Abstract
Purpose
Locking compression plates (LCP) allow trauma and orthopedic surgeons to have a variety of options for utilizing locking and non-locking screw features. In this study, the hybrid constructs of mixed unicortical and bicortical screws were investigated for humerus midshaft fractures. The locking and non-locking features were also incorporated into the hybrid LCP constructs. Kryptonite™ bone cement is biocompatible with low exothermic properties and strong metal adhesion. This novel bone cement was incorporated into the non-locking screw feature to compare its mechanical effect with that of a traditional locking screw feature.
Methods
A total of 24 synthetic bones (Sawbones® Inc., USA) were equally divided into three groups (n = 8). The control group obtained traditional LCP fixation (JSM Medimax Inc., India) with bicortical screws, while the hybrid locking constructs employed a mix of bicortical and unicortical screws. The two bicortical screws in hybrid constructs were placed at the end holes of the LCP constructs and the unicortical screws were placed into the remaining holes. The hybrid locking (HL) group contained locking unicortical screws, whereas the hybrid non-locking group (HNK) utilized non-locking screw features incorporating the Kryptonite™ bone cement in the plate/screw bone construct. Specimens were tested by dynamic and static analysis. The eight total constructs were equally divided into two subgroups (n = 4) to conduct axial compression and torsion test individually. The low cyclic test was conducted for dynamic analysis, which included 10,000 cycles at 1 Hz frequency with a cyclic loading of 0–500 N of axial force for the axial compression test and 0–20° of angular displacement for the torsion test. The static analysis was run by a failure test with a nondestructive strain rate of 0.1 mm/s for the axial compression test and 0.5° s−1 for the torsional test. The construct stiffness of axial compression and torsion were derived from the linear portion of the load-displacement curves. The yield strength of axial compression and torsion was determined by using offset methods. The results of stiffness and yield strength were compared by using both one-way ANOVA and Scheffe and Games-Howell post hoc tests to analyze statically significant differences among the three groups.
Results
Specimens completed 10,000 cycles in the dynamic analysis of axial and torsional cyclic tests without major deformation. To compare with the control group in static analysis, the HL and HNK groups achieved positive effect in axial stiffness, 12.3% and 10.5% greater than the control group respectively. HL obtained axial yield strength about 12% less than the control group. The HNK group was equivalent with the control group in axial yield strength. The torsional stiffness and yield strength were found similar in three groups, which indicated torsional equivalence among them. The stiffness and yield strength from axial compression and torsion were found statically non-significant among three groups.
Conclusions
Hybrid LCP constructs were initially showed to maintain equivalent axial and torsional stability with the traditional method. Kryptonite™ hosted mechanical and biological advantages for internal plate/screws (PLT) fixation.
Keywords: Internal bone fixation, PLT, LCP, Unicortical vs. bicortical screw, Locking vs. non-locking screw, Kryptonite™ bone cement
1. Introduction
Internal fixation with plate/screws (PLT) is a commonly elected treatment for displaced humeral shaft fractures. The PLT technique enables functional range of motion both the shoulder and elbow joints, while the fracture heal and thereby help to avoid joint stiffness and muscle atrophy.1 Locking compression plate (LCP) design maintains limited contact with the bone surface to preserve the periosteal membrane and helps to preserve periosteal blood flow, which promotes bone healing.2, 3, 10 The unique LCP design also creates a versatile opportunity to combine both locking and non-locking screws in the plate construct. The non-locking screw configuration permits a direct compression of the plate against the bone surface thereby closing fracture gap and achieving fracture compression. The locking screw is inserted perpendicular to the plate to help transfer axial load along the length of the plate.4 The locking screw head is locked in the bone plate, which significantly improves fixation in osteoporotic bone to prevent screw togging and micro-motion between screw and bone plate, but it is limited in comminuted fracture, since the locking screw is only allowed 5° or less angle deviation with screw insertion.2, 5 The non-locking screw is an alternative to the locking screw, because it can be inserted with a variety of angles, and when supplemented with appropriate bone cement, it may retain some of the beneficial features of the locking construct. Poly-methyl-methacrylate (PMMA) bone cement is approved for orthopedic surgery and has been used to enhance the fixation of plate construct in osteoporotic bone. Currently, an innovative bone cement, Kryptonite™ bone cement (Doctors Research Group Inc., Southbury, CT), is approved by FDA as a biocompatibility product for repairing cranial defect and sternal closure in cardiothoracic surgery.6 To compare with the PMMA bone cement, Kryptonite™ bone cement obtains feasible biological and mechanical properties, which are advantage in orthopedic fracture fixation. This bone cement has a low exothermic curing process (approximately 43 °C vs. about 90 °C for PMMA) and thereby avoids local tissue and bone necrosis.7 With a similar porous microstructure to PMMA bone cement, Kryptonite™ bone cement can stimulate bone growth and has a potential of integrating with intact bone tissue. Kryptonite™ bone cement exhibits equal axial yield-strength to PMMA, which is about 1200 N, and it has identical stiffness with an intact bone, which is approximately 800 MPa.8 In axial compression, Kryptonite™ bone cement demonstrates high toughness and failure strain to resist axial deformation. Kryptonite™ bone cement employs a strong metal adhesion, which is five times greater than PMMA. With its strong metal adhesive characteristic Kryptonite™ bone cement becomes attractive option in orthopedic application. Kryptonite™ bone cement could serve as an interface between bone plate and the bone, thus it is neglecting the need for additional screws.6, 8, 9 Studies of Kryptonite™ bone cement in fracture fixation are few, and the effects of the bone cement as a bonding interface between plate and screw has not been established to improve PLT technique in case of bone osteoporosis with comminuted fracture. A hybrid PLT construct is possibly achieved by mixing unicortical and bicortical screws in the fixation construct, which is considered a less invasive procedure for the patient.9 Roberts et al. in 2007 proved that hybrid screw fixation mechanically behaves as strong as traditional fixation, which employs all bicortical screws. The diversity of screw combinations in LCP constructs, therefore, creates an uncertainty for the mechanical behavior of the constructed implants in vivo.
This study investigates the effect of Kryptonite™ bone cement in internal long bone fixation, specifically the PLT technique in humerus diaphyseal fracture. Hybrid LCP constructs containing mixed unicortical and bicortical screws were used to biomechanically compare to the traditional method. Moreover, a combination of locking and non-locking screws was also incorporated in the hybrid constructs to compare the combination of non-locking screw adding Kryptonite™ bone cement (bicortical and unicortical) vs. locking screw (bicortical vs. unicortical). The ultimate goal of this study is to explore variety of screw options in LCP constructs to produce a less invasive PLT procedure, which is still able to maintain equivalent strength and stiffness for bone proliferation and healing.
2. Materials and methods
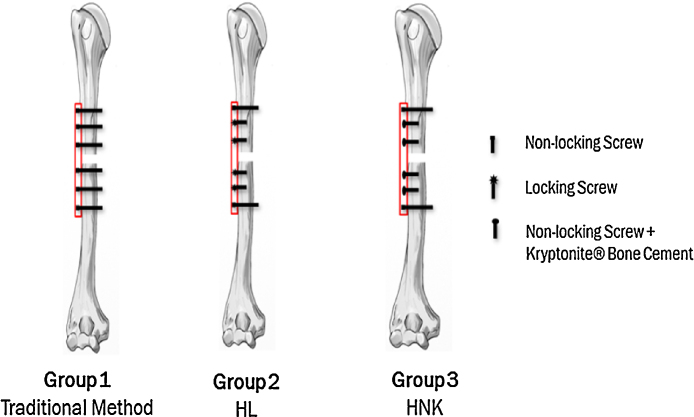
A total of 24 synthetic humerus specimens (Plastic cortical shell, Sawbones® Company, USA) were obtained. To conduct a study the specimens were divided into three groups (n = 8). All groups were fixed with 7-hole 3.5 mm LCP plates (JSM Medimax INC., India). The LCP plate was placed on the anterolateral surface of the humeral midshaft, where it has a conforming surface contact with the bone. Orthopedic screws include 3.5 mm self-tapping cortical non-locking and locking screws. Bicortical and unicortical screws have 34 mm and 14 mm in length respectively. Six holes of the LCP plate were utilized for screw fixation. Three screws were placed in either sides of the plate subsequently created a transverse osteotomy (10 mm in length) to optimize axial stability, which maintains screw density at 0.75.10 All screws were inserted into the bone plate construct with constant 4.5 N m torque by using a torque limited screw driver. Group 1, control group, had fixated with the traditional method, which has 6 bicortical non-locking screws. Group 2 and group 3 mixed unicortical and bicortical screws; two bicortical screws were placed at the end holes to gain maximum of axial support,2, 11 and the four unicortical screws were inserted in each fragment of the bone construct excepting the middle holes. Group 2 is a hybrid locking (HL), which obtains unicortical locking screw, whereas group 3 is a hybrid non-locking (HNK), which procures non-locking screw with adding of Kryptonite™ bone cement (Fig. 1). In hybrid groups, screws were placed according to principle of plate/screw fixation. Screws were simultaneously inserted from inferior to superior, and non-locking screws were applied prior to locking screws in order to achieve fracture reduction. Kryptonite™ bone cement became taffy phase, when it was kept curing for 4–5 min; after that it was injected into the LCP hole before the non-locking screw was applied.
Fig. 1.
Screw configuration of the 3 study groups.
The total of 8 fixated specimens in each group were subsequently separated into two subgroups (n = 4) to conduct biomechanical analyses. Axial and torsional perspectives were individually proposed for the mechanical analysis, because motion of the arm is heavily involved by axial and torsional forces. Following surgery, the constructed bone-implant montage must maintain axial and torsional stability efficient to allow functional painless motion of the limb. Axial compression and external rotation were used for axial and torsional analyses respectively. Tested specimens were fixated in a customized universal fixture, which was fabricated for testing of orthopedic bone implant. The mechanical tests including static and dynamic analyses were performed by a servo-hydraulic material testing system (Model Bionix 370.02, MTS systems, USA). Dynamic analysis with low cyclic tests were individually run at 1 Hz frequency with repeated loads 0–500 N in axial compression and 0–20° external rotation for 10,000 cycles. If the specimens successfully passed the cyclic tests without deformation, they were then studied for static analysis. Nondestructive failure tests were consequently carried out both axial compression and torsion, an axial displacement of 0.01 mm/s with maximum displacement of 10 mm and 0.5° s−1 and maximum angular displacement of 40° respectively was utilized.12 Load vs. displacement graph of each constructed was analyzed, and the slope of the linear region of the curve was defined as the stiffness of the construct. In addition, an intersection point between offset linear regression and the curve was defined as yield point of the construct. The axial yield point, stiffness were recorded for axial compression, whereas the torsional yield point and stiffness were collected for torsion. Statistical analysis was conducted to compare independent variables both axial and torsional perspectives, which are required of normal distribution using commercial statistical analysis software (SPSS Statistics Version 22, IBM Inc., USA). The independent variables of each group were analyzed for normality by using Shapiro–Wilk Test with a 95% confidence interval. One-way analysis of variances (ANOVA) was utilized to examine the significant differences among the three groups. Post hoc analysis was then conducted to evaluate the result of ANOVA test by performing multiple comparisons among the three groups. Depending on equal and unequal variances of the independent variables, Scheffe and Games-Howell post hoc analysis was chosen for interpretation. Examination of the equal variances assumption was conducted by Levene test of equal variances (P < 0.05).
3. Results
All specimens of the three groups passed 10,000 cycles of the axial and torsional cyclic tests without any major damage. The specimens of the three groups were then subjected to the load-failure tests. Results of axial and torsional failure tests are summarized in Table 1.
Table 1.
Stiffness and yield strength of the 3 groups in axial compression and torsion.
| Bone construct | Stiffness |
Yield strength |
||
|---|---|---|---|---|
| Compression (N/mm) | Torsion (N m/degree) | Compression (N) | Torsion (N m) | |
| Group 1 | 277 ± 28 | 0.34 ± 0.02 | 916 ± 65 | 6.86 ± 1.05 |
| Group 2 | 311 ± 32 | 0.33 ± 0.01 | 818 ± 167 | 6.58 ± 0.37 |
| Group 3 | 306 ± 30 | 0.35 ± 0.002 | 937 ± 68 | 6.57 ± 0.42 |
3.1. Axial compression
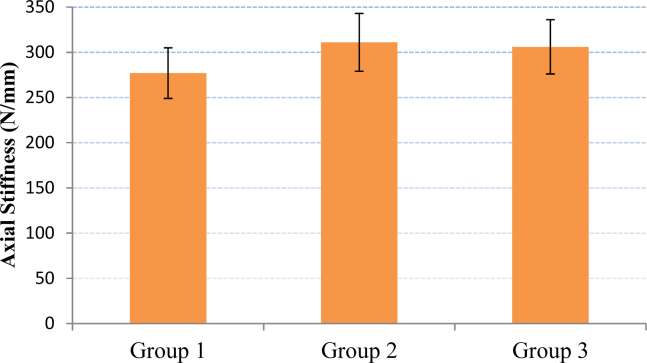
Both group 2 and group 3 were found superior to compare with the control group in the axial stiffness. The increase was 12.3% and 10.5% over group 2 and group 3 respectively (Fig. 2).
Fig. 2.
Mean (SD) construct stiffness under axial compression.
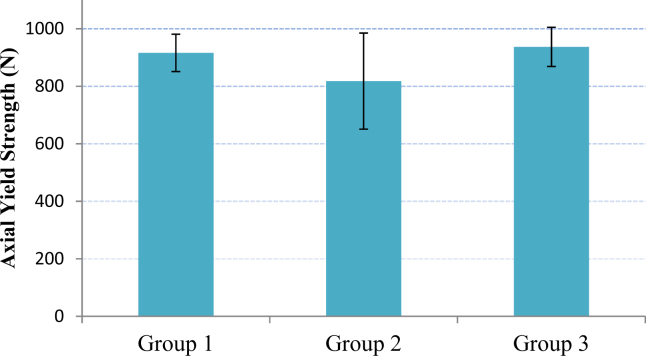
The axial yield points of the constructed groups were defined by a 0.025% offset for the axial failure analysis. The average value of constructed yield strength in group 3 was found 2.24% higher than group 1 or control group, but group 2 was found 12% decreasing of axial yield strength to compare with the control group (Fig. 3). The constructed groups experienced a small axial displacement, and morphology of the constructed group after failure test showed a typical plate bending at the osteotomy gap.
Fig. 3.
Mean (SD) construct yield strength under axial compression.
Both axial stiffness and yield strength among three constructed groups were normally distributed (Shapiro Wilk Test, P > 0.05). The result of ANOVA test initially revealed that the differences in axial stiffness and yield strength were found non-significant among the three groups (axial stiffness: P = 0.306 and axial yield strength: P = 0.315 > 0.05). Levene test indicated equal variances for axial stiffness (P = 0.965 > 0.05), while axial yield strength was found non-equal variances (P = 0.03 < 0.05). The Scheffe and Games-Howell post hoc analysis confirms the accuracy of ANOVA test, thus axial stiffness and yield strength were found statistically non-significant among three groups.
3.2. Torsion
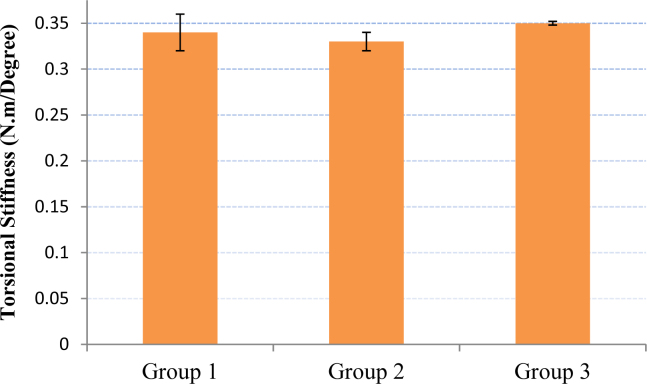
Torsional stiffness was found with a small difference among three groups. In fact, group 2 was found 3.03% less than control group, while group 3 was found 2.85% greater (Fig. 4). However, the small percentage difference (<10%) indicates equivalent of torsional stiffness among the three groups.
Fig. 4.
Mean (SD) construct stiffness under torsion.
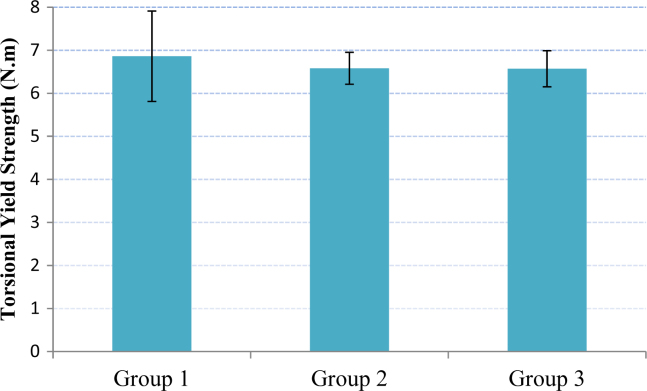
The torsional yield strength in failure test was defined by a 0.125% offset method. The decrease torsional yield strength was observed both group 2 and group 3 to compare with the control group. The values of torsional yield strength in groups 2 and 3 were found 4.25% and 4.41% smaller than the control group (Fig. 5). Nevertheless, the percentage differences were non-significant, and it also indicated equivalent torsional yield strength among the three groups. The constructed groups in torsional failure test appeared as plate twisting at the osteotomy gap.
Fig. 5.
Mean (SD) construct yield strength under torsion.
Torsional stiffness and yield strength were found normal distribution (Shapiro Wilk Test, P > 0.05). With small percentage difference torsional stiffness and yield strength were initially found non-significant (ANOVA test; torsional stiffness: P = 0.13; torsional yield strength: P = 0.81 > 0.05). Levene test indicated equal variances for torsional stiffness (P = 0.496 > 0.05), while torsional yield strength was found non-equal variances (P = 0.047 < 0.05). The Scheffe and Games-Howell post hoc analysis confirms the accuracy of ANOVA test; thus the differences for torsional stiffness and yield strength were found statistically non-significant among three groups.
4. Discussion
In the physiological environment humerus midshaft fractures are mostly influenced by axial and torsional forces because of natural human arm motion.13 During the post-op period, the bone implant should demonstrate axial and torsional stability. Dynamic analysis with low cyclic tests was successfully run at a 1 Hz frequency for 10,000 cycles to depict the low activity level of a 50 kg person during the first 20 days after post-op surgery with an assumption of 500 cycles of weight bearing each day. The results of static analysis indicated that the HL and HNK groups maintained similar axial stiffness values during the failure test, and were greater than the control group. However, the HL group was weaker in axial yield strength than both the HNK and control groups. There were no differences in torsional stiffness between the three groups. The HL and HNK groups obtained similar torsional yield strength values and were weaker than the control group.
Mechanical analysis, which utilizes the principles of statics and dynamics, elucidated the results of the biomechanical tests. The HL and HNK groups maintained higher axial stiffness than the control group, because they had smaller axial displacement. Also, the axial stiffness is determined by dividing the axial force over the displacement. Bending moment of the bone plate occurred at the middle and was the product of the reaction forces and distance with respect to the point of interest, where the moment occurs. The control group developed bone reaction forces between the near and far cortexes, which resulted in a higher bending moment and decreased the stiffness of the control group. Furthermore, the HL group has locking screws to lock the bone plate a distance away from the periosteum of the bone; therefore, external friction forces were absent in the bone construct, which made it less susceptible to a bending moment. Hence, the HL group performed the best in axial stiffness. Because of having reactions in one cortex and lacking external frictional forces, the HL construct's axial yield strength is greatly reduced and is smaller than those of the HNK and control groups. Moreover, the HNK construct having Kryptonite® bone cement enhances the magnitude of reaction force and increases the axial yield strength, which makes it equivalent to the control group. Torsional stiffness and ultimate torsional failure primarily depend on internal shear forces, which were developed by the external torque. In this case, the control group proved its torsional rigidity superiority over the HL and HNK constructs since the internal shear force developed at both cortices of the bone.
According to the biomechanical study, there is no doubt that Kryptonite™ bone cement positively alters the axial and torsional behavior of the LCP construct. From the axial perspective, adding of the bone cement with non-locking screws enhances the bone construct to make it equivalent with the bone construct with locking screws. Energy absorption of the bone cement maintains high axial yield strength in the constructed bone implants of non-locking screws. The energy absorption of the bone cement is considered a great advantage in fracture healing because it maintains minimal axial stiffness but still allows sufficient micro-motion between the bone implant interface and the bone to promote callus formation.14 There is no evidence of utilizing bone cement to improve the torsional rigidity of the constructed bone implant.
This study has successfully developed an applicable technique of long bone fixation, which utilizes a hybrid construct of mixed unicortical and bicortical screws. The hybrid construct is a minimally invasive technique that is able to facilitate early bone healing, reduce recovery time, and reduce the risk of re-fracture after screw plate removal. The use of unicortical screws eliminates the need for drilling through the far cortex and thus eliminates the risk of adjacent neurovascular injury or soft tissue compromise. In humerus mid-shaft fractures, screw prominence that potentially damages the radial nerve will also be less likely, when unicortical screws are applied. The LCP is beneficial in comminuted fracture scenarios, where locking and non-locking screws are required to stabilize the fracture. When a comminuted fracture contains oblique fragments, which require angled screws to obtain a direct compression of the bone plate with the bone fragment, locking screws become very limited, since they can only be inserted perpendicular to the bone plate with less than a 5° angle of deviation. Instead, non-locking screws could be utilized to obtain direct compression between the bone plate and bone fragment(s). Then, Kryptonite™ bone cement can be incorporated to enhance the axial strength of the bone construct as well as prevent screw loosening and togging.
Conflicts of interest
The authors have none to declare.
Acknowledgement
This study was supported by an internal grant in collaboration between Department of Biomedical Engineering, Mercer University and Orthopedic Trauma Institute, Navicent Heath Hospital, Macon GA, USA.
References
- 1.Denies E., Nijs S., Sermon A., Broos P. Operative treatment of humeral shaft fractures. Comparing of plating and intramedullary nailing. Acta Orthop Belg. 2010;76(6):735. [PubMed] [Google Scholar]
- 2.Gautier E., Perren S., Cordey J. Guidelines for the clinical application of the LCP. Injury. 2003;31:63–76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 3.Stoffel K., Dieter U., Stachowiak G., Gachter A., Kuster M. Biomechanical tetsing of the LCP-how can stability in locked internal fixators be controlled? Injury. 2003;34:11–19. doi: 10.1016/j.injury.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Patel V. Wright State University; Dayton, Ohio: 2008. Biomechanical Evaluation of Locked and Non-Locked Constructs Under Axial and Torsion Loading. [Google Scholar]
- 5.Gardner M., Griffith M., Demetrakopoulous D. Hybrid locked plating of osteoporetic fractures of the humerus. J Bone Jt Surg. 2006;88(9):1962–1967. doi: 10.2106/JBJS.E.00893. [DOI] [PubMed] [Google Scholar]
- 6.Lim W., Jariwala A., Wigderowitz C., Drew T. The use of bone adhesive for fracture fixation in long bones – a biomechanical study. Front Biol Life Sci. 2014:29–33. [Google Scholar]
- 7.Matthew L., Hirsch C. Temperatures measured in human cortical bone when drilling. J Bone Jt Surg. 1972;54(2):297–308. [PubMed] [Google Scholar]
- 8.Luong Q., Vo H., Webb L. Mercer University; Macon, Georgia: 2014. The Biomechanical Effects of Kryptonite Bone Cement: An In-Vitro Study of Porcine Femurs. [Google Scholar]
- 9.Cristea S., Groseanu F., Predescu V., Gavrila M., Gartonea D., Papalici A. A new approach in minimal invasive treatment of fractures. Eur J Orthop Surg Traumatol. 2012;22(4):283–287. [Google Scholar]
- 10.Miller D., Goswami T. A review of locking compression plate biomechanics and thier advantages as internal fixators in fracture healing. Clin Biomech. 2007;22(10):1049–1062. doi: 10.1016/j.clinbiomech.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Roberts J., Grindel S., Rebholz B., Wng M. Biomechanical evaluation of locking plate radial shaft fixation: unicortical locking fixation versus mised bicortical and unicortical fixation in a sawbone model. J Hand Surg. 2007;32(7):971–975. doi: 10.1016/j.jhsa.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 12.An Y., Draughn R. CRC Press; 1999. Mechanical Testing of Bone and the Bone Implant Interface. [Google Scholar]
- 13.Mannanal S. University of Akron; Akon, Ohio: 2009. Biomechanical Evaluation of Hybrid Locked Plating for Humeral Fracture Fixation. [Google Scholar]
- 14.Stoffel K., Klaue K., Perren S. Functional load of plates in fracture fixation in vivo and its correlate in bone healing. Injury. 2000;31:37–86. doi: 10.1016/s0020-1383(00)80042-x. [DOI] [PubMed] [Google Scholar]