Abstract
Objective
Given the prevalence of co-occurring risky sexual behavior and drinking among ED patients, we developed a motivational intervention (MI) to address both behaviors. This study tested efficacy of a single session MI compared to Brief Advice (BA) for reducing heavy drinking and condomless sex in adult ED patients screening positive for both.
Method
372 patients were randomized to MI (n = 184) or BA (n = 188). Alcohol and sex risk outcomes were assessed over 9-months.
Results
Generalized Estimating Equations models analyzing n = 327 patients with follow-up data provided strong support for efficacy of this integrated alcohol and sex-risk MI. Compared to BA, and after controlling for baseline covariates, those in MI reported significantly fewer heavy drinking days, drinks per week, and were less likely to engage in excessive drinking over follow up (all ps < .05). MI was also favored over BA for reducing sex risk. Compared to BA, those in MI reported significantly fewer days on which they engaged in condomless sex with casual partners, had lower odds of reporting any condomless sex with a casual partner, and reported fewer days of sex under the influence of alcohol/other drugs (all ps < .05).
Conclusion
This innovative MI was acceptable, feasible, and successfully delivered in two community hospitals and thus shows great promise for scalability and dissemination into complex health settings where newly insured at-risk individuals are likely to seek care.
Public Health Significance
This study strongly suggests that a multi-risk brief motivational intervention targeting both the heavy drinking and risky sexual behavior of at-risk Emergency Department patients is effective for reducing both risky behaviors when compared to brief advice.
Keywords: emergency care, alcohol, sex risk, motivational intervention
Emergency Departments (EDs) are the only source of medical care for many patients, particularly the uninsured and underinsured (Tang et al., 2010), and EDs serve as a primary site of care for many individuals at risk for STI/HIV (Rothman, 2004). Further, it is well known that people with alcohol use problems are likely to be treated in EDs for problems related or unrelated to their alcohol use (Cohen, et al., 2007), and alcohol-related ED visits have increased significantly over the past 15 years (Cherpitel & Ye, 2012). Though expanded Medicaid coverage may eventually reduce ED care, a recent study found increases in ED visits across various medical reasons for the visits among the newly insured (Taubman, et al., 2014).
The co-occurrence of heavy drinking and sexual risk taking contribute substantially to STI and HIV acquisition (Hendershot & George, 2007; Shuper, et al., 2010), and recent reviews call attention to the co-occurrence and reciprocal interactions of alcohol and HIV/STI risk behaviors in high-risk populations (e.g. Fritz, et al., 2010; Rehm, et al., 2012). Although the prevalence of these co-occurring risky behaviors has not been extensively studied in ED populations, a recent study reported the co-occurrence of heavy drinking and risky sexual behavior to be quite high among ED patients (Mastroleo et al., 2015). More specifically, we found approximately 50% of patients under age 35 screened positive for both risky behaviors.
Systematic reviews and meta-analyses indicate that the effect of alcohol use on sexual behavior varies by context, gender, familiarity with partner and experience (Halpern-Felsher, et al., 1996; Kalichman, et al., 2007). Further, there are inconsistencies in the presence and magnitude of the association between alcohol and specific sex-risk outcomes. As alcohol and other drug use before or during sex has been linked with risk for HIV and other STIs (Hendershot & George, 2007; Woolf et al., 2009), the co-occurrence of substance use with sex is worthy of clinical consideration. Specifically, condomless sex with nonsteady partners has been implicated in the risk for transmission of HIV and other sexually transmitted infections (Parsons et al. 2005), so reducing such risky sexual behavior is a reasonable clinical goal. However, before addressing the co-occurrence between heavy drinking and risky sexual behavior, it is important to consider dyadic, motivational, and contextual factors.
While the co-occurrence of alcohol and risky sexual behavior in high-risk populations has suggested the need to develop targeted interventions addressing both behaviors simultaneously (Fritz, et al., 2010; Sander et al., 2013; Wray et al., 2015), very few studies have attempted to do so. We know of only one study, conducted in the context of an ED that addressed both alcohol and risky sexual behavior. Edelman and colleagues (2012) combined alcohol/sex risk reduction counseling with rapid HIV testing in an uncontrolled feasibility study. The results showed reductions in both risky behaviors, leading the authors to call for a future randomized controlled trial to assess efficacy. Another study, conducted during an ED visit involved heroin/cocaine users and risky sexual behavior (Bernstein et al., 2012). While that study found reductions in both targeted risky behaviors, there were no differences between a condition that involved a brief motivational intervention (MI) with voluntary counseling/testing vs. the voluntary counseling/testing control alone. This study did not target or report on alcohol use. Furthermore, only 72% of the study patients were followed up at either the 6 or 12-month follow-up period, underscoring potential difficulties with attrition in such trials.
Given the above findings regarding the feasibility of multi-risk ED interventions, findings in the literature pointing to the efficacy of MI in medical care settings across a broad range of health risk behaviors (Lundahl et al., 2013), and the high prevalence of co-occurring risky sexual behavior and heavy drinking in the ED (Mastroleo et al., 2015), we developed a brief theory-based intervention to address both risky behaviors. We reasoned that a MI that considers and can address idiographic determinants of heavy drinking, sex risk, and risky sex while under the influence of alcohol, may be best suited to the treatment of these co-occurring behaviors. We chose to study multi-risk patients in the ED setting where they are likely to seek treatment. The objective of this paper was to test the efficacy of a single session individual MI that focused on both alcohol use and sexual risk behaviors compared to a Brief Advice (BA) condition in an adult ED sample indicating risk levels for both alcohol and sexual risk behaviors. We hypothesized that MI compared to BA would result in significantly greater reductions in heavy drinking and condomless sex over a 9 month follow up.
Methods
Patients and Recruitment
Recruitment took place in the EDs of two Rhode Island community hospitals (herein referred to as Site 1 and Site 2) from May 2011 to November 2013. English-speaking patients ages 18 to 65 who received medical care in the ED were approached during breaks in medical treatment and screened to determine degree of heavy/problem alcohol use and engagement in risky sexual behaviors. Eligibility criteria included: 1) meeting the criterion for hazardous drinking (total score ≥ 8 for males; ≥ 6 for females) on the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993) or endorsing at least one episode of heavy drinking [(≥ 5 drinks for males; ≥ 4 drinks for females; NIAAA (2004)] in the past three months; and 2) engaging in the following sex-risk behaviors in the past three months: condomless sex or consuming alcohol/other drugs prior to or during sex; and sexual activity with a non-steady partner in the same period or with a steady partner where infidelity is questioned or known. Patients in a mutually monogamous relationship for longer than six months, those receiving treatment for a self-inflicted injury/suicide attempt, and those in police custody were excluded.
Screening, Power Analyses and Randomization
Patients were approached and screened by trained masters- or doctoral-level interventionists. After establishing eligibility, interventionists conducted a mental status screen to ensure that patients were able to provide informed consent (i.e., were oriented, able to concentrate, and able to understand and remember study requirements). Screening was conducted Monday through Saturday, 8 AM to 8 PM (with occasional screening also occurring between 8 and 10 PM). Of 24,918 age-eligible adult patients on site during working shifts, 6,486 (26.0%) were screened, including 3,665 (56.5%) female and 2,821 (43.5%) male patients. Common reasons for not screening were: advised not to screen by clinician (20.5%), declined screen (16.9%), discharged prior to approach (13.7%), suicidal (7.4%) inadequate privacy (3.5%) and under medical isolation (3.2%). Of those screened (see Consort Figure 1), 645 (9.9%) met inclusion criteria, of which 400 (62.0%) agreed to participate and provided informed consent. Of the 245 patients who were eligible but did not consent, refusal was the primary reason (n = 146), followed by discharge prior to consent (n = 99).
Consort Figure 1.
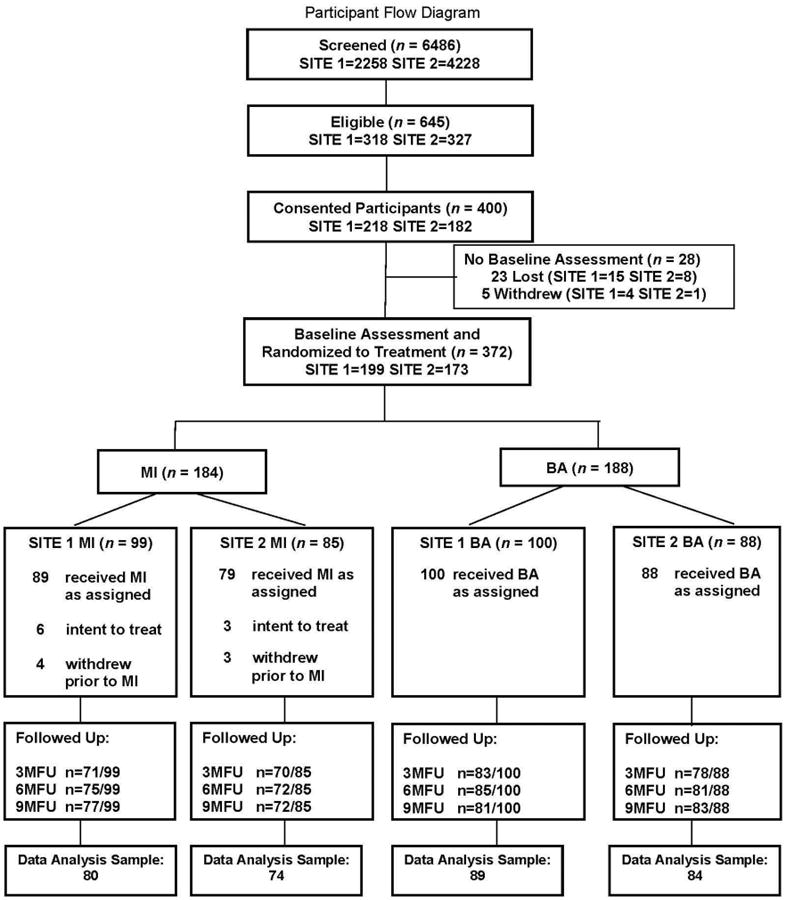
Note: Data Analysis Sample includes any participants with at least one follow up.
While the original power analysis called for recruiting 302 patients in order to retain 256, we extended the study to a second ED to increase generalizability. To achieve comparable sample sizes across sites additional patients were recruited. Importantly, interim analyses were not conducted to establish final sample size. The conservative expected effect for MI vs BA was at least Cohen's d = .40, based on several previous MI studies in which effect sizes for drinks per week, heavy drinking days, and number of drinking days ranged from .44 to .64 (Monti et al., 1999; Monti et al., 2007).
Of the 400 patients who consented, 372 (93.0%) completed baseline assessments and were then randomized to condition (MI or BA). The 28 patients who did not complete the baseline either were discharged before the baseline assessment (n = 28) or withdrew (n = 5). Completion of the baseline assessment took approximately 45-60 minutes, and all measures were completed during or within the two weeks following the patient's ED discharge. Among patients who completed the baseline assessment after the day of their ED discharge (n = 174), the average number of days to completion was 4.57 (SD = 3.57, Max Days = 18).
Of the 184 patients randomized to MI, 168 (91.3%) received intervention. All randomized to BA (n = 188; 100%) received BA. The final sample size of 372 includes all patients randomized to treatment condition regardless of whether they received treatment as assigned (i.e., intent-to-treat sample). Average number of days from baseline to treatment completion was 1.30 (SD = 2.99, Max Days = 16). The primary reasons for not conducting the intervention during the index visit were either that the patient had medical considerations that precluded conducting the intervention or was discharged. Phone calls, text messages and emails prompted return visits for these interventions. Patients were paid $50 for baseline assessments. University and hospital Institutional Review Boards approved all procedures.
Procedure
A breathalyzer was administered at the time of consent and if BAC was <.04, clinicians proceeded to administer a mental status screen (MSS). If the patient failed the MSS due to alcohol intoxication he/she was scheduled to return when sober. After informed consent, patients completed the baseline battery. The majority of assessments were collected using a web-based computerized assessment, with paper and pencil data collection used as a backup in cases when the internet was not available in the ED. The majority of measures were self-report questionnaires with several key measures administered in interview format by the project staff to ensure accuracy as described below. Patients were then randomized to either the MI or BA condition using a computer-based urn randomization procedure (Stout et al., 1994). Included in the urn to maximize the opportunity to create similar groups between conditions were patient age, gender, education, race, AUDIT score, and past 3-month condom use.
Follow-up Assessments
Patients were mailed a monthly postcard asking them to confirm contact information. Upon returning each card, patients received $5. Telephone and text message reminders also were used throughout the study. Follow-up assessments were conducted at equal intervals of 3, 6, and 9 months by trained research assistants masked to intervention condition, and patients were paid $50, $75, and $100, respectively for each. Patients earned a $25 bonus for completing all three follow ups within 10 days of their due dates. Interviews were completed in person, except when telephone interview was the only way to obtain the data (e.g., if a patient had relocated); 3.12% of all follow ups were completed by telephone. Three-, 6-, and 9-month follow-up rates were 81.4%, 84.4%, and 84.1%, respectively. All were completed within two weeks of their due date.
Seven patients withdrew after randomization but prior to completing the assigned intervention; all seven were assigned to MI. Ten MI patients withdrew during the follow-up period, five at 3-M, three at 6-M, and two at 9-M follow up. In the BA condition one patient had died at 3-M follow up and four withdrew during the 3-M follow-up period, three at 3M and one at 9M. Patients who withdrew from the study did not complete assessments at any follow ups. Of the patients assigned to treatment (n = 372), 45 did not complete any follow ups. One patient in MI had her data removed at 3-M and 6-M due to admitting falsifying answers.
Measures
Screening Measures
Alcohol Use Disorders Identification Test (AUDIT)
The AUDIT was administered as the primary screening assessment for alcohol use. This 10-item questionnaire was developed by the WHO to identify patients whose alcohol consumption has become harmful to their health (Babor, et al., 2001). Each item is scored on a 4-point scale with a cumulative score range of 0-40; higher scores suggest more harm. A score of eight or higher has been used to index hazardous alcohol use (Conigrave et al., 1995), but more recent research suggests a more appropriate cut point of six or higher for females (Reinert & Allen, 2002).
Sexual Risk-Taking
Inclusion criteria were assessed using a brief screening questionnaire comprising six items drawn from prior research (Kalichman, et al., 1998; Millstein & Moscicki, 1995) that have been successfully used to identify individuals at risk for HIV/STIs. The first item assessed the patient's total number of sexual partners (vaginal or anal sexual intercourse) over the past three months. If the patient indicated having only one sexual partner, the second question assessed length of the relationship. Four items measured sex-risk behaviors over past three months, including: 1) frequency that the partner(s) has been sexually active with anyone else; 2) frequency of condomless intercourse (vaginal or anal); 3) frequency of consuming alcohol before/during sex; and 4) frequency of using any drug before or during sex.
Mental Status Screen (MSS)
This brief neuropsychological screener assesses basic cognitive functions including orientation (8 items), memory (2 items), and attention (2 items). Highest possible score was 26 and patients who scored under 18 were not enrolled. It was used to determine if a patient had cognitive dysfunction and should therefore not be recruited.
Demographics and Key Variables
Relevant demographic information was obtained in a self-report questionnaire including specific items for age, gender, race, ethnicity, years of education, and annual household income. History of STI testing was also assessed.
Baseline Assessments
Primary Outcome Measures
Primary outcomes were selected as documented in the original grant proposal and study protocol (R01AA009892).
Time-Line Follow-back for Substance Use and Sexual Behavior (TLFB-SS; Carey, et al., 2001). The TLFB-SS is a structured, calendar-aided interview adapted from the Alcohol TLFB (Sobell & Sobell, 2003; Sobell et al., 1986) used to retrospectively assess drinking and sexual behavior over the previous 30 days. Project staff administered the TLFB-SS to determine the number of standard drinks consumed each day, and any sexual behavior each day. For days on which sexual activity occurred, patients were asked about partner type (steady, non-steady), partner gender (male, female), sex type (vaginal, anal-insertive, anal-receptive), and whether alcohol and/or drugs were consumed prior to sex. In addition, as a complementary measure we asked patients to estimate number of times they had sex in the past 3 months, number of times they had unprotected sex, and partner type. Alcohol indices derived from the TLFB-SS included number of heavy drinking days (≥ 4/5 drinks for women/men) and average number of drinks consumed per week. Sex-risk indices derived from the TLFB-SS included: 1) number of days on which condomless vaginal or anal sex occurred with a non-steady partner; and 2) a dichotomous variable reflecting whether a patient reported any condomless sex with a non-steady partner.
Secondary Outcome Measures
Clinical benefit outcomes
To aid in the interpretation of findings for public health guidelines two additional indices were derived from the TLFB-SS: the first was a dichotomous variable indicating whether one's past 30-day drinking pattern would be classified as excessive drinking by the CDC; (i.e., ≥ 8/15 drinks per week for women/men; Bouchery, et al., 2011; Esser, et al., 2014). The second followed FDA recommendations for alcohol trial efficacy endpoints: a dichotomous variable indicating whether patients' drinking “violates heavy drinking limits” of ≥ 4/5 drinks in one day for women/men (U.S FDA, 2015). The FDA standard is more stringent in that a single heavy drinking occasion results in a “heavy drinking” classification.
Alcohol-related problems were assessed using the Short Inventory of Problems (SIP; Feinn et al., 2003), a 15-item questionnaire developed as a short form of the Drinker Inventory of Consequences (DrInC; Miller et al., 1995). The SIP used a past 3-month timeframe to assess frequency of experiencing various alcohol-related problems on a 4-point scale (0 = never, 1 = once or a few times, 2 = once or twice a week, and 3 = daily or almost daily) and was administered at baseline and follow ups. The total score (Cronbach's alpha = .92 at baseline) was analyzed to assess treatment effects on frequency of adverse consequences of drinking.
Sex under the influence of alcohol and/or other drugs
The TLFB-SS provided number of days on which patients reported having engaged in sexual activity under the influence.
Interventions
Motivational Intervention
The MI session, based on the principles of Miller & Rollnick (2002), were conducted by six doctoral- and masters-level interventionists. Interventionists read Motivational Interviewing (Miller & Rollnick, 2002) and a treatment manual, and received 20 hours of training that included didactic presentations, video- and live-demonstration, and extensive role-plays. Training and weekly group supervision was conducted which included review of audio recordings in order to provide individual feedback to interventionists. Initially, a two-session MI was planned, however during a piloting phase we found we could incorporate all essential elements in just one session. As such we shifted to complete the intervention in one session as we determined requiring patients to return for a second session would negatively impact intervention completion rates.
The manualized, one-session MI incorporated open-ended exploration of pros/cons of drinking, personalized and printed graphic feedback of alcohol use and consequence assessments, normative comparisons, discussion about use and consequences and of sexual risk behaviors including engaging in sex with multiple partners and condomless sex. Feedback was generated using responses to baseline assessments, which were then incorporated into a printed report, discussed, and provided in confidential take-home packets. The goal was to help patients explore their alcohol use and sex risk behaviors and what they might want to change and, for those interested in change, establishing goals for reduced drinking or abstinence, increasing condom use, and discussing barriers to change. Therapists were trained to adapt to individual patient needs. Upon conclusion, all were offered opportunity to complete a HIV test free of charge and were provided lists of local sexual health, substance abuse treatment, and mental health resources. The MI was conducted within about two weeks of the baseline (average number of days from baseline = 2.40; range = 0 to 16 days). Average time to completion was 63.11 minutes (SD = 20.76). All sessions were conducted in a private office adjacent to the ED.
Brief Advice (BA)
Patients in BA received intervention consistent with standard medical practice when alcohol problems or sex-risk behaviors are indicated. Interventionists offered advice about patients' level of alcohol and sexual risk behaviors. Specifically, patients were told they show signs of risk associated with alcohol use in that they scored above a cut-score on our alcohol screening measure, and that they reported recently engaging in sexually risky behaviors. Patients were advised to reduce alcohol use and to use condoms. Identical to MI, at the conclusion of BA all were offered the opportunity to complete an HIV test and were provided a list of local resources. Average number of days from baseline to BA = 0.32 (range = 0 to 11). Average amount of time to complete BA was 1.92 minutes (SD = 0.88).
Intervention Integrity
All MI and BA sessions were audio recorded to evaluate integrity and fidelity. Of the MI sessions recorded, half (N = 93) were randomly selected across all interventionists and all years of data collection, and were then evaluated using the Motivational Interviewing Skills Code Version 2.5 (MISC; Houck, et al., 2010). The MISC has been used to establish MI fidelity in a number of studies testing brief interventions (e.g., Borsari et al., 2012). Each audiosession was parsed and then coded by independent raters to establish integrity to MI. Four independent raters were trained and then coded the 93 recordings while double codes were conducted on 20% to evaluate interrater reliability. Intraclass correlation coefficients were calculated to determine interrater reliability for each variable measured (using the 20% sample of double-coded tapes, n = 19). Reliabilities were all in the “good” or “excellent” range according to criteria established by Ciccetti (1994): (Empathy = .71, Support Autonomy = .76, Collaboration = .79, Acceptance = .51, Evocation = .62, Direction = .64). Results indicated interventionists demonstrated high levels of MI-consistent skills (MICO; i.e., complex reflections, affirmations, and open questions), and low levels of MI-inconsistent behaviors (i.e., confrontation and warning). On MISC global scores, therapists were rated above average on Empathy (M = 3.99, SD = .70, range 2 - 5), Support Autonomy (M = 4.03, SD = .57, range = 2 - 5), Collaboration (M = 3.99, SD = .69, range = 2 - 5), Acceptance (M = 4.16, SD = .85, range = 2 - 5), Direction (M = 4.24, SD = .74, range = 3 - 5), Evocation (M = 4.06, SD = .66, range = 2 - 5), with all meeting proficiency on these (scores ≥ 3).
Data Analysis Plan
The original analysis plan called for using transformations as needed. We first describe sample characteristics by condition and site and then present descriptive statistics on primary and secondary outcomes. To test between-groups differences on outcomes that had count distributions, including number of heavy drinking days, number of days of condomless sex with a non-steady partner in the past 30 days, and number of days of sex under the influence across follow ups, we ran Generalized Estimating Equations models (GEE; Zeger & Liang, 1986) specifying a negative binomial model for over-dispersed count data with a log link function; those models present incidence rate ratios (IRRs) as the index of effect size. Outcomes that had a continuous distribution, including (log-transformed) average number of drinks per week and frequency of drinking-related problems (SIP score) were analyzed with a normal GEE model; those models present effect sizes as in standardized units of the DV (i.e., effect size d). We also examined three dichotomous outcomes, each based on past 30-day data at each follow up: whether patient drinking patterns met the CDC excessive drinking criterion; whether patients' drinking met the FDA heavy drinking criterion; and whether patients engaged in any condomless sex with a non-steady partner. These GEE models used a binomial distribution with a logit link function and provide odds ratios (ORs) as a measure of effect size. Based on examination of quasi-likelihood information criterion, models for sex-risk behaviors specified a compound symmetric working correlation matrix, and models for alcohol use outcomes used an unstructured matrix. Condition was dummy-coded with BA as reference group. Models included as covariates: 1) value of the respective DV at baseline (number of days of condomless sex with a non-steady partner, and average number of drinks per week were log-transformed to correct positive skew); and 2) a term carrying linear effect of time, centered so the 6-M follow up had a value of 0. Models also included main effects for gender (dummy-coded with males as reference group) and recruitment site, as well as the time by treatment interaction, which indicated whether the effect of MI became stronger or weaker over follow up.
Prior to testing our primary GEE models, we first conducted analyses to examine whether there were site by treatment interactions in any model. None of these tests approached significance (ps > .15) and were therefore not considered further.
Missing Data
Ten patients had incomplete data at baseline for the TLFB for sex risk. Values for all of these patients were estimated based on the available TLFB data or from the past 3-month measure of sex-risk behaviors. The analytic sample consisted of all patients with valid data for at least one follow up (N = 327); 45 who had no follow up data were excluded from analyses. Of the patients in the data analytic sample, some data were missing due to either a missing follow up or a lack of response to items. The number of observations for the outcome variables across three follow ups ranged from 920 to 928. Analyses used all available data. Attrition analyses were conducted to determine whether follow-up completion was significantly associated with condition, and whether patients who provided data at follow up differed from those who did not on key variables of interest at baseline.
Results
Participants
The sample comprised slightly more females (53.5%) than males, and was predominantly White (80.1%), 14.2% was Hispanic. Average age was 29.19 years (range 18 – 60). Education varied, with 17.5% having not completed high school, 38.2% having a diploma or GED, and the rest (44.4%) completing at least some college/technical school. Average AUDIT total score was 10.96 (SD = 8.44; range: 1-40). Regarding history of STI testing, 76% had completed a previous STI test, of which 43% were positive. Additional descriptive information is provided in Table 1.
Table 1. Baseline differences on demographics and key variables by site and treatment condition.
| Variable | Sample Summary (n=372) N (%) or Mean (SD) | Site 1 (n=199) N (%) or Mean (SD) | Site 2 (n=173) N (%) or Mean (SD) | BA (n=188) N (%) or Mean (SD) | MI (n=184) N (%) or Mean (SD) |
|---|---|---|---|---|---|
| Demographics | |||||
| Age in yearsa* | 29.2 (9.3) | 30.2 (9.5) | 28.1 (9.0) | 30.0 (9.4) | 28.4 (9.1) |
| Gender: Female | 199 (53.5) | 104 (52.3) | 95 (54.9) | 95 (50.5) | 104 (56.5) |
| Ethnicity: Hispanic | 53 (14.2) | 33 (16.6) | 20 (11.6) | 29 (15.4) | 24 (13.0) |
| Race: Non-Whitea*** | 74 (19.9) | 60 (30.2) | 14 (8.1) | 41 (21.8) | 33 (18.0) |
| Education | |||||
| Less than high school | 65 (17.5) | 42 (21.1) | 23 (13.3) | 32 (17.0) | 33 (17.9) |
| High school/GED | 142 (38.2) | 78 (39.2) | 64 (37.0) | 71 (37.8) | 71 (38.6) |
| At least some college | 165 (44.4) | 79 (39.7) | 86 (49.7) | 85 (45.2) | 80 (43.5) |
| Employment: Unemployed | 151 (40.6) | 89 (44.7) | 62 (35.8) | 77 (41.0) | 74 (40.2) |
| Incomea** | |||||
| <$10,000/yr | 124 (33.5) | 78 (39.4) | 46 (26.7) | 64 (34.2) | 60 (32.8) |
| $10,000-30,000/yr | 120 (32.4) | 69 (34.8) | 51 (29.7) | 56 (29.9) | 64 (35.0) |
| >$30,000/yr | 126 (34.1) | 51 (25.8) | 75 (43.6) | 67 (35.8) | 59 (32.2) |
| Sexual Orientation | |||||
| Heterosexual | 321 (86.5) | 169 (85.4) | 152 (87.9) | 160 (85.6) | 161 (87.5) |
| Homosexual | 13 (3.5) | 8 (4.0) | 5 (2.9) | 7 (3.7) | 6 (3.3) |
| Bisexual | 33 (8.9) | 19 (9.6) | 14 (8.1) | 17 (9.1) | 16 (8.7) |
| Not Sure | 4 (1.1) | 2 (1.0) | 2 (1.2) | 3 (1.6) | 1 (0.5) |
| Alcohol Use Variables | |||||
| No. Heavy drinking days | 5.9 (7.0) | 5.7 (6.6) | 6.0 (7.5) | 5.9 (6.8) | 5.8 (7.3) |
| Average no. drinks/week | 17.1 (33.6) | 15.4 (19.8) | 19.0 (44.5) | 19.8 (43.3) | 14.3 (18.9) |
| CDC excessive drinking | 155 (41.7) | 83 (41.7) | 72 (41.6) | 87 (46.3) | 68 (37.0) |
| FDA heavy drinking | 322 (86.6) | 176 (88.4) | 146 (84.4) | 164 (87.2) | 158 (85.9) |
| SIPb* | 5.4 (4.7) | 5.4 (4.7) | 5.4 (4.8) | 6.0 (4.9) | 4.9 (4.4) |
| Sex Risk Variables | |||||
| No. days Condomless Sex with Non-steady partner | 2.2 (5.5) | 1.8 (4.3) | 2.8 (6.5) | 1.9 (5.0) | 2.6 (5.9) |
| Any Condomless Sex with Non-steady partner | 125 (33.6) | 58 (29.1) | 67 (38.7) | 60 (31.9) | 65 (35.3) |
| No. days Sex with Alcohol and/or Drugs | 5.1 (6.8) | 5.2 (6.7) | 4.9 (7.0) | 5.4 (7.1) | 4.7 (6.5) |
| History Positive STI Test | 119 (32.3) | 70 (35.9) | 49 (28.3) | 57 (31.0) | 62 (33.7) |
Note:
Significant differences by site are indicated by superscript
Significant differences by treatment condition are indicated by superscript
Accompanying asterisks indicate level of significance:
p<.05;
p<.01;
p<.001.
Untransformed values. SIP = Short Inventory of Problems. Non-steady partner = A non-committed relationship, in which you had sex one or more times, and you have the understanding that your partner may have sex with other people. Missing data from one participant for race, two for income, one for sexual orientation, and four for history of positive STI test.
Site and Treatment Condition Baseline Differences
There were no significant differences between hospital sites related to recruitment rates. Table 1 provides a site comparison of demographic and behavior variables at baseline. Patients at Site 1 were slightly older, more likely to be non-White, and had lower income. There were no site differences at baseline on alcohol or sex-risk outcomes. Table 1 also provides a comparison of the two conditions on demographics and baseline values of outcome variables. Only one difference emerged; patients in BA had significantly higher average SIP scores at baseline.
Analysis of Differential Treatment Completion
A greater number of patients in MI than BA did not receive assigned treatment (n = 16 versus 0, respectively, χ2 (df=1) = 17.08), likely because MI took longer to complete, and some patients could not schedule sufficient time. Pearson chi-square tests comparing those assigned to MI who did versus did not receive MI showed the two groups did not differ significantly on hospital site, gender, Hispanic ethnicity, non-White race, education, health insurance, our dichotomous drinking pattern variables, or our dichotomous sex-risk index (any condomless sex with a non-steady partner), all ps > .10. Those who completed MI were significantly more likely to be unemployed (42.9%) than those who did not (12.5%), χ2 (df=1) = 5.60, p = .018, and consistent with that, MI completers had lower levels of income (34.5% reported income < $10,000/year) than non-completers (13.3% < $10,000), χ2 (df=2) = 6.11, p = .047. Independent t-tests comparing those who did versus did not receive MI showed no differences on age or on baseline values of any of our alcohol or sex-risk outcome variables (all ps > .10).
Analysis of Potential Attrition Bias at Follow Up
Of the 372 patients assigned to treatment, 45 did not complete any of the follow ups, including 15 (8.0%) assigned to BA and 30 (16.3%) assigned to MI, a significant difference by condition, χ2 (df=1) = 6.06, p = .014. To evaluate whether differential follow-up rates might bias interpretation of obtained outcomes, we compared the 45 with no follow ups to the 327 who completed one or more. On average, completers were older (M = 29.69, SD = 9.49) than non-completers (M = 25.60, SD = 6.65), t (df=71.34) = -3.64, p = .001. Hispanic patients were more likely to complete follow ups (96.23%) than non-Hispanic patients (86.5%), χ2 (df = 1) = 4.03, p = .045. Patients who completed no follow ups showed a trend toward being from Site 1 (15.1% of Site 1 patients vs. 8.7% of Site 2 patients, χ2 (df = 1) = 3.57, p = .059). No other demographic variable tested (including gender, race, education, employment, having health insurance, or income) differed by completion (all ps > .05). Importantly, follow-up completion was not significantly related to baseline values of any of our alcohol use or sex outcomes (all ps > .15).
Outcome Analyses
Descriptive data for all study outcomes (Ns and percentages, or means and standard deviations) at baseline and each follow up are presented separately for each treatment condition in Table 2. Detailed data from the GEE models for all alcohol use outcomes are presented in Table 3, and for all sex-risk outcomes in Table 4.
Table 2. Outcomes at Follow Up by Treatment Condition.
| Variable | BA N (%) or Mean (SD) | MI N (%) or Mean (SD) |
|---|---|---|
| No. Heavy Drinking Days | ||
| Baseline | 5.9 (6.8) | 5.8 (7.3) |
| 3MFU | 5.6 (6.4) | 3.8 (5.4) |
| 6MFU | 4.7 (6.3) | 3.8 (5.8) |
| 9MFU | 4.7 (6.7) | 3.7 (5.9) |
| Average no. drinks/Week | ||
| Baseline | 19.8 (43.3) | 14.3 (18.9) |
| 3MFU | 16.5 (28.1) | 9.1 (11.5) |
| 6MFU | 12.6 (17.9) | 9.2 (12.4) |
| 9MFU | 12.1 (17.6) | 8.4 (11.6) |
| CDC Excessive drinking | ||
| Baseline | 87 (46.3) | 68 (37.0) |
| 3MFU | 67 (41.6) | 39 (27.7) |
| 6MFU | 61 (36.7) | 36 (24.5) |
| 9MFU | 62 (37.8) | 34 (22.8) |
| FDA Heavy drinking | ||
| Baseline | 164 (87.2) | 158 (85.9) |
| 3MFU | 125 (77.6) | 100 (70.9) |
| 6MFU | 119 (71.7) | 108 (73.5) |
| 9MFU | 110 (67.1) | 91 (61.1) |
| SIP | ||
| Baseline | 6.0 (4.9) | 4.9 (4.4) |
| 3MFU | 4.3 (4.8) | 2.8 (3.9) |
| 6MFU | 3.6 (4.5) | 2.5 (3.7) |
| 9MFU | 3.1 (4.5) | 2.4 (3.9) |
| No. days Condomless Sex with Non-Steady partner | ||
| Baseline | 1.9 (5.0) | 2.6 (5.9) |
| 3MFU | 1.3 (4.0) | 0.8 (2.6) |
| 6MFU | 1.7 (4.9) | 0.7 (2.6) |
| 9MFU | 0.9 (3.3) | 0.7 (2.9) |
| Any Condomless Sex with Non-steady partner | ||
| Baseline | 60 (31.9) | 65 (35.3) |
| 3MFU | 41 (25.5) | 28 (19.9) |
| 6MFU | 42 (25.3) | 21 (14.3) |
| 9MFU | 29 (17.7) | 23 (15.4) |
| No. days Sex with Alcohol and/or Drugs | ||
| Baseline | 5.4 (7.1) | 4.7 (6.5) |
| 3MFU | 4.8 (6.1) | 3.2 (5.4) |
| 6MFU | 5.0 (7.0) | 3.0 (5.1) |
| 9MFU | 4.7 (6.9) | 2.8 (5.3) |
Note: n's for any group ranged from 161-166 (BA) and 141-149 (MI).
Table 3. SAS GEE Models Alcohol Outcomes.
| Dependent Variable | Predictor | Model coefficient | SE | Effect Size d/OR/IRR | 95% CI | p value |
|---|---|---|---|---|---|---|
| Number of heavy drinking days (NHDD)1 | ||||||
| Female (vs. male) | -0.349 | 0.109 | 0.706 | 0.570, 0.875 | 0.001 | |
| Baseline NHDD | 0.072 | 0.006 | 1.074 | 1.061, 1.088 | 0.000 | |
| Site 2 (vs. Site 1) | -0.299 | 0.111 | 0.741 | 0.597, 0.921 | 0.007 | |
| MI (vs. BA) | -0.234 | 0.114 | 0.791 | 0.633, 0.990 | 0.041 | |
| Time (Centered) | -0.094 | 0.046 | 0.91 | 0.833, 0.995 | 0.039 | |
| Time × MI int. | 0.102 | 0.094 | 1.107 | 0.921, 1.332 | 0.279 | |
| Log, Avg # drinks per week (LDKWK)2 | ||||||
| Female (vs. male) | -0.143 | 0.045 | -0.265 | -0.429, -0.100 | 0.002 | |
| Baseline LDKWK | 0.456 | 0.048 | 0.846 | 0.673, 1.018 | 0.000 | |
| Site 2 (vs. Site 1) | -0.074 | 0.044 | -0.138 | -0.299, 0.022 | 0.090 | |
| MI (vs. BA) | -0.090 | 0.044 | -0.167 | -0.328, -0.006 | 0.042 | |
| Time (Centered) | -0.065 | 0.020 | -0.120 | -0.193, -0.048 | 0.001 | |
| Time × MI int. | 0.018 | 0.029 | 0.034 | -0.072, 0.140 | 0.531 | |
| CDC Excessive drinking (CDC)3 | ||||||
| Female (vs. male) | -0.188 | 0.207 | 0.828 | 0.552, 1.243 | 0.363 | |
| Baseline CDC | 1.565 | 0.207 | 4.781 | 3.178, 7.171 | 0.000 | |
| Site 2 (vs. Site 1) | -0.588 | 0.204 | 0.555 | 0.372, 0.828 | 0.004 | |
| MI (vs. BA) | -0.604 | 0.209 | 0.547 | 0.363, 0.824 | 0.004 | |
| Time (Centered) | -0.071 | 0.100 | 0.931 | 0.766, 1.133 | 0.478 | |
| Time × MI int. | -0.089 | 0.154 | 0.915 | 0.677, 1.238 | 0.566 | |
| FDA Heavy drinking (FDA)3 | ||||||
| Female (vs. male) | -0.320 | 0.192 | 0.726 | 0.498, 1.059 | 0.096 | |
| Baseline NHDD | 1.048 | 0.268 | 2.853 | 1.688, 4.821 | 0.000 | |
| Site 2 (vs. Site 1) | -0.185 | 0.190 | 0.832 | 0.573, 1.207 | 0.332 | |
| MI (vs. BA) | -0.178 | 0.190 | 0.837 | 0.576, 1.215 | 0.350 | |
| Time (Centered) | -0.272 | 0.099 | 0.762 | 0.628, 0.924 | 0.006 | |
| Time × MI int. | 0.001 | 0.151 | 1.001 | 0.744, 1.347 | 0.994 | |
| Short Inventory of Problems (SIP)2 | ||||||
| Female (vs. male) | -0.265 | 0.334 | -0.062 | -0.214, 0.091 | 0.429 | |
| Baseline SIP | 0.480 | 0.045 | 0.112 | 0.092, 0.132 | 0.000 | |
| Site 2 (vs. Site 1) | -0.605 | 0.330 | -0.141 | -0.292, 0.010 | 0.067 | |
| MI (vs. BA) | -0.602 | 0.326 | -0.140 | -0.289, 0.009 | 0.065 | |
| Time (Centered) | -0.522 | 0.139 | -0.122 | -0.185, -0.058 | 0.000 | |
| Time × MI int. | 0.328 | 0.201 | 0.076 | -0.015, 0.168 | 0.103 | |
Count variable analyzed using negative binomial distribution; effect size is the incidence rate ratio.
Normally distributed variable; effect size is in standardized units of the dependent variable (d).
Dichotomous variable; effect size is expressed as an odds ratio.
Table 4. SAS GEE Models Sex Risk.
| Dependent Variable | Predictor | Model coefficient | SE | OR/IRR | 95% CI | p value |
|---|---|---|---|---|---|---|
| # Days with no condom used with non-steady partner (SEXRISK)1 | ||||||
| Female (vs. male) | -0.112 | 0.268 | 0.894 | 0.529, 1.511 | 0.675 | |
| Baseline SEXRISK | 1.691 | 0.260 | 5.422 | 3.261, 9.016 | 0.000 | |
| Site 2 (vs. Site 1) | 0.034 | 0.258 | 1.034 | 0.624, 1.716 | 0.896 | |
| MI (vs. BA) | -1.008 | 0.257 | 0.365 | 0.221, 0.604 | 0.000 | |
| Time (Centered) | -0.061 | 0.149 | 0.941 | 0.703, 1.259 | 0.681 | |
| Time × MI int. | 0.054 | 0.261 | 1.056 | 0.633, 1.761 | 0.835 | |
| Any sex without a condom with non-steady partner (ANYRISK)2 | ||||||
| Female (vs. male) | -0.088 | 0.209 | 0.916 | 0.608, 1.380 | 0.676 | |
| Baseline SEXRISK | 1.318 | 0.250 | 3.737 | 2.291, 6.096 | 0.000 | |
| Site 2 (vs. Site 1) | -0.015 | 0.207 | 0.985 | 0.657, 1.479 | 0.944 | |
| MI (vs. BA) | -0.522 | 0.209 | 0.594 | 0.394, 0.894 | 0.013 | |
| Time (Centered) | -0.233 | 0.118 | 0.792 | 0.628, 0.999 | 0.049 | |
| Time × MI int. | 0.079 | 0.199 | 1.082 | 0.732, 1.599 | 0.691 | |
| # sex days w/ alcohol or drugs (SUI DAYS)1 | ||||||
| Female (vs. male) | -0.319 | 0.153 | 0.727 | 0.539, 0.981 | 0.037 | |
| Baseline SUI DAYS | 1.100 | 0.174 | 3.005 | 2.135, 4.230 | 0.000 | |
| Site 2 (vs. Site 1) | 0.040 | 0.151 | 1.041 | 0.774, 1.401 | 0.791 | |
| MI (vs. BA) | -0.319 | 0.149 | 0.727 | 0.543, 0.974 | 0.033 | |
| Time (Centered) | 0.026 | 0.057 | 1.027 | 0.918, 1.148 | 0.644 | |
| Time × MI int. | -0.053 | 0.094 | 0.948 | 0.788, 1.141 | 0.573 | |
Note: Non-steady partner = A non-committed relationship, in which you had sex one or more times, and you have the understanding that your partner may have sex with other people.
Count variable analyzed using negative binomial distribution; effect size is the incidence rate ratio.
Dichotomous variable; effect size is expressed as an odds ratio.
Primary Alcohol Use Outcomes
Number of heavy drinking days
GEE analyses showed a significant main effect of treatment, favoring MI over BA, on number of heavy drinking days, such that those in MI reported about a 20% lower number of heavy drinking days across follow ups [IRR = 0.79, 95% confidence interval (CI): .63 to .99, p = 0.04]. A significant effect of time (IRR = 0.91, 95% CI: .83 to .995, p = 0.04) showed that overall, heavy drinking days decreased by about 10% over each follow-up period. There was no significant interaction between treatment condition and time, however, indicating that the effect of MI on reducing heavy drinking as compared to BA persisted throughout the 9-month follow-up period.
Average number of drinks consumed per week
Similarly, GEE analyses showed a significant effect of MI on the log-transformed number of drinks per week variable, such that those in MI reported consuming a lower average number of drinks per week as compared to BA at follow up with a small effect size (d = -0.17, 95% CI: -0.33 to -0.01, p = 0.04). The significant time effect (d = -0.12, 95% CI: -0.19 to -0.05, p = 0.001) indicated that overall weekly alcohol consumption decreased just over 1/10 of an SD each 3-month follow-up interval. The interaction between treatment condition and time was not significant, indicating that MI's effect on reducing drinks per week did not weaken over the course of follow up.
Secondary Alcohol Use Outcomes
Clinical benefit outcomes
We examined the effect of treatment condition on whether patients' drinking pattern would meet criteria for excessive drinking at follow up. GEE analyses showed a significant effect of treatment condition, such that those in MI were about half as likely as those in BA to report drinking above this threshold at follow up (OR = 0.55, 95% CI: 0.36 to 0.82, p = 0.004). No significant main effect of time or time × condition interaction effect were found for predicting this lower risk pattern of drinking. We then examined effect of treatment on whether patients' drinking would be classified as heavy, using the lower-threshold criteria of reporting any heavy drinking days at follow up. There was also a significant main effect of time indicating that the overall likelihood of engaging in heavy drinking decreased over follow up. However, there was no significant effect of treatment condition, and no significant time × condition interaction. A significant effect of time (d = -0.12, 95% CI: -0.18 to -0.06, p = 0.0002) reflected that, overall, alcohol-related problems decreased in frequency over the follow-up period. There was no significant interaction between condition and time.
Alcohol-related problems (SIP Score)
We examined whether those in MI experienced less frequent adverse consequences of alcohol use, as reported on the SIP, as compared to those in BA, across follow up. GEE showed the main effect of treatment on the SIP to be consistent with the pattern of effects favoring MI over BA, but did not reach significance (d = -0.14, 95% CI: -0.29 to -0.01, p = 0.06). A significant effect of time (d = -0.12, 95% CI: -0.18 to -0.06, p = 0.0002) reflected that, overall, alcohol-related problems decreased in frequency over the follow up. There was no significant interaction between treatment condition and time.
Sex Risk Primary Outcomes
Frequency of condomless sex with non-steady partners
GEE analyses showed a significant main effect of treatment on our primary sex-risk outcome, such that those in MI reported fewer days on which they engaged in condomless sex with casual partners, compared to those in BA (IRR = 0.37, 95% CI: 0.22 to 0.60, p = 0.0001). There was no significant effect of time and no interaction between treatment condition and time.
Any condomless sex with non-steady partners
Similarly, we examined the effect of treatment condition on whether patients reported any risky sex (i.e., condomless sex with non-steady partners) in the month preceding each follow up. GEE showed a significant effect of treatment condition on reducing risky sex, such that those in MI had a more than 40% lower odds of engaging in any condomless sex with non-steady partners during follow up compared to those in BA (OR = 0.59, 95% CI: .39 to .89, p = 0.013). There was also a significant main effect of time indicating that the overall likelihood of engaging in risky sex decreased over the 9 months of follow up. There was no significant time × condition interaction.
Sex Risk Secondary Outcome
Sex under the influence of alcohol and/or drug use
Finally, we explored whether MI would reduce number of days on which patients reported engaging in vaginal or anal sex while under the influence of alcohol or other drugs. GEE analyses showed a significant effect of condition, such that those in MI reported fewer days on which they engaged in sex under the influence of alcohol/drugs during follow up compared to those in BA (IRR = 0.72, 95% CI: .54 to .97, p = 0.01). The effect of time was nonsignificant, as was the condition by time interaction.
Discussion
The purpose of this study was to evaluate the effects of a brief MI as compared to BA when targeting both risky alcohol use and risky sexual behavior in an ED population. Results offered strong support for our modified brief intervention. Both heavy drinking and risky sexual behavior showed significant reductions that persisted throughout the 9-month follow-up period. Findings on both risky alcohol use and risky sexual behavior are particularly impactful as they result from a relatively innovative brief MI targeting both behaviors. Reviews of the “twin epidemics” of alcohol and HIV have called for empirically supported interventions that address these co-occurring health outcomes, and that can be delivered in settings where high-risk individuals are likely to be reached (Edelman et al., 2012; Kalichman et al., 2007; Schneider et al., 2012). In the United States, ED settings frequently serve as a safety net and entry point into health care (Schuur & Venkatesh, 2012), thereby providing a context for reaching diverse populations with possible risk for HIV and alcohol disorders. This study suggests a brief MI can efficaciously reduce risk for both targeted behaviors. Furthermore, our results across two separate community hospital EDs enhance the likely generalizability of these findings.
Importantly, reductions in alcohol use outcomes were evidenced across several key outcome variables including number of heavy drinking days and average number of drinks per week. In addition, we examined two meaningful clinical endpoints. The first was whether patients' overall drinking pattern met commonly used criteria for excessive drinking. Results showed those receiving MI were less likely than those receiving BA to engage in excessive drinking. The second endpoint, avoidance of heavy drinking entirely, has recently been suggested by the FDA as a clinical endpoint in alcohol trials. Patients had more difficulty overall achieving this outcome, and MI did not significantly increase the odds of doing so.
Next we examined whether those receiving MI experienced less frequent adverse consequences of alcohol use, as reported on the SIP, when compared to those in BA. Main effect of treatment on the SIP was consistent with the above pattern of effects favoring MI over BA, though somewhat less robust. Findings on alcohol consequences proving to be somewhat less robust than those on drinking per se provide opportunity to further intervene with an extended intervention in future work, as this has proven fruitful with respect to impacting alcohol-related consequences in other ED alcohol interventions (e.g., Monti et al., 2007). Importantly, our findings on drinking and adverse consequences are consistent with those of patterns found in previous work and suggest that the MI effect on alcohol use was not significantly compromised when integrated with a focus on risky sexual behavior, even though our multi-risk brief intervention was approximately of the same duration as many alcohol only MIs.
Results on sex risk paralleled those for alcohol. Our primary sex-risk outcome, frequency of condomless sex with a non-steady partner, showed those receiving MI reported fewer days on which they engaged in condomless sex with casual partners, compared to BA. Reductions in condomless sex with casual partners is particularly noteworthy in light of the risk for transmission of HIV and other sexually transmitted infections with casual partners (Gorbach & Holmes, 2003; Parsons et al., 2005). We found similar results when examining whether patients reported any condomless sex with a non-steady partner in the month preceding follow ups.
Finally, we examined whether MI would reduce the number of days on which patients reported engaging in vaginal or anal sex while under the influence of alcohol or other drugs during follow up, as alcohol and other drug use before or during sex has been linked with risk for HIV and other sexually transmitted infections (Hendershot & George, 2007; Woolf et al., 2009). Again we found a significant effect of treatment such that those receiving MI reported fewer days on which they engaged in sex under the influence, as compared to those receiving BA.
While the results of our dual-focused MI are encouraging, greater expense is associated with administering MI compared with administering BA. A cost effectiveness analysis would be needed to determine whether the additional burden is worth the greater effect. While such an analysis was beyond the scope of the present study, earlier intervention studies in various ED settings have proven to be cost effective when targeting alcohol risk alone (e.g., Neighbors et al., 2010). Given that our dual-focused intervention took no more intervention time or effort than most alcohol MIs, and considering the economic burden of sexually transmitted diseases (Chesson et al., 2011), it is likely that our dual-focused intervention will prove to be cost effective. This will be the focus of a future report.
A notable strength of this study was its relatively large sample size and respectable follow-up rates. While we found some differential follow up such that more patients were followed up in BA than MI, importantly, follow up completion was not related to baseline values of any of our alcohol or sex risk outcomes. Our relatively large sample should enable examination of mediators and moderators of our treatment effects – a logical next step in our program of ED intervention research given the emergence of such effects in previous work (e.g., Barnett et al., 2010). Another strength of the study is related to the fact that the study was conducted across two community hospitals and not at a large university-affiliated teaching hospital. Among patients assigned to treatment, comparisons of those who did versus did not receive MI showed the two groups did not differ by site. Working in community hospitals poses certain challenges including that they tend not to do much research and have fewer resources. However, the scalability of our interventions depends on its feasibility in non-academic medical centers where most of the patients in the United States are seen for their medical care. Indeed, there is a growing focus on developing HIV prevention and other public health intervention programs that can be delivered in community settings (Norton et al., 2009), and findings from this brief and relatively low-resource intervention offer a promising foundation for implementation into community practice.
An initial concern when implementing this study was to insure that therapists would maintain intervention fidelity with addition of the second focus of sexual risk behaviors. As indicated by the intervention integrity evaluation, therapists showed MISC Global scores above the accepted threshold for successful delivery of MI. The combination of the MI skill delivery and the receptivity of patients to this combined intervention supports its value.
Limitations
While patients in this study reported maintenance of treatment gains in the areas of both alcohol and sexual risk behaviors through the follow-up period, results should be interpreted in light of the study's limitations. The study did not include an assessment-only control, and therefore the efficacy of the BA condition is not known.
Another limitation is that the sample was predominately Caucasian, so replication of these findings in more diverse samples is necessary. However, the fact that MI performed similarly in two EDs with different demographic profiles suggests that the intervention is promising in its ability to be applied to different socio-demographic groups. In addition, the results relied on self-report recall which might be prone to bias and the study had no biomarkers of alcohol use or sex-risk behaviors. However, many studies have supported the reliability and validity of self-report data on alcohol use (Sobell & Sobell, 2003) and on sexual behavior as well (Carey, Carey & Maisto, 2001). Future studies should consider using biomarkers and perhaps experience sampling techniques so as to minimize bias (Wray, Merrill & Monti, 2014). Such event sampling would also provide additional precision as to how much alcohol consumption preceded sexual behavior on a given occasion, enabling analyses that could further our understanding of the alcohol/risky sexual behavior link.
Finally, the use of research staff as interventionists should be considered a limitation. A worthy goal from a dissemination perspective is to have ED staff conduct such interventions. However, complexities stemming from this multiple behavior intervention and the state-of-the science, precluded our use of ED staff as interventionists.
In sum, findings provide evidence to support the feasibility and efficacy of a brief, theory-based intervention to reduce alcohol and sex risk behavior in an ED. Effects were observed on key alcohol and sex behaviors proximally linked with HIV and other sexually transmitted infections. Successful delivery of this MI in situ, while other urgent ED services were being delivered, provides support for its scalability in complex health settings where newly insured high-risk individuals are increasingly likely to seek care (Taubman et al., 2014).
Acknowledgments
NIH Grant Funding: 2R01 AA009892, K05 AA019681
Contributor Information
Peter M. Monti, Email: Peter_Monti@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-5, Providence, RI 02912, Phone: 401 863-6661, Fax: 401 863-6697.
Nadine R. Mastroleo, Email: Nadine_Mastroleo@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-5, Providence, RI 02912, Phone: 401 863-6624, Fax: 401 863-6697.
Nancy P. Barnett, Email: Nancy_Barnett@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-5, Providence, RI 02912, Phone: 401 863-6649, Fax: 401 863-6697.
Suzanne M. Colby, Email: Suzanne_Colby@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-4, Providence, RI 02912, Phone: 401 863-6655, Fax: 401 863-6647.
Christopher W. Kahler, Email: Christopher_Kahler@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-4, Providence, RI 02912, Phone: 401 863-6651, Fax: 401 863-6647.
Don Operario, Email: Don_Operario@brown.edu, Brown University, Center for Alcohol and Addiction Studies, Box G-S121-4, Providence, RI 02912, Phone: 401 863-6657, Fax: 401 863-6647.
Literature cited
- Babor TF, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No Ordinary Commodity—Research and Public Policy. Oxford, UK: Oxford University Press; 2010. [Google Scholar]
- Barnett N, Apodaca T, Magill M, Colby S, Gwaltney C, Rohsenow D, Monti PM. Moderators and mediators of two brief interventions for alcohol in the Emergency Department. Addiction. 2010;105:452–465. doi: 10.1111/j.1360-0443.2009.02814.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Ashong D, Heeren T, Winter M, Bliss C, Madico G, Bernstein J. The impact of a Brief Motivational Intervention on unprotected sex and sex while high among drug-positive Emergency Departments who receive STI/HIV VD/T and drug treatment referral as standard of care. AIDS and Behavior. 2012;16(5):1203–1216. doi: 10.1007/s10461-012-0134-0. [DOI] [PubMed] [Google Scholar]
- Borsari B, Hustad JTP, Mastroleo NR, Tevyaw TO, Barnett NP, Kahler CW, et al. Monti PM. Alcohol use and problems in mandated college students: A randomized clinical trial using stepped care. Journal of Consulting and Clinical Psychology. 2012;80:1062–1074. doi: 10.1037/a0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the US, 2006. American Journal of Preventive Medicine. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA. Assessing sexual risk behavior with the timeline followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. International Journal of STD and AIDS. 2001;12(6):365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y. Trends in Alcohol-and Drug-Related Emergency Department and Primary Care Visits: Data From Four US National Surveys (1995–2010) Journal of Studies on Alcohol and Drugs. 2012;73(3):454–458. doi: 10.15288/jsad.2012.73.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesson HW, Gift TL, Owusu-Edusei K, Jr, Tao G, Johnson AP, Kent CK. A brief review of the estimated economic burden of sexually transmitted diseases in the United States: inflation-adjusted updates of previously published cost studies. Sexually Transmitted Diseases. 2011;38:889–891. doi: 10.1097/OLQ.0b013e318223be77. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6:284–290. [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86(2-3):214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cut-off score. Addiction. 1995;90(10):1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. [DOI] [PubMed] [Google Scholar]
- Edelman EJ, Dinh A, Radulescu R, Lurie B, D'Onofrio G, Tetrault JM, et al. Fiellin LE. Combining rapid HIV testing and a brief alcohol intervention in young unhealthy drinkers in the emergency department: a pilot study. American Journal of Drug and Alcohol Abuse. 2012;38(6):539–543. doi: 10.3109/00952990.2012.701359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS. Prevalence of alcohol dependence among US adult drinkers, 2009–2011. Preventing Chronic Disease. 2014;11 doi: 10.5888/pcd11.140329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinn R, Tennen H, Kranzler HR. Psychometric properties of the Short Index of Problems as a measure of recent alcohol‐related problems. Alcoholism: Clinical and Experimental Research. 2003;27(9):1436–1441. doi: 10.1097/01.ALC.0000087582.44674.AF. [DOI] [PubMed] [Google Scholar]
- Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376(9739):398–400. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbach PM, Holmes KK. Transmission of STIs/HIV at the partnership level: beyond individual-level analyses. Journal of Urban Health. 2003;80:iii15–iii25. doi: 10.1093/jurban/jtg079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. Journal of Adolescent Health. 1996;19(5):331–336. doi: 10.1016/S1054-139X(96)00024-9. [DOI] [PubMed] [Google Scholar]
- Hendershot CS, George WH. Alcohol and sexuality research in the AIDS era: trends in publication activity, target populations and research design. AIDS and Behavior. 2007;11(2):217–226. doi: 10.1007/s10461-006-9130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houck JM, Moyers TB, Miller WR, Glynn LH, Hallgren KA. Motivational Interviewing Skill Code (MISC) version 2.5. 2010 Available from http://casaa.unm.edu/download/misc25.pdf.
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prevention Science. 2007;8(2):141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Tannenbaum L, Nachimson D. Personality and cognitive factors influencing substance use and sexual risk for HIV infection among gay and bisexual men. Psychology of Addictive Behaviors. 1998;12(4):262–271. [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, Rollnick S. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling. 2013;93:157–168. doi: 10.1016/j.pec.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Mastroleo NR, Operario D, Barnett NP, Colby SM, Kahler CW, Monti PM. Prevalence of Heavy Drinking and Risky Sexual Behaviors in Adult Emergency Department Patients. Alcoholism: Clinical and Experimental Research. 2015;39(10):1997–2002. doi: 10.1111/acer.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences DrInC: An instrument for assessing adverse consequences of alcohol abuse. Albuquerque, NM: Center on Alcoholism, Substance Abuse and Addictions; 1995. [Google Scholar]
- Millstein SG, Moscicki A. Sexually-transmitted disease in female adolescents: Effects of psychological factors and high risk behaviors. Journal of Adolescent Health. 1995;17(2):83–90. doi: 10.1016/1054-139X(95)00065-Z. [DOI] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, Woolard R. Motivational interviewing vs. feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA Council approves definition of binge drinking. Vol. 3. NIAAA Newsletter; 2004. p. 3. [Google Scholar]
- Neighbors CJ, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. Journal of Studies on Alcohol and Drugs. 2010;71(3):384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton WE, Amico KR, Cornman DH, Fisher WA, Fisher JD. An agenda for advancing the science of implementation of evidence-based HIV prevention interventions. AIDS and Behavior. 2009;13(3):424–429. doi: 10.1007/s10461-009-9556-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Schrimshaw EW, Bimbi DS, Wolitski RJ, Gómez CA, Halkitis PN. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005;19:S87–S97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107(1):51–59. doi: 10.1111/j.1360-0443.2011.03621.x. [DOI] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): A review of recent research. Alcoholism: Clinical and Experimental Research. 2002;26(2):272–279. [PubMed] [Google Scholar]
- Rothman RE. Current Centers for Disease Control and Prevention guidelines for HIV counseling, testing, and referral: critical role of and a call to action for emergency physicians. Annals of Emergency Medicine. 2004;44(1):31–42. doi: 10.1016/j.annemergmed.2004.01.016. [DOI] [PubMed] [Google Scholar]
- Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, et al. Ostrow DG. Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS. 2013;27(5):815–823. doi: 10.1097/QAD.0b013e32835cff4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M, Chersich M, Neuman M, Parry C. Alcohol consumption and HIV/AIDS: the neglected interface. Addiction. 2012;107(8):1369–1371. doi: 10.1111/j.1360-0443.2012.03824.x. [DOI] [PubMed] [Google Scholar]
- Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. New England Journal of Medicine. 2012;367(5):391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS-a systematic review. Alcohol Alcohol. 2010;45(2):159–166. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson V, editors. Assessing Alcohol Problems. 2nd. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. pp. 78–99. [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students' recent drinking history: Utility for alcohol research. Addictive Behaviors. 1986;11(2):149–162. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997-2007. Journal of the American Medical Association. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon's Health Insurance Experiment. Science. 2014;343(6168):263–268. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Food and Drug Administration/Center for Drug Evaluation and Research. Alcoholism: Developing Drugs for Treatment Guidance for Industry: FDA draft guidance document. Washington, DC: U.S. Department of Health and Human Services: FDA/CDER; 2015. Feb, [Google Scholar]
- Woolf SE, Maisto SE. Alcohol use and risk of HIV infection among men who have sex with men. AIDS and Behavior. 2009;13(4):757–782. doi: 10.1007/s10461-007-9354-0. [DOI] [PubMed] [Google Scholar]
- Wray TB, Grin B, Dorfman L, Glynn TR, Kahler CW, Marshall BD, et al. Operario D. Systematic review of interventions to reduce problematic alcohol use in men who have sex with men. Drug and alcohol review. 2015 doi: 10.1111/dar.12271. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray T, Merrill J, Monti PM. Using Ecological Momentary Assessment (EMA) to assess situation-level risk factors for heavy drinking and alcohol-related consequences. Alcohol Research: Current Reviews. 2014;36(1):19–27. [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–30. [PubMed] [Google Scholar]


