Abstract
Objective
As empirical evidence for the effectiveness of LGB-affirmative psychotherapy emerges, the question of whether some clients may derive greater benefit than others becomes important. The current study investigated whether internalized homonegativity (IH), both explicit and implicit, moderated the efficacy of a cognitive–behavioral intervention designed to improve the mental and sexual health of young gay and bisexual men through facilitating minority stress coping.
Method
At baseline, young gay and bisexual men (n=54) experiencing symptoms of depression and anxiety completed measures of explicit and implicit IH. Participants also completed self-reports of mental health and an interviewer-based assessment of past-90-day risk behavior before and after treatment in a 10-session individual LGB-affirmative intervention.
Results
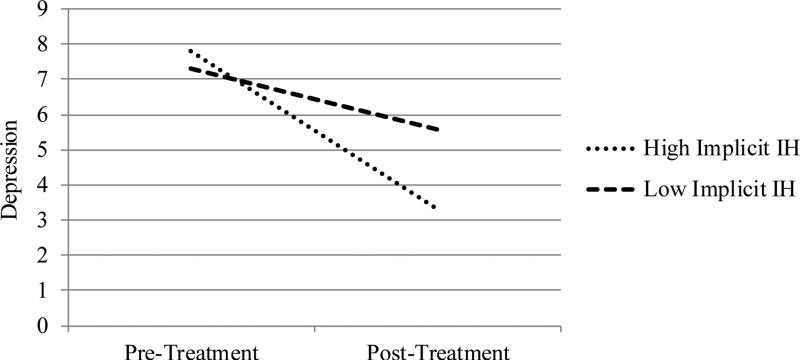
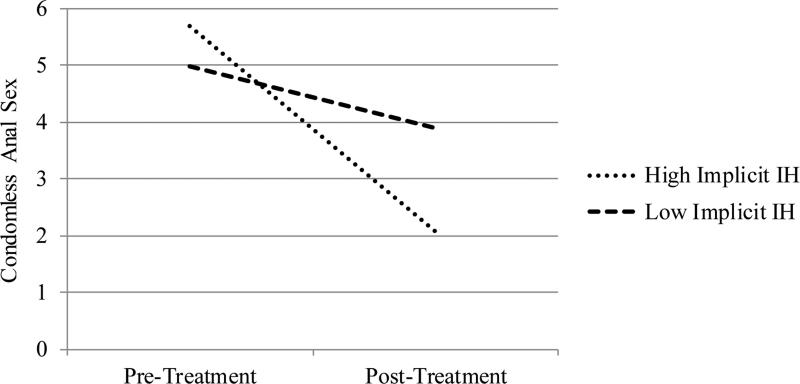
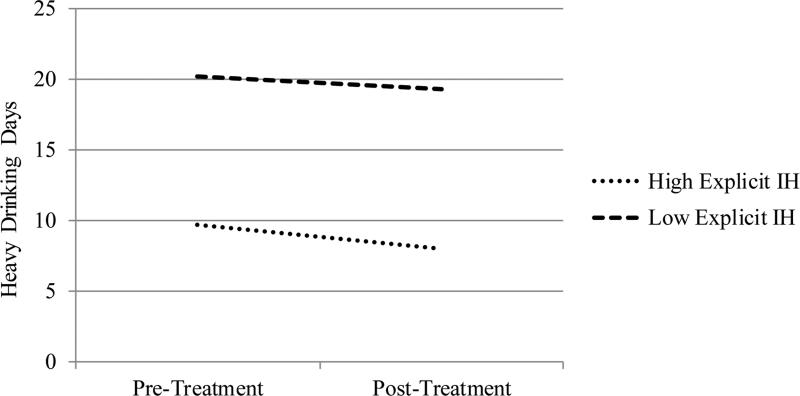
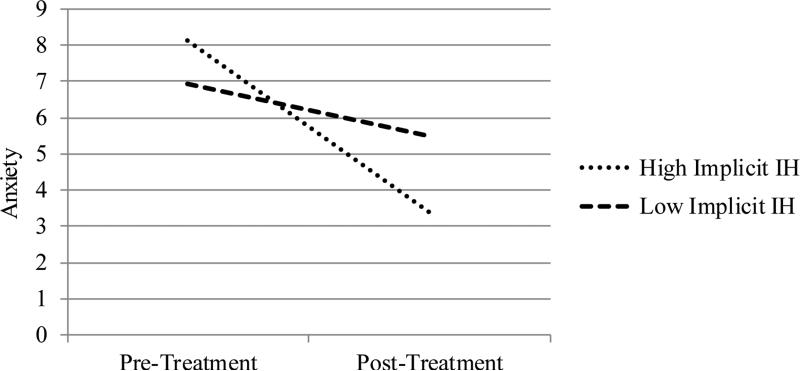
Moderation analyses showed that participants higher in implicit IH experienced greater reductions in depression (b=−2.99, p=.031, 95% CI: −5.69, −0.29), anxiety (b=−3.56, p=.014, 95% CI: −6.35, −0.76), and past-90-day condomless anal sex with casual partners (b=−1.29, p=.028, 95% CI: −2.44, −0.14). Participants higher in explicit IH experienced greater reductions in past-90-day heavy drinking (b=−0.42, p=.003, 95% CI: −0.69, −0.15).
Conclusions
These findings indicate that greater gains from LGB-affirmative psychotherapy were observed in gay and bisexual men who were higher in IH, particularly when measured implicitly. As the first study that examines factors that moderate the efficacy of LGB-affirmative psychotherapy, the present research has important implications for intervention development and highlights the value of incorporating implicit measures into clinical work.
Public Health Significance
Knowing what treatments work best for whom can guide the efficient dissemination of evidence-based treatments, an especially important goal given the move toward personalized medicine against a backdrop of constrained treatment resources. Gay and bisexual men with more negative biases against their sexual orientation might represent good candidates for LGB-affirmative mental and sexual health treatments. Implicit measurements of sensitive psychological processes like IH represent a promising direction for identifying suitable treatment candidates.
Keywords: minority stress, internalized homophobia, LGB-affirmative, Implicit Association Test (IAT), cognitive behavioral therapy (CBT)
Lesbian, gay, and bisexual (LGB) individuals experience disproportionately high rates of depression, anxiety, and substance use problems compared with heterosexual individuals (King et al., 2008), largely because of their exposure to sexual minority stressors—such as structural, social, and familial discrimination (Meyer, 2003). LGB-affirmative psychotherapy, which aims to facilitate the process of coping with stressors uniquely faced by sexual minorities, has been found efficacious in terms of its ability to reduce depression and anxiety symptoms as well as health risk behaviors such as substance use and risky sex (e.g., Pachankis, Hatzenbuehler, Rendina, Safren, & Parsons, 2015). However, given that not all LGB individuals experience their sexual identities in the same way and that minority stress might be a greater concern for some than for others (Pachankis & Goldfried, 2004), identifying individual differences that might moderate the efficacy of LGB-affirmative interventions represents an important area of inquiry.
Defined as the internalization of negative messages about homosexuality by LGB individuals, internalized homonegativity (IH) has been associated with depression, anxiety, and HIV risk behavior among gay and bisexual men (Meyer, 1995; Newcomb & Mustanski, 2010). These adverse consequences are further exacerbated by the fact that individuals higher in IH are less likely to be reached by health-promoting interventions designed for the general sexual minority community. As demonstrated by Huebner and colleagues (2002), gay and bisexual men who were higher in IH were less likely to be aware of the availability of HIV preventive community interventions and reported less behavioral change from such services.
While most of the research on IH has relied on self-report measures of the construct (i.e., explicit IH), recent research suggests that implicit measures, such as the Implicit Association Test (IAT), might better capture aspects of IH that the individual is not aware of or is unwilling to acknowledge (Hatzenbuehler, Dovidio, & Nolen-Hoeksema, 2009). Developed by Greenwald and colleagues (1998), the IAT has been found to be useful for capturing processes in socially sensitive domains, including biased associations towards one's own group. Of particular relevance to the present research, implicit IH, as assessed by a modified IAT, has been shown to uniquely predict involvement with the gay community (Jellison, McConnell, & Gabriel, 2004) and psychological distress in response to daily stigma experiences (Hatzenbuehler et al., 2009).
Given the important role of IH as a minority stress process, we examined whether IH, measured both implicitly (i.e., using an IAT) and explicitly (i.e., using traditional self-report), moderates the efficacy of a novel LGB-affirmative intervention. The ESTEEM (Effective Skills to Empower Effective Men) intervention is a 10-session, individually delivered cognitive behavioral treatment designed to reduce depression, anxiety, risky sexual behaviors, and substance use among gay and bisexual men by improving minority stress coping. Tested in a pilot randomized controlled trial, ESTEEM has demonstrated preliminary efficacy and represents a promising form of LGB-affirmative therapy that addresses sexual-orientation-based mental health disparities at their source in minority stress (Pachankis et al., 2015).
Because individuals higher in IH tend to experience more difficulties related to sexual identity development (Szymanski, Kashubeck-West, & Meyer., 2008), we proposed that they would therefore derive more benefit from ESTEEM, which provided a supportive, structured space for learning cognitive-behavioral skills for coping with stigma and developing a healthy sexual identity. Specifically, we hypothesized that participants with higher IH would experience greater reductions in depressive symptoms, anxiety, condomless sex, and alcohol use than those lower in IH. In light of evidence for the IAT's ability to capture self-stigmatizing processes better than explicit measures (Hatzenbuehler et al., 2009; Jellison et al., 2004), we also hypothesized that the moderating effect of implicit IH would be stronger than the moderating effect of explicit IH.
METHOD
Participants
Data were collected in 2013 and 2014 from New York City-based gay and bisexual men who were enrolled in a study to receive the ESTEEM intervention. Interested individuals completed a brief phone-screening questionnaire to assess whether they met eligibility criteria, which included: (1) identifying as a gay or bisexual man who was born male; (2) English fluency; (3) age 18 to 35; (4) New York City residence; (5) HIV-negative status; (6) engaging in HIV risk behavior (i.e., at least one instance of condomless anal sex with a casual male partner or with an HIV-positive or status-unknown main male partner); and (7) experiencing symptoms of depression and/or anxiety in the past 90 days, though not currently receiving mental health services more than once a month. Of the 63 participants who were enrolled into the study, the current analyses included the 54 men who completed both the pre- and post-treatment assessments (Table 1). Those excluded (n = 9) did not significantly differ from those included.
Table 1.
Demographics of total sample, N = 54
| Variable | n | % |
|---|---|---|
| Age, years | ||
| Mean | 26.1 | |
| SD | 4.0 | |
| Race | ||
| American Indian or Alaskan Native | 1 | 1.9 |
| Asian | 1 | 1.9 |
| Black / African American | 7 | 13.0 |
| Pacific Islander | 2 | 3.7 |
| White | 30 | 55.6 |
| Other/mixed | 13 | 24.1 |
| Hispanic / Latino | ||
| Yes | 22 | 40.7 |
| No | 32 | 59.3 |
| Sexual orientation | ||
| Gay/queer | 49 | 92.5 |
| Bisexual | 4 | 7.5 |
| Education | ||
| High school, GED, or less | 2 | 6.3 |
| Some college or Associates degree | 14 | 59.4 |
| Currently in college | 5 | 15.6 |
| 4-year college degree | 9 | 28.1 |
| Graduate school | 2 | 6.3 |
| Income | ||
| Less than $20,000 / year | 28 | 51.9 |
| $20,000 to $49,999 / year | 20 | 37 |
| More than $50,000 / year | 6 | 11.1 |
| Employment status | ||
| Full time | 16 | 30.2 |
| Part time | 18 | 34.0 |
| On disability | 2 | 3.8 |
| Student (unemployed) | 9 | 17.0 |
| Unemployed | 8 | 15.1 |
| Relationship status | ||
| Single | 44 | 83 |
| In a relationship | 9 | 17 |
Note: Some variables contain missing data. None of the variables were found to differ between the immediate and waitlist conditions.
Procedure
Upon completing the in-office portion of the baseline assessment and confirming eligibility, participants were randomized into one of two conditions: the immediate treatment condition, wherein participants began their ESTEEM treatment that day, or the waitlist condition, wherein participants began treatment three months later. Thus, while all participants received treatment, immediate treatment participants received treatment between the baseline and 3-month assessment and completed a follow-up assessment at six months; waitlist participants completed their pre-treatment assessment three months after their baseline assessment and then completed a post-intervention assessment after three months of treatment. In the current analyses, participants’ baseline assessment provided their implicit and explicit IH scores. For all participants, intervention impact was measured by comparing pre-treatment to post-treatment scores on outcome measures. Thus, 6-month follow-up assessments were not utilized here as only immediate participants completed this assessment.
The ESTEEM intervention consisted of 10 individually-delivered sessions. Based on the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (Barlow et al., 2010), it explores the impact of minority stress on participants’ mental health, interpersonal functioning, and substance use and sexual behavior, with the aim of improving minority stress coping through emotion regulation, cognitive restructuring, and assertiveness training. Three advanced clinical psychology doctoral students delivered the treatment, as supervised by the third author. Of the 54 participants, 35 (64.8%) completed at least half of the sessions, with 24 (44.4%) completing all 10 sessions, while 15 (27.8%) completed only one session. More detailed information on module content and treatment efficacy is described elsewhere (Pachankis et al., 2015). Research protocols were approved by the Human Subjects Committee of Yale University.
Measures
Implicit IH
A sexual minority adaptation of the IAT (Hatzenbuehler et al., 2009) measured participants’ implicit associations towards sexual minorities relative to heterosexuals. On an in-office computer, participants were instructed to categorize a series of images, as either gay or straight and pleasant or unpleasant, by pressing one of two keys. The pictures of four heterosexual couples and four same-sex couples (two male and two female couples) were matched with one of 16 words (eight positive words [e.g., lovely, joyful] and eight negative words [e.g., terrible, awful]). Participants completed three practice blocks and two critical blocks, each containing 72 trials. In one of the two critical blocks, participants were asked to identify positive words and images of same-sex couples using one key, and negative words and images of heterosexual couples using another key. In the other block, the matching of word valence and couple type was reversed, and their order counterbalanced. Differential response times and error rates are reflected in a D score calculated with the updated scoring algorithm (Greenwald, Nosek, & Banaji, 2003), with higher D scores indicating more negative associations for sexual minorities. In terms of screening, responses slower than 10000ms were excluded from analyses. No participants had more than 10% of trials faster than 300ms. The average error rate for the entire sample is 6.4%, and no participants were excluded for their rate of errors, as only four participants had a sitting in which errors exceeded 30%. Internal consistency was α = 0.54.
Explicit IH
The Internalized Homophobia Scale (IHS; Martin & Dean, 1992) assesses gay and bisexual men's self-reported distress in relation to their sexual minority identity over the past year. Nine items were rated on a 4-point scale, ranging from 1 (never) to 4 (often), with higher scores indicating greater explicit IH (α = 0.90).
Overall Depression Severity & Impairment Scale (ODSIS; Bentley, Gallagher, Carl, & Barlow, 2014)
The ODSIS contains five items assessing past-week severity of and impairment from depressive symptoms. All items are rated on a scale ranging from 0 to 4; each response option is labeled with item-specific qualitative anchors. For example, responses to the item “In the past week, how much has depression interfered with your social life and relationships?” range from 0 (None: My depression doesn't affect my relationships) to 4 (Extreme: My depression has completely disrupted my social activities. All of my relationships have suffered or ended. My family life is extremely strained) (α = 0.90).
Overall Anxiety Severity & Impairment Scale (OASIS; Norman, Cissell, Means-Christensen, & Stein, 2006)
The OASIS contains five items assessing past-week severity of and impairment from anxiety. Response options ranged from 0 to 4, with each item having a specific set of qualitative anchors. For example, for the item “In the past week, when you have felt anxious, how intense or severe was your anxiety?” response options range from 0 (Little or none: Anxiety was absent or barely noticeable), to 4 (Extreme: Anxiety was overwhelming. It was impossible to relax at all. Physical symptoms were unbearable) (α = 0.85).
90-day Time Line Follow Back (TLFB; Sobell & Sobell, 1992)
Past 90-day condomless anal sex with casual partners and heavy alcohol use were assessed utilizing the TLFB, during which a trained interviewer helps a participant to record recent risk events on a past-90-day calendar. The number of days for which heavy drinking (five or more drinks) was indicated constitutes the past-90-day heavy drinking variable, while the number of condomless anal sex acts with casual partners constitutes the past-90-day sexual risk variable.
Analytic plan
To measure changes in outcomes, we pooled pre-treatment measures from the baseline assessment for the immediate participants and the three-month assessment for the waitlist participants, and pooled post-treatment measures from the three-month assessment for the immediate participants and the six-month assessment for the waitlist participants. This pooled approach provided more power for testing interactions than treating each condition as separate. Before combining the two condition groups, t-tests and chi-square tests confirmed that the two groups did not differ on demographic variables. As scores on explicit IH were non-normally distributed, we used Spearman's rho to measure the correlation between implicit and explicit IH.
To test for changes in each of the continuous outcomes across time, and to detect whether baseline levels of IH interacted with time, we used linear mixed models with maximum likelihood estimation. For the two count variables (past-90-day heavy drinking and past-90-day number of condomless anal sex acts), we used generalized linear mixed models with negative binomial distributions and maximum likelihood estimation. Compound symmetry was used to model the covariance structure within participants. Sensitivity analyses confirmed that interactions for implicit IH and time did not differ when controlling for explicit IH, and that interactions for explicit IH and time did not differ when controlling for implicit IH. We therefore tested two separate models—one that included implicit IH and one that included explicit IH, and their respective interactions with time. Where significant, simple-slopes were calculated, with estimated means graphed at one SD above and below the mean of that predictor variable.
Results
Overall, depression (p < .001), anxiety (p < .001), and past-90-day condomless anal sex with casual partners (p = .025) showed significant reductions, whereas past-90-day heavy drinking (p = .095) showed marginally significant reductions, from pre- to post-treatment (Table 2). Baseline implicit and explicit IH were modestly correlated (Spearman's ρ = .31, p = .024). As hypothesized, baseline implicit IH interacted with time to predict reductions in depression (b = −2.99, p = .031, 95% CI: −5.69, −0.29), anxiety (b = −3.56, p = .014, 95% CI: −6.35, −0.76), and past-90-day condomless anal sex with casual partners (b = −1.29, p = .028, 95% CI: −2.44, −0.14). Those higher in implicit IH showed nearly three times greater reductions than those lower in implicit IH on depression (b = −4.50, p<.001, 95% CI: −6.29, −2.71, and b = −1.74, p = .048, 95% CI: −3.46, −0.01, respectively), anxiety (b = −4.74, p<.001, 95% CI: −6.59, −2.89, and b = −1.45, p = .11, 95% CI: −3.24, 0.34, respectively), and past-90-day condomless anal sex with casual partners (b = −1.29, p<.001, 95% CI: −2.05, −0.52, and b = 0.09, p = .80, 95% CI: −0.62, 0.81, respectively) (see Figures 1-3). At post-treatment, those higher in implicit IH showed reductions on depression and anxiety roughly equivalent to one standard deviation, and reported 3.6 fewer past-90-day condomless anal sex acts. In contrast, baseline explicit IH predicted reduction in past-90-day heavy drinking (b = −0.42, p = .003, 95% CI: −0.69, −0.15). Those higher in explicit IH showed nearly two times greater reduction in heavy drinking (1.7 fewer days, post-treatment; b = −0.55, p<.001, 95% CI:−0.84, −0.26) than those lower in explicit IH (b = −0.07, p = .63, 95% CI: −0.21, 0.34) (see Figure 4).
Table 2.
Implicit and explicit internalized homonegativity (IH) as predictors of mental and behavioral health outcomes (N = 54)
| Outcome Variable | Pre-treatment |
Post-treatment |
Interaction of Time with Implicit IH |
Interaction of Time with Explicit IH |
||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Est. | 95% CI | Est. | 95% CI | |
| Depression (ODSIS) | 7.46 | 4.30 | 4.37 | 4.54 | −2.99* | −5.69, −0.29 | −0.34 | −2.10, 1.42 |
| Anxiety (OASIS) | 7.50 | 3.76 | 4.41 | 4.15 | −3.56* | −6.35, −0.76 | −0.63 | −2.46, 1.20 |
| Condomless Anal Sex Acts with Casual Partners (past 90 days) | 5.91 | 8.93 | 3.09 | 5.90 | −1.29* | −2.44, −0.14 | −0.64 | −1.84, 0.56 |
| Days of Heavy Drinking (past 90 days) | 16.17 | 14.75 | 13.39 | 14.25 | −0.23 | −0.65, 0.19 | −0.42** | −0.69, −0.15 |
p ≤ .05
p ≤ .01
SE=Standard Deviation; Est.=Estimate; CI=Confidence Interval; OASIS=Overall Anxiety Severity and Impairment Scale; ODSIS=Overall Depression Severity and Impairment Scale.
Figure 1.
Treatment change in depression (ODSIS) for high and low implicit internalized homonegativity (IH)
Figure 3.
Treatment change in past-90-day condomless anal sex for high and low implicit internalized homonegativity (IH)
Figure 4.
Treatment change in past-90-day heavy drinking for high and low explicit internalized homonegativity (IH)
Discussion
The current study examined implicit and explicit IH as potential moderators of the efficacy of ESTEEM, an LGB-affirmative cognitive behavioral intervention designed to improve the mental and sexual health of gay and bisexual men by facilitating coping with minority stress. Implicit and explicit IH were not strongly correlated, confirming the utility of examining both measures of this construct. As expected, baseline implicit IH emerged as a stronger moderator of treatment change, predicting greater reductions in depression, anxiety, and past 90-day condomless anal sex with casual partners, among those higher in implicit IH. In contrast, baseline explicit IH only moderated treatment change in past 90-day heavy drinking, among those higher in explicit IH. These results suggest that the treatment's tailored emphasis on coping with minority stress and healthy sexual identity development was most appropriate for those who began treatment with more negative implicit associations regarding their sexual identity.
Previous research has shown that individuals with more IH are less likely to be reached by standard health promotion interventions (Huebner et al., 2002), making them particularly vulnerable to the health threats of minority stress. The present study complements this finding by suggesting that gay and bisexual men who scored higher in IH might be particularly responsive to LGB-affirmative therapy, potentially finding its focus on minority stress to be more helpful and relevant than would individuals lower in IH. Given the need for targeted treatments against a backdrop of constrained resources, our results provide initial support for considering IH as a useful predictor of clients’ suitability for LGB-affirmative therapy.
Furthermore, the present research highlights the potential utility of incorporating the IAT into clinical work with sexual minority individuals. Extending previous work (Hatzenbuehler et al., 2009; Jellison et al., 2004), we demonstrated that implicit IH was generally a stronger predictor of treatment change than explicit IH. The modest correlation between the implicit and explicit measures coheres with previous studies (Hofmann, Gawronski, Gschwendner, Le, & Schmitt, 2005; Hatzenbuehler et al., 2009). Given that little research has utilized the IAT to examine internalized stigma among sexual minorities, this study represents an important initial attempt to understand how it may be used to improve our ability to tailor mental health treatment to meet the needs of gay and bisexual men. Results also suggest that, in the absence of readily available implicit measures in clinical contexts, clinicians might pay particular attention to subtle behavioral (e.g., difficulties with male intimacy) and emotional (e.g., shameful self-schemas) indications of their clients’ IH to help identify ideal candidates for LGB-affirmative treatment.
Our results should be considered in light of study limitations. First, given the early stages of empirically supported mental health interventions for sexual minorities, ESTEEM was tested in a waitlist randomized controlled trial with a three-month follow-up to determine its preliminary efficacy (Pachankis et al., 2015). As a result, we were underpowered to account for differential interaction of time and IH by treatment group. Furthermore, without the inclusion of comparison groups, it is impossible to determine whether IH might also moderate the efficacy of other types of treatment, regardless of LGB-affirmative content. Future research is needed to further support the efficacy of this intervention and establish its moderators, both by monitoring participants over a longer follow-up duration and by comparing LGB-affirmative therapy with non-adapted cognitive behavioral interventions. Additionally, although our sample was diverse with respect to race/ethnicity, employment, and education, it consisted only of gay and bisexual men residing in New York City. Future research should carefully examine the generalizability of the current findings using larger, more representative samples. Future research might also examine the mechanisms through which higher baseline IH might generate improvement from LGB-affirmative treatment. For example, clients with greater IH might become particularly engaged in such treatments, potentially due to a lack of previous affirmative experiences.
The current study highlights the importance of considering IH, especially when measured implicitly, when evaluating clients’ suitability for LGB-affirmative therapy. As interventions for LGB individuals continue to be refined and tailored, a better understanding of who might benefit the most from such tailored treatments will help to ensure delivery of the most appropriate and efficacious treatments. By examining IH as a moderator of the preliminary efficacy of a promising cognitive behavioral intervention that focuses on minority stress, the present research provides a strong starting point for addressing this important research question.
Figure 2.
Treatment change in anxiety (OASIS) for high and low implicit internalized homonegativity (IH)
Acknowledgements
This project was supported by a research grant from the National Institute of Mental Health (R34-MH096607; PI: John E. Pachankis). Katie Wang was supported by a training fellowship from National Institute of Mental Health (T32-MH020031). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to acknowledge the members of the investigative team: Mark Hatzenbuehler, Steven Safren, and Jeffrey Parsons; the contributions of Curtis Phills; and the ESTEEM research team: Evie Arroyo, Aliza Boim, Demetria Cain, Michael Castro, Chris Cruz, Sitaji Gurung, Ethan Fusaris, Ruben Jimenez, Douglas Keeler, Alexa Michl, Chloe Mirzayi, Theresa Navalta, Luis Nobrega, Brian Salfas, Martez Smith, Laurie Spacek, Rachel Proujansky, Jonathon Rendina, Anita Viswanath, Jonathan Warren, and Thomas Whitfield.
References
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May JT. Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. Oxford University Press; New York, NY: 2010. [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, Barlow DH. Development and validation of the Overall Depression Severity and Impairment Scale. Psychological Assessment. 2014;26:815–830. doi: 10.1037/a0036216. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. Journal of Personality and Social Psychology. 1998;74(6):1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Dovidio JF, Nolen-Hoeksema S, Phills CE. An implicit measure of anti-gay attitudes: Prospective associations with emotion regulation. Journal of Experimental Social Psychology. 2009;45:1316–1320. doi: 10.1016/j.jesp.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann W, Gawronski B, Gschwendner T, Le H, Schmitt M. A meta-analysis on the correlation between the Implicit Association Test and explicit self-report measures. Personality and Social Psychology Bulletin. 2005;31(10):1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Davis MC, Nemeroff CJ, Aiken LS. The impact of internalized homophobia on HIV preventative interventions. American Journal of Community Psychology. 2002;30:327–348. doi: 10.1023/A:1015325303002. [DOI] [PubMed] [Google Scholar]
- Jellison WA, McConnell AR, Gabriel S. Implicit and explicit measures of sexual orientation attitudes: Ingroup preferences and related behaviors and beliefs among gay and straight men. Personality and Social Psychology Bulletin. 2004;30:629–642. doi: 10.1177/0146167203262076. [DOI] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, Nazareth I. A systematic review of mental disorder, suicide, and deliberate self-harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70–86. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JL, Dean L. Summary of measures: Mental health effects of AIDS on at-risk homosexual men. Columbia University, Mailman School of Public Health; New York, NY.: 1992. Unpublished manuscript. [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36:38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review. 2010;30:1019–1029. doi: 10.1016/j.cpr.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Norman SB, Cissell SH, Means-Christensen AJ, Stein MB. Development and validation of an overall anxiety severity and impairment scale (OASIS). Depression and Anxiety. 2006;23:245–249. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Goldfried MR. Clinical issues in working with lesbian, gay, and bisexual clients. Psychotherapy. 2004;41:227–246. [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology. 2015;83:875–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow– back: A technique for assessing self– reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biological methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Szymanski DM, Kashubeck-West S, Meyer J. Internalized heterosexism: Measurement, psychosocial correlates, and research directions. The Counseling Psychologist. 2008;36:525–574. [Google Scholar]