Abstract
Objective
This study examined the efficacy of Motivational Interviewing (MI) to reduce hazardous drinking and drug use among adults in treatment for depression.
Methods
Randomized controlled trial based in a large outpatient psychiatry program in an integrated health care system in Northern California. The sample consisted of 307 participants ages 18 and over who reported hazardous drinking, drug use (primarily cannabis) or misuse of prescription drugs in the prior 30 days, and who scored ≥ 5 on the Patient Health Questionnaire (PHQ-9). Participants were randomized to receive either 3 sessions of MI (one in person and two by phone) or printed literature about alcohol and drug use risks (control), as an adjunct to usual outpatient depression care. Measures included alcohol and drug use in the prior 30 days and PHQ-9 depression symptoms. Participants completed baseline in-person interviews and telephone follow-up interviews at 3 and 6 months (96% and 98% of the baseline sample, respectively). Electronic health records were used to measure usual care.
Results
At 6 months, MI was more effective than control in reducing rate of cannabis use (p=.037); and hazardous drinking (≥4 drinks in a day for women, ≥5 drinks in a day for men), (p= .060). In logistic regression, assignment to MI predicted lower cannabis use at 6 months (p= .016) after controlling for covariates. Depression improved in both conditions.
Conclusions
MI can be an effective intervention for cannabis use and hazardous drinking among patients with depression.
Keywords: depression, alcohol, hazardous drinking, cannabis, motivational interviewing
Introduction
Alcohol use has the potential to negatively impact patients in treatment for depression (Sullivan, Fiellin, & O'Connor, 2005). Prior studies in psychiatric settings have identified high rates of co-occurrence between depression and hazardous drinking, e.g., drinking over recommended limits (Roeloffs, Fink, Unutzer, Tang, & Wells, 2001; Sullivan et al., 2005). This can compromise antidepressant treatment (Worthington et al., 1996) and create risk for escalation of alcohol problems (Dixit & Crum, 2000; Kuo, Gardner, Kendler, & Prescott, 2006; Roeloffs et al., 2001). For example, alcohol consumption can increase symptoms of depression such as fatigue and poor sleep (Castaneda, Sussman, Levy, O'Malley, & Westreich, 1998), and suicidality is higher in patients with depression and alcohol problems than it is among those with depression alone. Therefore, it may be advisable for patients in depression treatment to minimize or eliminate drinking, as recommended by the American Psychiatric Association (2010).
Drug use also can be clinically problematic. Among primary care patients with depression, one survey found that 26.3% of women and 29.4% of men reported drug use, including misuse of prescription drugs and illicit drug use (Roeloffs et al., 2001). Cannabis can interfere with depression treatment by decreasing adherence to behavioral interventions or other aspects of care (Bricker et al., 2007). Based on national survey data (Shi, 2014), many adults with depression report efforts to stop using cannabis and thus potentially could be assisted by interventions with demonstrated efficacy.
Many patients with co-occurring substance problems first seek mental health care, yet few studies have examined treatments to reduce alcohol and drug use among depression patients. One promising intervention approach is Motivational Interviewing (MI). MI has been applied to a variety of behavioral health problems, but most extensively tested in reducing alcohol use (Vasilaki, Hosier, & Cox, 2006). MI is a short-term, directive, patient-centered style of counseling to help explore and resolve ambivalence. Active components include listening empathically and evoking patients’ individual reasons for changing their behavior. (Miller & Rollnick, 2012).The therapist's approach is one of non-judgmental guidance, helping the patient move to a higher degree of readiness to change.
To date, research on MI in mental health populations has focused largely on patients with schizophrenia or on psychiatric inpatients (Baker et al., 2002; Martino, Carroll, Nich, & Rounsaville, 2006; Swanson, Pantalon, & Cohen, 1999), and has not examined the broader population of outpatients with depression who might benefit. One study examined reduction in problematic drinking among patients with either comorbid anxiety or depression, including those with alcohol dependence, and did not find an effect of 4-session telephone-administered MI (Grothues et al., 2008). A pilot study examined 3 sessions of MI (one in person and two by telephone) compared with a control group that received an informational brochure on substance use risks. The sample included adults in an outpatient, university-based psychiatry department, who reported hazardous drinking (≥ 3 drinks per occasion) or drug use and who scored ≥ 15 on the Beck Depression Inventory-II (BDI-II). Among those reporting hazardous drinking at baseline (N=73), MI-treated participants were less likely than controls to report any hazardous drinking at 3 months (60.0% vs. 81.8%, p = .043) (Satre, Delucchi, Lichtmacher, Sterling, & Weisner, 2013). The current study examines a similar treatment model in the context of a psychiatry clinic in a health plan, and examines cannabis as well as drinking outcomes.
In this study we aimed to examine the efficacy of MI as a supplement to usual outpatient care. We hypothesized that the intervention would reduce hazardous drinking and potentially reduce drug use and depression. Alcohol and cannabis were identified as the primary substance use outcomes of interest because they are the most commonly used in this population (Davis et al., 2005). In addition to testing bivariate outcomes, we examined predictors of hazardous drinking and cannabis use at 6 months, including depression severity, baseline use, readiness to change, and demographic factors (e.g., older age) based on prior studies of motivation among adults with depression (Satre, Chi, Eisendrath, & Weisner, 2011; Wells-Parker, Dill, Williams, & Stoduto, 2006), controlling for usual care psychiatric and substance use treatment in an integrated health care system.
Materials and Methods
Participants
Study participants were adults 18 and older in the Kaiser Permanente Southern Alameda Medical Center Departments of Psychiatry in Union City and Fremont, California. The clinics provide evaluation, psychotherapy and medication management for patients with a range of mental health problems.
These clinics do not offer specialized services for patients whose primary presenting issue is substance dependence. Individuals are screened by telephone prior to intake, and those seeking substance use treatment or who report serious alcohol or drug problems are referred to the Kaiser Chemical Dependency Recovery Program (CDRP) located within the Union City medical center in a separate building approximately 100 yards from the psychiatry building.
Study inclusion criteria were based on recent hazardous drinking (i.e., any reported days of drinking ≥ 3 drinks in a day for women and ≥ 4 drinks in a day for men in the prior 30 days) or drug use (including any illicit drug use and non-prescribed use of prescription drugs in the prior 30 days) and mild or greater symptoms of depression based on a score of ≥ 5 on the Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer, & Williams, 2001). For study inclusion, we chose a hazardous drinking standard slightly more conservative than that recommended for the general population (≥ 3 drinks in a day for women and ≥ 4 drinks in a day for men), because psychiatry patients frequently are prescribed medications that can have adverse interactions with alcohol. However, we tested outcomes at both the ≥3/≥4 level for women/men respectively and more widely used ≥4/≥5 level. Patients with current mania or psychosis were excluded as such patients would likely require more intensive services.
Participants continued to receive usual depression care based on current best practices for medication management and empirically supported forms of psychological treatment (Kaiser Permanente Care Management Institute, 2006). Decisions on approach to care (e.g., choosing to receive medication and/or participate in psychotherapy) were made collaboratively by clinicians and patients following discussion of treatment options.
Measures
Demographic data were obtained from participants at baseline. Alcohol and drug questions included substance type (cannabis, cocaine, amphetamine-type stimulants, hallucinogens, inhalants, sedatives other than as prescribed, opioids other than as prescribed, heroin or methadone, alcohol, tobacco and other). For each substance, participants were asked the number of days of use in the past 30 days.
Rate of hazardous drinking (≥ 3 drinks for women and ≥4 drinks for men, as well as ≥ 4 drinks for women and ≥5 drinks for men) and cannabis use in the prior 30 days were the primary outcomes. Questions from the Addiction Severity Index (McLellan et al., 1992) were used to measure days of alcohol and drug related problems in the 30 days prior to each interview (baseline, 3 and 6 months): “How many days in the past 30 days have you experienced alcohol problems (for example, cravings or strong urges to drink, withdrawal or sickness, arguments, poor work performance)?” and “How many days in the past 30 days have you experienced problems with drugs other than alcohol?” The alcohol readiness ruler and cannabis readiness ruler are 10-point scales developed in prior MI studies to measure readiness to change. The scales asks how ready respondents are to cut down or stop use, ranging from 1 (not ready) to 10 (very ready) (Heather, Smailes, & Cassidy, 2008). Alcohol and drug dependence questions at baseline were based on the DSM-IV (American Psychiatric Association, 2000).
The Patient Health Questionnaire (PHQ-9) is a 9-item multiple-choice questionnaire based on DSM depression criteria asking patients about symptoms of depression in the prior two weeks (Kroenke et al., 2001). Possible scores range from 0 to 27. A score of 5 or higher indicates mild or greater depression.
Components of usual care were measured for use as covariates. Data were drawn from computerized administrative records (number of psychiatry department visits and initiation of specialty substance use services between study intake and 6 month follow up) and self-report interviews at 6 months (antidepressant medication utilization, based on response to the question, “During the past 3 months, were you prescribed or did you use prescribed medication for depression?”).
Procedures
Study procedures were approved by the University of California, San Francisco (UCSF) Committee on Human Subjects and Kaiser Permanente Institutional Review Board. Participants were identified via provider referrals and self-referral in response to flyers in clinic waiting area and in patient intake packets. Flyers indicated that the study was seeking individuals with depression or recent low mood who also consumed alcohol or other substances, and that a desire to cut back on substance use was not a requirement to participate. Study clinicians telephoned all potentially interested patients and determined eligibility based on alcohol and drug use patterns and PHQ-9 depression score. Because the PHQ-9 includes a question on suicidal ideation, to meet human subjects requirements to assess patient safety if needed, telephone recruitment was conducted by study clinicians (licensed psychologists, described below). Participants were offered $50 gift cards for the baseline, 3-month and 6-month interviews. At the conclusion of the phone call, an in-person appointment was scheduled.
At the in-person appointment, which took place in the same psychiatry building in which patients received their usual care, a study clinician or a research assistant further explained the study, and written informed consent was obtained. Enrolled participants then used laptop computers to complete baseline measures. The baseline measures used a simple interface on the laptop, and a study clinician or a research assistant was present and available to answer any questions participants had about the items or use of the computer, as needed. Standard randomization procedures used in psychotherapy studies were followed (Hulley et al., 2001), using a variable block size with a 1:1 allocation to the treatment or control condition. An additional research assistant who had no other involvement with the study used a web-based randomization tool to generate group assignments and placed individual assignments into sealed security envelopes given to the enrolling study clinician or research assistant, who was directed to open the envelopes in sequence as participants were enrolled.
The MI intervention consisted of one 45-minute in-person MI session followed by two 15-minute telephone “booster” sessions, similar to the format used in prior MI alcohol studies (Fleming et al., 2010; Satre et al., 2013). The treatment guidelines were based on Motivational Interviewing by Miller and Rollnick (Miller & Rollnick, 2012). MI is a short-term, directive, patient-centered style of counseling to help explore and resolve ambivalence. Active components include listening empathically and evoking patients’ individual reasons for changing their behavior. The therapist's approach is one of non-judgmental guidance, helping the patient move to a higher degree of readiness to change. Within a standardized protocol, the MI model allowed for flexibility in tailoring the intervention to individual patients. The therapist encouraged patients to minimize use of alcohol, illegal drugs, and misuse of prescription drugs, depending on which were reported at baseline. The intervention incorporated information about substance use risks for people in treatment for depression and other problems (e.g., alcohol/medication interactions and the potential for alcohol and drug use to interfere with depression treatment), provided in a collaborative manner consistent with MI (see Table 1). Intervention sessions were delivered within 6 weeks of enrollment.
Table 1.
Motivational Interviewing Intervention for Patients with Depression and Hazardous Drinking or Drug Use
| Format |
| 45-minute in-person session, as soon as possible after study enrollment |
| 20-minute phone “booster” session, approximately 10 days after in-person MI session |
|
20-minute phone “booster” session, approximately 14 days after initial booster |
| MI approach |
| Evocative, exploring patient's own reasons for change; empathic and nonjudgmental |
| Collaborative, meeting patients at their current level of motivation/phase of change |
|
Directive, gently guiding the patient in discussion of alcohol and drug use |
| Key MI strategies, adapted for patients with depression |
| Open-ended questions to evoke patients’ goals and values, particularly related to mood and other depression symptoms |
| Reflective listening, strategically emphasizing “change talk” such as patient-generated reasons to decrease drinking and other drug use |
| Summarizing, e.g., reviewing pros and cons of patient's current drinking and drug use patterns |
| Developing discrepancy between goals/values and current behaviors, especially potential discrepancies between current use patterns and goals such as improved energy and functioning |
| Rolling with resistance, acknowledging positive aspects of substance use, such as temporarily heightened mood or forgetting of problems |
| Supporting self-efficacy, noting patient's efforts and successes such as mental health treatment-seeking and medication adherence |
| Offering information about substance use and depression, e.g., impact on symptoms and medication effectiveness – in an MI-consistent manner (ask what patient already knows, ask permission to give additional information, tell brief information, ask for patient's thoughts/feelings in response to this new information) |
Control group participants were given 2-page brochures on substance use and risks specific to the substances they reported, consistent with prior MI studies (Dunn, Deroo, & Rivara, 2001; Satre et al., 2013). These brochures were produced by NIH and the National Office of National Drug Control Policy as part of their Fast Facts series, and included information on drug use risks and alcohol interactions with medications, including antidepressants (National Institute on Alcohol Abuse and Alcoholism, 2003; U.S. Department of Justice, 2003). Brochures were selected as the control condition in order to give patients some access to information regarding substance use, but not an experience of the specific MI treatment. All control participants received at least one brochure, and the brochures were provided immediately following completion of the baseline survey.
The study clinicians delivering the intervention were two licensed clinical psychologists experienced in substance use counseling who were not involved in usual patient care. These therapists participated in approximately 15 hours of instruction, and received supervised practice of 3 training patients in MI and study procedures, as in prior clinical trials (Dunn et al., 2001). Components included reading about the MI model, practice role-plays with feedback, and audiotaped practice sessions (Miller & Moyers, 2006).
Fidelity monitoring was conducted using the Motivational Interviewing Treatment Integrity code (MITI 3.1)(Moyers, Martin, Manuel, Miller, & Ernst, 2010). A sub-sample of 32 randomly chosen MI sessions was coded by an experienced MI trainer on the study team, using 20-minute recorded segments of each session. Of those assigned to the MI condition, 135 (88%) received all three sessions, 6 (4%) received in-person MI plus one booster (no 2nd booster), 6 (4%) received in-person MI only (no boosters), and 6 (4%) received no intervention.
Research assistants contacted participants by telephone 3 and 6 months after enrollment for a 30-minute interview. Patient reporting via telephone follow-up has been reliable in substance use studies (B. B. Cohen & Vinson, 1995). The research assistants were blinded to participants’ treatment condition.
Analyses
We examined comparability of the intervention and control groups on demographic characteristics, depression symptoms (PHQ-9), and baseline substance use and readiness to change alcohol and cannabis use, using t-tests and Pearson's chi-square test at baseline. We also compared the two groups at 6 months on measures of usual care services received (e.g., number of psychiatry clinic visits, any antidepressant use, and any alcohol or drug treatment received apart from the study). We calculated mean scores on the MITI subscales to determine results of fidelity monitoring in the MI intervention sample.
We used t-tests and Pearson's chi-square test to examine group differences in hazardous drinking, cannabis and depression outcomes by treatment group at 3 and 6 months and calculated effect sizes using Cohen's h for proportions and d for means (J. Cohen, 1988). We also tested a model of mediational effects to see if the assignment to treatment condition resulted in a change in hazardous drinking or cannabis use at the 3-month assessment which, in turn, might lead to a change in PHQ-9 scores at the 6-month assessment.
Multivariate logistic regression was used to examine predictors of hazardous drinking or cannabis use in the entire sample at 6 months, including study condition and factors based on the literature associated with better outcomes: older age, female gender, and baseline depression (Grothues et al., 2005; Satre et al., 2011; Wells-Parker et al., 2006). Control variables included baseline hazardous drinking or cannabis use frequency, readiness to reduce drinking or cannabis use, number of psychiatry visits, any CD department visits between baseline and 6 months and any antidepressant use at 6 months. Models for cannabis and hazardous drinking were run separately, and all predictors were entered simultaneously. Statistical analyses were conducted using SAS v9.3.
Results
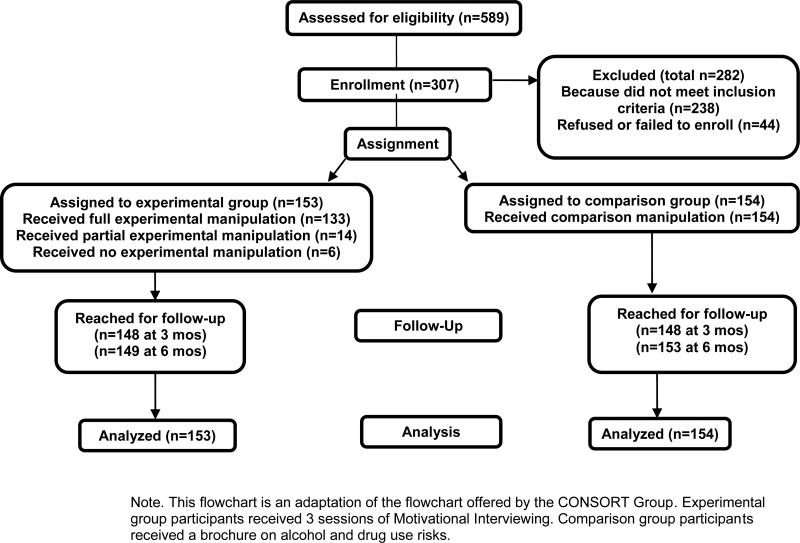
During the 24-month study intake window, 589 patients were contacted by phone for recruitment to the study. Of these, 238 did not meet study inclusion criteria: 175 (74%) based on lower than required substance use, 33 (14%) based on depression score, 19 (8%) based on manic or psychotic symptoms, and 11 (5%) for other reasons (e.g., they were already enrolled in specialty substance use treatment or had recently moved out of the area). Forty-four met criteria but either declined to participate or did not show up at the in-person enrollment appointment. Of the 307 enrolled participants, 296 (96%) completed the 3-month telephone follow up and 302 (98%) completed the 6-month follow up (Figure 1).
Figure 1.
Flow of Participants (Motivational Interviewing and Control Groups)
The sample ranged in age from 18 to 81, with a mean age of 37.0 (sd=13.0) and was 70.4% female. Mean PHQ-9 score was 14.0 (sd=5.6), a level consistent with moderate depression (Kroenke et al., 2001). Alcohol and cannabis use were most frequently reported, at 92.2% and 40.1%, respectively; 11.1% met criteria for alcohol dependence, and 12.0% met criteria for cannabis dependence, with no differences by study group. Other substances used in the prior 30 days reported at baseline included cocaine (1.6%), amphetamines (2.3%), hallucinogens/MDMA (3.9%), sedative misuse (5.2%) and opioid misuse (6.5%) (not shown). The control group had more Hispanic participants than the MI group, and the MI group had more African Americans; and readiness to reduce drinking was higher in the MI group (Table 2).
Table 2.
Characteristics of Adults with Depression Recruited to Motivational Interviewing (MI) Study to Reduce Hazardous Drinking and Drug Use (N=307)
| MI Intervention | Control | ||||
|---|---|---|---|---|---|
| N | % | N | % | X2 | |
| Total Study Group | 153 | 154 | |||
| Gender (% female) | 109 | 71.2 | 107 | 69.5 | 0.1 |
| Hispanic | 33 | 21.6 | 50 | 32.5 | 7.2* |
| Race/Ethnicity | 11.3* | ||||
| White | 56 | 36.6 | 61 | 39.6 | |
| Black | 41 | 26.8 | 24 | 15.6 | |
| Asian American | 23 | 15.0 | 20 | 13.0 | |
| Mixed/Other | 8 | 5.2 | 7 | 4.6 | |
| Marital status | 0.9 | ||||
| Married or partnered | 54 | 41.8 | 65 | 42.2 | |
| Separated or divorced | 32 | 20.9 | 26 | 16.9 | |
| Never married | 57 | 37.3 | 63 | 40.9 | |
| Highest educational degree | 0.3 | ||||
| Less than high school | 13 | 8.5 | 14 | 9.1 | |
| High school/GED | 46 | 30.1 | 49 | 31.8 | |
| Some college/AA | 37 | 24.2 | 40 | 26.0 | |
| BA or higher | 57 | 37.3 | 51 | 33.1 | |
| Employment status | 1.0 | ||||
| Employed | 105 | 68.6 | 99 | 64.3 | |
| Student/retired/homemaker | 19 | 12.4 | 25 | 16.2 | |
| Unemployed/disabled | 29 | 19.0 | 30 | 19.5 | |
| MI Intervention | Control | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t (df) | |
| Age | 37.6 | 13.4 | 36.8 | 13.0 | 0.5 (305) |
| Readiness to reduce drinking | 5.8 | 3.0 | 5.0 | 2.9 | 2.1 (281)* |
| Readiness to reduce cannabis | 5.4 | 2.9 | 5.1 | 2.9 | 0.68 (127) |
Notes: Readiness to reduce drinking and cannabis was measured at baseline. Significance of group differences was tested using chi-square and t-tests.
p < .05.
To measure MI fidelity, mean MITI scores were obtained for evocation (4.7 (sd=0.64)), collaboration (4.8 (sd=0.51)), autonomy/support (4.9 (sd=0.51)), direction (4.6 (sd=0.61)) and empathy (4.9 (SD=0.18)); reflection to question ratio (2.3 (sd=1.05)), percent open-ended questions (84.7 (sd=12.78)), percent complex reflections (63.7 (sd=12.78)), and percent MI adherent (100%). These scores are above competence level on each dimension and are indicative of a high degree of MI fidelity.
In usual care at 6 months, 48.3% of intervention participants and 60.1% of control participants reported antidepressant use, X2 (N=291) = 4.1, 1 df, p = .042. There were no differences between groups in number of usual care psychiatry clinic visits (mean = 5.3 (SD=8.1) or rate of chemical dependency treatment initiation (6.9% had one or more visits) between intake and 6 month follow up (not shown).
Rates of 30-day hazardous drinking, cannabis use and PHQ-9 depression scores were similar at baseline and decreased over time in both groups (Table 3). At 6 months, the MI group was less likely to report any cannabis use, X2 (N=291) = 4.4, 1 df, p = .037 and marginally less likely to report any hazardous drinking at the ≥4/≥5 level, X2 (N=291) = 3.5, 1 df, p = .060 (Table 3). Effect sizes in the differences between the two study groups were calculated for hazardous drinking, cannabis use and depression at 3 and 6 months (Table 3). The largest effect sizes were for cannabis use at 6 months (h = .23, 95% CI=.05-.24) and for hazardous drinking at the ≥4/≥5 level at 6 months (h = .21, 95% CI=.05-.22).
Table 3.
Motivational Interviewing (MI) Versus Control Group Outcomes Among Adults in Treatment with Depression Who Report Hazardous Drinking or Drug Use (N = 307)
| MI Intervention | Control | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | X2 | Effect size h (CI) | |
| Total Study Group | 153 | 154 | ||||
| Any ≥3/≥4 drinking days | ||||||
| Baseline | 127 | 83.0 | 123 | 79.9 | 0.5 | - |
| 3 Months | 81 | 55.5 | 82 | 56.2 | 0.0 | .08 (.06-.21) |
| 6 Months | 69 | 48.3 | 82 | 55.4 | 1.5 | .14 (.06-.19) |
| Any ≥4/≥5 drinking days | ||||||
| Baseline | 90 | 58.8 | 91 | 59.1 | 0.0 | - |
| 3 Months | 51 | 34.9 | 60 | 41.1 | 1.2 | .14 (.06-.18) |
| 6 Months | 42 | 29.4 | 59 | 39.9 | 3.5† | .21 (.05-.22) |
| Any cannabis use | ||||||
| Baseline | 60 | 39.2 | 65 | 42.2 | 0.3 | - |
| 3 Months | 43 | 29.5 | 52 | 35.6 | 1.3 | .12 (.06-.18) |
| 6 Months | 36 | 25.2 | 54 | 36.5 | 4.4* | .23 (.05-.24) |
| Mean | SD | Mean | SD | t (df) | Effect size d (CI) | |
|---|---|---|---|---|---|---|
| PHQ-9 Depression score | ||||||
| Baseline | 14.1 | 5.3 | 13.7 | 5.8 | 0.5 (305) | - |
| 3 Months | 8.4 | 5.5 | 8.6 | 5.0 | 0.3 (290) | .06 (−.19-.27) |
| 6 Months | 8.0 | 5.2 | 8.4 | 5.5 | 0.7 (289) | .08 (−.16-.31) |
Notes: Baseline, 3- and 6- month questions refer to alcohol and drug consumption in the previous 30 days. Hazardous drinking was measured two ways: any days of ≥3 drinks per day for women/≥4 drinks per day for men in the prior 30 days (study eligibility definition), and any ≥4 drinks per day for women and ≥5 drinks per day for men in the prior 30 days (a more widely used definition for alcohol problem screening). Significance of intervention and control group differences was tested using chi-square and t-tests.
p < .05
p < .10.
Mean number of days of alcohol problems were 3.0 (SD=5.9) at baseline, 2.4 (SD=6.8) at 3 months, and 1.4 (SD=4.7) at 6 months, and mean number of days of drug problems were 1.6 (SD=5.1) at baseline, 0.7 (SD=3.5) at 3 months, and 1.3 (SD=5.4) at 6 months, with no difference between treatment groups (not shown). We conducted mediational models of hazardous drinking and cannabis use reduction and changes in depression over time, using Baron and Kenny's mediator criteria and the less restrictive criteria suggested by Zhao (Zhao, Lynch, & Chen, 2010). Neither approach found evidence that hazardous drinking or cannabis use had a mediator effect (not shown).
Using logistic regression we tested candidate predictors of participants’ reporting hazardous drinking (≥4 drinks for women or ≥5 for men) or cannabis use in the 30 days preceding 6-month follow up. In the hazardous drinking model, baseline hazardous drinking frequency was significant. In the model predicting cannabis use at 6 months, significant factors included being in the control vs. MI treatment arm, older age, baseline depression severity, baseline frequency of cannabis use, readiness to reduce cannabis use, and use of antidepressant medications (Table 4).
Table 4.
Predictors of Prior 30-Day Hazardous Drinking and Cannabis Use at 6 Months Among Patients in Treatment for Depression.
| OR | 95% CI | p | |
|---|---|---|---|
| Hazardous Drinking | |||
| Treatment condition (MI intervention) | 0.72 | (0.41, 1.24) | .128 |
| Age in years | 0.98 | (0.96, 1.00) | .061 |
| Gender (female) | 0.77 | (0.42, 1.42) | .407 |
| Baseline PHQ-9 depression score | 0.97 | (0.92, 1.02) | .272 |
| Baseline ≥4/≥5 drinking frequency | 1.13 | (1.07, 1.19) | .001 |
| Baseline readiness to reduce drinking | 0.92 | (0.84, 1.02) | .101 |
| Any substance use treatment | 0.78 | (0.237, 2.57) | .684 |
| Any antidepressant use | 1.22 | (0.67, 2.21) | .521 |
| Number of psychiatry visits | 0.99 | (0.95, 1.03) | .622 |
| Cannabis Use | |||
| Treatment condition (MI intervention) | 0.29 | (0.11, 0.79) | .016 |
| Age in years | 0.95 | (0.91, 0.99) | .020 |
| Gender (female) | 2.34 | (0.82, 6.67) | .113 |
| Baseline PHQ-9 depression score | 1.10 | (1.01, 1.20) | .038 |
| Baseline cannabis use frequency | 1.07 | (1.02, 1.13) | .008 |
| Baseline readiness to reduce cannabis | 0.74 | (0.62, 0.88) | .001 |
| Any substance use treatment | 0.07 | (0.01, 1.17) | .064 |
| Any antidepressant use | 3.20 | (1.04, 9.54) | .042 |
| Number of psychiatry visits | 0.95 | (0.87, 1.03) | .232 |
Notes. Analyses used logistic regression. N= 269 for hazardous drinking and N = 121 for cannabis use samples. Hazardous drinking = any days of ≥4 drinks (for women) or ≥5 drinks (for men) in the prior 30 days, measured at 6 months. MI = Motivational interviewing. OR= odds ratio. 95% CI = 95% confidence interval. Specialty care substance use treatment (yes/no), antidepressant use (yes/no) and number of psychiatry visits since study enrollment were measured at 6-month follow up.
Discussion
This randomized controlled trial compared a 3-session MI intervention to a control group condition consisting of an educational brochure to reduce hazardous drinking and drug use among patients receiving treatment for depression. Both groups completed follow-up telephone interviews at 3 and 6 months. Although effect sizes were relatively small, results indicated that MI had an impact on cannabis use and hazardous drinking at 6 months.
In considering the clinical implications of these findings, it also should be noted that both the intervention group and control groups showed decreases in substance use, especially in hazardous drinking. This suggests that hazardous drinking may be easier to reduce than cannabis use via brief interventions, as noted in prior work among patients with depression (Baker, Turner, Kay-Lambkin, & Lewin, 2009). In both hazardous drinking and cannabis use outcomes, effect sizes were relatively small. This raises the question of what the added value of MI would be in a clinical context over and above a brief literature-based intervention, especially in light of the training required to deliver high-quality MI (Hall, Staiger, Simpson, Best, & Lubman, 2015). Before broad clinical recommendations are proposed, further work could explore which patients with depression would be adequately served by a briefer intervention (e.g., hazardous drinkers) and which would benefit most from the more extensive MI intervention (e.g., cannabis users or hazardous drinkers who do not respond to an initial brief intervention), in order to develop a stepped-care approach.
Findings contribute to the limited literature on MI in psychiatric populations and highlight the potential usefulness of this model among patients with depression. Previously, a study by Baker and colleagues of inpatients with substance abuse or dependence that randomized participants to a single motivational interview or a self-help booklet (Baker et al., 2002) found a modest short-term effect on alcohol and other drug use, but cannabis use remained high at 12 months. Martino and colleagues (Martino et al., 2006) compared two sessions of MI adapted for dual diagnosis to two sessions of a control condition psychiatric interview in patients with psychosis and drug use disorders. Results found no difference between the two conditions on substance use. In an alternative approach, there is some evidence that MI may effectively be combined with cognitive behavioral therapy to address both drinking and depression symptoms (Baker et al., 2014). In relation to pilot study findings that used a similar intervention approach (Satre et al., 2013), current results support the efficacy of MI on cannabis use and potentially on hazardous drinking.
These findings have implications for development of appropriate substance use interventions, which are integral to the delivery of effective psychiatric services. Although substance use treatment is most successful at early stages, many people do not seek treatment until their condition is severe (Babor et al., 2007). Those with potential substance-related problems often first seek mental health treatment (Edlund, Booth, & Han, 2012; Weisner & Matzger, 2003). Yet providers often fail to address hazardous drinking or drug use reduction (Institute of Medicine, 2006; Satre, Leibowitz, Mertens, & Weisner, 2014). This results in a missed opportunity for both substance use and depression treatment that MI could help to address. Given that both study conditions showed improvement over time, substance use interventions even briefer than MI, (e.g., brief feedback on drug and alcohol use risks combined with follow-up screening), could also be explored.
Findings are especially timely given the limited evidence base on MI for cannabis use (McCambridge, Slym, & Strang, 2008) and a large recent study showing that at six months, brief interventions including MI were not effective in reducing drug use among primary care patients (Saitz et al., 2014). In contrast, our results indicate that MI may reduce cannabis use in mental health service settings such as psychiatry. In addition, regression model findings indicate that MI had an independent effect on cannabis use reduction apart from other services participants received, highlighting the potential usefulness of MI as a supplement to usual care models in this population.
The multivariate model also identified characteristics of participants likely to continue substance use over time, such as those with greater baseline hazardous drinking and cannabis use frequency. Among cannabis users seeking mental health care, younger adults and those with greater depression severity potentially may benefit from more intensive or tailored interventions to address co-occurring mood and substance use problems.
Study Limitations and Strengths
The study clinic pre-screened patients with serious alcohol or drug problems and referred them to specialty substance use treatment within the health care system, and the intervention was not designed to address dependence. Yet these constraints may be similar in many settings, including primary care and outpatient mental health-focused clinics in which patients with depression often present with co-occurring substance use. It is possible that greater self-reported readiness to reduce alcohol use in the MI arm at baseline could have impacted hazardous drinking group differences at follow-up. Future studies should measure in greater detail the potential impact of usual care (e.g., specific medications prescribed, advice from usual care mental health providers to reduce alcohol and drug use). A further limitation is the use of a study team member (a psychologist other than the interventionists) to monitor MI fidelity rather than an independent rater outside the team.
The study also had a number of strengths. This was a well-controlled study with a high rate of enrollment and very high follow-up rates. The study was conducted in an outpatient depression treatment clinic, and the intervention was monitored for MI fidelity. Basing the study in an integrated health care system enhanced our ability to measure other components of care such as psychiatry and chemical dependency clinic visits. MI intervention delivery resulted in minimal logistical complications, suggesting that a supplemental intervention could be integrated into outpatient mental health treatment settings if efficacy is established.
Conclusions
This study examined the efficacy of MI among patients with depression as an adjunct to usual care in an outpatient psychiatry clinic, compared with a brief literature-based intervention on alcohol and drug use risks. Comparison of substance use outcomes in the two study conditions at six months provided evidence for an impact of MI on cannabis use and potentially on hazardous drinking, although effect sizes were small. Both the MI intervention and brief literature-based approaches resulted in reduction in substance use over time, especially alcohol, and could potentially be useful in addressing the adverse impact of substance use among patients with depression.
Public health significance.
Hazardous drinking and drug use are common among patients with depression. Results of this study indicate that motivational interviewing is a promising treatment approach to assist these patients.
Acknowledgments
We thank [blinded] for assistance in conducting the study and [blinded] for assistance in preparing the manuscript.
NIH Grant Funding: R01AA020463
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text rev. ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- American Psychiatric Association Practice guideline for the treatment of patients with Major Depressive Disorders. 2010 Retrieved from http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf.
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Baker A, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, McElduff P. Randomized controlled trial of MICBT for co-existing alcohol misuse and depression: outcomes to 36-months. Journal of Substance Abuse Treatment. 2014;46(3):281–290. doi: 10.1016/j.jsat.2013.10.001. doi: 10.1016/j.jsat.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, Terry M. Evaluation of a motivational interview for substance use within psychiatric in-patient services. Addiction. 2002;97(10):1329–1337. doi: 10.1046/j.1360-0443.2002.00178.x. doi: 10.1046/j.1360-0443.2002.00178.x. [DOI] [PubMed] [Google Scholar]
- Baker A, Turner A, Kay-Lambkin FJ, Lewin TJ. The long and the short of treatments for alcohol or cannabis misuse among people with severe mental disorders. Addictive Behaviors. 2009;34(10):852–858. doi: 10.1016/j.addbeh.2009.02.002. doi: 10.1016/j.addbeh.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Bricker JB, Russo J, Stein MB, Sherbourne C, Craske M, Schraufnagel TJ, Roy-Byrne P. Does occasional cannabis use impact anxiety and depression treatment outcomes? Results from a randomized effectiveness trial. Depression and Anxiety. 2007;24(6):392–398. doi: 10.1002/da.20248. doi: 10.1002/da.20248. [DOI] [PubMed] [Google Scholar]
- Castaneda R, Sussman N, Levy R, O'Malley M, Westreich L. A review of the effects of moderate alcohol intake on psychiatric and sleep disorders. Recent Developments in Alcoholism. 1998;14:197–226. doi: 10.1007/0-306-47148-5_9. [DOI] [PubMed] [Google Scholar]
- Cohen BB, Vinson DC. Retrospective self-report of alcohol consumption: Test-retest reliability by telephone. Alcoholism: Clinical and Experimental Research. 1995;19(5):1156–1161. doi: 10.1111/j.1530-0277.1995.tb01595.x. doi: 10.1111/j.1530-0277.1995.tb01595.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Davis LL, Rush JA, Wisniewski SR, Rice K, Cassano P, Jewell ME, McGrath PJ. Substance use disorder comorbidity in major depressive disorder: an exploratory analysis of the Sequenced Treatment Alternatives to Relieve Depression cohort. Comprehensive Psychiatry. 2005;46(2):81–89. doi: 10.1016/j.comppsych.2004.07.025. doi: 10.1016/j.comppsych.2004.07.025. [DOI] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. American Journal of Psychiatry. 2000;157(5):751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs. 2012;73(4):635–646. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming MF, Balousek SL, Grossberg PM, Mundt MP, Brown D, Wiegel JR, Saewyc EM. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. Journal of Studies on Alcohol and Drugs. 2010;71(1):23–31. doi: 10.15288/jsad.2010.71.23. doi: 10.15288/jsad.2010.71.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grothues JM, Bischof G, Reinhardt S, Hapke U, Meyer C, John U, Rumpf HJ. Intention to change drinking behaviour in general practice patients with problematic drinking and comorbid depression or anxiety. Alcohol and Alcoholism. 2005;40(5):394–400. doi: 10.1093/alcalc/agh182. doi: 10.1093/alcalc/agh182. [DOI] [PubMed] [Google Scholar]
- Grothues JM, Bischof G, Reinhardt S, Meyer C, John U, Rumpf HJ. Effectiveness of brief alcohol interventions for general practice patients with problematic drinking behavior and comorbid anxiety or depressive disorders. Drug and Alcohol Dependence. 2008;94(1-3):214–220. doi: 10.1016/j.drugalcdep.2007.11.015. doi: 10.1016/j.drugalcdep.2007.11.015. [DOI] [PubMed] [Google Scholar]
- Hall K, Staiger PK, Simpson A, Best D, Lubman DI. After 30 years of dissemination, have we achieved sustained practice change in motivational interviewing? Addiction. 2015 doi: 10.1111/add.13014. doi: 10.1111/add.13014. [DOI] [PubMed] [Google Scholar]
- Heather N, Smailes D, Cassidy P. Development of a Readiness Ruler for use with alcohol brief interventions. Drug and Alcohol Dependence. 2008;98(3):235–240. doi: 10.1016/j.drugalcdep.2008.06.005. doi: 10.1016/j.drugalcdep.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Hulley SB, Newman TB, Cummings SR, Hearst N, Grady D, Browner WS. Designing clinical research: an epidemiologic approach. 2nd ed. Lippincott Williams & Wilkins; New York: 2001. [Google Scholar]
- Institute of Medicine . Improving the quality of health care for mental and substance-use conditions. National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- Kaiser Permanente Care Management Institute Diagnosis and treatment of depression in adults: 2012 clinical practice guideline. 2006 Retrieved from http://www.guideline.gov/content.aspx?id=39432.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo PH, Gardner CO, Kendler KS, Prescott CA. The temporal relationship of the onsets of alcohol dependence and major depression: using a genetically informative study design. Psychological Medicine. 2006;36(8):1153–1162. doi: 10.1017/S0033291706007860. doi: 10.1017/S0033291706007860. [DOI] [PubMed] [Google Scholar]
- Martino S, Carroll KM, Nich C, Rounsaville BJ. A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction. 2006;101(10):1479–1492. doi: 10.1111/j.1360-0443.2006.01554.x. doi: 10.1111/j.1360-0443.2006.01554.x. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Slym RL, Strang J. Randomized controlled trial of motivational interviewing compared with drug information and advice for early intervention among young cannabis users. Addiction. 2008;103(11):1809–1818. doi: 10.1111/j.1360-0443.2008.02331.x. doi: 10.1111/j.1360-0443.2008.02331.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Argeriou M. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Miller WR, Moyers TB. Eight stages in learning motivational interviewing. Journal of Teaching in the Addictions. 2006;5(1):3–18. doi: 10.1300/J188v05n01_02. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. Guilford Press; New York: 2012. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised global scales: motivational interviewing treatment integrity 3.1.1 (MITI 3.1.1) 2010 Retrieved from http://casaa.unm.edu/download/miti3_1.pdf.
- National Institute on Alcohol Abuse and Alcoholism Harmful interactions: mixing alcohol with medicines. 2003 revised 2014. Retrieved from http://pubs.niaaa.nih.gov/publications/Medicine/Harmful_Interactions.pdf.
- Roeloffs CA, Fink A, Unutzer J, Tang L, Wells KB. Problematic substance use, depressive symptoms, and gender in primary care. Psychiatric Services. 2001;52(9):1251–1253. doi: 10.1176/appi.ps.52.9.1251. doi: 10.1176/appi.ps.52.9.1251. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Samet JH. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. Journal of the American Medical Association. 2014;312(5):502–513. doi: 10.1001/jama.2014.7862. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Eisendrath S, Weisner C. Subdiagnostic alcohol use by depressed men and women seeking outpatient psychiatric services: consumption patterns and motivation to reduce drinking. Alcoholism: Clinical and Experimental Research. 2011;35(4):695–702. doi: 10.1111/j.1530-0277.2010.01387.x. doi: 10.1111/j.1530-0277.2010.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Delucchi K, Lichtmacher J, Sterling SA, Weisner C. Motivational Interviewing to reduce hazardous drinking and drug use among depression patients. Journal of Substance Abuse Treatment. 2013;44(3):323–329. doi: 10.1016/j.jsat.2012.08.008. doi: 10.1016/j.jsat.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Leibowitz A, Mertens JR, Weisner C. Advising depression patients to reduce alcohol and drug use: factors associated with provider intervention in outpatient psychiatry. American Journal on Addictions. 2014;23(6):570–575. doi: 10.1111/j.1521-0391.2014.12140.x. doi: 10.1111/j.1521-0391.2014.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y. At high risk and want to quit: marijuana use among adults with depression or serious psychological distress. Addictive Behaviors. 2014;39(4):761–767. doi: 10.1016/j.addbeh.2013.12.013. doi: 10.1016/j.addbeh.2013.12.013. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Fiellin DA, O'Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. American Journal of Medicine. 2005;118(4):330–341. doi: 10.1016/j.amjmed.2005.01.007. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. Journal of Nervous and Mental Diseases. 1999;187(10):630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice Marijuana fast facts. Questions and answers. 2003 Retrieved from http://www.justice.gov/archive/ndic/pubs3/3593/3593p.pdf.
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Weisner C, Matzger H. Missed opportunities in screening for alcohol problems in medical and mental health services. Alcoholism: Clinical and Experimental Research. 2003;27(7):1132–1141. doi: 10.1097/01.ALC.0000075546.38349.69. doi: 10.1097/01.ALC.0000075546.38349.6. [DOI] [PubMed] [Google Scholar]
- Wells-Parker E, Dill P, Williams M, Stoduto G. Are depressed drinking/driving offenders more receptive to brief intervention? Addictive Behaviors. 2006;31(2):339–350. doi: 10.1016/j.addbeh.2005.05.011. doi: 10.1016/j.addbeh.2005.05.011. [DOI] [PubMed] [Google Scholar]
- Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, Rosenbaum JF. Consumption of alcohol, nicotine, and caffeine among depressed outpatients. Relationship with response to treatment. Psychosomatics. 1996;37(6):518–522. doi: 10.1016/S0033-3182(96)71515-3. doi: 10.1016/S0033-3182(96)71515-3. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JGJ, Chen Q. Reconsidering Baron and Kenny: myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. doi: 10.1086/651257. [Google Scholar]