, obese, and missing). The external environment factor was area of residence (metro, non-metro).
Statistical Techniques
Unadjusted subgroup differences in depression treatment were tested with chi-square tests. To examine depression treatment patterns among women with hypertension within a multivariate framework, we used a set of logistic regressions and a multinomial logistic regression. In the set of logistic regressions, in the first stage we modeled any treatment versus no treatment. In the multinomial regression, the dependent variable consisted of: (1) no depression treatment, (2) antidepressant use only, and (3) psychotherapy with or without antidepressants. In this regression, for the dependent variable, the reference group was “no depression treatment”. The parameter estimates from regressions were transformed to adjusted odds ratios (AOR) and their corresponding 95% confidence intervals (CI) were examined. All analyses were conducted utilizing SAS 9.2.
RESULTS
The characteristics of the sample population are displayed in Table 1. There were 1,304 in the sample, which was comprised of 788 Whites (74.4%), 218 African Americans (11.2%), 245 Latina (10.7%), and 53 who identified themselves as belonging to other racial groups (3.7%). The majority of the women (n=904 put the percent) were under the age of 65 years old (64.2%) Forty-three percent were married (43.1%) and 1,025 residing in a metropolitan area (80%). There were 34.7% employed women, with a high income (30.0%), with private insurance (56.6%). In addition, there were 924 women (68.6%) with a chronic condition; 651 (42.9%) perceived their health status as fair/poor; 444 (30.6%) indicated mental health status as fair/poor; 315 (22.1%) were current smokers; 882 (67.5%) didn't report regular physical activity; 679 (49.5%) were obese. Exercise (< 0.5%), current smoking (4.4%) and body mass index (BMI) categories (3.2%) had missing values.
Table 1.
Description of Women with Depression and Hypertension Medical Expenditure Panel Survey, 2006, 2007
| All | N 1,304 | Wt % 100.0 |
|---|---|---|
| Race/Ethnicity | ||
| White | 788 | 74.4 |
| African American | 218 | 11.2 |
| Latino | 245 | 10.7 |
| Other | 53 | 3.7 |
| Age | ||
| 22 - 39 | 103 | 7.4 |
| 40 - 49 | 248 | 18.2 |
| 50 - 64 | 553 | 38.6 |
| 65 + | 400 | 35.8 |
| Marital Status | ||
| Married | 531 | 43.1 |
| Widowed | 267 | 21.6 |
| Divorced/Separated | 380 | 26.1 |
| Never married | 126 | 9.2 |
| Metro | ||
| Metro | 1,025 | 80.0 |
| Non-metro | 279 | 20.0 |
| Education | ||
| Less Than High School | 444 | 24.6 |
| High School | 413 | 34.7 |
| Above High School | 440 | 40.7 |
| Employed | ||
| Yes | 424 | 34.7 |
| No | 880 | 65.3 |
| Poverty Status | ||
| Poor | 333 | 18.1 |
| Near Poor | 340 | 24.0 |
| Middle Income | 332 | 27.8 |
| High Income | 299 | 30.0 |
| Health Insurance | ||
| Private | 609 | 56.6 |
| Public | 557 | 34.9 |
| Uninsured | 138 | 8.4 |
| Usual Source of Care | ||
| Yes | 1,207 | 94.0 |
| No | 90 | 6.0 |
| Any Chronic Condition | ||
| Yes | 924 | 68.6 |
| No | 380 | 31.4 |
| Perceived Health | ||
| Excellent/Very Good | 256 | 24.4 |
| Good | 397 | 32.7 |
| Fair/Poor | 651 | 42.9 |
| Mental Health | ||
| Excellent/Very Good | 371 | 31.6 |
| Good | 489 | 37.8 |
| Fair/Poor | 444 | 30.6 |
| Current Smoker | ||
| Yes | 315 | 22.1 |
| No | 924 | 72.7 |
| Exercise | ||
| Yes | 420 | 32.5 |
| No | 882 | 67.5 |
| Body Mass Index (BMI) | ||
| Normal | 250 | 20.5 |
| Overweight | 322 | 25.8 |
| Obese | 679 | 49.5 |
Note: Based on women with hypertension and depression observed in 2006 or 2007 and who were alive as of the end of observation year and not pregnant during the observation year. Exercise (< 0.5%), current smoking (4.4%) and BMI categories (3.2%) had missing values.
Abbreviations include: N (Number) and Wt (Weighted).
Unadjusted Subgroup Differences in Depression Treatment
Overall, 338 (23.9%) had no depression treatment, 711 (56.8%) had antidepressant use only and 255 (19.3%) had psychotherapy with or without antidepressants (as shown in Table 2). Based on the results of the bivariate analysis (Table 2), there were significant subgroup differences in depression treatment patterns using the 3-level depression treatment variable among women with hypertension and depression. Statistically significant differences in depression treatment patterns were found for race/ethnicity, age, marital status, metro area, education, health insurance, mental health, and current smoker. However, the relationships between depression treatment patterns and employment status, poverty status, usual source of care, presence of chronic conditions, physical activity and body mass index categories were not significant.
Table 2.
Depression Treatment Among Women with Hypertension and Depression Medical Expenditure Panel Survey, 2006, 2007
| No Tx | AD Use Only | Psy w/o AD | Sig | ||||
|---|---|---|---|---|---|---|---|
| All | N 338 | Wt % 23.9 | N 711 | Wt % 56.8 | N 255 | Wt % 19.3 | |
| Race/Ethnicity | *** | ||||||
| White | 162 | 19.9 | 482 | 62.2 | 144 | 17.9 | |
| African American | 73 | 34.8 | 94 | 40.3 | 51 | 24.9 | |
| Latino | 86 | 37.0 | 115 | 43.3 | 44 | 19.6 | |
| Other | 17 | 33.5 | 20 | 36.6 | 16 | 29.9 | |
| Age | *** | ||||||
| 22 - 39 | 37 | 28.7 | 41 | 39.3 | 25 | 32.0 | |
| 40 - 49 | 72 | 27.6 | 119 | 49.1 | 57 | 23.3 | |
| 50 - 64 | 136 | 21.2 | 290 | 56.2 | 127 | 22.6 | |
| 65 + | 93 | 24.0 | 261 | 65.0 | 46 | 10.9 | |
| Marital Status | *** | ||||||
| Married | 128 | 22.0 | 314 | 61.1 | 89 | 16.9 | |
| Widowed | 84 | 30.1 | 155 | 60.8 | 28 | 9.2 | |
| Divorced/Separated | 90 | 21.9 | 200 | 54.7 | 90 | 23.3 | |
| Never married | 36 | 23.9 | 42 | 33.2 | 48 | 42.9 | |
| Metro | * | ||||||
| Metro | 274 | 25.2 | 540 | 54.5 | 211 | 20.4 | |
| Non-metro | 64 | 18.9 | 171 | 66.2 | 44 | 14.9 | |
| Education | *** | ||||||
| Less Than HS | 134 | 28.3 | 236 | 56.5 | 74 | 15.2 | |
| HS | 105 | 24.2 | 241 | 61.4 | 67 | 14.4 | |
| Above HS | 96 | 21.1 | 230 | 52.8 | 114 | 26.1 | |
| Employed | |||||||
| Yes | 122 | 24.4 | 221 | 53.8 | 81 | 21.8 | |
| No | 216 | 23.6 | 490 | 58.4 | 174 | 18.0 | |
| Poverty Status | |||||||
| Poor | 99 | 27.0 | 154 | 50.2 | 80 | 22.8 | |
| Near Poor | 90 | 25.2 | 190 | 58.9 | 60 | 15.9 | |
| Middle Income | 84 | 22.9 | 197 | 60.3 | 51 | 16.7 | |
| High Income | 65 | 21.9 | 170 | 55.9 | 64 | 22.2 | |
| Health Insurance | *** | ||||||
| Private | 130 | 20.1 | 358 | 60.4 | 121 | 19.4 | |
| Public | 146 | 25.6 | 290 | 52.8 | 121 | 21.5 | |
| Uninsured | 62 | 42.1 | 63 | 49.0 | 13 | 8.9 | |
| Usual Source of Care | |||||||
| Yes | 297 | 23.4 | 674 | 57.3 | 236 | 19.3 | |
| No | 39 | 32.5 | 32 | 47.2 | 19 | 20.2 | |
| Any Chronic Condition | |||||||
| Yes | 223 | 22.9 | 521 | 58.3 | 180 | 18.8 | |
| No | 115 | 26.2 | 190 | 53.5 | 75 | 20.3 | |
| Perceived Health | |||||||
| Excellent/Very Good | 67 | 24.5 | 144 | 57.5 | 45 | 18.0 | |
| Good | 100 | 22.7 | 229 | 58.9 | 68 | 18.4 | |
| Fair/Poor | 171 | 24.5 | 338 | 54.8 | 142 | 20.7 | |
| Mental Health | ** | ||||||
| Excellent/Very Good | 101 | 23.6 | 220 | 61.8 | 50 | 14.6 | |
| Good | 131 | 26.6 | 273 | 55.9 | 85 | 17.5 | |
| Fair/Poor | 106 | 20.9 | 218 | 52.8 | 120 | 26.3 | |
| Current Smoker | *** | ||||||
| Yes | 95 | 31.8 | 146 | 45.7 | 74 | 22.5 | |
| No | 232 | 21.7 | 522 | 59.7 | 170 | 18.6 | |
| Exercise | |||||||
| Yes | 120 | 24.9 | 224 | 54.9 | 76 | 20.1 | |
| No | 218 | 23.4 | 486 | 57.7 | 178 | 18.8 | |
| Body Mass Index (BMI) | |||||||
| Under/Normal | 71 | 27.8 | 137 | 52.2 | 42 | 20.0 | |
| Overweight | 101 | 27.6 | 159 | 54.4 | 62 | 18.0 | |
| Obese | 148 | 19.9 | 390 | 60.4 | 141 | 19.7 | |
Note: Based on women with hypertension and depression who were observed either in 2006 or 2007 and alive as of the end of the observation year and were not pregnant during the observation year. Abbreviations include: Wt (Weighted), Tx (Treatment), AD (Antidepressant), Sig (Significance), HS (High School), and w/o (without). Asterisks represent significant differences in depression treatment and subgroups.
p< .001
.01 ≤ p < 0.01
.01 ≤ p < 0.05.
Logistic Regression on Any Depression Treatment
Logistic regression on any treatment versus no treatment revealed statistically significant differences by race/ethnicity, marital status, health insurance, physical and mental health, current smoker and BMI categories (Table 3). African Americans (AOR=0.47, 95% CI=0.31, 0.71), Latina (AOR=0.46, 95% CI=0.31, 0.69) were less likely than Whites to receive any treatment for depression. Being widowed (AOR=0.61, 95% CI=0.40, 0.94) compared to married, uninsured (AOR=0.39, 95% CI=0.25, 0.62) compared to those with private health insurance, and current smoker (AOR=0.64, 95% CI=0.46, 0.89) compared to non-smoker were less likely to receive any depression treatment. Women who were obese (AOR=1.47, 95% CI=1.03, 2.09) were more likely to receive treatment when compared to women with underweight/normal body weight.
Table 3.
Adjusted Odds Ratios and 95% Confidence Intervals from Logistic Regression on Any Depression Treatment Medical Expenditure Panel Survey, 2006, 2007
| AOR | 95%CI | Sig | |
|---|---|---|---|
| Race/Ethnicity | |||
| White | |||
| African American | 0.47 | [0.31, 0.71] | *** |
| Latina | 0.46 | [0.31, 0.69] | *** |
| Other | 0.42 | [0.23, 0.77] | ** |
| Age | |||
| 22 - 39 | |||
| 40 - 49 | 1.06 | [0.57, 1.96] | |
| 50 - 64 | 1.36 | [0.76, 2.45] | |
| 65 + | 1.15 | [0.54, 2.43] | |
| Marital Status | |||
| Married | |||
| Widowed | 0.61 | [0.40, 0.94] | * |
| Divorced/Separated | 1.21 | [0.81, 1.81] | |
| Never married | 1.13 | [0.65, 1.96] | |
| Metro | |||
| Metro | |||
| Non-metro | 1.37 | [0.90, 2.07] | |
| Education | |||
| Less Than High School | 0.83 | [0.56, 1.26] | |
| High School | 0.85 | [0.60, 1.22] | |
| Above High School | |||
| Employed | |||
| Yes | |||
| No | 1.15 | [0.78, 1.69] | |
| Poverty Status | |||
| Poor | 1.06 | [0.64, 1.74] | |
| Near Poor | 1.16 | [0.78, 1.74] | |
| Middle Income | 1.12 | [0.74, 1.70] | |
| High Income | |||
| Health Insurance | |||
| Private | |||
| Public | 0.82 | [0.56, 1.20] | |
| Uninsured | 0.39 | [0.25, 0.62] | *** |
| Usual Source of Care | |||
| Yes | |||
| No | 0.73 | [0.46, 1.16] | |
| Any Chronic Condition | |||
| Yes | 1.09 | [0.75, 1.59] | |
| No | |||
| Perceived Health | |||
| Excellent/Very Good | |||
| Good | 1.12 | [0.78, 1.62] | |
| Fair/Poor | 1.02 | [0.68, 1.53] | |
| Mental Health | |||
| Excellent/Very Good | |||
| Good | 0.79 | [0.54, 1.15] | |
| Fair/Poor | 1.24 | [0.77, 2.00] | |
| Current Smoker | |||
| Yes | 0.64 | [0.46, 0.89] | ** |
| No | |||
| Exercise | |||
| Yes | |||
| No | 1.01 | [0.72, 1.42] | |
| Body Mass Index (BMI) | |||
| Under/Normal | |||
| Overweight | 0.97 | [0.66, 1.42] | |
| Obese | 1.47 | [1.03, 2.09] | * |
Note: Based on women with hypertension and depression who were observed either in 2006 or 2007, who were alive as of the observation year and were not pregnant during the observation year. Missing categories for smoking and BMI are not presented. Abbreviations include: AOR (Adjusted Odds Ratio), w/o (without), CI (confidence interval), and Significance (sig). Asterisks represent significant group differences compared to the reference group. The reference group for the dependent variable is “No Depression Treatment”.
p< .001
.01 ≤ p < 0.01
.01 ≤ p < 0.05.
Multinominal Logistic Regression on Depression Treatment
We also examined the relationship between no depression treatment and type of depression treatment using multinomial logistic regression (Table 4) on the 3-level depression treatment variable. In this regression, we used “no depression treatment” as the reference group for the dependent variable. African Americans (AOR=0.43, 95% CI=0.28, 0.66) and Latina (AOR=0.41, 95% CI=0.27, 0.62) were less likely to receive antidepressant only when compared to Whites (Table 4). Other significant variables were: marital status (widowed (AOR=0.61, 95% CI=0.40, 0.95) versus married), uninsured (AOR=0.47, 95% CI=0.29, 0.75) versus private insurance; and current smoker (AOR=0.61, 95% CI=0.43, 0.85) compared to those who did not smoke. Women who were obese were more likely to receive antidepressants only than no treatment (AOR=1.62, 95% CI=1.10, 2.37) compared to those with underweight/normal body weight.
Table 4.
Adjusted Odds Ratios and 95% Confidence Interval from Multinomial Logistic Regression On Type of Depression Treatment Medical Expenditure Panel Survey, 2006, 2007
| Antidepressant Use Only | Psychotherapy w/o Antidepressants | |||||
|---|---|---|---|---|---|---|
| AOR | 95%CI | Sig | AOR | 95% CI | Sig | |
| Race/Ethnicity | ||||||
| White | ||||||
| African American | 0.43 | [0.28, 0.66] | *** | 0.60 | [0.36, 1.01] | |
| Latino | 0.41 | [0.27, 0.62] | *** | 0.66 | [0.37, 1.16] | |
| Other | 0.32 | [0.16, 0.64] | ** | 0.82 | [0.39, 1.74] | |
| Age | ||||||
| 22 - 39 | ||||||
| 40 - 49 | 1.16 | [0.59, 2.29] | 0.95 | [0.46, 1.99] | ||
| 50 - 64 | 1.55 | [0.79, 3.02] | 1.15 | [0.58, 2.25] | ||
| 65 + | 1.53 | [0.67, 3.51] | 0.58 | [0.24, 1.40] | ||
| Marital Status | ||||||
| Married | ||||||
| Widowed | 0.61 | [0.40, 0.95] | * | 0.50 | [0.25, 1.04] | |
| Divorced/Separated | 1.11 | [0.74, 1.67] | 1.52 | [0.86, 2.68] | ||
| Never married | 0.68 | [0.36, 1.28] | 2.34 | [1.26, 4.36] | ** | |
| Metro | ||||||
| Metro | ||||||
| Non-metro | 1.50 | [1.00,2 .25] | 0.96 | [0.49, 1.89] | ||
| Education | ||||||
| Less Than HS | 0.98 | [0.63, 1.51] | 0.52 | [0.30, 0.90] | * | |
| HS | 0.98 | [0.67, 1.44] | 0.54 | [0.36, 0.83] | ** | |
| Above HS | ||||||
| Employed | ||||||
| Yes | ||||||
| No | 1.12 | [0.75, 1.68] | 1.20 | [0.73, 1.96] | ||
| Poverty Status | ||||||
| Poor | 1.10 | [0.65, 1.86] | 0.95 | [0.50, 1.82] | ||
| Near Poor | 1.23 | [0.78, 1.92] | 0.97 | [0.59, 1.58] | ||
| Middle Income | 1.28 | [0.82, 1.99] | 0.74 | [0.44, 1.25] | ||
| High Income | ||||||
| Health Insurance | ||||||
| Private | ||||||
| Public | 0.80 | [0.54, 1.19] | 0.90 | [0.53, 1.52] | ||
| Uninsured | 0.47 | [0.29, 0.75] | ** | 0.22 | [0.11, 0.46] | *** |
| Usual Source of Care | ||||||
| Yes | ||||||
| No | 0.76 | [0.46, 1.25] | 0.70 | [0.33, 1.47] | ||
| Any Chronic Condition | ||||||
| Yes | 1.05 | [0.71,1.57] | 1.17 | [0.74, 1.83] | ||
| No | ||||||
| Perceived Health | ||||||
| Ex/Very Good | ||||||
| Good | 1.14 | [0.78, 1.65] | 1.03 | [0.57, 1.89] | ||
| Fair/Poor | 1.09 | [0.71, 1.68] | 0.78 | [0.40, 1.50] | ||
| Mental Health | ||||||
| Ex/Very Good | ||||||
| Good | 0.72 | [0.50, 1.03] | 1.14 | [0.61, 2.13] | ||
| Fair/Poor | 0.96 | [0.59, 1.56] | 2.74 | [1.36, 5.52] | ** | |
| Current Smoker | ||||||
| Yes | 0.61 | [0.43, 0.85] | ** | 0.74 | [0.48, 1.13] | |
| No | ||||||
| Exercise | ||||||
| Yes | ||||||
| No | 1.07 | [0.76, 1.51] | 0.90 | [0.58, 1.39] | ||
| Body Mass Index (BMI) | ||||||
| Under/Normal | ||||||
| Overweight | 1.02 | [0.68, 1.52] | 0.82 | [0.45, 1.50] | ||
| Obese | 1.62 | [1.10, 2.37] | * | 1.10 | [0.64, 1.87] | |
Note: Based on women with hypertension and depression who were observed either in 2006 or 2007, who were alive as of the observation year and were not pregnant during the observation year. Missing categories for smoking and BMI are not presented. Abbreviations include: w/o (without), Ex (excellent), HS (High School), and Significance (sig). Asterisks represent significant group differences compared to the reference group. The reference group for the dependent variable is “No Depression Treatment”.
p< .001
.01 ≤ p < 0.01
.01 ≤ p < 0.05.
Women with high school compared to above high school and uninsured compared to private insurance were less likely to receive psychotherapy with or without antidepressant treatment. However, when compared to women with perceived excellent/very good mental health, women who perceived themselves to be in fair/poor mental health were more likely (AOR=2.74, 95% CI=1.36, 5.52) to receive psychotherapy with or without antidepressants. Similarly, compared to women who were married, those who were never married were more likely to report psychotherapy use (AOR = 2.34, 95% CI=1.26, 4.36).
DISCUSSION
We set out to examine depression treatment patterns among women with hypertension utilizing MEPS, a nationally representative survey of families and individuals, their medical providers, and employers across the United States (AHRQ, 2011a). To the best of our knowledge, we are the first to analyze depression treatment in women with hypertension and depression in a nationally representative sample of households. Therefore, we discuss our findings in the context of studies that include both men and women. To the extent possible, we try to compare our findings to the studies that focus on depression treatment in the presence of any chronic disease.
Nearly 56% of women in our study received antidepressants only. In studies where rates of antidepressant by gender were analyzed, investigators reported that women were more likely to use antidepressants than men in those with acute coronary syndrome (Shin, Hagerty, & Williams, 2010) and in the general population (Unützer et al., 2003; Williams et al., 1995). In a study of women veterans with hypertension, heart disease or diabetes, Leeners et al. (2007) reported that 51% received antidepressants. Although no statistically significant differences were found by gender in adult veterans with diabetes, nearly 53% of women used antidepressants (Tiwari et al., 2008). The range of antidepressant use investigators reported in these studies (Leeners et al., 2007; Shin et al., 2010; Tiwari et al., 2008; Unützer et al., 2003; Williams et al., 1995) suggests that rates of antidepressant use observed in our study are consistent with other studies.
Compared to the findings reported in general studies that include men and women, our overall rate of psychotherapy (26.9%) is somewhat comparable to those reported in the literature (Mojtabai & Olfson, 2008). In a study where researchers analyzed trends in psychotherapy in office-based psychiatrists, researchers reported that 24% of both men and women had psychotherapy visits for major depression in 2005 (Mojtabai & Olfson, 2008). The rate of psychotherapy visits among our study population was 26.9%, although this figure included visits for depression and other reasons.
In our study, 24% of the women with hypertension did not receive treatment for depression. There are no published results clinical trials establishing good chronic care outcomes with treatment for depression in hypertension. This may be due to the lack of clinical guidance as to how to treat depression in individuals with hypertension. Based on a review of clinical trials on the effects of depression treatment in diabetes (Petrak & Herpertz, 2009) and heart disease (Joynt & O'Connor, 2005), investigators concluded that depression treatment may not improve chronic medical outcomes but does provide relief from depression. In addition, some providers may not prescribe antidepressants for some individuals with chronic medical conditions due to serious side effects. Furthermore, the association between some types of antidepressants and increased risk of stroke, and all cause mortality among women may discourage use of antidepressants (Krantz et al., 2009; Smoller et al., 2009). Further research is needed to examine the non-treatment of depression in women with hypertension.
In addition to estimation of depression treatment rates, we also examined variations in treatment among women with hypertension predisposing, enabling, need-related, personal health practices, and external environment factors. In this regard, we found many significant subgroup differences in depression treatment patterns within a multivariate framework. Among demographic characteristics, we note the racial/ethnic differences. Lower rates and likelihood of depression treatment in racial/ethnic minorities in our study were similar to those found in the general population of women (Ward, 2007). In a review on treatment of depression in patients with medical comorbidities, that included both men and women, there were provider, patient, and practice-setting barriers to effective management of depression care in African Americans (Das, Olfson, McCurtis, & Weissman, 2006). In another review, Simpson et al. (2007) reported that African Americans and ethnic minorities are less likely to be treated for depression. However, we did not find differences in use of psychotherapy by race/ethnicity. This finding is somewhat surprising given racial minorities in general prefer counseling for depression over antidepressants (Givens, Houston, Van Voorhees, Ford, & Cooper, 2007).
Our study findings highlighted the well documented access barrier to care (i.e. health insurance). The negative consequences of under insurance on health have been well documented by the 2003 Institute of Medicine Report entitled, “Institute of Medicine Committee on the Consequences of Uninsurance, Hidden Costs, Value Lost: Uninsurance in America)”. Specific to depression treatment, in a sample of persons with a major depressive episode from the 2005-2006 National Survey on Drug Use and Health, one of the largest mental health surveys of the U.S, one of the major reasons for not seeking treatment for a major depressive episode was insurance (Mojtabai, 2009). In this regard, our study confirms being uninsured is a barrier to treatment among women with hypertension.
Among life-style practices, smoking is often considered to be a barrier to depression treatment. Although only 22% of the women in our study stated that they were current smokers, those who were current smokers were less likely to be on antidepressants only or any treatment for depression. It is possible that women with depression and who smoke, may use smoking to self-medicate depressive symptoms (Mineur & Picciotto, 2009) and therefore less likely to seek treatment for depression. Women who were obese had higher rates of antidepressants-only and were more likely to be on antidepressants, even after adjusting for other independent variables included in our study. To our knowledge, there have not been any studies on depression treatment in women with obesity. However, given that some antidepressants and not all are associated with weight gain (Azarbad & Gonder-Frederick, 2010; Serretti & Mandelli, 2010), it is possible that providers may consider antidepressants-only treatment for those with obesity.
Implications of Our Study in the International Context
We found that overall 76.1% of women in our study sample received depression treatment and 57% were treated with antidepressants only. Rates of depression treatment in our study sample are higher than in other developed countries. For example, though not specific to women, a study across six different countries in Western Europe (Belgium, France, Germany, Italy, the Netherlands and Spain), only 21.2% were treated with antidepressants (Alonzo et al., 2004). However, the factors that influenced depression treatment in this nationally representative sample of US women were not very different than those in other developed or developing countries. For example, in our study we found that uninsured individuals were less likely to get depression treatment, similarly in the study by Simons et al. (2004), which was conducted in six sites all over the world, financial barriers (as in out-of-pocket expenditures) was the most significant barrier to seeking care for depression.
We found that widowed women were less likely to seek depression treatment as compared to married women. In a study based in England Wales, there were no differences in receipt of depression treatment by marital status (Weich, Nazareth, Morgan, & King, 2007). However, in another study by the same authors, study participants who received antidepressant treatment were open to their family members about their depression (Weich, Morgan, King, & Nazareth, 2007). This may indicate that lack of social support in widowed women may be a reason for not getting depression treatment. It was not surprising to observe that African-American women were less likely than Whites to receive any depression treatment. Racial and ethnic minorities world over often do not have access and do not receive adequate care for depression and other diseases (WHO, 2005).
ABM Theoretical Framework
We based our choice of variables utilizing the ABM theoretical framework. As it appears from the results, the use of this framework helped us to successfully identify certain factors that predicted depression treatment with hypertension. The use of ABM for identification of predictors of healthcare use is well documented and this model can be used in different countries and healthcare settings to identify factors associated with depression treatment.
Strengths and Limitations
Our study had several strengths, such as it is a nationally representative sample, the ability to identify conditions that are both relevant to depression and hypertension, the availability of prescription medication and psychotherapy, and comprehensive set of variables that may influence depression treatment rates. Some of the limitations include that the information is self-reported; therefore, recall bias could have occurred during the interview process. To minimize this bias, more intervals of interviews should have been performed. We reported only a cross-sectional snap shot of the available data. In addition, we did not control for the severity of chronic illnesses or depression. In addition, it was not indicated within the data if women in the study met the criteria for minor or major depression.
CLINICAL IMPLICATIONS
Despite these limitations, we believe that our study adds to the nascent literature on depression care in the presence of chronic medical illnesses, specifically hypertension among non-pregnant women. There were subgroup differences in treatment patterns among women with hypertension. To improve overall health status of those with the co-occurring diseases, these subgroups need to be monitored and given special attention. For future studies, researchers may want to explore whether co-management of depression and hypertension in women with hypertension may reduce subgroup differences or whether depression treatment is beneficial for women with hypertension by including chronic care outcomes.
Figure 1.
Conceptual Model – Andersen Behavioral Model (ABM) of Healthcare Services Utilization in Predicting Variations in Treatment for Depression
REFERENCES
- Agency for Healthcare Research and Quality Survey background. 2011a doi: 10.1080/15360280802537332. Retrieved from http://www.meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. [DOI] [PubMed]
- Agency for Healthcare Research and Quality MEPS HC-110A: 2007 prescription medicines, October 2009. 2011b Retrieved from http://www.meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h110a/h110adoc.pdf.
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, Vollebergh WA. Use of mental health services in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica Supplementum. 2004;420:47–54. doi: 10.1111/j.1600-0047.2004.00330.x. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen R, Newman J. Societal and Individual determinants of medical care utilization in the United States. Health & Society. 1973;51:95–124. [PubMed] [Google Scholar]
- Azarbad L, Gonder-Frederick Obesity in women. Psychiatric Clinics of North America. 2010;33:423–440. doi: 10.1016/j.psc.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Bostwick JM. A generalist's guide to treating patients with depression with an emphasis on using side effects to tailor antidepressant therapy. Mayo Clinic Proceedings. 2010;85:538–550. doi: 10.4065/mcp.2009.0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Effective treatments exists: People with depression and anxiety should seek help as early as possible to reduce health effects and improve quality of life. 2011 Retrieved from http://www.cdc.gov/Features/dsBRFSS DepressionAnxiety/
- Chatterjee S, Kotelchuck M, Sambamoorthi U. Prevalence of chronic illness in pregnancy, access to care, and health care costs: implications for interconception care. Womens Health Issues. 2008;18:S107–S116. doi: 10.1016/j.whi.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe NR, Jenckes MW, Gonzales JJ, Levine DM, Ford DE. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12:431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das AK, Olfson M, McCurtis HL, Weissman MM. Depression in African Americans: Breaking barriers to detection and treatment. Journal of Family Practice. 2006;55:30–39. [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Whiteford HA. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Medicine. 2013;10(11):e1001547. doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn HA, Blow FC, Marcus SM. Rates and predictors of depression treatment among pregnant women in hospital-affiliated obstetrics practices. General Hospital Psychiatry. 2006;28:289–295. doi: 10.1016/j.genhosppsych.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Frackiewicz EJ, Sramek JJ, Cutler NR. Gender differences in depression and antidepressant pharmacokinetics and adverse events. Annuals of Pharmacotherapy. 34:80–88. doi: 10.1345/aph.18465. [DOI] [PubMed] [Google Scholar]
- Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. General Hospital Psychiatry. 2007;29:182–191. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Goldberg D. The detection and treatment of depression in the physically ill. World Psychiatry. 2010;9:16–20. doi: 10.1002/j.2051-5545.2010.tb00256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatric Services. 2004;55:1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- Hobfall SE, Ritter C, Lavin J, Hulsizer M, Cameron RP. Depression prevalence and incidence among inner-city pregnant and post-partum women. Journal of Consulting and Clinical Psychology. 1995;63:445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on the Consequences of Uninsurance . Hidden costs, value lost: Uninsurance in America. National Academies Press; Washington: 2003. 2003. [PubMed] [Google Scholar]
- Joynt KE, O'Connor CM. Lessons from SADHART, ENRICHD, and other trials. Psychosomatic Medicine. 2005;67:S63–S66. doi: 10.1097/01.psy.0000163454.25036.fc. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, De Graaf R, Demyttenaere K, Gasquet I, Ustün TB. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Krantz DS, Whittaker KS, Francis JL, Rutledge T, Johnson BD, Barrow G, Merz CN. Psychotropic medication use and risk of adverse cardiovascular events in women with suspected coronary artery disease: Outcomes from the Women's Ischemia Syndrome Evaluation (WISE) study. Heart. 2009;95:1901–1906. doi: 10.1136/hrt.2009.176040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeners B, Neumaier-Wagner P, Kuse S, Stiller R, Rath W. Emotional stress and the risk to develop hypertensive disease in pregnancy. Hypertension in Pregnancy. 2007;26:211–226. doi: 10.1080/10641950701274870. [DOI] [PubMed] [Google Scholar]
- Licht CM, de Geus EJ, Seldenrijk A, van Hout HP, Zitman FG, van Dyck R, Penninx BW. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension. 2009;53:631–638. doi: 10.1161/HYPERTENSIONAHA.108.126698. [DOI] [PubMed] [Google Scholar]
- Marcus M, Yasamy MT, van Ommeren M, Chisholm D, Saxena S. Depression: A Global public health concern. 2012 Retrieved from http://www.paho.org/equity/index2.php?option=com_docman&task=doc_view&gid=82&Itemid.
- Menke R, Flynn H. Relationships between stigma, depression, and treatment in White and African American care patients. Journal of Nervous & Mental Disease. 2009;197:407–411. doi: 10.1097/NMD.0b013e3181a6162e. [DOI] [PubMed] [Google Scholar]
- Meyer CM, Armenian HK, Eaton WW, Ford DE. Incident hypertension associated with depression in the Baltimore Epidemiologic Catchment area follow-up study. Journal of Affective Disorders. 2004;83:127–133. doi: 10.1016/j.jad.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Mineur YS, Picciotto MR. Biological basis for the co-morbidity between smoking and mood disorders. Journal of Dual Diagnosis. 2009;5:122–130. doi: 10.1080/15504260902869964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. National trends in psychotherapy by office-based psychiatrists. Archives of General Psychiatry. 2008;65:962–70. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Unmet need for treatment of major depression in the United States. Psychiatric Services. 2009;60:297–305. doi: 10.1176/ps.2009.60.3.297. [DOI] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patwl V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Petrak F, Herpertz S. Treatment of depression in diabetes: An update. Current Opinion in Psychiatry. 2009;22:211–217. doi: 10.1097/YCO.0b013e3283207b45. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: Scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Scalco AZ, Scalco MZ, Azul JB, Lotufo NF. Hypertension and depression. Clinics. 2005;60:241–250. doi: 10.1590/s1807-59322005000300010. [DOI] [PubMed] [Google Scholar]
- Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. Journal of Clinical Psychiatry. 2010;71:1259–1272. doi: 10.4088/JCP.09r05346blu. [DOI] [PubMed] [Google Scholar]
- Shin NM, Hagerty B, Williams R. Gender comparison in depressive symptoms and use of antidepressant medications after acute coronary syndrome. Applied Nursing Research. 2010;23:73–79. doi: 10.1016/j.apnr.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Simon GE, Fleck M, Lucas R, Bushnell DM. Prevalence and predictors of depression treatment in an international primary care study. American Journal of Psychiatry. 2004;161:1626–1634. doi: 10.1176/appi.ajp.161.9.1626. [DOI] [PubMed] [Google Scholar]
- Simonsick E, Wallace R, Blazer D, Berkman L. Depressive symptomatology and hypertension-associated morbidity and mortality in older adults. Psychosomatic Medicine. 1995;57:427–435. doi: 10.1097/00006842-199509000-00003. [DOI] [PubMed] [Google Scholar]
- Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: A literature review. Psychiatric Quarterly. 2007;78:3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Allison M, Cochrane BB, Curb JD, Perlis RH, Robinson JG, Wassertheil-Smoller S. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women's Health Initiative study. Archives of Internal Medicine. 2009;169:2128–2139. doi: 10.1001/archinternmed.2009.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Shear MK, Thase ME, Fleming MA, Scott J. A pilot study of brief interpersonal psychotherapy for depression among women. Psychiatric Services. 2004;55:448–450. doi: 10.1176/appi.ps.55.4.448. [DOI] [PubMed] [Google Scholar]
- Tiwari A, Rajan M, Miller D, Pogach L, Olfson M, Sambamoorthi U. Guideline-consistent antidepressant treatment patterns among veterans with diabetes and major depressive disorder. Psychiatric Services. 2008;59:1139–1147. doi: 10.1176/ps.2008.59.10.1139. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Oishi S. Depression treatment in a sample of 1,801 depressed older adults in primary care. Journal of the American Geriatric Society. 2003;51:505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Non-compliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. Journal of General Internal Medicine. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Aquilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, Wells JE. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370:841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward E. Examining differential treatment effects for depression in racial and ethnic minority women: a qualitative systematic review. Journal of the National Medical Association. 2007;99:265–274. [PMC free article] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Applegate WB, Berge K, Chang CJ, Davis BR, Grimm R, Jr., Schron E. Change in depression as a precursor of cardiovascular events. SHEP Cooperative Research Group (systolic hypertension in the elderly). Archives of Internal Medicine. 1996;156:553–561. [PubMed] [Google Scholar]
- Weich S, Nazareth I, Morgan L, King M. Treatment of depression in primary care. Socio-economic status, clinical need and receipt of treatment. British Journal of Psychiatry. 2007;191:164–169. doi: 10.1192/bjp.bp.106.032219. [DOI] [PubMed] [Google Scholar]
- Weich S, Morgan L, King M, Nazareth I. Attitudes to depression and its treatment in primary care. Psychological Medicine. 2007;37(9):1239–1248. doi: 10.1017/S0033291707000931. [DOI] [PubMed] [Google Scholar]
- Williams JB, Spitzer RL, Linzer M, Kroenke K, Hahn SR, deGruy FV, Lazev A. Gender differences in depression in primary care. American Journal of Obstetrics & Gynecology. 1995;173(2):654–659. doi: 10.1016/0002-9378(95)90298-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization Depression. 2014 Retrieved from http://www.who.int/mediacentre/factsheets/fs369/en/
- World Health Organization Mental health: Facing the challenges, building solutions. 2005 Retrieved from http://www.euro.who.int/_data/assets/pdf_file/0008/96452/E87301.pdf.
- Yoder SR, Thornburg LL, Bisognano JD. Review: Hypertension in pregnancy and women of childbearing age. American Journal of Medicine. 2009;122:890–895. doi: 10.1016/j.amjmed.2009.03.036. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, Lockwood C. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. General Hospital Psychiatry. 2009;31:403–413. doi: 10.1016/j.genhosppsych.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]