Abstract
Context:
Lack of literature on psychological aspects of survivors of farmers' suicides is hurdle in devising effective helping strategies for rising number of survivors across the country.
Aims and Objectives:
To assess the psychological distress and its correlates in survivors of farmers' suicides.
Settings and Design:
Case–control study design was used in Wardha District of Vidarbha region in the central India.
Materials and Methods:
A predesigned and pretested semistructured questionnaire was used to assess sociodemographic variables. Self-Reporting Questionnaire-20 was used to evaluate psychological distress in 98 survivors of farmers' suicides and 98 age, sex, and occupation-matched controls.
Statistical Analysis:
Significance of differences between case and control groups were assessed using Chi-square test or Fisher's two-tailed exact test for class variables. For continuous variables, Student's t-test was used P < 0.05 was considered significant.
Results:
Significantly higher proportion of survivors had psychological distress than controls. Female survivors, spouse and parents of suicide victims had a high risk of distress. Psychological distress was commonly expressed by depressive and somatic symptoms.
Conclusions:
Survivors of farmers' suicides are suffering from significant psychological distress.
Keywords: Farmers' suicide, psychological distress, survivor
INTRODUCTION
Factors peculiar to farming as an industry have been attributed to suicide by farmers across the various cultures.[1] Beginning in early 1990's, there has been a consistent rise in number of farmers' suicides in India.[2] An analysis of data from the National Crime Records Bureau of India reveals that in 12 years period from 1995 to 2006, approximately 200,000 farmers had committed suicides in India and situation has not improved since then.[3] With rising number of farmers' suicides, there is a large number of survivors left behind them. Suicide in a family triggers a wide range of negative outcomes.[4] High rates of anxiety, depression, and pathological grief along with difficulties in social life have been reported among suicide survivors.[5] Though suicide by farmers is reported as special category and studies are available on suicide victims, to the best of our knowledge, there are very few systematic studies focusing exclusively on “farmers” suicide survivors' across the world, and this is the first study from the Indian subcontinent.
Aims and objectives
The present study was undertaken with objective to assess the psychological distress and its correlates in survivors of farmers' suicides.
MATERIALS AND METHODS
This is a case–control study conducted from July 2008 to December 2009 in wardha District, located in Vidarbha region of Maharashtra State, one of the hotbeds of farmers' suicides.[2] Ethics Committee approval was obtained from the Institute ethics committee for research on human subjects, Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, India. A written informed consent was obtained in the local language (Marathi) from the subjects before participating in the study. A team of psychiatry resident and psychologist collected data by home visits.
Selection of survivors
One close relative of all 111 consecutive cases of suicides listed under farmers' suicide category in Wardha District that occurred from April 1, 2007, to March 31, 2008, was approached for participation in the study. This list was provided by the office of District Magistrate Wardha, Government of Maharashtra, India, on their official website.[6] One close relative was interviewed and assessed for the presence of psychological distress. The subject was asked whether he had any psychiatric illness or was on treatment for any mental health problems before the occurrence of suicide in family. If the answer was yes, then other survivor in family without such history was interviewed. In a situation where more than one eligible relative were present in home at the time of interview, preference was given to spouse, parent, sibling, offspring of deceased (above 18 years of age), and others in that order, respectively. Of the 111 families, ten were absent and neither could be assessed on first and nor on the second home visit. One family refused to participate in the study, while two suicide victims were not farmers by occupation so not included in the study. Thus, data were obtained from 98 suicide survivors.
Selection of controls
We selected 1:1 age (±2 years), sex, and occupation (farming) matched general population controls who were residing in the same village without a history of suicide by a close relative. Those with known psychiatric illness were excluded from the study. They were identified from the same lane where cases were residing. In a situation where eligible controls could not be identified or declined to participate in the study from the same lane, adjacent lanes were visited for selection of controls.
Interview technique
A predesigned and pretested semistructured questionnaire was used to record sociodemographic variables of suicide survivors and controls. Demographic variables such as age, sex, relationship with suicide victim, occupation, method of suicide, and any government help received were recorded. Economic status was ascertained by the color of ration card and reported income. The Government of India had issued yellow ration card to those families below poverty line and red colored card to those above poverty line. Psychological distress was measured using Indian version of Self-Reporting Questionnaire-20 (SRQ-20). Originally, it was a 25-item questionnaire devised by the World Health Organization to screen for the presence of psychiatric morbidity in primary health care setting, especially in developing countries. In its 20-item version, it is also used for the assessment of psychological distress.[7] It has a high face, content, criterion, and construct validity for adults (≥15 years) and can be used both as a self-rated or interviewer-administered questionnaire.[8] In the present study, SRQ-20 was interviewer administered (by psychiatry resident and psychologist who visited households) for all the participants in the study. Total SRQ-20 score is obtained by the sum of all positive responses. This instrument has been widely used in a variety of settings in different countries.[9,10,11,12] In a recent study in Pune, India, which is near to our center; sensitivity and specificity of SRQ-20 were reported to be 83% and 92%, respectively, using 10 as cutoff score.[13] Taking this as nearest validation study, we used total SRQ score of 10 as cutoff point, meaning those respondents scoring ≥10 were considered to be experiencing psychological distress.
Statistical analysis
Statistical differences between case and control groups were assessed using Chi-square test or Fisher's two-tailed exact test for class variables. For continuous variables, Student's t-test was used P < 0.05 was considered significant.
RESULTS
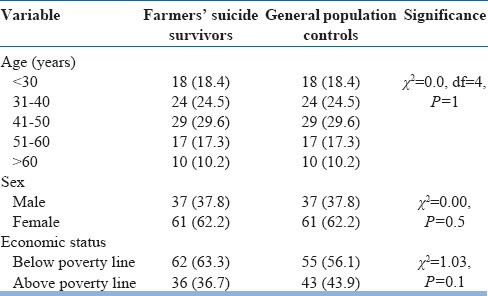
Overall response rate was 88.28%. Minimum and maximum intervals between the date of suicide and date of assessment were 7 months and 31 months, respectively. Eighty-one percent of the suicide victims were married with a male to female ratio of 8.8:1. An average number of survivors was 4 per suicide. Age of survivors and controls assessed in the study was almost evenly spread over 3–6th decade of life with very few younger or older than this. More females (62.2%) were assessed in the study than males [Table 1]. Among all relatives, spouse of suicide victims (48%) and parents (27.6%) were most frequently assessed in the study.
Table 1.
Sociodemographic details of farmers suicide survivors and controls
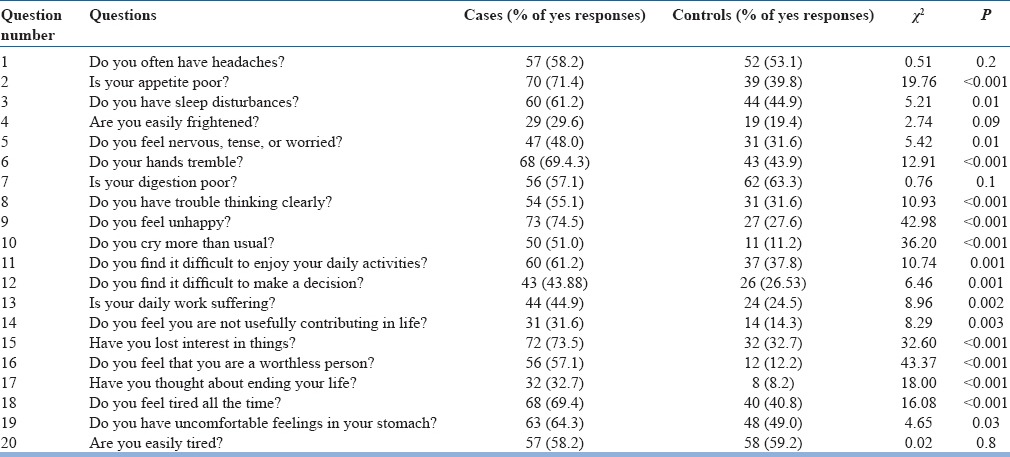
Sixty-one (62.2%) farmers' suicide survivors had psychological distress (total SRQ-20 score ≥10) compared to 20 (20.4%) of controls (odds ratio [OR] =6.3, 95% confidence interval [95% CI] =3.3–12.2, P < 0.001). This difference in psychological distress remains highly significant even if cutoff score of SRQ-20 is lowered to 8 (OR = 3.6, 95% CI = 2.0–6.7, P < 0.001) or increased to 12 (OR = 9.0, 95% CI = 4.4–19.3, P < 0.001). Nearly, one-third (30%) of the survivors had total SRQ-20 scores between 15 and 20 as compared to only 5% of the general population controls. Age of survivors did not have a significant correlation with the presence of psychological distress (χ2 = 6.8, df = 4, P = 0.1). Of all female survivors (n = 61), 78.69% were psychologically distressed compared to only 35.1% of all the male farmers' suicide survivors (risk ratio [RR] =2.2, 95% CI = 1.4–3.5, P < 0.001). Surviving spouses were significantly more likely to have psychological distress than other relatives of suicide victims (RR = 2.1, 95% CI = 1.4–2.9, P < 0.001). This high proportion of spouses of suicide victims having psychological distress than other relatives remains highly significant even when weighed for sex (RR = 3.76, 95% CI = 1.79–7.51, P = 0.002). There was no difference in psychological distress among those who were below or above poverty line (RR = 0.9, 95% CI = 0.6–1.3, P = 0.4). There was no significant difference in the presence of psychological distress in survivors of suicide victims who committed suicide by violent method as compared to survivors of those who used nonviolent method (RR = 1.04, 95% CI = 0.75–1.45, P = 0.3). Suicide survivors had significantly high proportion of yes responses compared to controls on all but four questions (having headaches, easily frightened, digestion problems, and getting easily tired). Most common expression of psychological distress among survivors was through symptoms of feeling unhappy (74%), loss of interest (73%), poor appetite (71%), tiredness (69%), trembling of hands (69%), and sleep disturbances (61%) followed by others [Table 2]. Nearly, one-third (32.7%) survivors confessed of having suicidal ideas within a month prior to assessment compared to 8% of the controls (OR = 5.4, 95% CI = 2.4–13.2, P < 0.01).
Table 2.
Comparison of affirmative (yes) responses to questions in Self Reporting Questionnaire-20 questionnaire between survivor and control groups
Only 45% of survivors had received some kind of government aid. There was no difference in the presence of psychological distress among those who did not receive government aid (Ex-gratia financial help) and those who received it (RR = 0.8, 95% CI = 0.36–1.91, P = 0.3).
DISCUSSION
Number of persons counted as survivors vary according to whether one includes only close relatives and friends or includes acquaintances and professional colleagues as well, but a conservative estimate counts about six survivors for every suicide.[14] In our study, average number of survivors per suicide was four. This included only family members and excluded close friends or work acquaintances. An American study revealed that surviving suicide is more prevalent than is realized. It reports that 7% people in the community had experienced the loss of someone by suicide during the previous year. In most cases, the suicide victims were friends or acquaintances, but in 3% they were members of their immediate family.[15] More numbers of females and spouses in the present study are due to preference given to the spouse of suicide victims (most victims were married men) for assessment of psychological distress. Suicide by a member results in series of negative outcomes in the family. Survivors of suicides in general are more prone for psychological distress.[9,16] Survivors experience elevated symptoms of anxiety, depression, and guilt and have substantial difficulties in social functioning. A qualitative research from South India shows that most families have financial problems and suicide in the family is stigmatizing and sometimes leads to social isolation.[17] On the other hand, the presence of psychological distress is associated with substantially increased socioeconomic dysfunction.[18] This compounding relationship between psychological distress and socioeconomic dysfunction leads to long-term impairments in family functioning delaying recovery of survivors from grief. After a period of heightened grief, families and survivors take years to cope with the loss. Thus, even after 2–3 years, farmers' suicide survivors were still experiencing significant psychological distress. Saarinen et al. had reported that even after 10 years suicide survivors had significantly more psychological morbidity than general population controls.[16] As found in our study, female survivors have been reported to experience more psychological distress than males in previous studies.[14,15,16]
Relationship of a survivor with suicide victim has a significant bearing on psychological distress. Spouse and parents are known to have higher psychological morbidity than other relatives of suicide victims.[16,17,18,19] Various explanations put forth for high vulnerability of spouse for psychological distress are trauma of loss of adult intimate relationship, guilt arising out of dyadic crisis, burden of taking care of children and other family responsibilities, experience of stigma, etc. These factors may be given due consideration when interventions are being planned to help suicide survivors. Survivors of suicide victims who used violent method of suicide have been reported to have higher psychological distress than survivors of suicides who used nonviolent method to commit suicide.[20] There was no significant difference in this study among these two groups. Psychological distress was commonly expressed through somatic and depressive symptoms. Early identification of these symptoms at primary care level may help in providing specific interventions at the earliest. Expression of suicide ideas by almost one-third of survivors was another alarming finding. Similar high proportion of survivors having suicide ideation was recently reported by McMenamy et al. in their study where a quarter of survivors have mild to moderate suicide intentions.[5] These high suicide ideations may be an indication of the severity of distress, lack of coping, lack of psychological help provided to them, or may be due to genetic factors as suicide behavior is known to run in the family.[21] Considering findings of present study, psychological interventions should be implemented at the earliest as mere financial help has not shown any impact on reducing psychological distress among farmers' suicide survivors.
CONCLUSIONS
Survivors of farmers' suicides have significantly higher psychological distress than controls. Female sex and being the spouse of suicide victim are significantly associated with the presence of psychological distress. Psychological distress is commonly expressed through somatic and depressive symptoms which may help in early identification of at-risk survivors. The current strategy of Indian Government to provide merely financial help to suicide households, though important in itself, does not seem to be working and a more comprehensive strategy involving psychological, social, and economic interventions is needed.
Limitations
There are several limitations in this study. We could make only cross-sectional comparisons between suicide survivors and controls. Our sample size is relatively small which may increase false negative findings (Type II error). We did not take into consideration coping methods and other stressful life events which may have an impact on psychological distress. Finally, this study measured only psychological distress without going into details of grief, depression, or other phenomenology.
Financial support and sponsorship
Study was funded by intramural grant by MGIMS Sevagram Wardha which was used for travel expenses. No external funding was received for the study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors would like to express gratitude toward Dr. RS Murthy for guidance and support for the study. We are thankful to all the staff at the Department of Psychiatry, MGIMS Sevagram, Wardha, for the support in the study.
REFERENCES
- 1.Behere PB, Bhise MC. Farmers' suicide: Across culture. Indian J Psychiatry. 2009;51:242–3. doi: 10.4103/0019-5545.58286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behere PB, Behere AP. Farmers' suicide in Vidarbha region of Maharashtra state: A myth or reality? Indian J Psychiatry. 2008;50:124–7. doi: 10.4103/0019-5545.42401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagaraja K. Farmers' Suicides in India: Magnitude, Trends and Partial Patterns. Madras Institute of Development Studies. 2007. [Last cited on 2008 Dec 12]. Available from: http://www.macroscan.com/anl/mar08/pdf/farmers_suicides.pdf .
- 4.Ratnarajah D, Schofield MJ. Survivors' narratives of the impact of parental suicide. Suicide Life Threat Behav. 2008;38:618–30. doi: 10.1521/suli.2008.38.5.618. [DOI] [PubMed] [Google Scholar]
- 5.McMenamy JM, Jordan JR, Mitchell AM. What do suicide survivors tell us they need? Results of a pilot study. Suicide Life Threat Behav. 2008;38:375–89. doi: 10.1521/suli.2008.38.4.375. [DOI] [PubMed] [Google Scholar]
- 6.Office of District Magistrate. List of Farmers' Suicides in Wardha District. 2008. [Last cited on 2008 Jun 10]. Available from: http://www.wardha.nic.in/en/htmldocs/gr/farmer-suicide.pdf .
- 7.Harding TW, deArango MV, Baltaker J, Climent CE, Ibrahim HH, Igansio LL, et al. WHO collaborative study on strategies for expanding mental health care II: The development of new research methods. Am J Psychiatry. 1983;140:1474–80. doi: 10.1176/ajp.140.11.1474. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. User's Guide to the Self Reporting Questionnaire. World Health Organization, Division of Mental Health Geneva, WHO/MNH/PSF/94.8, Division of Mental Health. 1994. [Last cited on 2008 Jun 12]. Available from: http://www.who.int/iris/handle/10665/61113#sthash.m93Vdx1b.dpuf .
- 9.Mari JJ, Williams P. A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Br J Psychiatry. 1986;148:23–6. doi: 10.1192/bjp.148.1.23. [DOI] [PubMed] [Google Scholar]
- 10.Sen B, Williams P. The extent and nature of depressive phenomenon in primary health care. Br J Psychiatry. 1987;45:406–49. doi: 10.1192/bjp.151.4.486. [DOI] [PubMed] [Google Scholar]
- 11.Harding TW, de Arango MV, Baltazar J, Climent CE, Ibrahim HH, Ladrido-Ignacio L, et al. Mental disorders in primary health care: A study of their frequency and diagnosis in four developing countries. Psychol Med. 1980;10:231–41. doi: 10.1017/s0033291700043993. [DOI] [PubMed] [Google Scholar]
- 12.Kishore J, Reddaiah VP, Kapoor V, Gill JS. Characteristics of mental morbidity in a rural primary health centre of Haryana. Indian J Psychiatry. 1996;38:137–42. [PMC free article] [PubMed] [Google Scholar]
- 13.Chincholkar SV. Use of SRQ in psychiatric epidemiology. Indian J Community Med. 2004;XXIX(4):190–1. [Google Scholar]
- 14.Sakinofsky I. The aftermath of suicide: Managing survivors' bereavement. Can J Psychiatry. 2007;52(6 Suppl 1):129S–36S. [PubMed] [Google Scholar]
- 15.Crosby AE, Sacks JJ. Exposure to suicide: Incidence and association with suicidal ideation and behavior: United States, 1994. Suicide Life Threat Behav. 2002;32:321–8. doi: 10.1521/suli.32.3.321.22170. [DOI] [PubMed] [Google Scholar]
- 16.Saarinen PI, Hintikka J, Lehtonen J, Lonnqvist JK, Viinamaki H. Mental health and social isolation among survivors ten years after a suicide in family: A case control study. Arch Suicide Res. 2002;6:221–6. [Google Scholar]
- 17.Manoranjitham S, Charles H, Saravanan B, Jayakaran R, Abraham S, Jacob KS. Perceptions about suicide: A qualitative study from Southern India. Natl Med J India. 2007;20:176–9. [PubMed] [Google Scholar]
- 18.Cardozo BL, Bilukha OO, Crawford CA, Shaikh I, Wolfe MI, Gerber ML, et al. Mental health, social functioning, and disability in postwar Afghanistan. JAMA. 2004;292:575–84. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
- 19.Séguin M, Lesage A, Kiely MC. Parental bereavement after suicide and accident: A comparative study. Suicide Life Threat Behav. 1995;25:489–92. [PubMed] [Google Scholar]
- 20.Barry LC, Kasl SV, Prigerson HG. Psychiatric disorders among bereaved persons: The role of perceived circumstances of death and preparedness for death. Am J Geriatr Psychiatry. 2002;10:447–57. [PubMed] [Google Scholar]
- 21.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families. A controlled family study of adolescent suicide victims. Arch Gen Psychiatry. 1996;53:1145–52. doi: 10.1001/archpsyc.1996.01830120085015. [DOI] [PubMed] [Google Scholar]


