Abstract
Evidence on ethnic enclave-health associations for Asian Americans is limited due to an inconsistent definition of ethnic enclave. The authors aimed to establish a robust criterion for defining Asian enclaves in New York City (NYC) and assessed the association between enclave residence and health outcomes among Asian American adults. Data came from 2009-12 NYC Community Health Surveys and 2008-12 American Community Survey. Asian enclave was defined as an area with high dissimilarity and isolation scores as well as high concentration of Asians. Five of 55 NYC community districts were identified as Asian enclaves. After controlling for confounding, enclave residence was associated with positive perception of general health with borderline significance (prevalence ratio = 1.06, 95% CI = 0.98, 1.15), but not with current smoking, hypertension, and diabetes. Ethnic enclave residence in urban areas may not produce a substantial impact on chronic health outcomes for Asian Americans beyond individual-level factors.
Keywords: Asian Americans, New York City, Residence Characteristics, Statistical Model
Introduction
An ethnic enclave is a geographical area where a particular ethnic group is spatially clustered and socially and economically distinct from the majority group. Living in an ethnic enclave has been hypothesized to protect immigrants from potential health hazards owing to increased family ties, familiar culture and help in finding work,1 but evidence for Asian Americans is limited and inconclusive. For example, ethnic enclave residence has been associated with low likelihood of smoking among Asian American women living in California2 and yet higher smoking rates among first-generation Asian immigrant men in New York City (NYC).3 Living in an ethnic enclave has also been associated with diets lower in fat compared to non-enclave residence.4 Both smoking and dietary behaviors mirror those in origin countries demonstrating a preservation of culture within the ethnic enclave after immigration. Other NYC studies have found no independent association between enclave residence and the prevalence of gestational diabetes among recent Chinese immigrants,5 or with urinary sodium or potassium (a marker of fruit and vegetable intake) after adjustment for demographic and socioeconomic factors.6 In contrast, living in an ethnic enclave was associated with limited healthcare access among Asian Americans in California.7
This mixed evidence about the relationship between ethnic enclave residence and health among Asian American populations may be due to inconsistent definitions of ‘ethnic enclave’ across studies and other methodological issues. For instance, the cutpoint in the sociological literature for high segregation for blacks and for Hispanics is typically a dissimilarity or isolation index of 0.6 or greater, however no similar quantitative cutpoint has been established in Asian Americans.8 The diversity of Asian Americans (i.e., cultural and economic differences between South versus East Asians) also presents another challenge, with many available datasets not including information disaggregated by Asian subgroup. Finally, limited statistical treatment of confounding by individual-level characteristics in these studies makes it difficult to isolate true neighborhood-level impacts from individual-level ones. Observed associations between ethnic enclave residence and health may be more likely to be a reflection of particular behaviors (e.g., healthy diets) or underlying health conditions than an independent association between living in an ethnic enclave and health.
This study aimed to address these methodological issues in estimating the association between living in an Asian ethnic enclave and chronic health outcomes among Asian American adults in NYC. Specifically, we examined data using numerical and graphical methods to strengthen validity of presence of an Asian enclave in NYC. In addition, we evaluated differences in demographic and behavioral characteristics between enclave residents and non-residents, and then used propensity score matching to reduce any observed differences. This allowed us to objectively assess whether individual-level confounding was adequately controlled for in estimating a hypothesized link between ethnic enclave residence and self-reported health outcomes.
Methods
Data collection
The primary data source was the NYC Community Health Survey (CHS), a random-digit dial annual telephone survey of 9,000 non-institutionalized NYC adults. Using combined years 2009-2012, it gave rise to 2,863 NYC adults who reported their race as Asian out of approximately 36,000 NYC adults. CHS was conducted using four language options (English, Spanish, Russian, and Chinese), and 36% of 2,863 Asian respondents took the CHS in Chinese. Additional data sources included the United States Census 2010 and 2008-2012 American Community Survey to obtain neighborhood-level information. NYC Department of Health and Mental Hygiene institutional review board determined that this study was not subject to the review because the CHS was considered surveillance.
Measures
To define an Asian ethnic enclave, we first calculated the dissimilarity and isolation indices using United States 2010 Census tract-level race/ethnicity data for 55 NYC community districts, which are local jurisdictions represented by the community boards, and recognized by local residents as neighborhoods. These 55 community districts were defined as slight modified boundaries of the original 59 community districts in order to be mapped against zip code tabulation areas. Because CHS data collected zip codes as a neighborhood of residence, this approach allowed us to identify neighborhood of CHS participants according to NYC community districts. The dissimilarity index measures a proportion of Asians in a particular area that would need to move out of that area in order to achieve an even distribution of non-Hispanic white and Asian populations.9 For example, if one community district were scored with a dissimilarity index of 0.75, 75% of Asians living in that area should move to other areas to make both racial/ethnic groups evenly distributed in NYC overall. The isolation index measures the degree of interaction between Asian residents in a particular area relative to interaction between Asian and non-Hispanic white residents.8,9 If the isolation index were 0.60, the proportion of Asian residents in that area would exceed that of Asians in NYC overall by 60% on average. Both indices, ranging from 0 to 1, were calculated across all census tracks and summed at community district levels. The resulting two indices had a positive correlation (correlation coefficient = 0.27, p-value = 0.04).
Because there is no known cutpoint for Asian versus non-Hispanic white spatial segregation, we graphically examined how NYC community districts were located in terms of two indices and defined community districts with both indices distinctively higher than others as an Asian ethnic enclave. To validate this finding and capture concentration of ethnic groups, which is another dimension of segregation, we calculated percent of Asian residents as well as percent of residents speaking Asian languages at home and speaking English less than very well in NYC census tracts, using 2008-2012 American Community Survey data. We mapped these estimates using ArcMap 10.2.1. If neighborhoods were an Asian ethnic enclave, clusters of these residents should be observed.
Health outcomes included self-reported status on current smoking, hypertension, diabetes, and general health (excellent/very good/good vs. fair/poor). To describe underlying characteristics that might be a common cause of enclave residence-health association, we included detailed information about demographics (age, sex, language at home, household income, education, employment, marital status, nativity, years of living in the United States), health care access (health insurance status, flu shot in the past 12 months, seen provider in last 12 months when needed, told by a doctor to take medicine for high blood pressure), total servings of fruit and/or vegetables yesterday, physical activity, and body mass index (BMI; BMI <18.5: underweight; 18.5≤BMI<25: normal; 25≤BMI<30: overweight; 30≤BMI: obese).
Analysis
Descriptive statistics were calculated to describe demographic and health care access characteristics between ethnic enclave residents and non-residents. We tested whether these characteristics were independent of enclave residence using chi-squared tests. We then estimated association between ethnic enclave residence and chronic health outcomes after accounting for demographic and health care access characteristics using propensity score matching. Our choice of propensity score matching over multilevel regression modeling in multivariate analysis is two-fold: 1) the former, unlike the latter, has statistical and graphical tools to assess the extent to which a large number of confounders are controlled for; 2) complex sample design can be properly incorporated in the former using the conventional analytic approach (e.g., survey weight, Taylor series linearization), whereas sample design adjustment in the latter requires strict assumptions (e.g., large sample size per each cluster, weak sampling bias).10,11
We calculated the likelihood of living in an ethnic enclave (propensity scores) using logistic regression with ethnic enclave residence (dependent variable) and demographic and health care access variables (independent variables) (see Table 1 for the full list of independent variables). Following DuGoff and colleagues’ approach,12 we also included the survey weight as a predictor of the propensity score model in order to strengthen external validity. We created six strata based on propensity scores; ethnic enclave residents and non-residents who shared similar propensity scores were matched within a same stratum. This subclassification option, instead of 1:1 matching, allowed us to have the original complex sample design intact, which prevented from introducing selection bias associated with propensity score matching.10 We then assessed whether this subclassification sufficiently balanced differences in underlying characteristics. Specifically, assessment was based on change of the standardized absolute difference in an average covariate value between enclave residents and non-residents before and after propensity score matching. Because the difference was less than 0.1, we concluded that propensity score matching performed well in reducing observed differences.13
Table 1.
Socio-demographic, behavioral, and healthcare access characteristics of Asian American New York adults by ethnic enclave residence, New York City, 2009-2012
| Living in Asian enclaves | p-values | ||
|---|---|---|---|
|
| |||
| Yes (n=855) | No (n=1,946) | ||
| Socio-demographic/behavioral characteristics | |||
| Sex | |||
| Male | 49% | 52% | 0.30 |
| Female | 51% | 48% | |
| Mean age in years (standard errors) | 45 (0.83) | 43 (0.52) | 0.04 |
| Language at home | |||
| English | 21% | 44% | <0.01 |
| Chinese | 67% | 36% | |
| Indian | 3% | 5% | |
| Others | 9% | 15% | |
| Marital status | |||
| Married | 61% | 57% | 0.15 |
| Divorced | 4% | 4% | |
| Widowed | 3% | 3% | |
| Separated | 1% | 1% | |
| Never married | 26% | 32% | |
| Member of unmarried couple living together | 3% | 3% | |
| Education | |||
| <High school diploma | 29% | 19% | <0.01 |
| High school diploma or GED | 23% | 21% | |
| Some college | 16% | 19% | |
| College graduate or higher | 32% | 41% | |
| Household poverty | |||
| <100% FPL | 41% | 34% | <0.01 |
| 100-200% FPL | 26% | 22% | |
| 200-400% FPL | 12% | 13% | |
| 400-600% FPL | 13% | 16% | |
| >600% FPL | 7% | 15% | |
| Employment | |||
| Employed | 61% | 60% | 0.94 |
| Unemployed | 9% | 10% | |
| Not in labor force | 30% | 30% | |
| Nativity | |||
| US born | 12% | 14% | 0.32 |
| Foreign born | 88% | 86% | |
| Number of years living in the US | |||
| < 5 years | 8% | 12% | 0.21 |
| 5-9 years | 12% | 11% | |
| 10+ years | 68% | 63% | |
| Not asked for US-born adults | 12% | 14% | |
| Physical activity in the past 30 days | 67% | 72% | 0.09 |
| Mean total servings of fruit and/or vegetables yesterday (standard errors) |
2.8 (0.1) | 2.6 (0.1) | 0.04 |
| BMI | |||
| Underweight | 9% | 7% | 0.23 |
| Normal | 60% | 57% | |
| Overweight | 25% | 26% | |
| Obese | 6% | 9% | |
| Healthcare access characteristics | |||
| Any kind of health insurance coverage | 80% | 85% | 0.03 |
| Flu shot or flu vaccine in the past 12 months | 45% | 39% | 0.02 |
| Was there a time in the past 12 months when you needed medical care but did not get it? |
9% | 9% | 0.93 |
| Have been told by a doctor that you need to take medicine for high blood pressure |
23% | 23% | 0.75 |
Abbreviations: BMI = body mass index; FPL = federal poverty level.
Using propensity score-matched data, we estimated the association between ethnic enclave residence and health outcomes via regression models: health outcomes ~ enclave residence + propensity score strata + enclave residence × propensity score strata. Because prevalence of health outcomes were common (i.e., >10%), we used log-linear Poisson regression over logistic regression to address a violation of rare disease assumption.14 We first calculated prevalence ratio (PR) for each propensity score strata and then combined PRs according to proportions to the weighted totals. There were small missing data (household income: 6%, age: 4 %, BMI: 4%, other covariates: <3%), and to address bias due to missing data, we performed multiple imputation using IVEware software and accounted for uncertainties resulting from imputation via Schaffer’s method. All the analyses were performed using STATA 12.0 except for propensity score matching (MatchIt package from R 3.0.2 software). All the estimates accounted for complex sample design. Statistical significance was determined at two-sided p-values <0.05.
Results
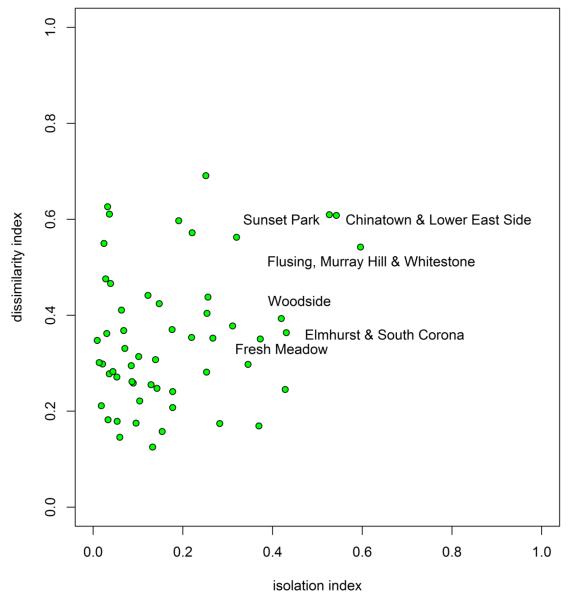
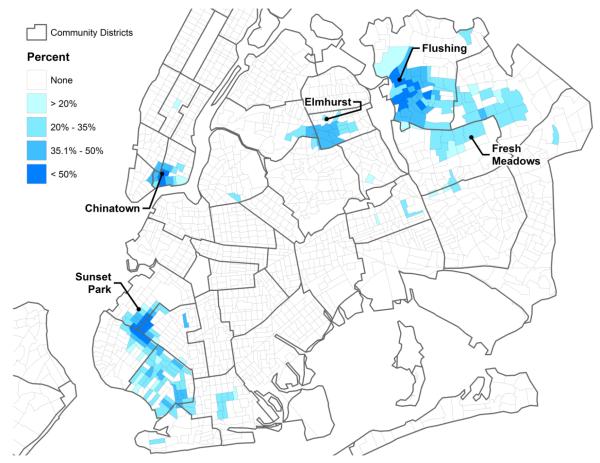
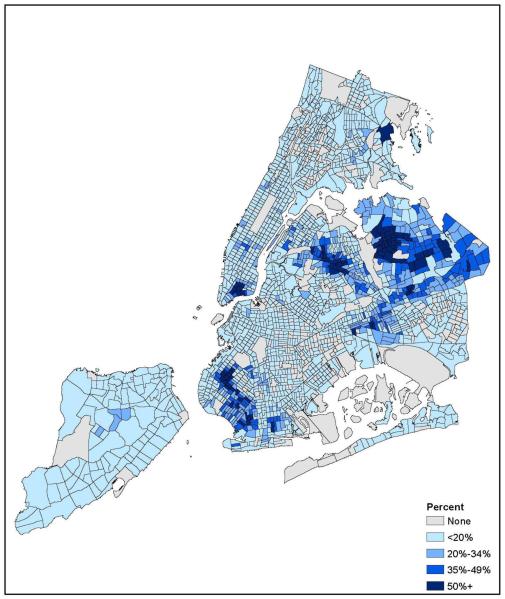
Fig. 1 shows that six community districts had high scores of both indices (>0.35) and were uniquely clustered from other neighborhoods in the upper left corner of the plot. These neighborhoods had Asian residents segregated and isolated from non-Hispanic white residents to the greater extent than the overall trend in NYC. In addition, these neighborhoods, except for Woodside, encompassed areas having >50% of Asian residents speaking Asian languages with limited English proficiency, which also overlapped with areas having >50% of Asian residents (Fig. 2; Appendix I). These graphical examinations led us to determine five community districts as Asian enclaves in NYC: Chinatown, Fresh Meadows, Flushing, Sunset Park, and Elmhurst.
Fig. 1.
Dissimilarity and isolation indices in 55 New York City Community Districts, New York City, 2010
This figure is a scatterplot of 55 New York City Community Districts between dissimilarity and isolation indices. Each dot in the plot represents a position of each New York City Community District in terms of spatial clustering of Asian residents.
Fig. 2.
Percent of Asian residents aged 5 years or older who speak an Asian language at home with limited English proficiency in census tracts, New York City, 2008-2012
This figure describes spatial distributions of Asian residents who have reported speaking an Asian language at home with limited English proficiency.
Source: American Community Survey 2008-2012
Nearly one-third (31%) of Asian American adults in NYC lived in an ethnic enclave. Table 1 shows that Asians living in an ethnic enclave were more likely to be of low socioeconomic status (e.g., low household income and low education attainment; p<0.01) and low health insurance coverage (p=0.03) than those not living in the enclave. Ethnic enclave residents were also more likely to speak foreign languages at home and receive flu vaccinations in the past 12 months, whereas there was no significant difference in employment, nativity, years of living in the United States, BMI, and physical activity between two groups. Total servings of fruit/vegetables on average were slightly higher among ethnic enclave residents versus non-residents (2.8 vs. 2.6, p=0.04).
Asian enclave vs. non-enclave residents had significantly lower crude prevalence of excellent/very good/good general health status (65% vs. 73%, p<0.01), but there was no association between three other health outcomes (current smoking, diabetes, and hypertension) and the ethnic enclave residence (Table 2). Stratified by sex, men living in an ethnic enclave were more likely to smoke than non-residents (25% vs. 14%, p=0.03). For women, crude prevalence of positive perception of general health status was lower among enclave residents relative to non-residents (63% vs. 73%, p<0.01).
Table 2.
Prevalence of chronic health conditions by ethnic enclave residence among Asian American New York City adults, New York City, 2009-2012
| Total |
Males |
Females |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Living in Asian enclaves |
Living in Asian enclaves |
Living in Asian enclaves |
|||||||
|
|
|||||||||
| Yes (n=855) |
No (n=1,946) |
p-values | Yes (n=431) |
No (n=939) |
p-values | Yes (n=424) |
No (n=1,007) |
p-values | |
| Current smoking | 14% | 11% | 0.14 | 25% | 17% | 0.03 | 4% | 4% | 0.71 |
| Diabetes | 10% | 9% | 0.84 | 11% | 10% | 0.56 | 8% | 8% | 0.75 |
| Hypertension | 23% | 23% | 0.75 | 26% | 23% | 0.29 | 21% | 23% | 0.57 |
| General health | 65% | 74% | <0.01 | 68% | 75% | 0.07 | 63% | 73% | <0.01 |
After controlling for individual-level characteristics, the prevalence ratio for perceived general health status by enclave residence was reversed from crude PR (1.06 vs. 0.89), and borderline significant (95% CI = 0.98, 1.15; Table 3). Adjusted prevalence estimates of current smoking, hypertension, and diabetes were not associated with living in an ethnic enclave. In stratified analyses, ethnic enclave residence was associated with current smoking for men (PR = 1.42) and it was borderline significant (95% CI = 0.98, 2.05). All the other chronic health outcomes were not associated with enclave residence after adjusting for confounding.
Table 3.
Adjusted ratiosa of chronic health conditions by ethnic enclave residence among Asian American New York City adults, New York City, 2009-2012
| Total | Males | Females | |
|---|---|---|---|
|
|
|||
| PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Current smoking | 1.19 (0.80, 1.78) | 1.42 (0.98, 2.05) | NE |
| Diabetes | 0.87 (0.58, 1.30) | 1.19 (0.74, 1.91) | 0.79 (0.47,1.35) |
| Hypertension | 0.95 (0.75, 1.20) | 1.10 (0.80, 1.52) | 0.79 (0.56,1.10) |
| General health | 1.06 (0.98, 1.15) | 1.05 (0.95, 1.16) | 1.04 (0.85,1.27) |
Abbreviations: CI = confidence interavl; NE = not estimable due to small cases; PR = prevalence ratio.
Notes: Prevalence Ratio was adjusted for individual-level sociodemogrpahic and healthcare access characteristics via propensity score matching.
Discussion
In this study, we identified five NYC community districts where multiple measures of spatial segregation intersected, capturing the multidimensional construct of ethnic enclave. From a relative perspective, we assessed dissimilarity and isolation with respect to city-wide residential distribution of non-Hispanic whites and Asians. In absolute terms, we captured concentration of Asian residents with limited English proficiency. This approach improved construct validity of ethnic enclave, compared with the conventional approach that an ethnic enclave has been identified by a single measure of segregation or arbitrary cutoff points of segregation measures15 or by anecdotal evidence.1
For Asian American adults, living in these areas was associated with low socioeconomic status. This might reflect greater availability of affordable housing in an ethnic enclave or a tendency to live outside of enclaves among more affluent and educated Asians due to familiarity with economic and social systems. These results are in contrast with previous research that Asian Americans with low acculturation levels but high economic resources are opting to live in an ethnic enclave.1 Inconsistency between current and previous findings is likely due to the fact that our analysis was restricted to NYC only, whereas the prior analysis included NYC as well as wealthier suburbs/enclaves in New Jersey and had larger samples to examine specific Asian subgroups who might have different settlement patterns.
After controlling for individual-level characteristics, enclave residence was not associated with current smoking, diabetes, and hypertension. This null finding persisted even after data were stratified by sex, except for weak evidence on association between current smoking and enclave residence among men. It is inconsistent with existing evidence that ethnic enclave residence has been reported as a health protectant (e.g., current smoking among women) or a risk factor (e.g., gestational diabetes among NYC women from South Central Asian countries, limited healthcare access in California’s ethnic enclaves).2,5,7 One possible explanation of this difference is that individual-level confounding on enclave residence-health relationship might be insufficiently controlled for in previous studies. With limited individual-level variables or lack of control for confounding, previous findings are more likely to be a reflection of individual characteristics associated with ethnic enclave residence than unique neighborhood-level health impacts of living in an ethnic enclave. Another possible explanation is negligible impact of enclave residence on chronic health outcomes beyond individual-level factors. Compared with larger geographic areas, this may be especially true in small urban areas with high population density where an ethnic enclave is easily accessible to residents and nonresidents alike. Lastly, influences of enclave residence on chronic health outcomes might vary across Asian ethnic subgroups, which might be obscured when these were grouped as Asian residents.2,6 However, small sample sizes, even of the largest two groups in NYC (i.e., Chinese, South Asian), prevented us from performing subgroup analyses.
Our study found weak evidence that general perception of health was more positive among enclave residents. It could be explained by the hypothesis that ethnic enclave influences individual health behaviors beyond individual-level characteristics. As Osypuk and colleagues pointed out in their study of Chinese immigrants,4 one mechanism for the pathway from ethnic enclave to individual health is that ethnic enclave provides easy access to ethnic groceries and restaurants, which allow residents to retain traditional diets (e.g., healthier diets than the typical American diet). Another possible pathway is that an ethnic enclave creates ethnically familiar social and physical environments where social networks and social capital can be developed.16 These provide fertile grounds for ethnic businesses, community organizations, and civic institutions.17 Living in ethnic enclaves, immigrants can be economically, culturally and socially connected, and receive essential resources for survival in foreign countries.16 This could help reduce discriminatory exposure and corresponding stress.18
Despite positive perception of general health associated with enclave residence, in our study, this potential benefit may not be seen in actual health conditions including diabetes and hypertension. A possible explanation for this discrepancy is that translation might alter the meaning of the general health question, as enclave residents were more likely to respond to survey questions in their own languages. Evidence shows that foreign language speakers with limited English proficiency tend to rate their health conditions more accurately if the general health question is asked along with a battery of other health-related questions.19 Given the general health question was asked without a health context in the NYC Community Health Survey, rating of health conditions might be more inaccurate among enclave residents, as opposed to non-enclave residents.
In this study, weak evidence of association between enclave residence and prevalence of current smoking was also observed for Asian American men. It is consistent with a previous NYC study that reported the higher odds of smoking among Asian American men living in ethnic enclave after controlling for acculturation and sociodemographic characteristics.3 Living in NYC Asian ethnic enclave might influence them to retain smoking behaviors which are socially and culturally accepted among Asian men.20,21 Given similar distributions of years of living in the United States and nativity between enclave residents and nonresidents, there might be a unique impact of enclave residence on smoking behaviors beyond acculturation (e.g., social cohesion, targeted smoking marketing). Future studies are warranted to contextualize how living in Asian ethnic enclave influences smoking behaviors among Asian American men in NYC.
There were several limitations in this study. First, we did not examine data by specific Asian ethnic groups. Despite growing evidence for the importance of disaggregated data to describe health in Asian Americans,4,6,22 as mentioned earlier, sample sizes were too small to produce reliable estimates when data were stratified by ethnic groups among Asian Americans – even after combining four years of data. Second, the Community Health Survey sample design was based on aggregated zip codes in NYC, which prevented us from estimating health conditions and behaviors in smaller areas such as census tract. Some areas may be misclassified as an ethnic enclave. Third, causal association between ethnic enclave residence and health could not be tested because of lack of temporal information in these cross-sectional data. Fourth, these data may be generalizable to Asian Americans who speak English or Chinese well because other Asian languages were not used as a CHS language option. Lastly, health outcomes were based on self-reported responses, and measurement bias associated with characteristics of respondents cannot be ruled out.
Despite these limitations, this study identified an Asian ethnic enclave using multiple measures of spatial segregation, which strengthens construct validity. Another strength of this study was the use of well-designed local health surveys allowed for describing detailed underlying characteristics associated with ethnic enclave residence among Asian American adults. It enabled us to control for potential individual-level confounding when assessing association between ethnic enclave residence and health outcomes.
New Contribution to the Literature
We identified presence of five Asian ethnic enclaves using spatial measures of dissimilarity, isolation, and concentration. Asian NYC residents in these ethnic enclaves, compared with non-residents, were more likely to be of low socioeconomic status. After controlling for individual-level differences, enclave residence was weakly associated with positive perception of general health status and current smoking for men only, but not associated with diabetes and hypertension. This study demonstrates an analytic approach to capture an Asian ethnic enclave with improved construct validity. It also suggests that ethnic enclave residence in densely populated urban areas may not produce a substantial impact on chronic health outcomes among NYC Asian American residents beyond individual-level factors.
Acknowledgements
The authors thank Cynthia Driver, Kenneth Mort, and Gary Belkin for their helpful comments on the analysis. This research was supported by P60MD000538 from the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities, U48DP005008 from the Centers for Disease Control and Prevention (CDC) and UL1TR001445 from NCATS/NIH. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH and CDC.
Abbreviations
- CHS
Community Health Survey
- BMI
Body Mass Index
- NYC
New York City
- PR
Prevalence Ratio
Appendix I. Percent of Asian residents aged 5 years or older in census tracts, New York City, 2008-2012
Source: American Community Survey 2008-2012
References
- 1.Logan JR, Zhang W, Alba RD. Immigrant enclaves and ethnic communities in New York and Los Angeles. American Sociological Review. 2002;67:299–322. [Google Scholar]
- 2.Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Association between neighborhood context and smoking prevalence among Asian Americans. Am J Pub Health. 2009;99(5):885–892. doi: 10.2105/AJPH.2007.131854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li S, Kwon SC, Weerasinghe I, Rey MJ, Trinh-Shevrin C. Smoking among Asian Americans: Acculturation and Gender in the Context of Tobacco Control Policies in New York City. Health Promot Pract. 2013;14(5):18S–28S. doi: 10.1177/1524839913485757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Social Science & Medicine. 2009;69(1):110–120. doi: 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Janevic T, Borrell LN, Savitz DA, Echeverria SE, Rundle A. Ethnic enclaves and gestational diabetes among immigrant women in New York City. Social Science & Medicine. 2014;120(C):180–189. doi: 10.1016/j.socscimed.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 6.Yi SS, Ruff RR, Jung M, Waddell EN. Racial/ethnic residential segregation, neighborhood poverty and urinary biomarkers of diet. Social Science & Medicine. 2014 doi: 10.1016/j.socscimed.2014.10.030. online first. [DOI] [PubMed] [Google Scholar]
- 7.Chang E, Chan KS. Variations in Asian Americans: how neighborhood concordance is associated with health care access and utilization. Am J Pub Health. 2015;105(1):66–68. doi: 10.2105/AJPH.2014.302275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glaeser EL, Vigdor JL. The Brookings Institution Survey Series. Center on Urban and Metropolitan Policy; 2001. Racial Segregation in the 2000 Census: Promising News. Available at http://www.brookings.edu/es/urban/census/glaeser.pdf. [Google Scholar]
- 9.Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67(2):281–315. [Google Scholar]
- 10.Lim S, Marcus SM, Singh TP, Harris TG, Levanon Seligson A. Bias due to sample selection in propensity score matching for a supportive housing program evaluation in New York City. PLos ONE. 2014;9(10):e109112. doi: 10.1371/journal.pone.0109112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brumback BA, Dailey AB, Zheng HW. Adjusting for confounding by neighborhood using a proportional odds model and complex survey data. Am J Epidemiol. 2012;175(11):1133–1141. doi: 10.1093/aje/kwr452. [DOI] [PubMed] [Google Scholar]
- 12.DuGoff EH, Shuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. HSR. 2014;49(1):284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Normand SL, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following an acute myocardial infarction in the elderly: A matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 14.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 15.Allen JP, Turner E. Ethnic residential concentrations in United States metropolitan areas. The Geographical Reviews. 2005;95(2):267–285. [Google Scholar]
- 16.Zhou M, Lin M. Community transformation and the formation of ethnic capital: immigrant Chinese communities in the United States. Journal of Chinese Overseas. 2005;1(2):260–284. [Google Scholar]
- 17.Zhou M, Cho M. Noneconomic effects of ethnic entrepreneurship: a focused look at the Chinese and Korean enclave economies in Los Angeles. Thunderbird International Business Review. 2010;52(2):83–96. [Google Scholar]
- 18.Shell AM, Peek MK, Eschbach K. Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas city, Texas. Soc Sci Med. 2013;99:56–63. doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee S. Self-rated health in health surveys. In: Johnson TP, editor. Health Survey Methods. Wiley; Hoboken, NJ: 2014. [Google Scholar]
- 20.Chae DH, Gavin AR, Takeuchi DT. Smoking prevalence among Asian Americans: findings from the national Latino and Asian American study (NLAAS) Public Health Rep. 2006;121(6):755–763. doi: 10.1177/003335490612100616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma GX, Shive S, Tan Y, Freeley RM. The impact of acculturation on smoking in Asian American homes. J Health Care Poor Underserved. 2004;15:267–280. doi: 10.1353/hpu.2004.0024. [DOI] [PubMed] [Google Scholar]
- 22.Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. J Health Care Poor Underserved. 2010;21(4):1354–1381. doi: 10.1353/hpu.2010.0939. [DOI] [PMC free article] [PubMed] [Google Scholar]