Abstract
AIM: To investigate if the clinical outcome of intra-articular lumbar facet joint injections is affected by the therapist’s attitude.
METHODS: A total of 40 patients with facet joint-associated chronic low back pain were randomly divided into two groups. All patients received computed tomography-guided, monosegmental intra-articular facet joint injections. Following the therapeutic procedure, the patients of the experimental group (EG) held a conversation with the radiologist in a comfortable atmosphere. During the dialog, the patients were encouraged to ask questions and were shown four images. The patients of the control group (CG) left the clinic without any further contact with the radiologist. Outcome was assessed using a pain-based Verbal Numeric Scale at baseline, at 1 wk and at 1, 3, and 6 mo after first treatment.
RESULTS: The patient demographics showed no differences between the groups. The patients of the EG received 57 interventional procedures in total, while the patients of the CG received 70 interventional procedures. In both groups, the pain scores decreased significantly over the entire observation period. Compared to the CG, the EG showed a statistically significant reduction of pain at 1 wk and 1 mo post-treatment, while at 3 and 6 mo after treatment, there were no significant differences between both groups.
CONCLUSION: Our results show a significant effect on pain relief during the early post-interventional period in the EG as compared to the CG. The basic principle behind the higher efficacy might be the phenomenon of hetero-suggestion.
Keywords: Facet joint injection, Hetero-suggestion, Low back pain, Lumbar spine, Magnetic resonance imaging, Facet joint osteoarthritis
Core tip: The presented results show a significantly positive effect of the therapist’s attitude on pain relief within the first month after facet joint intra-articular injections. Increased therapeutic efficacy seems to be evident in those patients who have a better understanding of therapies applied on them.
INTRODUCTION
Facet joint osteoarthritis (FJOA) is one of the major causes of chronic low back pain (CLP)[1,2]. FJOA and its secondary disorders set an increasing burden on health care systems[3]. Therefore, multiple therapeutic options have been reported and established in the management of FJOA-associated CLP[4]. Among others, injections of glucocorticoid-anaesthetic compositions into the lumbar facet joints (LFJ) are regularly implemented[5]. The concept of this therapeutic approach relies on the idea that the synovia of the degenerated facet joints is inflamed. Following this approach, intra-articular injections of above-mentioned drugs are performed to generate an anti-inflammatory effect leading to pain relief. To date, there is controversy about the effectiveness of intra-articular steroid injections[6]. Recently, several studies were conducted to learn more about the clinical benefit of LFJ infiltration with glucocorticoids in comparison to alternative treatment options[7-9].
Comparing the clinical outcome of radiofrequency denervation and intra-articular steroid injections in degenerated facet joints of the lumbar segments L3-S1, Lakemeier et al[7] analyzed 56 patients suffering from chronic low back pain in a double-blinded, randomized survey. Over a 6-mo observation period, the authors found no significant differences in pain-relief between the two procedures.
Apart from technical aspects of the interventional procedure, numerous other factors are known to be involved in the outcome of LFJ infiltration. Gryll et al[10] already pointed out that situational parameters contribute to placebo effect in oral surgery interventions (attitudes of dentist and dental technician, status of communicator of drug effects, and information on drug effects). Of these factors, a significant fear reduction and more acceptable pain experience from mandibular block injection was only achieved by the attitudes of the dentist and the dental technician.
The aim of our study was to investigate the influence of the therapist’s attitude and empathy on the effectiveness of LFJ infiltrations.
MATERIALS AND METHODS
Ethical committee approval was obtained for the study. All study participants gave their written informed consent prior to the therapy.
Study participants
Demographics are presented in Table 1. Forty consecutive patients with diagnosed facet joint syndrome of the segments L4/5 or L5/S1 were included in this non-blinded randomized controlled study. Every new patient was alternately assigned to the expermiental group (EG) or the control group (CG). The diagnosis was based on the clinical criteria for facet joint-associated CLP: Paraspinal pain with or without pseudoradicular symptoms; absence of neurological deficiency and pain on hyperextension. Prior to therapy, all patients also received standardized magnetic resonance imaging (MRI) of the lumbar spine (sagittal STIR images, sagittal T2- and T1-weighted images, axial T2-weighted images) to confirm morphologic signs of facet joint degeneration and to rule out other pain-related changes like a herniated lumbar disc or neoplasm.
Table 1.
Demographics of experimental group and control group
| EG | CG | |
| Gender | ||
| Male | 40% (8) | 50% (10) |
| Female | 60% (12) | 50% (10) |
| Age | ||
| Mean ± SD | 58.6 ± 15.4 | 57.5 ± 14.5 |
| Range | 29-83 | 30-84 |
EG: Experimental group; CG: Control group.
Inclusion criteria
The inclusion criteria were as follows: > 18 years of age; CLP for at least 3 mo and clinical diagnosis of facet joint-related pain syndrome; MRI-proven facet joint degeneration.
Exclusion criteria
The exclusion criteria were as follows: Prior surgery on the lumbar spine; prior LFJ intra-articular injections in the last 12 mo; vertebral fractures or stenosis of the lumbar spinal canal; poorly regulated diabetes; known allergy to bupivacaine or triamcinolone acetate.
Intervention
All patients were handled in an outpatient set-up and had an informed consent discussion at least 24 h before the interventional procedure. All interventions were performed under computed tomography (CT; Siemens 40, Siemens Medical Systems, Forchheim, Germany) guidance. The exposure parameters for CT scanning were 120 kv and 40 mA. All scans were reconstructed in 2.4 mm slice thickness and 1.2 mm overlap. Before therapy, it was ensured that patients were not taking anticoagulants or aspirin. All interventions were performed by a staff radiologist (A. M.) with more than 10 years of experience in interventional radiology. The L4/5 or L5/S1 facet joints were injected bilaterally in a mono-segmental set-up.
The course of the interventional procedure was as follows: (1) the target joints were identified by the pain pattern and the reproduction of pain with deep pressure directly before the interventional procedure; (2) after positioning the patient in a prone position, two wire markers were placed on the patient’s back. The first one was oriented lengthwise along the spinal processes and was used to plan the right and left puncture sites in an axial CT image. The second one was oriented crosswise at the level of maximum pain and was used to identify the lumbar level (L4/5 or L5/S1) to be treated on the sagittal scout view; (3) the skin around the puncture site was disinfected with 10% iodine solution; (4) under CT guidance, the needles were manually shifted to the target area and the correct needle position was documented by axial CT images; and (5) a mixture of 4 mL of 0.5% bupivacaine and 1 mL of triamcinolone acetate (20 mg) was injected into each of the target joints.
EG
Following the therapeutic procedure, the patients were shown four images on a quartered monitor view by the staff radiologist (Figure 1). The images are as follows: (1) the sagittal scout view of the lumbar spine; (2) an axial CT image showing the degenerated joints of the lumbar levels L4/5 or L5/S1; (3) an axial CT image showing the planned course of the needles as drawn with a digital caliper; and (4) an axial CT image showing the final, intra-articular positions of the needle tip on each side.
Figure 1.
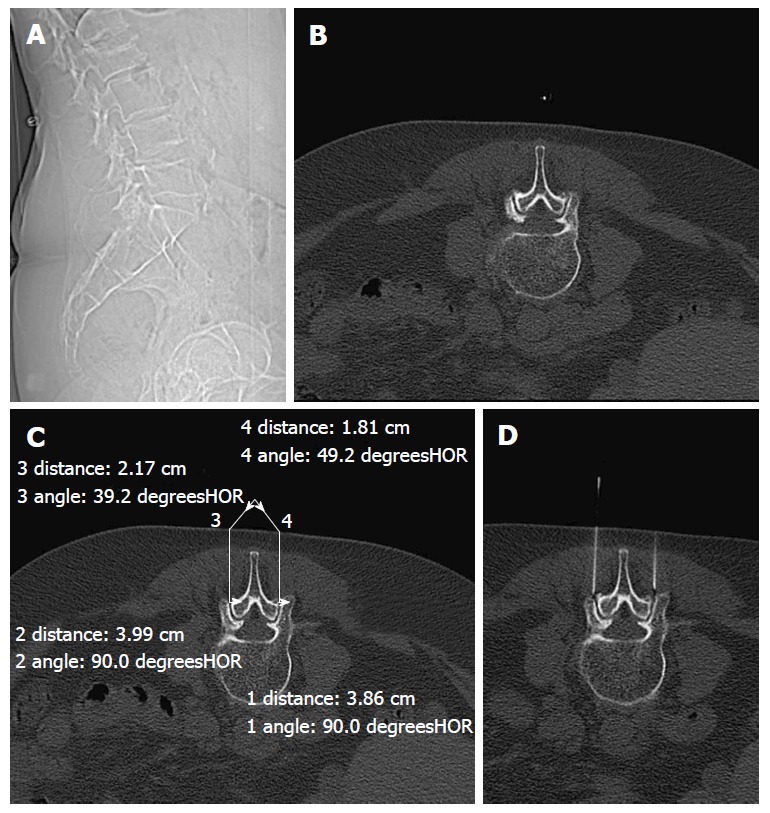
Set of four standard images presented to the experimental group. A: Sagittal scout view of the lumbar spine; B: Axial CT image showing the degenerated facet joints; C: Axial CT image showing the planned course of the needles; D: CT image showing the final positions of the needle tip on each side. CT: Computed tomography.
During the conversation with the patients of the EG in a comfortable atmosphere, the radiologist empathically emphasized the technical success of the procedure. Also, the patients were encouraged to ask questions during the dialog. After the conversation, the patients were asked to stay in the waiting room for an additional 30 min. If no side effects occurred, the patients were allowed to leave the medical facility.
CG
After the therapeutic procedure, the radiologist left the interventional unit. As in the EG, the patients of the CG were asked to stay in the waiting room for 30 min. If no side effects occurred, they were allowed to leave the medical facility. No further face-to-face contact with the interventional radiologist was provided.
Outcomes
Outcome was assessed using a Verbal Numeric Scale (VNS). The options ranged from 1 to 10, with 1 representing no pain and 10 representing the worst pain imaginable. Patients of both groups were instructed to give feedback 2 d after the therapeutic procedure. A reduction of pain of at least 50% as assessed by the VNS was defined as therapeutic success. If pain reduction was less than 50% or if subjective pain relief was insufficient, the patients were invited for further treatments according to the above-mentioned therapeutic process. Pain was assessed using the VNS at baseline (day of first treatment) and at 1 wk, 1 mo, 3 mo, and 6 mo after the first treatment.
Statistics analysis
Data analysis was performed using the BIAS software package (Epsilon publisher, Frankfurt/Main, Germany, http://www.bias-online.de) and comprised descriptive statistics inclusive of SD. The Wilcoxon-Mann-Whitney test was used to compare pre- and post-treatment results of the VNS pain scores. A P-value less than 0.05 was considered statistically significant. No attempt at imputation was made for missing data.
RESULTS
Demographics
The patients’ demographics are listed in Table 1. Both mean age (approx: 58 ± 15) and age range (29-84) showed no differences among the groups. In the EG, more female patients were randomly enrolled compared to the CG.
Procedural characteristics
The procedural characteristics are presented in Table 2. The patients of the EG received 57 interventional procedures in total, while the patients of the CG received 70 interventional procedures. The average number of procedures ranged from 2.85 ± 1.1 (EG) to 3.5 ± 2.1 (CG) and showed no statistical significance (EG vs CG, P = 0.39 > 0.05).
Table 2.
Frequency of procedures over a period of 6 mo
| No. procedures in 6 mo | EG | CG |
| 1 | 5 | 2 |
| 2 | 2 | 2 |
| 3 | 4 | 5 |
| 4 | 4 | 7 |
| 5 | 4 | 4 |
| Total procedures in 6 mo | 57 | 70 |
| Average | 2.85 ± 1.1 | 3.5 ± 2.1 |
EG: Experimental group; CG: Control group.
Pain relief
VNS data are listed in Table 3. Compared to baseline, the pain scores decreased significantly (P < 0.05) at all investigated points in time in both groups (first week, first month, third month, and sixth months after treatment). In the EG, the median pain score decreased from 9 at baseline (range 8-10) to 3 at first week and first month after treatment (range 1-5). The baseline median pain score of 9 (range 4-10) in the CG declined to 4.5 at 3 mo (range 1-8) and 6 mo (range 1-9).
Table 3.
Comparison of pain improvement based on a verbal numeric scale
| Pain score | EG | CG |
| Median (range) | ||
| Baseline | 9 (8-10) | 9 (4-10) |
| 1 wk | 3 (1-5) | 6.5 (3-8) |
| 1 mo | 3 (1-5) | 5 (3-8) |
| 3 mo | 4 (1-6) | 4.5 (1-8) |
| 6 mo | 5 (1-10) | 4.5 (1-9) |
EG: Experimental group; CG: Control group.
Compared to the CG, the pain scores in the EG showed a higher decline in the early posttherapeutic phase, which was significant at 1 wk (P < 0.001) and at 1 mo (P = 0.004 < 0.05) post-treatment. Statistical analysis did not reveal significant differences between both groups at 3 mo (EG vs CG, P = 0.07 > 0.05) and 6 mo (EG vs CG, P = 0.71 > 0.05) after treatment.
Adverse events
No adverse events were observed within the 6-mo post-interventional period.
DISCUSSION
Our study demonstrates a distinct therapist’s effect on pain relief during the first month after LFJ intra-articular injections in the EG in comparison to the CG. Increased therapeutic efficacy seems to be evident in those patients who have a better understanding of the interventional procedures. The underlying basic principle might be the effect of hetero-suggestion, which is a method to convey a message into the subconscious of another person. In our study, this effect occurred during the patient-physician interaction immediately after treatment when the standardized images of the performed therapy were presented to the patient. From the psychodynamic perspective, hetero-suggestion always comes along with a variable, inter-individual amount of auto-suggestion[11]. Having this in mind, it is understood that despite standardized hetero-suggestive procedures, the positive effect of therapies can vary among patients. Moreover, the level of suggestibility is not constant in humans but rather intra-individual, and depends on the type of intervention as well as on the therapeutic setup[11]. Patients are regularly more impressed by surgical setups as compared to medication alone. Therefore, surgical approaches have a higher auto-suggestive potential than non-surgical approaches[11]. The patient’s perception of the therapeutic effect can depend on how a drug is administered to the patient. Patients report a better efficacy of drugs after intramuscular injections as compared to oral administration, though pharmacokinetics does not provide evidence of that. Symptom red[12] uction is not possible merely by consciously wanting it but can rather be achieved by subconscious belief[11]. In this context, pain and Parkinson’s disease are best evaluated where the associated neurobiological effects cannot provide a conclusive explanation, but indicate a rather complex mode of action of placebo effects[13,14]. The involvement of cannabinoids and opioids is considered to be assured because placebo-associated effects can be antagonized by drugs[14]. Concurrently, the production endorphins and other neurotransmitters are regarded as possible neurophysiological mediators in pain relief as a result from hetero-suggestion[15].
Both placebo and suggestion are difficult to conceptualize, and therefore, cannot be directly evaluated scientifically. Nonetheless, both factors are considered as disruptive factors in studies[11]. A positive patient-physician relationship is empirically approved to have the best curative effect in the field of psychotherapy[16]. Empathy, transparency, and the exchange of information on the treatment applied contribute to that curative effect.
Both medical staff and patients associate the use of placebo effect with a form of deception[17]. Our study demonstrates how the comprehensible use of the placebo effect positively influences the therapeutic benefit of patients by a reproducible patient-physician interaction.
Over the past years, facet joint interventions were increasingly applied[5], while evidence of efficacy for therapeutic LFJ applications of glucocorticoids and local anaesthetics is only moderate for short-term improvement and limited for long-term improvement of facet joint-associated pain syndromes[18].
Ribeiro et al[8] investigated the therapeutic outcome of intra-articular vs intramuscular glucocorticoid applications in patients with facet joint-associated chronic low back pain. The experimental group was administered bilateral intra-articular injections in the three lower lumbar segments (L3-S1). In contrast, six intramuscular injections were given on the bilateral surface points of the paravertebral lumbar musculature in the control group. Both intra-articular and intramuscular injections led to pain relief in the 6-mo observation period with no significant difference between both groups. In order to analyze the therapeutic potency of intra-articular administration of corticosteroids, Manchikanti et al[9] randomized 60 patients in four groups. Groups I and II received intra-articular injections of either bupivacaine alone or in combination with Sarapin, while groups III and IV additionally received corticosteroids. The results of the 12-mo observation period revealed a statistically relevant pain relief and an improved functional status in all groups compared to baseline measurements. Interestingly, the average number of treatments, the average duration of pain relief, and the recorded pain scores at 3, 6, and 12 mo did not differ significantly between the study groups.
Regarding these studies using a variety of different interventional procedures for the treatment of facet joint-associated pain syndromes[7-9], two aspects become obvious: (1) regardless of the applied technique or drug combinations, the pain scores decrease significantly in the course of the respective observation period compared to the baseline; and (2) long-term pain scores show no significant differences after LFJ intra-articular injection with different drug combinations.
Considering the above-mentioned aspects, it is evident that the most important factor to overcome facet joint-associated CLP is time, i.e., for patients, the most critical phase is the first weeks after pain onset. Against this background, the results of this study should find consideration in the daily clinical routine. Radiologists should be aware of the phenomenon of hetero-suggestion, which can be easily and effectively applied to support therapies such as LFJ infiltrations.
Limitations of this study are the relatively small patient cohort and the non-blinded study design, which could have resulted in the generation of an observer bias. Furthermore, this study focused on the therapist’s attitude. Of course, there are several other factors that can induce placebo effects, e.g., patients’ beliefs and values and sociocultural factors. Another limitation is the non-standardization of the post-procedural conversation with its open-ended questions and the impossible quantification of the therapist’s hetero-suggestive effects.
The therapist’s attitude has a significant positive effect on pain relief in patients with LFJ-associated CLP during the early post-interventional period after LFJ intra-articular injection. The underlying principle might be the phenomenon of hetero-suggestion. Radiologists should be aware of such psychological phenomena in order to use them as a powerful and easy-to-apply tool, which can support therapeutic procedures such as intra-articular injections.
COMMENTS
Background
Lumbar facet joint infiltration is an widely used therapy in patients with chonic low back pain (CLP). Lack of clarity exist about the degree of underlying psychophysiological effects. The objective of the authors’ study was to analyze the impact of the therapist’s attitude on the clinical outcome of lumbar facet joints (LFJ) intra-articular injections.
Research frontiers
Auto-suggestion and hetero-suggestion are known phenomena to explain placebo effects. Very few articles deal with these phenomena in computed tomography (CT)-guided interventional pain therapies of the lumbar spine.
Innovations and breakthroughs
The authors compared the clinical outcomes between two groups that both received a routine LFJ intra-articular injection. The experimental group additionally held a post-procedural conversation with the therapist that included the demonstration of four standardized CT images. The control group passed without any posttherapeutic contact.
Applications
The results of this study suggest that hetero-suggestion might have a positive effect on pain relief in patients with LFJ-associated CLP during the early post-interventional period after LFJ intra-articular injection. However, larger blinded randomized controlled trials are needed to confirm these findings.
Terminology
Hetero-suggestion is a psychological method and easy-to-apply tool to induce short-term placebo effects.
Peer-review
This is a very interesting study on the phenomenon of hetero-suggestion as underlying explanation of short-term pain relief in patients with CLP after LFJ intra-articular injections. Good conclusion of the therapist’s effect but there are of course several other possible factors that can influence the clinical outcome as the patient’s attitude.
Footnotes
Institutional review board statement: The study inclusive of patient information and consent form was reviewed and approved by the ethics committee of the State Authorisation Association for Medical Issues of Hesse, Germany (FF 141/2014). Furthermore, the study was registered at the German Clinical Trials Register (DRKS00010011). All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Clinical trial registration statement: The study inclusive of patient information and consent form was reviewed and approved by the ethics committee of the State Authorisation Association for Medical Issues of Hesse, Germany (FF 141/2014). Furthermore, the study was registered at the German Clinical Trials Register (DRKS00010011). All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Informed consent statement: The study inclusive of patient information and consent form was reviewed and approved by the ethics committee of the State Authorisation Association for Medical Issues of Hesse, Germany (FF 141/2014). Furthermore, the study was registered at the German Clinical Trials Register (DRKS00010011). All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: All authors ensure that there are no conflicts of interest.
Data sharing statement: Consent was not obtained but the presented data are anonymized and risk of identification is very low. No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: December 23, 2015
First decision: January 15, 2016
Article in press: March 23, 2016
P- Reviewer: Chow J, Gao BL S- Editor: Qiu S L- Editor: A E- Editor: Li D
References
- 1.Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol. 2013;9:216–224. doi: 10.1038/nrrheum.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suri P, Dharamsi AS, Gaviola G, Isaac Z. Are facet joint bone marrow lesions and other facet joint features associated with low back pain? A pilot study. PM R. 2013;5:194–200. doi: 10.1016/j.pmrj.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, Dellavalle R, Danaei G, Ezzati M, Fahimi A, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen SP, Huang JH, Brummett C. Facet joint pain--advances in patient selection and treatment. Nat Rev Rheumatol. 2013;9:101–116. doi: 10.1038/nrrheum.2012.198. [DOI] [PubMed] [Google Scholar]
- 5.Manchikanti L, Pampati V, Singh V, Falco FJ. Assessment of the escalating growth of facet joint interventions in the medicare population in the United States from 2000 to 2011. Pain Physician. 2013;16:E365–E378. [PubMed] [Google Scholar]
- 6.Manchikanti L, Datta S, Gupta S, Munglani R, Bryce DA, Ward SP, Benyamin RM, Sharma ML, Helm S, Fellows B, et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 2. Therapeutic interventions. Pain Physician. 2010;13:E215–E264. [PubMed] [Google Scholar]
- 7.Lakemeier S, Lind M, Schultz W, Fuchs-Winkelmann S, Timmesfeld N, Foelsch C, Peterlein CD. A comparison of intraarticular lumbar facet joint steroid injections and lumbar facet joint radiofrequency denervation in the treatment of low back pain: a randomized, controlled, double-blind trial. Anesth Analg. 2013;117:228–235. doi: 10.1213/ANE.0b013e3182910c4d. [DOI] [PubMed] [Google Scholar]
- 8.Ribeiro LH, Furtado RN, Konai MS, Andreo AB, Rosenfeld A, Natour J. Effect of facet joint injection versus systemic steroids in low back pain: a randomized controlled trial. Spine (Phila Pa 1976) 2013;38:1995–2002. doi: 10.1097/BRS.0b013e3182a76df1. [DOI] [PubMed] [Google Scholar]
- 9.Manchikanti L, Manchikanti KN, Manchukonda R, Cash KA, Damron KS, Pampati V, McManus CD. Evaluation of lumbar facet joint nerve blocks in the management of chronic low back pain: preliminary report of a randomized, double-blind controlled trial: clinical trial NCT00355914. Pain Physician. 2007;10:425–440. [PubMed] [Google Scholar]
- 10.Gryll SL, Katahn M. Situational factors contributing to the placebos effect. Psychopharmacology (Berl) 1978;57:253–261. doi: 10.1007/BF00426747. [DOI] [PubMed] [Google Scholar]
- 11.Mommaerts JL, Devroey D. The placebo effect: how the subconscious fits in. Perspect Biol Med. 2012;55:43–58. doi: 10.1353/pbm.2012.0005. [DOI] [PubMed] [Google Scholar]
- 12.Acar B, Kamburoğlu K. Use of cone beam computed tomography in periodontology. World J Radiol. 2014;6:139–147. doi: 10.4329/wjr.v6.i5.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harden RN, Gracely RH, Carter T, Warner G. The placebo effect in acute headache management: ketorolac, meperidine, and saline in the emergency department. Headache. 1996;36:352–356. doi: 10.1046/j.1526-4610.1996.3606352.x. [DOI] [PubMed] [Google Scholar]
- 14.Benedetti F. Placebo-induced improvements: how therapeutic rituals affect the patient’s brain. J Acupunct Meridian Stud. 2012;5:97–103. doi: 10.1016/j.jams.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Manchikanti L, Giordano J, Fellows B, Hirsch JA. Placebo and nocebo in interventional pain management: a friend or a foe--or simply foes? Pain Physician. 2011;14:E157–E175. [PubMed] [Google Scholar]
- 16.Kato S. [Review of placebo effect and re-evaluation of psychotherapy focusing on depressive disorders] Seishin Shinkeigaku Zasshi. 2013;115:887–900. [PubMed] [Google Scholar]
- 17.Cohen S, Shapiro H. “Comparable placebo treatment” and the ethics of deception. J Med Philos. 2013;38:696–709. doi: 10.1093/jmp/jht052. [DOI] [PubMed] [Google Scholar]
- 18.Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, Bowman RC, Deer TR, Datta S, Colson JD, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005;8:1–47. [PubMed] [Google Scholar]


