Abstract
Objective
Few studies have examined distinct patterns (i.e., repertoires) of coping skills among alcohol use disorder (AUD) populations. We examined patterns of coping among individuals following AUD treatment and were particularly interested in whether the broadness of one’s repertoire, or the degree of utilizing a broad range of different coping skills, was related to alcohol treatment outcomes.
Method
We conducted secondary analyses of data from the COMBINE Study (N=1,101; mean age=45.14 (SD=10.19), 68.8 % male; 21.3 % non-white) and Project MATCH (N=1,587; mean age=40.25 (SD=11.07), 75.7 % male; 19.7 % non-white). Finite mixture models were conducted to examine patterns of alcohol-specific coping, as measured by the Processes of Change Questionnaire (Prochaska, Velicer, DiClemente, & Fava, 1988).
Results
Three latent coping repertoire classes provided the best fit to the data in both studies: (1) a broad class that had a broad range of different skills that were consistently used, (2) a moderate class that had a moderate range of different skills that were consistently used, and (3) a narrow class that had a limited range of different skills that were consistently used. In both studies the broad repertoire class generally had the best treatment outcomes. Receiving the combined behavioral intervention in COMBINE predicted a greater likelihood of expected classification in the broad class.
Conclusion
Having a broad coping repertoire was associated with better alcohol treatment outcomes and may be an important target in AUD treatment. Further research examining distinct patterns or repertoires of coping among AUD populations is warranted.
Keywords: Coping Repertoire, Alcohol-Specific Coping, Alcohol Use Disorder, Alcohol Treatment, Drinking Outcomes
Introduction
For over thirty years the alcohol treatment field has considered the acquisition of coping skills as a key treatment target to prevent alcohol relapse (Litman, Eiser, Rawson, & Oppenheim, 1979; Marlatt & Gordon, 1985; Moser & Annis, 1996). As such, alcohol-specific coping skills, or behaviors directly aimed at preventing one from drinking, are taught in many behavioral treatments and mutual help programs for alcohol use disorder (AUD). Cognitive-behavioral therapy (CBT) approaches for AUD explicitly focus on teaching a variety of alcohol-specific coping skills (Kadden, 1995) and twelve-step oriented programs for AUD focus on teaching certain coping skills such as seeking social support, avoiding cues, and spiritual coping. Numerous studies have shown that an overall increase in self-reported frequency of using alcohol-specific coping skills following treatment is related to better alcohol use outcomes (Litt, Kadden, Cooney, & Kabela, 2003; Litt, Kadden, & Kabela-Cormier, 2009; Witkiewitz & Masyn, 2008). Studies using role-play assessments to measure coping have also consistently supported the notion that coping is an important predictor of alcohol relapse (Chaney, O’Leary, and Marlatt, 1978; Kiluk, Nich, Babuscio, & Carroll, 2010; Morgenstern & Longabaugh, 2000). Yet, despite the explicit emphasis on coping skills training in CBT, there is still little empirical evidence suggesting that improvement in coping skills is a unique mechanism of change in CBT for AUD (Litt et al., 2003; Morgenstern & Longabaugh, 2000, see Kiluk, et al., 2010 as one exception). Hence, we still have a very limited understanding of coping as a mechanism of change in alcohol treatment, which in turn hinders efforts to most effectively target coping in AUD treatment.
In order to better understand the role of coping in AUD treatment, novel approaches for conceptualizing and measuring coping are warranted. To date, the vast majority of empirical studies on coping among individuals with AUD have measured coping by either using total scores on self-report measures of coping frequency (e.g., Litt et al., 2003) or using performance-based scores on role-play assessments (Kiluk, et al., 2010; Morgenstern & Longabaugh, 2000). However, few studies to date among AUD populations have examined how particular patterns in one’s overall repertoire of alcohol-specific coping skills are related to alcohol use outcomes. In other words, few studies have attempted to look more closely at each individual’s entire “coping toolbox” and to understand how different combinations or patterns of using skills are more or less effective. Increases in total coping frequency scores only show that an individual is using coping skills more often, but do not shed light on how exactly an individual’s pattern of using skills has changed. Of note, studies have investigated how different types of coping skills are related to alcohol use outcomes (Dolan, Rohsenow, Martin, & Monti, 2013; Rohsenow et al., 2001). Yet, these studies examine one-to-one associations and do not reveal how using combinations or patterns of skills together over a period of time may be related to outcomes.
Only a few studies have examined patterns of coping among individuals with AUD. Moser and Annis (1996) found that combining active and avoidant skills increased one’s odds of terminating a drinking episode. Carbonari & DiClemente (2000) examined different patterns of cognitive and behavioral coping following AUD treatment. Individuals who were abstinent following treatment reported the highest use of behavioral coping skills and only moderate use of cognitive skills. Wong et al. (2013) used latent profile analysis to identify distinct profiles of using coping and emotion regulation skills among young adult alcohol and drug users. Results indicated that profiles characterized by frequent use of a broad range of coping and emotion regulation skills had the best substance use outcomes. Finally, existing studies among adults in AUD treatment suggest that having a greater number of different alcohol-specific coping skills in one’s repertoire is associated with better alcohol use outcomes (Litman et al., 1979; Litt et al., 2009; Moser & Annis, 1996).
The importance of examining patterns or repertoires of coping has received increased attention in areas of psychological research outside of the AUD field (Bonanno & Burton, 2013; Dixon-Gordon, Aldao, & De Los Reyes, 2015; Lougheed & Hollenstein, 2012). Several studies outside the addiction field (Dixon-Gordon et al., 2015; Lougheed & Hollenstein, 2012) have used person-centered approaches (e.g., latent class analysis; Collins & Lanza, 2010) to empirically identify typologies of coping based on similar patterns of data. Many researchers have focused on measuring the broadness of one’s coping repertoire, or the degree of using a wide range of different skills. Bonanno and Burton (2013) posit that having a broad repertoire of different skills may enhance one’s ability to flexibly cope with divergent situational demands. Studies across a variety of populations have consistently shown that a broader repertoire of skills is associated with better mental health outcomes (Bonanno & Burton, 2013; Cheng, Lau, & Chan, 2014).
Overall, there is still limited research to date on patterns or repertoires of coping among individuals with AUD. The present study used person-centered analyses to examine patterns of alcohol-specific coping following AUD treatment. Drawing from research on broad coping repertoires outside the AUD field, we were particularly interested in whether the broadness of one’s coping repertoire following AUD treatment played an important role in predicting alcohol use outcomes. We also examined how pre-treatment factors were related to different patterns of coping.
Method
Participants and Procedures
This study was a secondary data analysis using data from two alcohol treatment studies: the COMBINE study and Project MATCH. The COMBINE study (Anton et al., 2006) was a multisite randomized clinical trial (RCT) comparing combinations of medications (acamprosate, naltrexone, or placebo) and psychosocial treatments (combined behavioral intervention or medication management) for AUD. The combined behavioral intervention (CBI) was an intensive behavioral intervention that integrated key components from various behavioral treatments for AUD including CBT (Kadden et al., 1992), Twelve Step Facilitation (TSF; Nowinski, Baker, & Carroll, 1992), and Motivation Enhancement Therapy (MET; Miller, Zweben, DiClemente, & Rychtarik, 1992). Medical management was a less intensive intervention that involved 9 sessions and focused on improving medication adherence. In COMBINE, a total of 1,383 participants received treatment over 16 weeks and were followed up for a 12-month period following treatment.
Project MATCH (Project MATCH Research Group, 1998) was a multisite RCT comparing three behavioral treatments for AUD: CBT (Kadden et al., 1992), MET (Miller et al., 1992), and TSF (Nowinski, Baker, & Carroll, 1992). A total of 1,726 participants received treatment over 12 weeks and were followed up for a 12-month period following treatment. In MATCH, there was an outpatient arm (n = 952; i.e., participants who were actively drinking during the 3 months before study entry) and an aftercare arm (n = 774; i.e., participants who has completed at least 7 days of inpatient or intensive outpatient treatment and were referred to aftercare treatment). We utilized the full MATCH sample (n = 1726) because we were interested in the overall role of coping repertoire across individuals with varying levels of alcohol dependence severity and at different stages of treatment.
For analyses in this study, we only included participants who had available data for the measure of alcohol-specific coping skills. In COMBINE, the available sample was 1,101 participants (80 % of the full sample). Among the available sample of 1,101 in COMBINE the demographic data were: male (n = 758, 69.8 %), mean age = 45.14 (SD = 10.19), non-Hispanic white (n = 867, 76.7 %), Black/African American (n = 95, 8.6 %), Asian (n = 2, 0.2 %), Hispanic (n = 96, 8.7 %), multi-racial (n = 15, 1.4 %), other race (n = 15, 1.4 %), married (n =462, 42 %), mean years of education = 14.65 (SD = 1.01). In MATCH, the available sample was 1587 (92 % of the full sample). Among the available sample of 1,587 in MATCH the demographic data were: male (n = 1202, 75.7 %), mean age = 40.25 (SD = 11.07), non-Hispanic white (n = 1274, 80.3%), Black/African American (n = 149, 9.4 %), Asian (n = 2, 0.1 %), Hispanic (n = 132, 8.3 %), multi-racial (not available), other race (n = 8, 0.5 %), married (n =531, 33.5 %), mean years of education = 13.3 (SD = 2.1). In both COMBINE and MATCH, there were no significant differences in client demographics or baseline alcohol consumption between the full study sample and the sample available for this study.
Measures
Alcohol-specific coping skills
In both COMBINE and MATCH, the Processes of Change Questionnaire (PCQ; Prochaska, Velicer, DiClemente, & Fava, 1988) was used to assess alcohol-specific coping skills. The PCQ is a 40-item self-report measure assessing the frequency with which individuals use various behaviors to help them not drink. The PCQ was originally developed and validated among smokers (Prochaska et al., 1988) and an adapted version of the PCQ for AUD populations was developed initially for Project MATCH (DiClemente, Carroll, Connors, & Kadden, 2004) and also used in COMBINE. The alcohol version of the PCQ has also been used in other studies among AUD populations (Freyer et al., 2006; Snow, Prochaska, & Rossi, 1994). Participants respond to each item on a five-point Likert-type scale ranging from 1 (never) to 5 (repeatedly). A list of all 40 PCQ items is included in Table 2. The PCQ was designed to assess 10 types of coping skills including 5 behavioral skills: contingency management (items 1, 9, 27, 36), counterconditioning (items 8, 17, 26, 35), self-liberation (items 12, 20, 30, 37), seeking social support (items 2, 10, 28, 28), and stimulus control (items 7, 16, 25, 34), and 5 cognitive skills: consciousness raising (items 15, 24, 33, 40), dramatic relief (items 3, 11,19, 29), environmental reevaluation (items 5, 14, 22, 31), self-reevaluation (items 6, 23, 32, 39), and social liberation (items 4, 13, 21, 38). The PCQ was administered at the end of treatment in both COMBINE (week 16) and MATCH (week 12). Reliability analyses indicated the reliabilities of each subscale were generally within an acceptable range in both COMBINE (α = 0.647 – .922; 9 out of 10 subscales above .7) and MATCH (α = 0.645 – .917, 8 out of 10 subscales above .7).
Table 2.
Latent class item response probabilities for PCQ Items in COMBINE (bolded) and MATCH (unbolded)
| Class 1 (Narrow) | Class 2 (Moderate) | Class 3 (Broad) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Response | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 |
| Contingency Management Items | |||||||||||||||
| 1 Do something nice for making efforts to change | .344 | .218 | .292 | .112 | .034 | .061 | .290 | .511 | .134 | .004 | .099 | .128 | .407 | .313 | .053 |
| .322 | .291 | .311 | .075 | .000 | .042 | .217 | .5 | .227 | .015 | .075 | .108 | .322 | .339 | .157 | |
| 9 Reward myself when I don’t give in to my urge | .609 | .253 | .096 | .033 | .008 | .157 | .379 | .398 | .060 | .006 | .179 | .156 | .307 | .258 | .099 |
| .492 | .254 | .200 | .043 | .011 | .073 | .247 | .419 | .243 | .018 | .118 | .125 | .279 | .232 | .247 | |
| 27 Don’t let myself have fun when I drink | .846 | .089 | .040 | .021 | .004 | .365 | .396 | .190 | .045 | .004 | .477 | .192 | .146 | .120 | .064 |
| .584 | .272 | .107 | .029 | .007 | .272 | .341 | .232 | .132 | .023 | .386 | .149 | .172 | .12 | .173 | |
| 36 Spend time with people who reward me | .758 | .118 | .074 | .033 | .017 | .203 | .398 | .297 | .102 | .000 | .137 | .172 | .268 | .274 | .149 |
| .564 | .303 | .103 | .031 | .000 | .101 | .346 | .351 | .187 | .015 | .15 | .139 | .235 | .251 | .225 | |
| Counterconditioning Items | |||||||||||||||
| 8 Calm myself when I get the urge to drink | .486 | .254 | .172 | .097 | .009 | .045 | .230 | .512 | .201 | .011 | .057 | .074 | .258 | .427 | .184 |
| .334 | .262 | .291 | .103 | .01 | .012 | .012 | .012 | .012 | .012 | .052 | .067 | .256 | .387 | .238 | |
| 17 Think about other things | .293 | .276 | .310 | .090 | .031 | .012 | .142 | .482 | .335 | .029 | .025 | .035 | .145 | .453 | .342 |
| .193 | .279 | .347 | .149 | .031 | .002 | .065 | .364 | .52 | .049 | .034 | .038 | .151 | .392 | .385 | |
| 26 Do something else to deal with tension | .287 | .185 | .292 | .160 | .076 | .008 | .176 | .505 | .295 | .015 | .007 | .034 | .176 | .480 | .302 |
| .177 | .210 | .330 | .222 | .060 | .006 | .077 | .341 | .526 | .051 | .009 | .023 | .127 | .381 | .461 | |
| 35 Find that doing things is a substitute for drinking | .135 | .151 | .259 | .307 | .147 | .007 | .079 | .355 | .499 | .059 | .006 | .005 | .101 | .394 | .493 |
| .104 | .128 | .374 | .264 | .13 | .001 | .023 | .226 | .618 | .131 | .008 | .006 | .063 | .339 | .582 | |
| Helping Relationship Items | |||||||||||||||
| 2 Can talk to at least 1 special person | .305 | .168 | .273 | .186 | .068 | .050 | .203 | .410 | .302 | .036 | .058 | .066 | .265 | .396 | .215 |
| .217 | .200 | .345 | .189 | .049 | .016 | .122 | .288 | .473 | .102 | .02 | .027 | .089 | .37 | .493 | |
| 10 Have someone to talk with who understands | .373 | .209 | .181 | .155 | .082 | .071 | .207 | .400 | .273 | .049 | .051 | .083 | .224 | .374 | .269 |
| .287 | .226 | .304 | .138 | .045 | .024 | .129 | .308 | .437 | .102 | .028 | .024 | .076 | .284 | .587 | |
| 18 Have someone I can count on to help me with drinking | .466 | .156 | .177 | .132 | .069 | .081 | .226 | .360 | .288 | .046 | .070 | .078 | .187 | .339 | .327 |
| .314 | .207 | .267 | .148 | .064 | .031 | .127 | .320 | .422 | .101 | .039 | .044 | .096 | .210 | .61 | |
| 28 Have someone who listens when I want to talk | .355 | .247 | .169 | .163 | .066 | .064 | .199 | .395 | .295 | .047 | .053 | .067 | .214 | .325 | .341 |
| .239 | .197 | .334 | .158 | .072 | .015 | .128 | .285 | .458 | .115 | .035 | .027 | .098 | .227 | .614 | |
| Stimulus Control Items | |||||||||||||||
| 7 Remove things from my home that remind me of drinking | .778 | .116 | .059 | .026 | .021 | .289 | .338 | .264 | .105 | .005 | .245 | .134 | .194 | .253 | .174 |
| .708 | .198 | .061 | .033 | .000 | .181 | .325 | .279 | .195 | .019 | .219 | .143 | .163 | .216 | .259 | |
| 16 Avoid situations that encourage me to drink | .392 | .255 | .251 | .072 | .030 | .014 | .192 | .487 | .292 | .015 | .033 | .057 | .190 | .418 | .302 |
| .245 | .302 | .308 | .092 | .053 | .018 | .107 | .371 | .442 | .063 | .045 | .067 | .137 | .326 | .425 | |
| 25 Use reminders to help me not to drink | .719 | .153 | .106 | .013 | .010 | .094 | .386 | .381 | .132 | .007 | .096 | .094 | .248 | .359 | .203 |
| .427 | .289 | .198 | .064 | .022 | .034 | .181 | .434 | .33 | .021 | .056 | .087 | .177 | .319 | .361 | |
| 34 Stay away from places associated with my drinking | .477 | .261 | .146 | .091 | .025 | .049 | .245 | .400 | .277 | .029 | .059 | .083 | .187 | .386 | .285 |
| .432 | .299 | .175 | .051 | .043 | .067 | .198 | .328 | .366 | .04 | .071 | .043 | .132 | .285 | .468 | |
| Dramatic Relief Items | |||||||||||||||
| 3 Get upset when I think about illnesses caused by drinking | .527 | .216 | .151 | .081 | .025 | .213 | .309 | .365 | .111 | .002 | .227 | .217 | .311 | .189 | .055 |
| .377 | .26 | .212 | .128 | .024 | .062 | .257 | .382 | .26 | .04 | .088 | .155 | .300 | .221 | .236 | |
| 11 Warnings about health hazards have emotional effect on me | .468 | .256 | .195 | .060 | .021 | .131 | .376 | .351 | .129 | .012 | .122 | .173 | .297 | .268 | .140 |
| .37 | .277 | .239 | .092 | .022 | .061 | .265 | .388 | .249 | .038 | .100 | .125 | .264 | .285 | .225 | |
| 19 Stories about alcohol/effects upset me | .610 | .220 | .095 | .051 | .024 | .141 | .365 | .390 | .093 | .011 | .159 | .207 | .299 | .234 | .102 |
| .39 | .278 | .26 | .061 | .012 | .073 | .323 | .398 | .182 | .024 | .18 | .184 | .284 | .202 | .149 | |
| 29 Read newspaper stories that affect me emotionally | .765 | .146 | .075 | .014 | .000 | .253 | .428 | .292 | .026 | .002 | .261 | .235 | .324 | .123 | .058 |
| .599 | .258 | .124 | .019 | 000 | .138 | .402 | .379 | .079 | .003 | .254 | .211 | .278 | .186 | .072 | |
| Social Liberation Items | |||||||||||||||
| 21 Society changes in ways that helps me overcome drinking | .407 | .261 | .228 | .069 | .035 | .111 | .317 | .402 | .162 | .009 | .128 | .156 | .278 | .303 | .135 |
| .282 | .308 | .286 | .107 | .017 | .044 | .204 | .43 | .313 | .008 | .101 | .105 | .235 | .359 | .201 | |
| 4 See signs helping people not drink | .582 | .245 | .135 | .033 | .004 | .242 | .380 | .333 | .045 | .000 | .247 | .249 | .347 | .121 | .035 |
| .471 | .239 | .231 | .053 | .006 | .141 | .328 | .388 | .129 | .015 | .21 | .211 | .299 | .177 | .102 | |
| 13 People make known desire not to be pressed to drink | .647 | .191 | .112 | .029 | .021 | .185 | .408 | .331 | .068 | .008 | .163 | .193 | .343 | .222 | .078 |
| .353 | .342 | .245 | .05 | .009 | .063 | .268 | .444 | .213 | .013 | .089 | .132 | .307 | .285 | .186 | |
| 38 See ads on TV how society helps people not to drink | .508 | .298 | .153 | .041 | .000 | .171 | .412 | .349 | .063 | .004 | .150 | .286 | .336 | .156 | .071 |
| .247 | .324 | .309 | .094 | .027 | .043 | .244 | .449 | .242 | .022 | .06 | .145 | .287 | .296 | .212 | |
| Environmental Reevaluation Items | |||||||||||||||
| 5 Think about how my drinking is hurting people | .472 | .256 | .154 | .089 | .028 | .089 | .259 | .464 | .180 | .007 | .092 | .122 | .257 | .416 | .113 |
| .186 | .295 | .362 | .128 | .030 | .025 | .094 | .360 | .480 | .041 | .049 | .050 | .160 | .351 | .39 | |
| 14 People around me would be better off without my drinking | .414 | .253 | .188 | .097 | .048 | .093 | .206 | .416 | .272 | .013 | .094 | .075 | .146 | .375 | .310 |
| .259 | .243 | .321 | .135 | .042 | .045 | .127 | .337 | .422 | .068 | .086 | .057 | .148 | .297 | .413 | |
| 22 Strong feeling how my drinking has hurt people I care about | .316 | .250 | .233 | .166 | .034 | .047 | .226 | .405 | .295 | .027 | .027 | .061 | .175 | .387 | .350 |
| .128 | .219 | .378 | .188 | .087 | .002 | .067 | .268 | .546 | .117 | .013 | .018 | .075 | .268 | .626 | |
| 31 Think my drinking is causing problems for others | .455 | .237 | .227 | .062 | .020 | .068 | .309 | .442 | .174 | .006 | .080 | .060 | .208 | .388 | .264 |
| .260 | .289 | .315 | .100 | .035 | .028 | .134 | .366 | .44 | .031 | .044 | .044 | .141 | .331 | .44 | |
| Self Reevaluation Items | |||||||||||||||
| 6 Feeling good about myself includes changing my drinking | .074 | .127 | .297 | .338 | .164 | .016 | .068 | .247 | .561 | .081 | .013 | .010 | .050 | .395 | .532 |
| .079 | .158 | .353 | .307 | .104 | .011 | .016 | .158 | .667 | .148 | .004 | .009 | .040 | .250 | .696 | |
| 23 Disappointed with self when I depend on alcohol | .320 | .164 | .214 | .205 | .096 | .032 | .109 | .334 | .415 | .110 | .099 | .057 | .100 | .276 | .469 |
| .179 | .16 | .292 | .234 | .136 | .034 | .072 | .207 | .485 | .202 | .057 | .019 | .07 | .185 | .669 | |
| 32 Feel more competent when I decide not to drink | .162 | .149 | .187 | .274 | .229 | .014 | .070 | .306 | .508 | .103 | .005 | .000 | .050 | .310 | .634 |
| .128 | .118 | .307 | .299 | .148 | .001 | .009 | .18 | .641 | .006 | .004 | .008 | .206 | .775 | .006 | |
| 39 Think about type of person I will be if I control my drinking | .185 | .150 | .331 | .221 | .114 | .004 | .102 | .440 | .388 | .066 | .023 | .020 | .088 | .392 | .477 |
| .101 | .135 | .356 | .267 | .141 | .026 | .07 | .224 | .560 | .119 | .058 | .031 | .053 | .211 | .647 | |
| Self Liberation Items | |||||||||||||||
| 12 Use will power to stop from drinking | .197 | .202 | .244 | .194 | .163 | .024 | .133 | .420 | .346 | .077 | .040 | .033 | .185 | .345 | .398 |
| .16 | .173 | .306 | .203 | .159 | .036 | .135 | .342 | .41 | .077 | .096 | .101 | .172 | .241 | .390 | |
| 20 Make myself aware I can choose to overcome my drinking | .114 | .209 | .285 | .226 | .166 | .006 | .074 | .367 | .455 | .098 | .005 | .008 | .041 | .350 | .597 |
| .078 | .122 | .331 | .326 | .143 | .008 | .024 | .231 | .595 | .141 | .005 | .000 | .032 | .228 | .735 | |
| 30 Tell myself if I try hard enough, I can stop drinking | .234 | .235 | .231 | .204 | .096 | .024 | .116 | .398 | .391 | .064 | .021 | .015 | .102 | .351 | .511 |
| .122 | .177 | .33 | .251 | .12 | .014 | .054 | .285 | .519 | .128 | .041 | .034 | .07 | .205 | .65 | |
| 37 Make commitments to myself not to drink | .236 | .217 | .237 | .168 | .142 | .017 | .131 | .372 | .388 | .093 | .008 | .013 | .071 | .354 | .554 |
| .160 | .198 | .287 | .201 | .154 | .004 | .044 | .252 | .530 | .170 | .010 | .025 | .064 | .259 | .643 | |
| Consciousness Raising Items | |||||||||||||||
| 15Read newspaper stories that may help me quit | .731 | .175 | .075 | .015 | .004 | .269 | .358 | .325 | .047 | .000 | .239 | .221 | .315 | .155 | .071 |
| .57 | .286 | .118 | .024 | .002 | .138 | .412 | .354 | .094 | .001 | .233 | .217 | .303 | .182 | .065 | |
| 24 Look for information related to problem drinking | .618 | .194 | .145 | .033 | .011 | .073 | .314 | .449 | .143 | .021 | .079 | .165 | .335 | .248 | .173 |
| .447 | .310 | .193 | .047 | .003 | .050 | .267 | .467 | .197 | .018 | .091 | .115 | .282 | .308 | .203 | |
| 33 Seek groups who increase my awareness | .812 | .116 | .036 | .027 | .008 | .268 | .395 | .265 | .057 | .014 | .218 | .192 | .248 | .207 | .135 |
| .526 | .295 | .129 | .042 | .008 | .056 | .269 | .309 | .314 | .052 | .097 | .084 | .149 | .224 | .446 | |
| 40 Think about information on the benefits of quitting drinking | .424 | .242 | .210 | .099 | .024 | .048 | .195 | .522 | .222 | .012 | .022 | .062 | .223 | .382 | .311 |
| .190 | .230 | .371 | .167 | .043 | .005 | .076 | .35 | .524 | .045 | .020 | .020 | .096 | .319 | .545 | |
Note. Response option 1 = Never, 2 = Seldom, 3 = Occasionally, 4 = Frequently, 5 = Repeatedly. PCQ = Processes of Change Questionnaire
Alcohol use outcomes
The Form-90 (Miller, 1996) and the Timeline Follow-back Interview (TLFB; Sobell & Sobell, 1992) were used to assess alcohol use outcomes. The Form-90 and the TLFB are both calendar-based interview methods to assess a person’s drinking behavior. In COMBINE, the Form-90 was used to assess drinking behavior during the period prior to beginning treatment and the period following treatment and the TLFB was used to assess drinking behavior during the 16-week treatment period. In MATCH, the Form-90 was used to assess drinking behavior prior to, during, and following treatment. In this study, we examined two indices of alcohol consumption derived from the Form-90 and TLFB: percent days abstinent (PDA), defined as the percentage of days during a given interval in which the individual reported no drinking, and drinks per drinking day (DDD), defined as the average number of drinks on days that an individual reported any drinking. In both COMBINE and MATCH, we examined PDA and DDD during the final week of the treatment period (week 16 for COMBINE and week 12 for MATCH) and during the 30 days prior to the first post-treatment follow-up assessment (month 6.5 for COMBINE and month 6 for MATCH, corresponding to approximately 3 months post-treatment in both studies). Baseline values for PDA and DDD were computed based on the 30-days prior to the baseline assessment. For covariate analyses of predictors of latent class membership, we examined baseline percent heavy drinking days (PHD), defined as the percentage of days during the 30-day baseline period in which an individual reported heavy drinking (5 or more standard drinks for men; 4 or more standard drinks for women.
Alcohol-related consequences
In both COMBINE and MATCH, alcohol-related consequences were assessed with the Drinker Inventory of Consequences (DrInC; Miller, Tonigan, & Longabaugh, 1995), a 50-item measure using a Likert-type response scale (1 = never, 4 = daily or almost daily). In this study, we used the DrInC to assess alcohol-related consequences at baseline and the 3-month post-treatment follow-up. The DrInC administration at baseline asked participants to report on alcohol-related consequences in the past 90 days whereas the DrInC administration at the 3-month post-treatment follow-up asked participants to report on alcohol-related consequences experienced since the last interview, which was at the end-of-treatment for both studies. In COMBINE, the DrInC was administered to all participants regardless of their drinking status at a given assessment. In MATCH, the DrInC was only administered to individuals who reported drinking at a given assessment (e.g., it was not administered to abstainers).
Covariates
A demographic questionnaire was used to assess a number of demographic covariates including gender, race, marital status, ethnicity, age, and years of education. The University of Rhode Island Change Assessment (URICA) was used to measure baseline readiness to change (McConnaughy, Prochaska, & Velicer, 1983). The URICA is a 24-item measure using Likert-type responses (1 = Strongly Disagree, 5 = Strongly Agree). To assess readiness to change, we used the Overall Readiness Score, which is derived by summing the means of the contemplation, action, and maintenance subscales and then subtracting the mean of the precontemplation subscale. The Alcohol Dependence Scale (ADS), a 25-item self-report measure, was used to assess baseline severity of alcohol dependence (Skinner & Allen, 1982). In COMBINE only, the Treatment Experiences and Expectancies questionnaire which included a question about drinking goals from the Thoughts about Abstinence Scale (Hall, Havassy, & Wasserman, 1990) was used to assess drinking goal at baseline.
Statistical Analyses
SPSS Version 22 was used to prepare the data and conduct descriptive analyses. Mplus Version 7.2 (Muthén & Muthén, 2012) was used to conduct all other analyses. We used finite mixture modeling to examine subpopulations of coping based on the PCQ data. First we examined whether qualitatively distinct patterns of coping could be observed among the 40 items of the PCQ using latent class analysis (LCA). Second, in supplementary analyses, we examined whether qualitatively distinct patterns of coping could be observed among the 10 subscales of the PCQ using latent profile analysis (LPA). Our primary focus was on the LCA models of the 40 items of the PCQ because this analysis provided the broadest range of coping items with each item as a categorical indicator of latent class using the full range of responses across the 5 responses on the Likert-type scale (1= Never to 5 = Repeatedly) of the PCQ items. Our secondary focus was an LPA of the 10 subscales of the PCQ, which we included to build upon prior literature that has examined PCQ subscales (Belding, Iguchi, Lamb, Lakin, & Terry, 1995; Carbonari & DiClemente (2000); Freyer et al., 2006; Snow et al., 1994).
LCA and LPA are latent variable modeling methods for classifying individuals into distinct groups based on similar patterns of data (Collins & Lanza, 2010). To determine the optimal number of classes to represent the data, we used the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (Lo et al., 2001), which compares whether a k class solution fits better than a k – 1 class solution. We also examined Akaike’s Information Criterion (AIC), the Bayesian Information Criterion (BIC), sample size adjusted BIC (aBIC), and entropy to determine the optimal number of classes to represent the data. Lower values of AIC, BIC and aBIC indicate a better fitting model. Higher entropy values indicate better classification precision, meaning that a response pattern is characteristic of a particular class and not other classes. Parameters were estimated using maximum likelihood estimation with robust standard errors (MLR). For LCA, parameters of interest were: latent class prevalences and the probability of each response for a variable given that an individual belongs to a particular latent class. For LPA, parameters of interest were latent class prevalences and conditional response means for each class.
To examine the association between baseline covariates and latent class membership, we used the Modal Maximum Likelihood (ML) method for analyzing predictors of latent class (Vermunt, 2010), which accounts for classification error when estimating the associations between covariates and latent class. For COMBINE, the covariates used in the regression model predicting latent classes included baseline PHD, treatment assignment (received CBI vs. did not receive CBI), age, marital status (married vs. not married), gender, years of education completed, race (white vs. non-white), baseline readiness to change, baseline alcohol dependence severity, and drinking goal (abstinence vs. other goal). For MATCH, the covariates used included baseline PHD, treatment contrast 1 (TSF vs. MET), treatment contrast 2 (CBT vs. MET), treatment arm (outpatient vs. aftercare), age, marital status (married vs. not married), gender, years of education completed, race (white vs. non-white), baseline readiness to change, and baseline alcohol dependence severity. Because PDA, DDD, and PHD are highly correlated, including all of these variables as predictors may have produced collinearity issues. Hence, we decided to include PHD alone as a drinking variable in the covariate model because PHD captures how often a person is drinking a certain amount, rather than just capturing how much one is drinking per episode (DDD) or how often one is drinking overall (PDA).
We also examined differences in alcohol-related outcomes (i.e., “distal outcomes”) among latent classes using the BCH method (Bakk &Vermunt, 2016). The BCH method accounts for classification error when estimating the means of continuous distal outcome variables across latent classes. For each of the distal outcome analyses conducted in both COMBINE and MATCH we controlled for the following covariates: baseline alcohol use or alcohol-related consequences (using the baseline summary score that corresponds to the distal outcome used in the analysis), treatment assignment (COMBINE only: received CBI vs. did not receive CBI), treatment arm (MATCH only: outpatient vs. aftercare), age, marital status, gender, years of education completed, race, baseline readiness to change, and baseline alcohol dependence severity. These covariates were chosen based on prior research on the COMBINE data (Anton et al., 2006) and MATCH data (Project MATCH Research Group, 1998), as well as considerations of what other variables might be related to coping repertoire. The first set of distal outcome analyses examined differences in PDA and DDD, during the final week of treatment. The second set of analyses evaluated differences in PDA, DDD, and alcohol-related consequences at the 3-month post-treatment follow-up assessment.
Results
Latent Class Analyses
Class enumeration
In both COMBINE and MATCH, the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LRT) indicated a two-class solution fit better than a one-class solution (p < 0.01), a three-class solution fit better than a two-class solution (p < 0.01), but a 4-class solution did not fit significantly better than a three-class solution (p > .05). Table 1 presents fit statistics for class solutions ranging from one class to six classes. Entropy is high for classes one through six and the AIC, BIC, and adjusted BIC continue to decrease from classes one through five. Based on the results from the LRT we chose the three-class solution, which had an entropy level of .950 in COMBINE and .944 in MATCH, indicating excellent classification precision.
Table 1.
Fit Statistics for Class Solutions 1 through 6 for Latent Class Analysis
| COMBINE | ||||||
|---|---|---|---|---|---|---|
| Number of Classes | ||||||
| Fit Statistics | 1 | 2 | 3 | 4 | 5 | 6 |
| AIC | 128593.747 | 120637.022 | 116677.467 | 114669.244 | 113621.000 | 112887.470 |
| BIC | 129394.383 | 122243.297 | 119089.382 | 117886.799 | 117644.195 | 117716.305 |
| Adjusted BIC | 128886.185 | 121223.725 | 117558.435 | 115844.478 | 115090.499 | 114651.235 |
| Lo-Mendell-Rubin test | 8271.390 | 4277.761 | 2327.578 | 1368.844 | 1075.537 | |
| ----- | p < 0.01 | p < 0.01 | p = .812 | p = .7667 | p = .7636 | |
| Entropy | ----- | 0.945 | 0.950 | 0.953 | 0.952 | 0.954 |
| MATCH | ||||||
| AIC | 184893.035 | 172408.585 | 165638.973 | 163017.482 | 161485.498 | 160242.561 |
| BIC | 185752.171 | 174132.227 | 168227.121 | 166470.135 | 165802.657 | 165424.226 |
| Adjusted BIC | 185243.884 | 173112.476 | 166695.906 | 164427.456 | 163248.514 | 162358.619 |
| Lo-Mendell-Rubin test | 12795.665 | 7085.640 | 2941.015 | 1852.423 | 1563.619 | |
| ----- | p < 0.01 | p < 0.01 | p = .7580 | p = .8324 | p = .8062 | |
| Entropy | ----- | 0.936 | 0.944 | 0.943 | 0.944 | 0.940 |
Note. Akaike’s Information Criterion (AIC), the Bayesian Information Criterion (BIC), sample size adjusted BIC (adjusted BIC). Lower values of AIC, BIC and Adjusted BIC indicate a better fitting model
Class descriptions
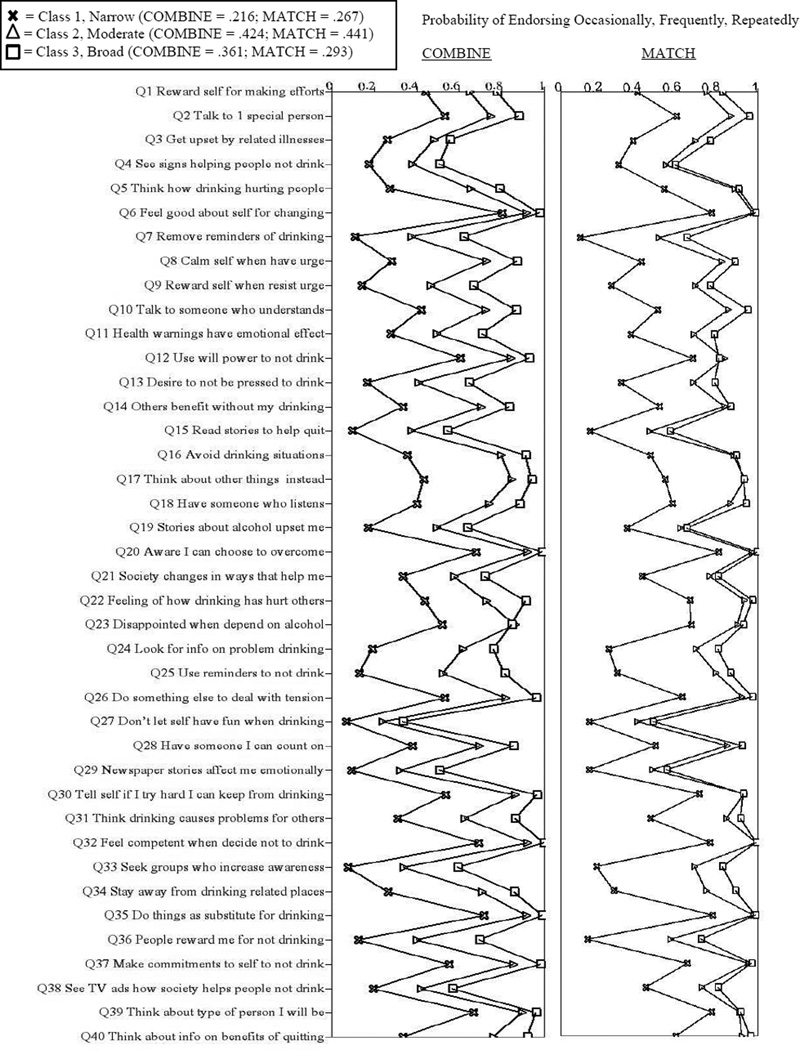
The latent class prevalence (P) within each class provides an estimation of the proportion of individuals most likely classified in each class based on estimated posterior probabilities and these proportions were similar in both COMBINE and MATCH: (Class 1: COMBINE P = .216; MATCH P = .267; Class 2: COMBINE P=.424; MATCH P = .441; Class 3: COMBINE P = .361; MATCH P = .293). Table 2 presents the response probabilities for each latent class across the 40 PCQ items. The values in Table 2 indicate the probability that an individual would provide a certain response to each item (values 1 = never through 5= repeatedly) given expected classification to a particular class. Overall, the patterns of latent class response probabilities among the 3 classes were remarkably similar between COMBINE and MATCH. An inspection of Table 2 reveals that in both COMBINE and MATCH Class 3 had the highest probability of responding with a response of 5 (repeatedly) across all 40 items compared to Class 1 and 2. Additionally, in both COMBINE and MATCH Class 1 had the highest probability of responding with a response of 1 (Never) across all 40 items compared to Class 2 and 3. To summarize these data we produced a line graph (Figure 1) that depicts the probability of endorsing either occasionally, frequently, or repeatedly (responses 3, 4, and 5 on the Likert Scale) on a given item based on expected class membership. Based the overall patterns of results from Table 2 and Figure 1, we labeled class one in both samples as the “narrow repertoire class,” because results indicated that this class only had a narrow range of skills that were used consistently. We labeled class two as the “moderate repertoire class” because results indicated that this class had a moderate range of skills that were used consistently. We labeled class three as the “broad repertoire class” because this class because results indicated that this class had a broad range of skills that were used consistently. Compared to the moderate class in COMBINE, the moderate class in MATCH had a somewhat higher probability of endorsing occasionally, frequently, or repeatedly across the 40 items.
Figure 1.
Latent class item response probabilities for occasionally, frequently, or repeatedly.
Predictors of class membership
Table 3 depicts covariate effects on class membership with the broad class (Class 3) as the reference group. In both studies, greater baseline readiness to change (COMBINE: OR = 0.677; MATCH: OR= 0.613) and greater baseline alcohol dependence severity (COMBINE: OR = 0.923; MATCH OR: 0.946) were significantly associated with a decreased probability for expected classification in the narrow class relative to the broad class. In addition, receiving the combined behavioral intervention (OR = 0.684), being married (OR = 0.600), and an abstinence drinking goal (OR = 0.571) in COMBINE; and older age (OR = .974), female gender (OR = 0.476), and being in the aftercare treatment arm (OR = .676) in MATCH were significantly associated with a decreased probability for expected classification in the narrow class relative to the broad class. In MATCH, percent heavy drinking (PHD) days at baseline (OR = 1.010) was significantly associated with an increased probability for expected classification in the narrow class relative to the broad class.
Table 3.
Predictors of Class Membership with Class 3 (Broad Class) as the Reference Class
| COMBINE | ||||||
|---|---|---|---|---|---|---|
| Class 1 (Narrow Repertoire) | Class 2 (Moderate Repertoire) | |||||
| Variable | OR | 95% CI | B (SE) | OR | 95% CI | B (SE) |
| Age | .9880 | 0.968, 1.007 | − 0.012(0.010) | 0.989 | 0.973,1.004 | − 0.011(0.008) |
| Married | 0.600 | 0.153,1.047 | − 0.510(0.228)* | 0.829 | 0.496,1.162 | − 0.187(0.170) |
| Female | 0.936 | 0.546,1.326 | − 0.066(0.199) | 0.813 | 0.500,1.127 | − 0.206(0.160) |
| Years of Education | 1.000 | 0.921,1.078 | − 0.000(0.040) | 1.010 | 0.949,1.070 | 0.010(0.031) |
| Non-White | 0.757 | 0.277,1.237 | − 0.278(0.245) | 0.623 | 0.247,1.000 | − 0.472(0.192)* |
| Baseline Readiness | 0.677 | 0.548,0.807 | − 0.389(0.066)** | 0.734 | 0.630,0.838 | − 0.309(0.053)** |
| Baseline ADS | 0.923 | 0.893,0.952 | − 0.080 (0.015)** | 0.985 | 0.963,1.097 | − 0.015(0.011) |
| Received CBI | 0.684 | 0.324, 1.045 | − 0.379(0.184)* | 0.876 | 0.580,1.172 | − 0.132(0.151) |
| Abstinence Goal | 0.571 | 0.193,0.949 | − 0.560 (0.193)** | 0.810 | 0.498,1.122 | −0.211 (0.159) |
| MATCH | ||||||
| Age | 0.974 | 0.958,0.990 | − 0 .026 (0.008)** | 0.985 | 0.973,0.998 | − 0.015 (0.006)* |
| Married | 0.898 | 0.5648,1.231 | − 0.108 (0.170) | 0.758 | 0.466,1.050 | − 0.277 (0.149) |
| Female | 0.476 | 0.133,0.819 | − 0.741 (0.175)** | 0.470 | 0.176,0.764 | − 0.756 (0.150)** |
| Years of Education | 1.078 | 0.999,1.156 | 0.076 (0.040) | 1.058 | 0.993,1.123 | 0.057 (0.033) |
| Non-White | 0.500 | 0.112,0.888 | − 0.693(0.198) | 0.527 | 0.197,0.856 | − 0.640 (0.168)** |
| Baseline Readiness | 0.613 | 0.486,0.740 | − 0.490 (0.065)** | 0.691 | 0.579,0.803 | − 0.370 (0.057)** |
| Baseline ADS | 0.946 | 0.924,0.968 | − 0.055 (0.011)** | 0.990 | 0.972,1.008 | − 0.010 (0.009) |
| Treatment Arm | 0.676 | 0.358,0.994 | − 0.392 (0.162)* | 0.763 | 0.483,1.043 | − 0.270 (0.143) |
| TSF vs MET | 0.872 | 0.554,1.190 | − 0.137 (0.162) | 0.974 | 0.696,1.252 | − 0.026 (0.142) |
| CBT vs MET | 1.018 | 0.700,1.336 | 0.018 (0.162) | 1.001 | 0.723,1.279 | 0.001 (0.142) |
Note.
p < 0.05
p < 0.01.
OR = odds ratio; CI = Confidence Interval; CBI = Combined Behavioral Intervention; PHD = Percent heavy drinking days; ADS = Alcohol Dependence Scale scores; Treatment Arm (Outpatient=1; Aftercare = 2).
Being non-white (COMBINE: OR = 0.623; MATCH: OR = 0.527) and greater baseline readiness to change (COMBINE: OR = 0.734; MATCH: OR = 0.691) were significantly associated with a decreased probability of expected classification in the moderate class relative to the broad class in both studies. In addition, older age (OR = 0.985) and female gender (OR = 0.470) were significantly associated with a decreased probability of expected classification in the moderate class relative to the broad class in MATCH. When the narrow class was compared to the moderate class, greater baseline alcohol dependence severity in both studies (COMBINE: OR = 1.067; MATCH: OR = 1.046), being married in MATCH (OR= 1.470), and greater baseline readiness to change in MATCH (OR = 1.127) were associated with an increased probability of expected classification in the moderate class relative to narrow class (other non-significant findings from narrow vs moderate class comparison not presented).
Differences in alcohol-related outcomes among latent classes
Table 4 presents comparisons of alcohol-related outcomes among the three coping repertoire classes in both COMBINE and MATCH. In COMBINE, at the end-of-treatment (EOT) and at the 3-month post treatment follow-up (month 3), the broad class demonstrated significantly greater PDA, less DDD, and PHD, and fewer alcohol-related consequences than the moderate and narrow classes. In COMBINE, there were no differences in any alcohol use outcomes between the moderate and narrow classes. In MATCH, at EOT and month 3, the broad class also had significantly greater PDA, and less DDD and PHD than the moderate and narrow classes. However, unlike COMBINE, in MATCH the moderate class had better outcomes than the narrow class on PDA and PHD at EOT and month 3, and on DDD at EOT. There were no differences between the moderate and narrow classes on DDD at month 3. Finally, in MATCH the broad class had fewer alcohol-related consequences than the moderate class at month 3. However, there were no significant differences at month 3 on alcohol-related consequences between the broad and narrow class and between the moderate and narrow class. Thus, in both studies the broad class fared the best across outcome measures compared to the moderate and narrow classes, whereas there were no differences between the moderate and narrow classes in COMBINE and the moderate class fared somewhat better than the narrow class in MATCH.
Table 4.
Mean Comparisons on Alcohol Outcomes among Latent Classes
| COMBINE | ||||||
|---|---|---|---|---|---|---|
| Means | Class Comparisons | |||||
| Class 1: | Class 2: | Class 3: | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | |
| Narrow | Moderate | Broad | χ2 | χ2 | χ2 | |
| PDA End of treatment | 70.038 | 71.171 | 87.521 | 0.128 | 32.866** | 66.357** |
| PDA Month 3 | 63.869 | 64.451 | 80.49 | 0.034 | 28.049** | 53.389** |
| DDD End of treatment | 3.451 | 3.754 | 2.085 | 0.467 | 9.666** | 29.375** |
| DDD Month 3 | 4.360 | 5.097 | 2.982 | 2.412 | 8.986** | 33.454** |
| DrInC Month 3 | 18.596 | 20.100 | 13.218 | 0.468 | 6.245* | 23.962** |
| MATCH | ||||||
| PDA End of treatment | 73.214 | 84.545 | 91.814 | 25.541** | 66.884** | 19.644** |
| PDA Month 3 | 71.425 | 78.989 | 87.946 | 10.919** | 48.737** | 23.066** |
| DDD End of treatment | 4.969 | 3.549 | 2.025 | 7.752** | 35.026** | 14.00** |
| DDD Month 3 | 6.056 | 5.548 | 3.608 | 0.995 | 20.629** | 15.750** |
| DrInC Month 3 | 30.729 | 33.23 | 27.72 | 1.557 | 1.193 | 4.20** |
Note.
p < 0.05
p < 0.01;
PDA = Percent days abstinent. PHD = Percent heavy drinking days; DDD = Drinks per drinking day; DrInC = Drinker Inventory of Consequences.
Examining Patterns of Coping across the PCQ Subscales using Latent Profile Analysis
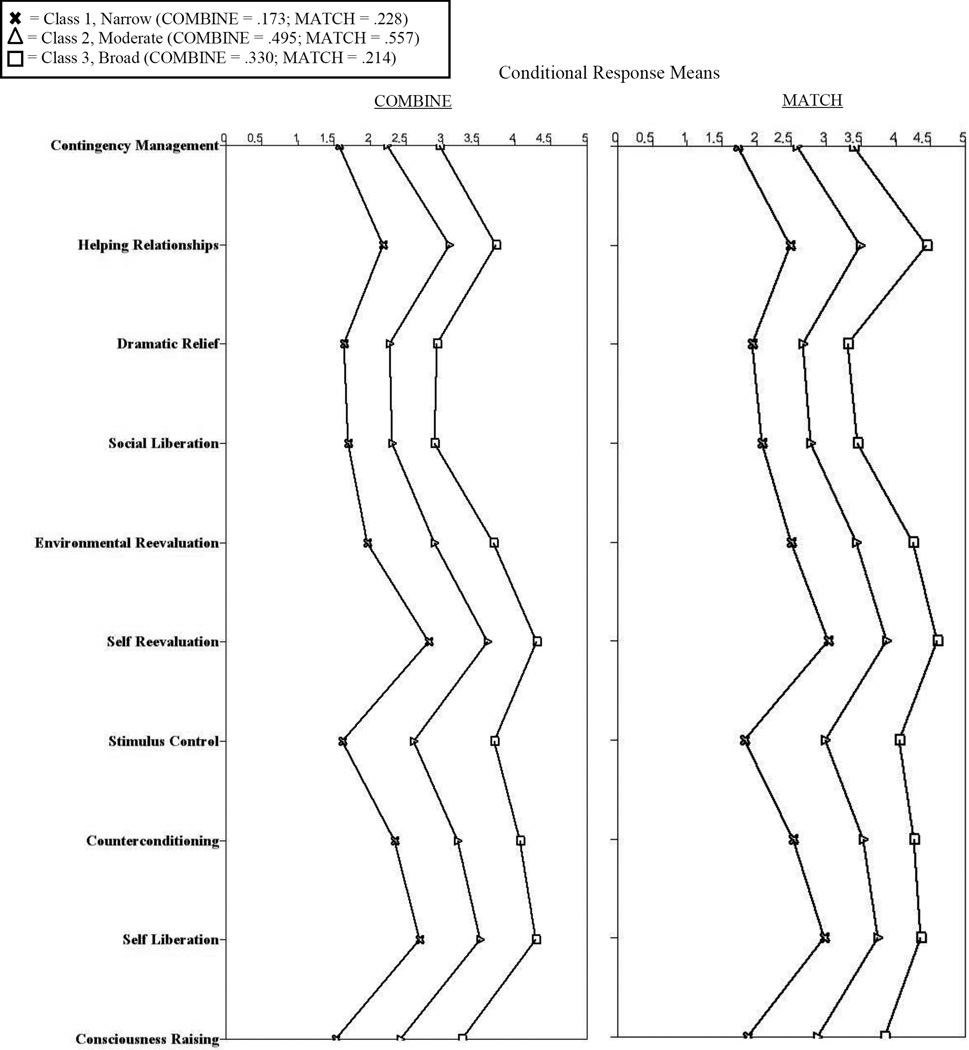
We conducted latent profile analyses to explore patterns of using different types of coping skills, as presented by the 10 PCQ subscales. Given latent profile models were supplementary analyses, we do not report the predictors of class membership and have focused on examining mean differences in alcohol outcomes across identified classes from the latent profile analyses. The predictors of class membership were similar to the LCA results and are available upon request from the first author. Based on the Likelihood Ratio Test (3-class fit better than 2-class solution) and AIC, BIC, and aBIC fit indices (sharp increase from 3-class to 4-class), we settled on a 3-class solution for COMBINE and MATCH. The entropy of the 3-class solution was high in both samples (MATCH: .856 and COMBINE: .883). Figure 2 depicts the estimated pattern of means on the 10 PCQ subscales across the latent classes. The estimated class proportions were similar in both COMBINE and MATCH: (Class 1: COMBINE P = .173; MATCH P = .228; Class 2: COMBINE P=.495; MATCH P = .557; Class 3: COMBINE P = .330; MATCH P = .214). Again, in both COMBINE and MATCH we found a broad repertoire class, a moderate repertoire class, and a narrow repertoire class. A mean of at least 3 on the PCQ indicates that a skill was used at least occasionally. The broad repertoire class is clearly using a wider range of skills at a level of at least occasionally or more (COMBINE: 7 out of 10 skills; MATCH: 10 out of 10 skills). On the other hand, the moderate repertoire class is using a moderate range of skills at a level of at least occasionally (COMBINE: 4 out of 10; MATCH: 5 out of 10) and the narrow repertoire class is barely using any skills at a level of at least occasionally (COMBINE: 0 out of 10: MATCH: 1 out of 10). Table 5 shows the mean comparisons on alcohol outcomes across the three classes identified from the latent profile analyses. Overall, the pattern of mean differences among classes was identical to that obtained from the latent class models, except for some differences. We found the following results in LPA models but not LCA models: 1) in COMBINE the broad class did not have significantly fewer alcohol-related consequences than the moderate class, 2) in COMBINE the moderate class had significantly better outcomes than the narrow class on PDA at end of treatment and month 3, and on alcohol-related consequences, 3) in MATCH the broad class did not have significantly fewer alcohol-related consequence than the narrow class. Despite these differences, the substantive pattern of results from Table 5 (LPA models) mirrors the results from Table 4 (LCA models).
Figure 2.
Latent class conditional response means derived from latent profile analysis of subscale scores.
Table 5.
Mean Comparisons on Alcohol Outcomes among Latent Classes Derived From Latent Profile Analyses of Subscale Scores
| COMBINE | ||||||
|---|---|---|---|---|---|---|
| Means | Class Comparisons | |||||
| Class 1: | Class 2: | Class 3: | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | |
| Narrow | Moderate | Broad | χ2 | χ2 | χ2 | |
| PDA End of treatment | 62.674 | 73.086 | 86.831 | 5.3410* | 30.357** | 38.886** |
| PDA Month 3 | 55.384 | 67.439 | 78.046 | 7.462** | 26.734** | 18.503** |
| DDD End of treatment | 4.210 | 3.619 | 2.246 | 0.941 | 10.680** | 15.051** |
| DDD Month 3 | 5.187 | 4.708 | 3.387 | 0.665 | 9.853** | 10.971** |
| DrInC Month 3 | 23.770 | 15.994 | 13.962 | 9.104** | 14.913** | 1.660 |
| MATCH | ||||||
| PDA End of treatment | 68.039 | 83.749 | 93.552 | 30.316** | 80.042** | 32.758** |
| PDA Month 3 | 68.153 | 78.500 | 87.806 | 13.312** | 41.057** | 18.281** |
| DDD End of treatment | 5.878 | 3.446 | 2.049 | 15.443** | 35.910** | 9.279** |
| DDD Month 3 | 6.664 | 5.482 | 3.604 | 3.567 | 21.479** | 12.372** |
| DrInC Month 3 | 30.448 | 32.753 | 27.242 | 1.098 | 0.926 | 2.937 |
Discussion
This study used two large samples of individuals receiving treatment for AUD (the COMBINE study and Project MATCH) to examine how patterns of using alcohol-specific coping skills following treatment were related to alcohol treatment outcomes. We used finite mixture modeling to identify coping repertoire classes, characterized by distinct patterns of coping, as measured by the Processes of Change Questionnaire (PCQ; Prochaska et al., 1988). From the latent class analysis (LCA) models, we identified three latent classes in both samples: 1) a broad repertoire class, which had a broad range of coping skills that were consistently used, 2) a moderate repertoire class, which had a moderate range of coping skills that were consistently used, and a narrow repertoire class, which had a limited range of coping skills that were consistently used. From the LCA models, across both samples the broad repertoire class generally had the best alcohol-related outcomes (drinking frequency and intensity, and alcohol-related consequences), whereas the moderate and narrow repertoire classes had poorer outcomes. Specifically, in both COMBINE and MATCH, at the end-of-treatment (EOT) and the 3-month follow-up (month 3), the broad class demonstrated less drinking frequency (PDA) and intensity (DDD) than the moderate and narrow classes. With respect to alcohol-related consequences, in COMBINE, the broad class had fewer alcohol-related consequences at month 3 than both the narrow and moderate classes. In MATCH, however, the broad class had fewer alcohol-related consequences than the moderate class, but the broad class was not significantly different from the narrow class. The inconsistency in these findings between COMBINE and MATCH may be partly due to the fact that in MATCH the DrInC was only administered to individuals who reported drinking at a given assessment; however, in COMBINE the DrInC was administered to all participants. Thus, in MATCH the results regarding differences in alcohol-related consequences among classes should be viewed in light of the important caveat that the findings could have been affected by the large portion of individuals (n = 566) in MATCH who were abstinent from drinking and not administered the DrInC. Across both samples we found inconsistent evidence that the moderate class had better outcomes than the narrow class. In COMBINE, there were no differences on any outcomes between the narrow and moderate class. In MATCH, however, the moderate class had better outcomes than the narrow class on PDA and PHD at EOT and month 3, and on DDD at EOT, but not month 3. Differences in these findings between COMBINE and MATCH may have resulted in part because the moderate class in MATCH displayed a somewhat greater probability of using coping skills more frequently compared to the moderate class in COMBINE. A moderately broad repertoire may confer some advantage over a narrow repertoire, yet this is still not entirely clear.
Prior studies among individuals with alcohol and drug use disorders have used subscales of the PCQ to measure different types of coping (Belding et al., 1995; Carbonari & DiClemente (2000); Freyer et al., 2006; Snow et al., 2010). Thus, as supplementary analyses we also conducted latent profile analyses (LPA) to explore patterns of coping across the 10 subscales of the PCQ. Using LPA we identified the same 3 latent classes in both samples. Results from the LPA models regarding differences in alcohol-related outcomes among latent classes were very similar to results from the LCA models. Based on the collective results from the LCA and LPA models, the main findings were: 1) the broad class clearly had better alcohol use outcomes than the moderate and narrow classes, 2) there was inconsistent evidence that the moderate class fared better than the narrow class on alcohol use outcomes, and 3) results regarding alcohol-related consequences were slightly mixed and provided modest support for the broad class having fewer alcohol-related consequences than the moderate and narrow repertoire classes.
The present study also examined pre-treatment factors as predictors of patterns of coping following treatment. In both COMBINE and MATCH, greater baseline readiness to change and greater baseline alcohol dependence severity predicted expected classification to the broad class, relative to the narrow class. These findings may have resulted in part because individuals with greater alcohol dependence may need the assistance of a wider range of strategies to change their alcohol use and because individuals who are more motivated to change are more willing to try various strategies. In MATCH, we found that being in the aftercare arm predicted expected classification to the broad class, relative to the narrow class, which may have resulted because individuals in the aftercare arm may have entered the study already having more coping skills from prior treatment. In COMBINE, we found that an abstinence-based drinking goal predicted expected classification to the broad class, relative to the narrow class. Those with the goal of stopping drinking altogether may be more motivated to acquire and utilize a variety of strategies in order to remain abstinent. In both COMBINE and MATCH, we found that being non-white predicted expected classification to the broad class, relative to the moderate class. In MATCH, we found that female gender was a strong predictor of expected classification to the broad class, relative to both the narrow and moderate class. However, in COMBINE, gender was not a significant predictor of class membership. The reasons behind these findings regarding gender and race predicting coping repertoire are not clear. Altogether, future studies should aim to replicate the effects of individual difference factors in predicting coping repertoire to ensure that they are meaningful and not the result of sample specific findings.
In COMBINE, we found that receiving the combined behavioral intervention (CBI) predicted expected classification to the broad class, relative to the narrow class. These results indicate that clients who received CBI, which involved teaching coping skills to clients, were in fact more likely to acquire a diverse range of coping skills. In MATCH, however, we did not find evidence that one of the three types of behavioral treatment differentially predicted coping repertoire. Notably, cognitive-behavioral therapy (CBT) in MATCH was not a significant predictor of expected classification in the broad class. This finding is consistent with other studies that have shown that CBT does not uniquely predict increases in coping compared to other behavioral treatments for AUD (Morgenstern & Longabaugh, 2000). Thus, one type of behavioral treatment may not influence coping repertoire more than another. However our findings do indicate that compared to medical management, more intensive behavioral interventions are more likely to enhance coping skills, and that broadening a client’s coping repertoire may be one specific way by which behavioral interventions affect coping behaviors.
The current study has several limitations. We relied on self-report data to examine coping repertoire and participants’ retrospective reports of coping skills may not accurately reflect actual coping skills used by the individual. The three latent classes of alcohol-specific coping skills identified in this study may be specific to the COMBINE and MATCH participants and may not be representative of different AUD populations. We may have failed to assess important alcohol-specific skills in clients’ repertoires because these skills were not measured on the PCQ. We did not examine how changes in self-efficacy may factor into the present study findings. Self-efficacy and other unexamined variables may be driving the association between a broad coping repertoire and outcomes. Finally, COMBINE and MATCH did not assess coping at baseline so we were unable to examine change in coping repertoire over time.
Besides differences in the broadness of individuals’ repertoires, we did not identify any other qualitative differences between patterns of coping. For example, we did not find a class using a unique combination of types of coping skills. Our results are not consistent with results from Carbonari & DiClemente (2000), who also examined patterns of coping on the PCQ among Project MATCH participants. Whereas their study indicated that abstinent clients had the highest use of behavioral coping and moderate use of cognitive coping, our study does not indicate that this pattern of coping is most effective. Rather the broad class in our study, which had the best outcomes, was frequently using both cognitive and behavioral skills. Differences in the findings from our study and the Carbonari and DiClemente (2000) study may be due to differences in analytic approaches, such as the fact that our study examined patterns across each PCQ item and the 10 PCQ lower-order subscales, whereas Carbonari & DiClemente (2000) used scores on the two higher-order subscales.
Overall, our findings suggest that the broadness of one’s alcohol-specific coping repertoire may be a key factor that mobilizes changes in alcohol use. We found that having a broad coping repertoire following AUD treatment was predictive of better alcohol use outcomes above and beyond other known predictors of alcohol use outcomes including readiness to change, dependence severity, and baseline alcohol use. Our findings are consistent with prior studies among AUD populations (Litman et al., 1979; Litt et al., 2009; Moser & Annis, 1996) and studies among non-AUD populations (Bonanno & Burton, 2013; Lougheed & Hollenstein, 2012). There are several plausible reasons why a broad coping repertoire (i.e., more tools in one’s toolbox) may be adaptive for individuals with AUD. Individuals with a broad coping repertoire may be more equipped to avoid relapse in high-risk situations because they have access to a greater range of strategies that can be flexibly implemented to meet the fluctuating demands of divergent high-risk situations (Bonanno & Burton, 2013; Witkiewitz & Marlatt, 2004). A broad coping repertoire may be effective because individuals have a wider range of alternative responses to choose from besides drinking when they encounter a stressful situation. Moreover, having a broad coping repertoire may foster great self-efficacy to resist drinking in high-risk situations (Marlatt & Gordon, 1985). Future studies are warranted to further examine patterns of coping among AUD populations and to understand how the broadness of one’s coping repertoire plays a role in AUD behavior change.
Public Health Significance: This study shows that coping repertoire, defined as utilizing a broad range of different coping skills, is significantly associated with alcohol treatment outcomes. The findings from this study highlight that coping repertoire may be an important target in the treatment of alcohol use disorder.
Acknowledgments
This research was supported by a grant funded by the National Institute on Alcohol Abuse and Alcoholism (R01 AA022328, Witkiewitz, PI), The content is solely the responsibility of the authors and does not necessarily reflect the views of NIH.
The authors would like to acknowledge Dr. Barbara McCrady and Dr. Kevin Vowles for their valuable feedback on this manuscript.
Contributor Information
Corey R. Roos, Department of Psychology, University of New Mexico
Katie Witkiewitz, Department of Psychology, Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico.
References
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Bakk Z, Vermunt JK. Robustness of stepwise latent class modeling with continuous distal outcomes. Structural Equation Modeling: A Multidisciplinary Journal. 2016;23(1):20–31. [Google Scholar]
- Belding MA, Iguchi MY, Lamb RJ, Lakin M, Terry R. Stages and processes of change among polydrug users in methadone maintenance treatment. Drug and Alcohol Dependence. 1995;39(1):45–53. doi: 10.1016/0376-8716(95)01135-l. [DOI] [PubMed] [Google Scholar]
- Bonanno Ga, Burton CL. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspectives on Psychological Science. 2013;8(6):591–612. doi: 10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- Carbonari JP, DiClemente CC. Using transtheoretical model profiles to differentiate levels of alcohol abstinence success. Journal of Consulting and Clinical Psychology. 2000;68:810–817. [PubMed] [Google Scholar]
- Chaney EF, O’Leary MR, Marlatt GA. Skill training with alcoholics. Journal of Consulting and Clinical Psychology. 1978;46(5):1092–1104. doi: 10.1037//0022-006x.46.5.1092. [DOI] [PubMed] [Google Scholar]
- Cheng C, Lau HPB, Chan MPS. Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychological Bulletin. 2014;140(6):1582–1607. doi: 10.1037/a0037913. [DOI] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Vol. 718. John Wiley & Sons; 2010. [Google Scholar]
- DiClemente CC, Carroll KM, Connors GJ, Kadden RM. Process assessment in treatment matching research. Journal of Studies on Alcohol. 2004;(Supplement 12):156–162. doi: 10.15288/jsas.1994.s12.156. [DOI] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Aldao A, De Los Reyes A. Repertoires of emotion regulation: A person-centered approach to assessing emotion regulation strategies and links to psychopathology. Cognition and Emotion. 2015;29(7):1314–1325. doi: 10.1080/02699931.2014.983046. [DOI] [PubMed] [Google Scholar]
- Dolan SL, Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of alcoholics: relationships of specific strategies to treatment outcome. Drug and Alcohol Dependence. 2013;128(1–2):8–14. doi: 10.1016/j.drugalcdep.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freyer J, Bott K, Riedel J, Wedler B, Meyer C, Rumpf HJ, Hapke U. Psychometric properties of the “processes of change” scale for alcohol misuse and its short form (POC-20) Addictive Behaviors. 2006;31(5):821–832. doi: 10.1016/j.addbeh.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. Journal of Consulting and Clinical Psychology. 1990;58(2):175. doi: 10.1037//0022-006x.58.2.175. [DOI] [PubMed] [Google Scholar]
- Kadden R, Carroll K, Donovan D, Cooney N, Monti P, Abrams…Hester R. Cognitive-behavioral coping skills therapy manual (Project MATCH Monograph Series No. 3) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105(12):2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman GK, Eiser JR, Rawson NS, Oppenheim AN. Differences in relapse precipitants and coping behaviour between alcohol relapsers and survivors. Behaviour Research and Therapy. 1979;17(2):89–94. doi: 10.1016/0005-7967(79)90016-0. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E. Individualized assessment and treatment program for alcohol dependence: results of an initial study to train coping skills. Addiction. 2009;104(11):1837–1838. doi: 10.1111/j.1360-0443.2009.02693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology. 2003;71(1):118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Biometrika. Vol. 88. Los Angeles, CA: Muthén & Muthén; 2001. Testing the number of components in a normal mixture; pp. 767–778. [Google Scholar]
- Lougheed JP, Hollenstein T. A limited repertoire of emotion regulation strategies is associated with internalizing problems in adolescence. Social Development. 2012;21(4):704–721. [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford; 1985. [Google Scholar]
- McConnaughy EA, Prochaska JO, Velicer WF. Stages of change in psychotherapy: Measurement and sample profiles. Psychotherapy: Theory, Research & Practice. 1983;20(3):368–375. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (NIH Publication No. 94–3723) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC) (Project MA.) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Miller WR. Form 90: a structured assessment interview for drinking and related behaviors: test manual (NIH Publication No. 96-4004) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: a review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95(10):1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- Moser AE, Annis HM. The role of coping in relapse crisis outcome: a prospective study of treated alcoholics. Addiction. 1996;91(8):1101–1114. doi: 10.1046/j.1360-0443.1996.91811013.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh 1998–2012. [Google Scholar]
- Nowinski J, Baker S, Carroll K. (NIH Publication No. 94-3722) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. Twelve-step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. [Google Scholar]
- Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: Applications to the cessation of smoking. Journal of Consulting and Clinical Psychology. 1988;56(4):520–528. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical & Experimental Research. 1998;22(6):1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, Abrams DB. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6-and 12-month outcomes. Addiction. 2001;96(8):1161–1174. doi: 10.1046/j.1360-0443.2001.96811619.x. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;91(3):199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Snow MG, Prochaska JO, Rossi JS. Processes of change in alcoholics anonymous: maintenance factors in long-term sobriety. Journal of Studies on Alcohol. 1994;55(3):362–371. doi: 10.15288/jsa.1994.55.362. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Measuring alcohol consumption. New York: Humana Press; 1992. Timeline follow-back; pp. 41–72. [Google Scholar]
- Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Political Analysis. 2010;18(4):450–469. [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychology of Addictive Behaviors. 2008;22(2):157–167. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CF, Silva K, Kecojevic A, Schrager SM, Bloom JJ, Iverson E, Lankenau SE. Coping and emotion regulation profiles as predictors of nonmedical prescription drug and illicit drug use among high-risk adults. Drug and Alcohol Dependence. 2013;132:165–171. doi: 10.1016/j.drugalcdep.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]