Abstract
Ultrasound-guided thrombin injection has been well described as a safe and effective treatment for pseudoaneurysms of the femoral artery. However, cases for subclavian artery pseudoaneurysm are rare. An 82-year-old man developed an iatrogenic right subclavian artery pseudoaneurysm. The pseudoaneurysm, which was partially thrombosed, was successfully treated by ultrasound-guided percutaneous thrombin injection. A trial injection with saline under color Doppler ultrasonography was helpful for confirming that the tip of the needle was in the sac with blood flow in the partially thrombosed pseudoaneurysm. Ultrasound-guided thrombin injection can be the first treatment of choice to treat subclavian artery pseudoaneurysm.
Keywords: subclavian artery pseudoaneurysm, thrombin injection
Introduction
An uncommon complication associated with central venous access is development of a pseudoaneurysm after inadvertent puncture of the artery. Subclavian artery pseudoaneurysms were historically treated by open surgical repair, but this can be associated with significant morbidity. Recent literature has describes less invasive techniques of treating subclavian artery pseudoaneurysms, such as thrombin injection1) or endovascular repair.2,3) We report a case of an iatrogenic subclavian artery pseudoaneurysm, which was formed secondary to incorrect central venous catheter insertion, and was successfully treated by ultrasound-guided thrombin injection.
Case Report
An 82-year-old man had a history of graft replacement for abdominal arterial aneurysm via a midline abdominal incision and total aortic arch replacement for thoracic arterial aneurysm via median sternotomy. He was diagnosed with postoperative abdominal aortic pseudoaneurysm at the anastomosis site of graft replacement, and it was treated by endovascular aortic aneurysm repair. In the operation, a central venous catheter was inserted into the right jugular vein. At this time, the adjacent artery was inadvertently punctured and local pressure was applied to the puncture site to achieve hemostasis. The patient complained of worsening right neck pain from postoperative day 9, but we initially thought that the pain was orthopedic, and simply observed. On postoperative day 11, a computed tomography was performed to evaluate the site of the treated abdominal aneurysm. This showed a 39-mm-diameter pseudoaneurysm superior to the right subclavian artery in the neck. On physical examination, a pulsatile hematoma was noted in the patient’s right neck just superior to the clavicle. Therefore, the patient’s pain was considered to be due to the mass effect of the pseudoaneurysm. An ultrasound examination showed an aneurysm arising from the subclavian artery. Color Doppler ultrasonography revealed that the neck of the aneurysm originated from the subclavian artery and was approximately 3 mm wide. Additionally, part of the aneurysm was thrombosed and blood flow had entered part of the aneurysm (Fig. 1). Magnetic resonance angiography showed that the pseudoaneurysm originated from the right subclavian artery just proximal to the vertebral artery and the vertebral artery was right-side dominant. First, compression repair, including ultrasound-guided compression repair, was performed, but failed to treat the pseudoaneurysm. Consequently, percutaneous injection of thrombin into the aneurysm was performed on postoperative day 14. The area was prepped and draped in a sterile fashion bovine thrombin at a concentration of 1000 U/ml in a 1-ml syringe and saline in another 1-ml syringe were attached to a T-shaped stopcock with a 22-gauge spinal needle. After local anesthesia, under non-color Doppler ultrasound guidance, a 22-gauge needle tip was passed into the pseudoaneurysm away from its neck. A trial injection with saline under color Doppler ultrasonography was then performed. This confirmed that the saline was going to be injected into the non-thrombosed site of the pseudoaneurysm because injected saline caused swirling flow in the aneurysm as observed by ultrasound. Subsequently, thrombin was injected into the sac at the speed of 0.1 ml/s or slower until complete thrombosis in the pseudoaneurysm was confirmed with color Doppler ultrasonography (Fig. 2). As a result, 400 units of thrombin were injected. Ultrasonography also showed a patent subclavian artery and vertebral artery. The patient’s symptom of neck pain improved immediately, and ultrasonography 6 months after thrombin injection showed no evidence of pseudoaneurysm in the subclavian artery (Fig. 3).
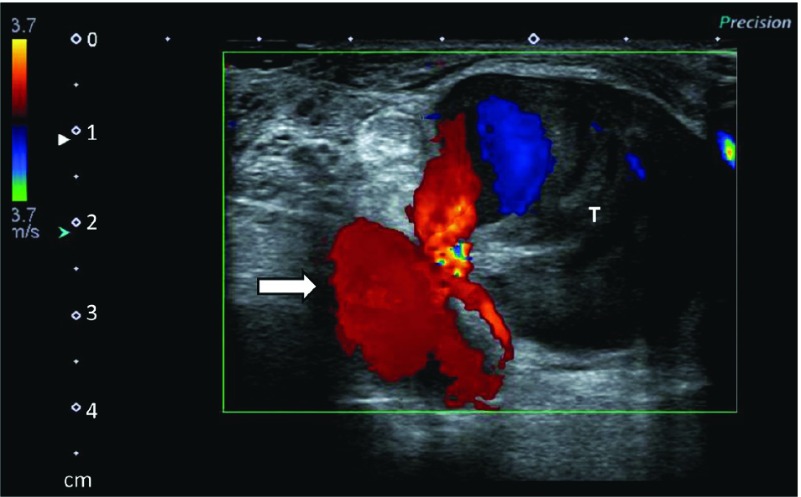
Fig. 1.
Ultrasonography before thrombin injection showing a pseudoaneurysm originating from the subclavian artery (arrow). The pseudoaneurysm is partially thrombosed (T) and blood flow can be seen in part of the pseudoaneurysm.
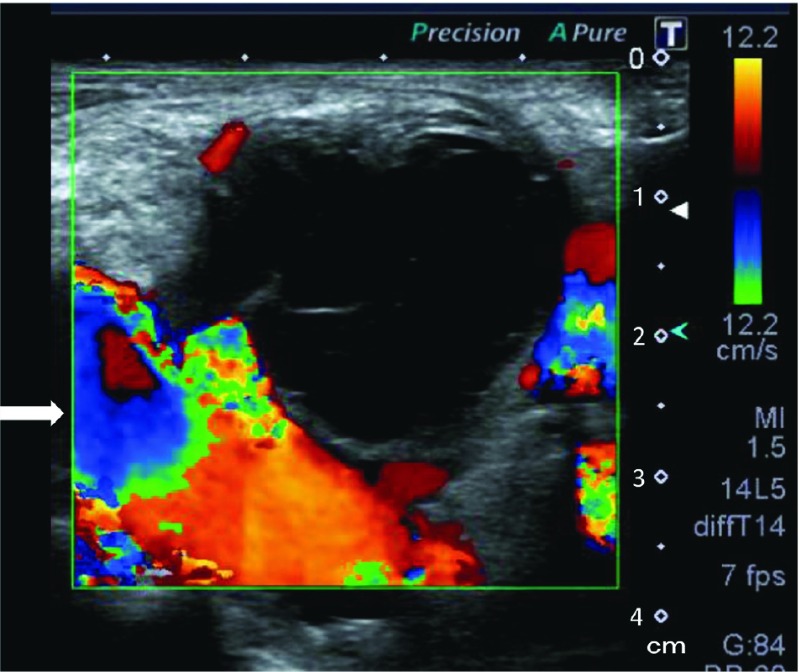
Fig. 2.
Ultrasonography just after thrombin injection showing absence of flow within the pseudoaneurysm and a patent subclavian artery (arrow).
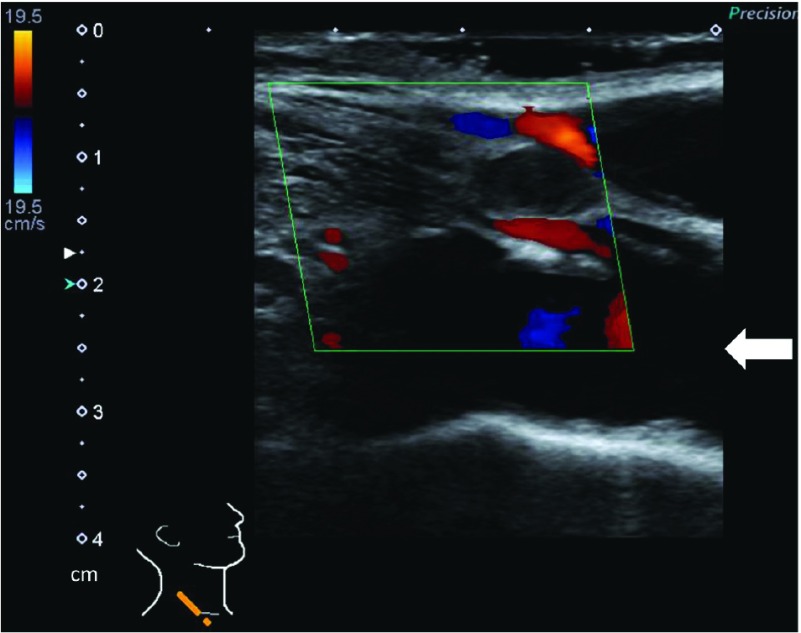
Fig. 3.
Ultrasonography 6 months after thrombin injection showing no evidence of pseudoaneurysm in the right subclavian artery (arrow).
Discussion
A rare, but potentially serious, complication of central line catheter insertion is development of a pseudoaneurysm of the subclavian artery after inadvertent puncture of the artery. Treatment options include ultrasound-guided compression repair, ultrasound-guided thrombin injection, endovascular repair, and open surgical repair. Ultrasound-guided compression is usually unsuitable for subclavian artery pseudoaneurysms, such as in the present case, because of the close proximity of the clavicle, which makes it difficult to compress the subclavian artery. Surgical repair of subclavian artery pseudoaneurysm can be associated with significant morbidity because it often requires thoracotomy to obtain proximal control of the artery. Our patient had a history of median sternotomy and this was expected to be more challenging to examine the proximal artery because of adhesion. Endovascular repair might be effective in this situation.2,3) However, attempts at stenting the subclavian artery could occlude the close right vertebral artery or even lead to cerebral ischemia, especially because our patient’s vertebral artery was right-dominant. Therefore, we selected ultrasound-guided thrombin injection, which is less invasive, to treat the subclavian artery pseudoaneurysm. Ultrasound-guided thrombin injection is a safe and effective treatment for pseudoaneurysms of the femoral artery.4–6) However, reports of thrombin injection that involve the subclavian artery are rare.1,6,7) A potential complication of thrombin injection includes thromboembolic complications, but this is infrequent. Krueger et al.4) reported only two thromboembolic complications in 240 patients when treating post-catheterization pseudoaneurysms. They considered that the reason for the complications was that thrombin was directly injected into the native artery or the pseudoaneurysm neck. Therefore, care must be taken in thrombin injection therapy in that the tip of the needle should be in the pseudoaneurysm away enough from the neck and the amount of thrombin should be small enough not to accidentally be injected into the native artery. The center of the pseudoaneurysm appears to be first of choice of injection because of easy access and a low risk of thromboembolic complications.5,7) However, in our case, the pseudoaneurysm was partially thrombosed. In this situation, injecting thrombin accurately into the non-thrombosed site of the aneurysm is challenging. Only confirmation of blood backflow or imaging of the needle tip by ultrasonography potentially has a risk of direct injection into the native artery. Describing the accurate location of the needle tip on ultrasound is sometimes difficult. Therefore, in our case, after revealing the tip of the needle in the aneurysm under non-color Doppler ultrasonography, a trial injection with saline under color Doppler ultrasonography was performed. This caused swirling flow in the pseudoaneurysm and confirmed that the saline would be injected into the non-thrombosed site in the pseudoaneurysm. In the present case, subclavian artery pseudoaneurysm was successfully treated by thrombin injection; however, if it had failed, another strategy would have been necessary. Options include endovascular repair such as stent-grafting2) and open surgery. If stenting to the subclavian artery requires coverage of the vertebral artery, a preoperative balloon occlusion test of the vertebral artery can be performed, and if it is positive, reconstruction of the vertebral artery8) followed by stenting to the subclavian artery is taken into consideration.
Conclusion
We report a case of successful treatment of iatrogenic subclavian artery pseudoaneurysm by ultrasound-guided thrombin injection. Ultrasound-guided thrombin injection is a minimally invasive, safe, and effective technique, and can be the first treatment of choice to treat subclavian artery pseudoaneurysms.
Disclosure Statement
All authors have no conflict of interest.
Authors’ Contributions
Study conception: YY
Data collection: YY, SK
Investigation: YY, KK, YU
Writing: YY
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).McConnell PI, Rehm J, Oltman DL, et al. Thrombin injection for treating a subclavian artery pseudoaneurysm. Surgery 2000; 127: 716-8. [DOI] [PubMed] [Google Scholar]
- 2).Yamagami T, Yoshimatsu R, Tanaka O, et al. A case of iatrogenic subclavian artery injury successfully treated with endovascular procedures. Ann Vasc Dis 2011; 4: 53-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Watelet J, Clavier E, Reix T, et al. Traumatic subclavian artery pseudoaneurysm: periprocedural salvage of failed stent-graft exclusion using coil embolization. J Endovasc Ther 2001; 8: 197-201. [DOI] [PubMed] [Google Scholar]
- 4).Krueger K, Zaehringer M, Strohe D, et al. Postcatheterization pseudoaneurysm: results of US-guided percutaneous thrombin injection in 240 patients. Radiology 2005; 236: 1104-10. [DOI] [PubMed] [Google Scholar]
- 5).Kuma S, Morisaki K, Kodama A, et al. Ultrasound-guided percutaneous thrombin injection for post-catheterization pseudoaneurysm. Circ J 2015; 79: 1277-81. [DOI] [PubMed] [Google Scholar]
- 6).Kang SS, Labropoulos N, Mansour MA, et al. Expanded indications for ultrasound-guided thrombin injection of pseudoaneurysms. J Vasc Surg 2000; 31: 289-98. [DOI] [PubMed] [Google Scholar]
- 7).Lee GS, Brawley J, Hung R. Complex subclavian artery pseudoaneurysm causing failure of endovascular stent repair with salvage by percutaneous thrombin injection. J Vasc Surg 2010; 52: 1058-60. [DOI] [PubMed] [Google Scholar]
- 8).Kakino S, Ogasawara K, Kubo Y, et al. Symptomatic occlusion at the origin of the vertebral artery treated using external carotid artery-cervical vertebral artery bypass with interposed saphenous vein graft. Surg Neurol 2008; 69: 164-8; discussion 168. [DOI] [PubMed] [Google Scholar]