Abstract
Background
Most women with histories of gestational diabetes mellitus do not receive a postpartum screening test for type 2 diabetes, even though they are at increased risk. The objective of this study was to identify factors associated with high rates of postpartum glucose screening.
Methods
This cross-sectional analysis assessed characteristics associated with postpartum diabetes screening for patients with gestational diabetes mellitus (GDM)-affected pregnancies self-reported by randomly sampled licensed obstetricians/gynecologists (OBs/GYNs) in Ohio in 2010.
Results
Responses were received from 306 OBs/GYNs (56.5% response rate), among whom 69.9% reported frequently (always/most of the time) screening women with GDM-affected pregnancies for abnormal glucose tolerance at the postpartum visit. Compared to infrequent screeners, OBs/GYNs who frequently screen for postpartum glucose tolerance were statistically (p < 0.05) more likely to have a clinical protocol addressing postpartum testing (67.2% vs. 26.7%), an electronic reminder system for providers (10.8% vs. 2.2%) and provide reminders to patients (16.4% vs. 4.4%). Frequent screeners were more likely to use recommended fasting blood glucose or 2-hour oral glucose tolerance test (61.8% vs. 34.6%, p < 0.001) than infrequent screeners.
Conclusions
Strategies associated with higher postpartum glucose screening for GDM patients included clinical protocols for postpartum testing, electronic medical records to alert providers of the need for testing, and reminders to patients.
Introduction
Gestational diabetes mellitus (GDM) affects 2%–10% of pregnant women in the United States.1 Approximately 30% of U.S. women with GDM continue to have abnormal results on fasting plasma glucose or impaired glucose tolerance tests (GTTs) after delivery.2,3 In the decades following a GDM pregnancy, these women are at higher risk of developing cardiovascular disease4 and up to 70% may develop type 2 diabetes mellitus.5,6 Therefore, women with histories of GDM are at high risk for developing type 2 diabetes and should be tested for abnormal glucose tolerance postpartum and in subsequent years.7,8 Although postpartum testing is needed to rule out type 2 diabetes after delivery, studies using data from medical centers9–11 and health care organizations12 have found that an estimated 50% to 80% of women with GDM do not receive a postpartum test for type 2 diabetes. To date, surveys of health care providers have not assessed clinical factors that are associated with the highest postpartum testing rates.
In addition, to our knowledge, surveys have not assessed whether providers counsel women with GDM affected pregnancies on their future testing needs or on lifestyle prevention activities. Since the onset of type 2 diabetes may be prevented or delayed through nutrition, exercise, maintenance of a healthy weight, and breastfeeding,13–15 the post-partum visit is an opportunity not only to educate women with recent GDM-affected pregnancies on their increased risk of type 2 diabetes, but also to provide counseling on the importance of physical activity and make referrals to appropriate nutrition resources. Both the American Diabetes Association (ADA) and the American College of Obstetricians and Gynecologists (ACOG) recommend lifestyle counseling for women with GDM-affected pregnancies. The ADA recommends that all women with a history of GDM should be educated about lifestyle modification whereas ACOG recommends that women with risk factors, such as obesity, receive diet, exercise, and weight-management counseling.7,8 It is also recommended that women with a past GDM-affected pregnancy be screened prior to another pregnancy.16 Health care providers have previously reported barriers to postpartum screening for GDM patients, such as poor knowledge of guidelines among health care providers, inconsistent guidelines, limited communications between obstetricians/gynecologists (OBs/GYNs) and primary care physicians, poor documentation of patients’ GDM status, patients lost to follow-up, and patient inconvenience.17,18
Prevention and detection of type 2 diabetes is a priority for Ohio, where GDM affects an estimated 9000 pregnancies per year.19 The Ohio Department of Health was interested in identifying opportunities to improve risk reduction education and follow-up to prevent or delay type 2 diabetes among women who have recent histories of GDM. Thus, our study sought to assess what provider characteristics and practices were associated with higher rates of postpartum testing for GDM and to estimate the prevalence of lifestyle modification counseling or referrals for women with GDM by Ohio’s OBs/GYNs.
Materials and Methods
We developed a 37-item questionnaire on clinical practitioners’ knowledge, attitudes, and postpartum practices regarding diabetes prevention for women with a history of GDM. The questionnaire required approximately 15 minutes to complete, was reviewed for face validity, and was piloted with 5 OBs/GYNs, 5 certified nurse-midwives, and 4 family medicine physicians. We selected a random sample of 700 from 1327 OBs/GYNs who had current certifications listed in public access state licensure files that were not part of the pilot tests. Internal medicine physicians, family medicine physicians, and certified nurse midwives were also sampled for the survey. This manuscript will focus on findings specific to OBs/GYNs. From October through December 2010, we surveyed selected OBs/GYNs using a dual-mode (mail and internet) approach to optimize response rates.20 OBs/GYNs who had retired, moved out of state, or indicated that they did not practice postpartum care were excluded (n = 84). A postcard was first mailed to the sample of OBs/GYNs to notify them of the forthcoming survey. The paper questionnaire was then mailed one week later, with a description of options to complete the survey online or to return it by mail. Reminder postcards were sent a week later, followed in one week by duplicate surveys, mailed only to non-responders. Reminders were sent to non-responders if the duplicate survey was not returned within two weeks. If mailings were returned undeliverable, attempts were made to find correct addresses. The response rate was 56.5% (n = 348/616), but 42 were further excluded due to missing data on frequency of postpartum screening, leaving 306 in the analytic sample.
Data were directly entered if the surveys were completed online or otherwise entered via Teleform software and analyzed using STATA 10.0 (StataCorp, 2007). OBs/GYNs were considered frequent screeners if they reported that they screen for postpartum glucose tolerance always or most of the time and infrequent screeners if they sometimes, rarely, or never screened. We used Chi-square tests to assess statistical differences for categorical variables by frequency of postpartum screening. The survey underwent research determination by the Centers for Disease Control and Prevention and was considered to be public health practice; thus, exempted from IRB approval.
Results
Characteristics of surveyed obstetricians/ gynecologists
Among all OBs/GYNs, the mean time in practice was 16.2 years (Table 1). Half of OBs/GYNs were female. Most (73.5%) reported working in a private group, and 22.1% reported that more than half of their patients were Medicaid-insured. The majority of OBs/GYNs saw 6 to 10 pregnant patients (40.5%) or 11 to 20 pregnant patients (37.8%) per month.
Table 1.
Characteristics of Surveyed Obstetricians/ Gynecologists in Ohio by Frequency of Postpartum Screening
| Characteristics | Total (n = 306) | Frequent screeners (n = 214) | Infrequent screeners (n = 92) | |
|---|---|---|---|---|
| Years in practice, mean (SE) | 16.2 (9.8) | 15.6 (9.3) | 17.0 (9.7) | |
| % | % | % | Chi-square p-value | |
| Sex | ||||
| Female | 49.8 | 53.8 | 40.5 | 0.04 |
| Male | 50.2 | 46.2 | 59.6 | |
| Primary practice type | ||||
| Private group | 73.5 | 69.2 | 83.5 | 0.12 |
| Government funded clinic | 3.3 | 3.8 | 2.2 | |
| Hospital | 10.6 | 12.8 | 5.5 | |
| University | 10.3 | 11.9 | 6.6 | |
| Other (includes HMO) | 2.3 | 2.4 | 2.2 | |
| Percent of patients insured by Medicaid | ||||
| 0%–25% | 38.7 | 39.0 | 37.8 | 0.49 |
| 26%–50% | 39.0 | 37.4 | 42.7 | |
| 51%–75% | 15.2 | 15.0 | 15.9 | |
| > 75% | 7.1 | 8.6 | 3.7 | |
| New pregnancies typically seen each month | ||||
| 1–5 | 9.9 | 8.7 | 12.5 | 0.80 |
| 6–10 | 40.5 | 41.3 | 38.6 | |
| 11–20 | 37.8 | 37.9 | 37.5 | |
| ≥ 21 | 11.9 | 12.1 | 11.4 | |
HMO, health maintenance organization; SE, standard error.
Approximately 70% of OBs/GYNs reported frequently screening for abnormal glucose tolerance at the postpartum visit after a GDM pregnancy (69.9%) compared with 30.1% of OBs/GYNs who reported infrequently screening. Those who frequently screened were more likely to be female and more often reported African Americans and Hispanics as one of their predominant patient race/ethnicities (p < 0.05 for each; data not shown). There were no differences in postpartum screening rates by percent of practice that was Medicaid, primary population location (rural/suburban/urban), or the number of new pregnancies typically seen each month.
Knowledge and attitudes of obstetricians/ gynecologists
Compared with OBs/GYNs who infrequently screen, those who frequently screen for postpartum glucose tolerance were more likely to consider screening a high priority for their practice (25.5% vs. 13.3%), to correctly estimate future type 2 diabetes risk as over 40% (33.6% vs. 23.1%), and to strongly agree that GDM has long-term implications (81.6% vs. 69.2%) and that there is a need for periodic screening for type 2 diabetes among women with GDM histories (65.9% vs. 50.6%; Table 2).
Table 2.
Knowledge and Attitudes of Obstetricians/Gynecologists in Ohio by Frequency of Postpartum Screening
| Questionnaire items | Total (n = 306) % | Frequent screeners (n = 214) % | Infrequent screeners (n = 92) % | Chi-square p value |
|---|---|---|---|---|
| Screening for type 2 diabetes among non-pregnant women with a history of GDM is a __ priority in my practice. | ||||
| High | 21.8 | 25.5 | 13.3 | < 0.001 |
| Moderate | 37.6 | 42.8 | 25.6 | |
| Low | 40.6 | 31.7 | 61.1 | |
| Percent of women with GDM pregnancies will progress to type 2 diabetes within 10 years? | ||||
| > 40% | 30.5 | 33.6 | 23.1 | < 0.001 |
| ≤ 40% | 65.3 | 64.9 | 65.9 | |
| Unsure | 4.3 | 1.4 | 11.0 | |
| GDM has long term implications for a woman’s health. | ||||
| Strongly agree | 77.9 | 81.6 | 69.2 | 0.08 |
| Somewhat agree | 20.5 | 17.5 | 27.5 | |
| Disagree | 1.0 | 0.5 | 2.2 | |
| Unsure | 0.7 | 0.5 | 1.1 | |
| There is a need for periodic screening for type 2 diabetes among women with a history of GDM. | ||||
| Strongly agree | 61.3 | 65.9 | 50.6 | 0.02 |
| Somewhat agree | 30.5 | 28.4 | 35.2 | |
| Disagree | 3.3 | 2.8 | 4.4 | |
| Unsure | 4.9 | 2.8 | 9.9 | |
GDM, Gestational diabetes mellitus.
Clinical practices and strategies
Compared with OBs/GYNs who infrequently screen patients for abnormal glucose tolerance at the postpartum visit, OBs/GYNs who frequently screen patients were more likely to say that they discussed postpartum testing for type 2 diabetes, informed women that they are at increased risk for type 2 diabetes, and recommended testing for type 2 diabetes before a future pregnancy (Table 3; p < 0.001). They also were more likely to report counseling women to exercise regularly and referring overweight or obese postpartum women for diet support or nutritional counseling (p < 0.001).
Table 3.
Clinical Practices by Obstetricians/Gynecologists in Ohio by Frequency of Postpartum Screening
| Questionnaire items | Total (n = 306) % | Frequent screeners (n = 214) % | Infrequent screeners (n = 92) % | Chi-square p value |
|---|---|---|---|---|
| If a woman has GDM, I discuss her plans for follow-up postpartum care for testing of type 2 diabetes. | ||||
| Always/most times | 87.1 | 95.6 | 67.1 | < 0.001 |
| Some of the time | 8.5 | 3.9 | 19.3 | |
| Never/rarely | 4.4 | 0.5 | 13.6 | |
| Postpartum women with a recent history of GDM are told that they are at an increased risk for type 2 diabetes. | ||||
| Always/most times | 91.8 | 97.2 | 79.4 | < 0.001 |
| Some of the time | 7.3 | 2.8 | 17.4 | |
| Never/rarely | 1.0 | 0.0 | 3.3 | |
| In addition to routine screening, postpartum women with a recent history of GDM are told that they should be tested for diabetes when considering having another child or becoming pregnant in the future. | ||||
| Always/most times | 80.6 | 87.2 | 65.2 | < 0.001 |
| Some of the time | 11.5 | 9.0 | 17.4 | |
| Never/rarely | 7.8 | 3.8 | 17.4 | |
| Postpartum women with a recent history of GDM are counseled to exercise regularly. | ||||
| Always/most times | 75.1 | 81.7 | 59.8 | < 0.001 |
| Some of the time | 17.4 | 15.0 | 22.8 | |
| Never/rarely | 7.5 | 3.3 | 17.4 | |
| Overweight or obese postpartum women with a recent history of GDM are referred to a diet support group or other nutrition counseling. | ||||
| Always/most times | 39.5 | 43.0 | 31.5 | 0.02 |
| Some of the time | 31.1 | 32.2 | 28.3 | |
| Never/rarely | 29.4 | 24.8 | 40.2 |
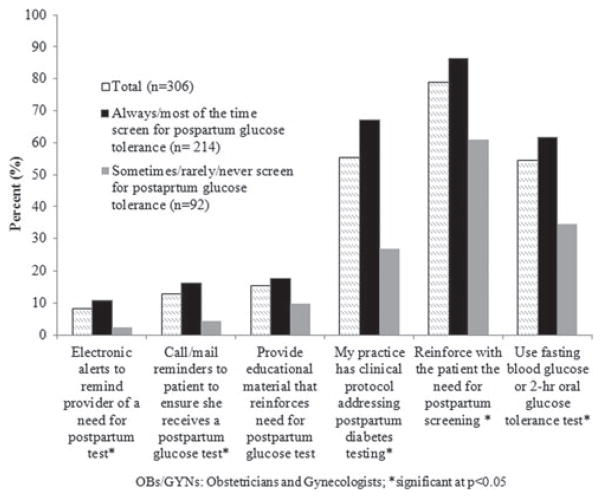
Overall, the most commonly used GTT was the 2-hour oral GTT (50.7% of all responding OBs/GYNs), followed by other tests (20.7%), self-monitoring (11.4%), hemoglobin A1c (9.7%), fasting blood sugar (3.8%), and random glucose (3.8%) (data not shown). Over half of OBs/GYNs reported using one of the two ACOG and ADA recommended postpartum GTTs,7,8 either the fasting blood sugar or the oral GTT test, as their primary test for glucose tolerance, while 45.5% used tests that do not meet recommended standards of care (Fig. 1). OBs/ GYNs who frequently screen were more likely to use a recommended GTT than OBs/GYNs who infrequently screen (61.8% vs. 34.6%; p < 0.001).
FIG. 1.
Strategies used by obstetricians/gynecologists (OBs/ GYNs) to ensure that women with gestational diabetes mellitus receive a postpartum glucose tolerance test. *p < 0.05.
Reinforcing the need for postpartum GTT with patients (Fig. 1) was the most common strategy reported for ensuring that women with GDM receive a postpartum screening. Over half of all OBs/GYNs had a clinical protocol that addresses postpartum diabetes screening. Fewer than 20% of OBs/ GYNs offered educational material to the patients (15.4%), called or mailed reminders to patients (12.8%), or used electronic medical record alerts (i.e., electronic reminder systems) (8.2%). OBs/GYNs who frequently screened were more likely to reinforce with the patient the need for postpartum screening, have a clinical protocol addressing postpartum screening, call or mail reminders to patients, or use electronic medical record alerts (p < 0.01 for all).
Discussion
Nearly 7 of 10 OBs/GYNs in Ohio reported frequently screening for glucose tolerance after a GDM pregnancy. Those who screened frequently were more likely to provide the recommended follow up care than those who did not screen frequently. For example, they were more likely to use the appropriate type of glucose test and to follow ADA and ACOG postpartum care recommendations for women with a recent GDM-affected pregnancy that stress the importance of lifestyle counseling to prevent the development of future type 2 diabetes. Thus, our study suggests that screening is associated with the provision of higher quality of care. However, we do not know what led to this higher quality of care. Possible explanations include mandates by administrators/ clinical directors or exposure to new ACOG guidelines and/or training.
The postpartum screening prevalence reported in our study (69.9%) is greater than the prevalence in another statewide survey in North Carolina, which found that only 21% of responding OBs/GYNs, family practice physicians, and nurse-midwives screened for type 2 diabetes during post-partum visits.17 Our prevalence is similar to a national survey of ACOG Fellows and Junior Fellows, in which approximately 74% of obstetricians stated that they routinely perform post-partum evaluations of glucose tolerance in patients diagnosed with GDM.21 The ACOG survey and our survey relied on self-reported provider practices, while screening rates are generally lower in studies that use hospital records with documentation of test results (range 38%–58%).11,12 This discrepancy may be attributed to a recent increased awareness of the importance of postpartum screening since the studies using hospital records were published before the 2009 ACOG guidelines, or more likely, it may reflect a reporting bias and be an overestimate of the true percent of OBs/GYNs who regularly screen for postpartum glucose intolerance.
Only half of the OBs/GYNs who responded to our survey reported that they use either the oral GTT test or the fasting blood sugar for postpartum screening. ACOG guidelines state that while the oral GTT has greater sensitivity than the fasting blood sugar test, both are acceptable postpartum screening tests.7,8 The percent of OBs/GYNs reporting that they use an appropriate test is similar to estimates from other studies that found 54% of providers in North Carolina17 and 51% of ACOG fellows use the oral GTT.21 The percentage of providers using either test in clinic and health center studies is lower, ranging from 17% to 45%.2,3,10,11,22 Hemoglobin A1c was used as a postpartum test for diabetes by 9.7% of respondents in this study; although this test has been approved for use as a GTT among the general population, it has not been validated among postpartum women. Increased use of appropriate postpartum tests can be achieved with ongoing provider education.
While the ADA recommends that all women with a history of GDM should be educated about lifestyle modification,8 many OBs/GYNs in this study did not routinely counsel women to exercise regularly or refer overweight/obese postpartum women to a diet support group or other nutrition counseling. This finding may be due to the lack of coverage for obesity treatment by the Medicaid program in Ohio.23 Exercise and weight loss have been shown to effectively prevent or delay the onset of type 2 diabetes.13 Furthermore, overweight/obese women who have recent histories of GDM are at greater risk of developing type 2 diabetes in the future.6
In this study, a clinical protocol for postpartum testing and automatic reminders within electronic medical record systems were associated with providers who reported frequently screening women for glucose intolerance postpartum. Studies have documented that postpartum screening rates can improve with patient education and counseling,24 mailed reminders to the patient and her health practitioner,25 and use of a case-manager nurse to follow up patients during and after pregnancy.26 Use of reminder systems (electronic or automated) for patients has been shown to improve patient compliance with screening for other types of tests, such as mammography and colon cancer, and would likely improve postpartum diabetes screening as well.27,28 In recent studies from Canada and Finland, postpartum women who received a reminder call were almost twice as likely to have a post-partum GTT than women who received usual care, with no reminder call.29,30 Given the low percent of reminder calls or mailings, educational materials, and electronic alerts reported by OBs/GYNs in our survey, increased use of these strategies may improve postpartum type 2 diabetes screening rates among OBs/GYNs in Ohio.
This study has several limitations. First, these data are based on self-reporting and could be subject to social desirability bias. Additionally, OBs/GYNs who completed the survey are likely to be more interested in GDM compared with those who did not, and thus, the responders may be more informed of and more likely to follow recommended guidelines in their care of women with recent histories of GDM compared with non-responders. Therefore, results from this survey may not be representative of all licensed OBs/ GYNs in Ohio or other states.
Despite these limitations, this study’s use of a dual-mode survey design may have allowed us to capture more respondents than a standard mail or phone survey alone. Approximately 17% of OBs/GYNs responded through the Internet. Although the response rate (56.5%) is moderate, it is relatively high compared with other surveys of physicians, which typically have response rates of 40% or less.17,21 Unlike many prior surveys, where only one medical center or academic institution is examined, our survey sampled OBs/ GYNs across the state, in a variety of practice settings, enabling us to capture clinical practices in many locations. Additionally, we surveyed providers about clinical characteristics, type of postpartum glucose test used, and level of lifestyle counseling provided to patients in order to identify strategies to improve the care of women with recent histories of GDM.
In summary, our study found some strategies were associated with higher postpartum glucose screening for GDM patients including clinical protocols for postpartum testing, electronic medical records to alert providers of the need for testing, and reminders to patients. We also found that OBs/ GYNs who frequently conducted postpartum screening for women affected by GDM are valued advocates and counselors for prevention as postpartum women transition to primary care.
Acknowledgments
The authors would like to thank the following individuals for their contributions to this study: Ryan Kofran, MSSA, CNM, Case Western University; Andrew Wapner, DO, Ohio Department of Health; Norma Ryan, PhD, RN, Ohio Department of Health; Amy Dunn, RN, Ohio Department of Health; Gwen Stacey, RD, Ohio Department of Health; Thomas Joyce, MA, Ohio Department of Health; Karen Foster, Ohio Department of Health; and Jessica Londeree, Ohio Department of Health. Funding for this work was provided by the U.S. Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure Statement
No competing financial interests exist.
References
- 1.Hunt KJ, Schuller KL. The increasing prevalence of diabetes in pregnancy. Obstet Gynecol Clin North Am. 2007;34:173–199. doi: 10.1016/j.ogc.2007.03.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaefer-Graf UM, Buchanan TA, Xiang AH, Peters RK, Kjos SL. Clinical predictors for a high risk for the development of diabetes mellitus in the early puerperium in women with recent gestational diabetes mellitus. Am J Obstet Gynecol. 2002;186:751–756. doi: 10.1067/mob.2002.121895. [DOI] [PubMed] [Google Scholar]
- 3.Retnakaran R, Qi Y, Sermer M, Connelly PW, Hanley AJ, Zinman B. Glucose intolerance in pregnancy and future risk of pre-diabetes or diabetes. Diabetes Care. 2008;31:2026–2031. doi: 10.2337/dc08-0972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah BR, Retnakaran R, Booth GL. Increased risk of cardiovascular disease in young women following gestational diabetes. Diabetes Care. 2008;31:1668–1669. doi: 10.2337/dc08-0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Sullivan J. Subsequent morbidity among gestational diabetic women. In: Southerland HW, Stowers J, editors. Carbohydrate metabolism in pregnancy and the newborn. Edinburgh: Churchill Livingstone; 1984. pp. 174–180. [Google Scholar]
- 6.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care. 2002;25:1862–1868. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 7.American College of Obstetricians and Gynecologists Committee. Opinion No. 435: Postpartum screening for abnormal glucose tolerance in women who had gestational diabetes mellitus. Obstet Gynecol. 2009;113:1419–1421. doi: 10.1097/AOG.0b013e3181ac06b6. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34:S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almario CV, Ecker T, Moroz LA, Bucovetsky L, Berghella V, Baxter JK. Obstetricians seldom provide postpartum diabetes screening for women with gestational diabetes. Am J Obstet Gynecol. 2008;198:528, e1–5. doi: 10.1016/j.ajog.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Smirnakis KV, Chasan-Taber L, Wolf M, Markenson G, Ecker JL, Thadhani R. Postpartum diabetes screening in women with a history of gestational diabetes. Obstet Gynecol. 2005;106:1297–1303. doi: 10.1097/01.AOG.0000189081.46925.90. [DOI] [PubMed] [Google Scholar]
- 11.Kim C, Tabaei BP, Burke R, et al. Missed opportunities for type 2 diabetes mellitus screening among women with a history of gestational diabetes mellitus. Am J Public Health. 2006;96:1643–1648. doi: 10.2105/AJPH.2005.065722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dietz PM, Vesco KK, Callaghan WM, et al. Postpartum screening for diabetes after a gestational diabetes mellitus-affected pregnancy. Obstet Gynecol. 2008;112:868–874. doi: 10.1097/AOG.0b013e318184db63. [DOI] [PubMed] [Google Scholar]
- 13.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE, Michels KB. Duration of lactation and incidence of type 2 diabetes. JAMA. 2005;294:2601–2610. doi: 10.1001/jama.294.20.2601. [DOI] [PubMed] [Google Scholar]
- 15.Bentley-Lewis R, Levkoff S, Stuebe A, Seely EW. Gestational diabetes mellitus: Postpartum opportunities for the diagnosis and prevention of type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2008;4:552–558. doi: 10.1038/ncpendmet0965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007;30(Suppl 2):S251–S260. doi: 10.2337/dc07-s225. [DOI] [PubMed] [Google Scholar]
- 17.Baker AM, Brody SC, Salisbury K, Schectman R, Hartmann KE. Postpartum glucose tolerance screening in women with gestational diabetes in the state of North Carolina. N C Med J. 2009;70:14–19. [PubMed] [Google Scholar]
- 18.Stuebe A, Ecker J, Bates DW, Zera C, Bentley-Lewis R, Seely E. Barriers to follow-up for women with a history of gestational diabetes. Am J Perinatol. 2010;27:705–710. doi: 10.1055/s-0030-1253102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohio Department of Health. The Ohio gestational diabetes mellitus (GDM) collaboration: Working to prevent or delay type 2 diabetes among women with a history of gestational diabetes. [Accessed July 7, 2011];2011 Available at: http://www.odh.ohio.gov/*/media/ODH/ASSETS/Files/hprr/diabetes%20prevention%20prevention%20and%20control/ohiogestationaldiabetesmellitusgdmcollaboration.ashx.
- 20.Dillman DA. Mail and internet surveys: The tailored design method. New York: Wiley; 2000. [Google Scholar]
- 21.Gabbe SG, Gregory RP, Power ML, Williams SB, Schulkin J. Management of diabetes mellitus by obstetrician-gynecologists. Obstet Gynecol. 2004;103:1229–1234. doi: 10.1097/01.AOG.0000128045.50439.89. [DOI] [PubMed] [Google Scholar]
- 22.Russell MA, Phipps MG, Olson CL, Welch HG, Carpenter MW. Rates of postpartum glucose testing after gestational diabetes mellitus. Obstet Gynecol. 2006;108:1456–1462. doi: 10.1097/01.AOG.0000245446.85868.73. [DOI] [PubMed] [Google Scholar]
- 23.Ohio Medicaid Program. [Accessed May 25, 2012];2012 Available at: http://jfs.ohio.gov/ohp/index.stm.
- 24.Stasenko M, Liddell J, Cheng YW, Sparks TN, Killion M, Caughey AB. Patient counseling increases postpartum follow-up in women with gestational diabetes mellitus. Am J Obstet Gynecol. 2011;204:522, e1–6. doi: 10.1016/j.ajog.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clark HD, Graham ID, Karovitch A, Keely EJ. Do postal reminders increase postpartum screening of diabetes mellitus in women with gestational diabetes mellitus? A randomized controlled trial. Am J Obstet Gynecol. 2009;200:634, e1–7. doi: 10.1016/j.ajog.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Hunt KJ, Conway DL. Who returns for postpartum glucose screening following gestational diabetes mellitus? Am J Obstet Gynecol. 2008;198:404, e1–4. doi: 10.1016/j.ajog.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mosen DM, Feldstein AC, Perrin N, et al. Automated telephone calls improved completion of fecal occult blood testing. Med Care. 2010;48:604–610. doi: 10.1097/MLR.0b013e3181dbdce7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldstein AC, Perrin N, Rosales AG, et al. Effect of a multimodal reminder program on repeat mammogram screening. Am J Prev Med. 2009;37:94–101. doi: 10.1016/j.amepre.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Korpi-Hyovalti E, Laaksonen DE, Schwab U, Heinonen S, Niskanen L. How can we increase postpartum glucose screening in women at high risk for gestational diabetes mellitus? Int J Endocrinol. 2012;2012:6. doi: 10.1155/2012/519267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shea AKSB, Clark HD, Malcolm J, Walker M, Karovitch A, Keely EJ. The effectiveness of implementing a reminder system into routine clinical practice: Does it increase post-partum screening in women with gestational diabetes? Chronic Dis Can. 2011;31:58. [PubMed] [Google Scholar]