Abstract
Background
Paraquat and diquat are among the most commonly used herbicides in the world.
Objectives
Determine the magnitude, characteristics, and root causes for acute paraquat- and diquat-related illnesses in the US
Methods
Illnesses associated with paraquat or diquat exposure occurring from 1998 through 2011 were identified from the Sentinel Event Notification System for Occupational Risks (SENSOR)-Pesticides Program, the California Department of Pesticide Regulation (CDPR) Pesticide Illness Surveillance Program (PISP), and the Incident Data System (IDS). Cases identified by the National Poison Data System (NPDS) were reviewed for the years 1998–2003 and 2006–2013.
Results
A total of 300 paraquat- and 144 diquat-related acute illnesses were identified by SENSOR, PISP, and IDS. NPDS identified 693 paraquat- and 2128 diquat-related acute illnesses. In SENSOR/PISP/IDS, illnesses were commonly low severity (paraquat=41%; diquat=81%); however, SENSOR/PISP/IDS identified 24 deaths caused by paraquat and 5 deaths associated with diquat. Nineteen paraquat-related deaths were due to ingestion, seven of which were unintentional, often due to improper storage in beverage bottles. In SENSOR/PISP/IDS, paraquat and diquat-related acute illnesses were work-related in 68% (n=203) and 29% (n=42) of cases, respectively. When herbicide application site was known, the vast majority of acute paraquat-related illnesses (81%) arose from agricultural applications. Common root causes of illness were failure to use adequate personal protective equipment (PPE), application equipment failure, and spill/splash of herbicide.
Conclusions
Although the magnitude of acute paraquat/diquat-related illnesses was relatively low, several fatalities were identified. Many illnesses could be prevented through stricter compliance with label requirements (e.g. ensuring proper herbicide storage and PPE use), and through enhanced training of certified applicators.
Keywords: Paraquat, Diquat, Pesticides, Acute Poisonings, Surveillance
1. Introduction
Paraquat, a non-selective contact herbicide and desiccant, was first registered in the United States (US) in 1964. It is currently approved for use in nearly 90 countries and is one of the most commonly used herbicides worldwide (Paraquat Information Center, 2014). In the US, products containing paraquat are classified as “restricted use” pesticides due to their high toxicity, meaning they can only be purchased and used by certified applicators or by those working under their direct supervision (USEPA, 1997). The lethal dose (LD50) of paraquat in humans is 20–40 mg ion/kg of body weight, which is 1.2–2.4 US teaspoons of a paraquat product with a 30% concentration (Vale et al., 1987). Contact with paraquat via inhalation, ingestion, ocular, or skin routes of exposure can cause severe health effects including pulmonary fibrosis, pulmonary edema, erythema, dermatitis, ulceration of the mouth, and brain damage (Roberts and Reigert, 2013). Given its strong irritant properties, handlers (i.e. mixers, loaders, and applicators) are required to take precautions to prevent skin and eye exposure and to prevent splashes into the mouth by adopting engineering controls or using personal protective equipment (PPE) including chemical resistant gloves, eye protection, and an air-purifying respirator (USEPA, 1997). In California, a closed system is required when mixing and loading paraquat (closed systems are devices designed to prohibit the escape of the pesticide outside the system, thereby preventing exposure to a handler). Due to its high toxicity, paraquat has not been approved for use in the European Union since 2007 (The Court of First Instance Annuls, 2007) and is banned or not registered in at least seven other countries (Watts, 2011).
Diquat dibromide, like paraquat, is in the dipyridyl chemical class and is also a non-selective contact herbicide and desiccant that was first registered for use in the US in 1986 (Roberts and Riegert, 2013). With an oral LD50 of 231 mg/kg in rats, diquat is considered to be less toxic than paraquat (the oral paraquat LD50 is 150 mg/kg in rats) (WHO, 2005). Products containing diquat are not classified as restricted use and are available for purchase to non-professionals (USEPA, 1995). Exposure to diquat causes corrosive effects to tissue, including the skin and gastrointestinal tract (Jones and Vale, 2000). Systemic toxicity, including kidney failure and central nervous system toxicity, is usually associated with diquat ingestion. Unlike paraquat, diquat is not selectively concentrated in the lung (Rose and Smith, 1977) and is not known to directly cause pulmonary fibrosis (Vanholder et al., 1981; Jones and Vale, 2000).
Despite their high toxicity and availability for purchase over multiple decades, little information on the magnitude, characteristics, and root causes for acute paraquat and diquat-related illnesses in the US is available. The purpose of this study is to address this gap.
2. Methods
2.1. Data sources
Data from three systems were combined to identify cases of acute paraquat and diquat-related illnesses and to assess their characteristics and root causes: the National Institute for Occupational Safety and Health (NIOSH) Sentinel Event Notification System for Occupational Risks (SENSOR)-Pesticides Program; the California Department of Pesticide Regulation (CDPR) Pesticide Illness Surveillance Program (PISP); and, the US Environmental Protection Agency (EPA), Office of Pesticide Programs’ (OPP) Incident Data System (IDS). In addition, data from a fourth separate system that is national in scope were also assessed: the National Poison Data System (NPDS) maintained by the American Association of Poison Control Centers (AAPCC). Because few details were available on NPDS cases, they were not cross-referenced with cases from the other three data sources. As such, NPDS data were used only to assess the national magnitude and trend of acute paraquat- and diquat-related illness. Given the likely overlap in cases between NPDS and the other data systems, NPDS findings should be considered separately and not be combined with data from the other three systems. Because all personal identifiers were removed from the data prior to NIOSH submission, this study was exempt from consideration by the federal Institutional Review Board.
The SENSOR-Pesticides program has collected pesticide poisoning data from state health departments using standardized definitions and variables since 1998 (Calvert et al., 2008). Data for this study were provided by the following 11 states: California Department of Public Health (CDPH) (1998–2011), Florida Department of Health (1998–2011), Iowa Department of Public Health (2006–2011), Louisiana Department of Health and Hospitals (2000–2011), Michigan Department of Community Health (2000–2011), New Mexico Department of Health (2005–2008), New York State Department of Health (1998–2011), North Carolina Department of Health and Human Services (2007 –2011), Oregon Department of Human Services (1998–2011), Texas Department of State Health Services (1998–2011), and Washington State Department of Health (2001–2011).
In California, two programs identify cases of acute pesticide-related illness/injury: CDPH, a SENSOR-Pesticides participant; and, the Pesticide Illness Surveillance Program (PISP), which is administered by the California Department of Pesticide Regulation (CDPR). PISP operates similarly to the SENSOR-Pesticides program, but there are differences in the case definition and the variables used to characterize cases. PISP does not formally participate in the SENSOR-Pesticides program, but collaborates on joint activities (e.g. manuscripts) (Calvert et al., 2010). CDPH collects only work-related cases, while PISP collects data for both work-related and non-work-related acute pesticide-related illness/injury. An illness is considered work-related if the pesticide exposure occurred at the case’s place of work. To ensure California cases were counted only once, CDPH cross-referenced its cases with those from PISP using name, date of illness/injury, social security number and date of birth. A total of 28 California cases were identified by both programs and counted only once. All other SENSOR-Pesticides states collect data on both work-related and non-work-related acute pesticide-related illness/injury, except New Mexico and Iowa (only work-related cases).
SENSOR-Pesticides and PISP case ascertainment sources primarily are poison control centers (PCC), other government agencies (such as a state’s Department of Agriculture), workers’ compensation documents, and physician reports. Staff from state surveillance programs attempt to interview cases and review medical records, and use standardized variables to systematically code all information about a case (CDC, 2005).
IDS began in 1992 and is a national database of alleged or anecdotal human health incidents. Under FIFRA Section 6a2, pesticide registrants are required to submit all eligible incident reports they receive to EPA. Incident reports are submitted primarily by pesticide registrants, but some are also submitted by other sources such as government and non-governmental organizations (USEPA, 2007). For this report, fatal, high, and moderate severity paraquat incidents reported in IDS between 1998 and 2011 were identified and included. IDS data for diquat were unavailable for this paper because they were under review in the EPA reregistration process. NIOSH used information from IDS reports to populate SENSOR-Pesticides variables. To ensure IDS cases were counted only once, IDS cases were cross-referenced with those from SENSOR-Pesticides and PISP using date of illness, date of birth, and case narrative. A total of 4 cases were identified by IDS and another program, and were counted only once.
NPDS data for the years 1998–2003 and 2006–2013 were available to NIOSH (the cost to access additional NPDS data was prohibitive). NPDS stores the data provided by the nation’s 57 PCCs (Mowry et al., 2014). Only symptomatic exposures occurring in the US or Puerto Rico were included. In 2006–2013, cases with intentional exposures (e.g. suicides, attempted suicides, malicious intent) were not available to the authors; however these cases generally account for fewer than 5% of NPDS-captured paraquat and diquat cases (Bronstein et al., 2012).
2.2. Case definition
Persons were considered cases if they became ill or injured after exposure to paraquat only, diquat only, or pesticide mixtures that included paraquat and/or diquat. The SENSOR-Pesticides case definition, described in detail elsewhere (CDC, 2012), requires information about pesticide exposure and health effects, and this information is compared to the known toxicology of the pesticide exposure. The PISP case definition is similar to SENSOR-Pesticides (California Department of Pesticide Regulation, 2015). Cases in SENSOR-Pesticides and PISP determined to be related to paraquat or diquat exposure are categorized as definite, probable, and possible. Definite cases are based exclusively on objective data about exposure and health effects, probable cases are based on a mix of objective and subjective data, and possible cases are based on subjective exposure and health effects data. IDS and PISP cases were reviewed for consistency with the SENSOR-Pesticides case definition. Cases not consistent with the case definition were excluded. NPDS cases assigned the following medical outcomes by the PCC specialist managing the specific case were included in the analysis: death; major effect; moderate effect; minor effect; not followed, minimal clinical effects possible; and, unable to follow, judged as potentially toxic exposure.
Illness severity was categorized into four groups using standardized criteria (CDC, 2005). In low severity cases, the illness usually resolves without treatment and there are fewer than 3 days lost from work. In moderate severity cases, the illness is non-life threatening, but requires medical treatment. No residual impairment is expected, and time lost from work is five days or fewer. In high severity cases, illness is life threatening, requires hospitalization, often has greater than 5 days lost from work, and may result in permanent impairment. Finally, fatal cases of pesticide poisoning were placed in a separate category. Severity of NPDS cases was determined by the PCC specialist. Cases classified as “minor effect” or “no follow-up, minimal toxicity” were defined as low severity; those classified as “moderate effect” or “no follow-up, potentially toxic” were defined as moderate severity; those classified as “major effect” were defined as high severity; and, those classified as “death” were defined as fatal.
Root causes of the illness-causing paraquat/diquat exposure were identified from several sources. Some root causes were systematically gathered by SENSOR-Pesticides state partners (e.g. drift and lack of required PPE use). All cases captured by PISP are investigated by the relevant county agriculture commissioner. The commissioner’s investigation reports were reviewed by PISP staff to identify root causes (i.e. drift, early re-entry, failure to use required PPE, and equipment failure). Root causes (e.g. label requirements, transport for care, improper storage, etc.) were also identified using narrative descriptions, and documentation of violations.
2.3. Data analysis
Data analyses were performed using SAS software (9.3; SAS Institute Inc., Cary, NC). Descriptive statistics were calculated for both work- and non-work-related cases. One case was exposed to both paraquat and diquat in the SENSOR-Pesticides database, and there were nine such cases in NPDS; these cases were counted only once and included with paraquat mixtures.
3. Results
3.1. Findings from NPDS
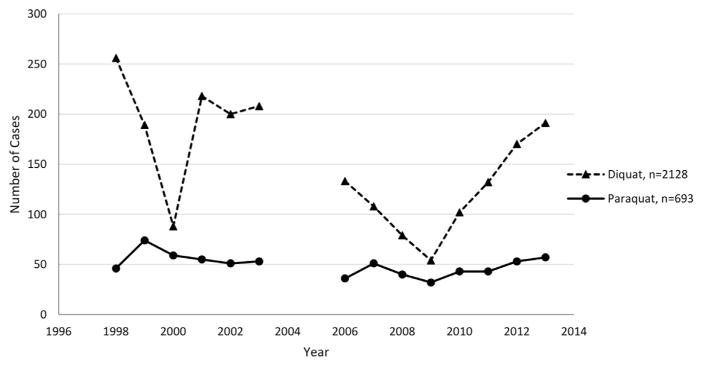
NPDS identified 693 and 2128 cases related to paraquat and diquat exposures, respectively (Table 1). The majority of acute paraquat-related illnesses occurred in the Southeastern region (53%). Males accounted for a majority of acute paraquat- (85%; n=588) and diquat-related (56%; n=1188) illnesses, and paraquat-related illnesses were more likely to arise from work-related exposures compared to diquat-related illnesses. The annual number of paraquat-related illnesses was range-bound between the years 1998 and 2013 (49–75 cases per year), showing no clear trend, whereas the trend for diquat is trimodal, with dips in 2000 and 2009 and increasing counts since 2009 (Fig. 1).
Table 1.
Descriptive characteristics of acute paraquat- and diquat-related illness cases.
| SENSOR, PISP and IDS (1998–2011)
|
NPDSa (1998 –2003 –2006–2013)
|
|||
|---|---|---|---|---|
| Paraquat | Diquat | Paraquat | Diquat | |
|
| ||||
| Variable | Count (%) | Count (%) | Count (%) | Count (%) |
| Total | 300 | 144 | 693 | 2128 |
| Regiona | ||||
| West | 139 (46) | 59 (41) | 200 (29) | 497 (23) |
| Southwest | 106 (35) | 66 (46) | 365 (53) | 833 (39) |
| Midwest | 11 (4) | 16 (11) | 84 (12) | 497 (23) |
| Northwest | 6 (2) | 3 (2) | 44 (6) | 301 (14) |
| Sex | ||||
| Male | 179 (60) | 91 (63) | 588 (85) | 1188 (56) |
| Female | 30 (10) | 53 (37) | 104 (15) | 932 (44) |
| Unknown | 91 (30) | 0 | 1 (<1) | 8 (<1) |
| Work-related cases | ||||
| Yes | 203 (68) | 42 (29) | 315 (45) | 167 (8) |
| No | 63 (21) | 81 (56) | 371 (54) | 1959 (92) |
| Unknown | 34 (11) | 21 (15) | 7 (1) | 2 (<1) |
| Suicide/near-suicide | ||||
| Yes | 15 (5) | 13 (9) | 12 (2) | 17 (1) |
| No | 271 (90) | 128 (89) | 673 (97) | 2107 (99) |
| Unknown | 3 (1) | 1 (<1) | 8 (1) | 4 (<1) |
| Illness severity | ||||
| Fatal | 24 (8) | 5 (3) | 13 (2) | 3 (<1) |
| High | 19 (6) | 7 (5) | 24 (3) | 14 (1) |
| Moderate | 133 (44) | 15 (10) | 237 (34) | 264 (12) |
| Low | 124 (41) | 117 (81) | 419 (60) | 1847 (87) |
| Age (years) | ||||
| 0–12 | 4 (2) | 14 (10) | 16 (3) | 240 (11) |
| 13–19 | 9 (3) | 12 (8) | 36 (5) | 66 (3) |
| 20–39 | 86 (29) | 39 (27) | 274 (40) | 538 (25) |
| 40–59 | 61 (20) | 39 (27) | 218 (32) | 653 (31) |
| 60 and over | 15 (5) | 19 (13) | 76 (11) | 415 (20) |
| Unknown | 125 (42) | 21 (15) | 73 (11) | 216 (10) |
| Case definition status | ||||
| Definite | 52 (17) | 23 (16) | ||
| Probable | 55 (18) | 34 (24) | ||
| Possible | 71 (24) | 87 (60) | ||
| Exposed to a mixtureb | ||||
| Yes | 50 (17) | 110 (76) | ||
| No | 250 (83) | 34 (24) | ||
| Data system | ||||
| SENSOR-excluding California | 114 (38) | 109 (76) | ||
| California (PISP+SENSOR-CA)c | 62 (21) | 35 (24) | ||
| IDSc | 124 (41) | 0 | ||
| NPDSc | 693 | 2128 | ||
West-Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington; Southeast-Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, Oklahoma, Puerto Rico, South Carolina, Tennessee, Texas, Virginia; Midwest-Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, West Virginia, Wisconsin; Northeast-Connecticut, Delaware, Maine, Maryland, Massa-chusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont.
Those not exposed to a mixture were only exposed to paraquat or diquat, whereas those exposed to a mixture were exposed to another pesticide in addition to paraquat or diquat.
NDPS=National Poison Data System; PISP=Pesticide Incident Surveillance Program; CA=California; IDS=US Environmental Protection Agency Incident Data System.
Fig. 1.
Acute paraquat- and diquat-related illness counts captured in the National Poison Data System (NPDS), 1998–2003 and 2006–2013.
3.2. Findings from SENSOR/PISP/IDS
A total of 300 paraquat- and 144 diquat-related acute illnesses were reported in 35 states and 1 US territory; 255 cases were identified by SENSOR, 93 cases by PISP (65 were uniquely PISP-identified), and 128 cases by IDS (124 were uniquely IDS-identified) (Table 1). States in the western US accounted for the highest proportion of paraquat and diquat illness cases. Work-related paraquat and diquat exposures accounted for 68% (n=203) and 29% (n=42) of all paraquat and diquat cases, respectively. Among cases with paraquat-related illnesses, 83% (n=250) were exposed to paraquat only (the other 17% were also exposed to other pesticides) (Table 1). In contrast, the majority of individuals exposed to diquat were also exposed to at least one other pesticide (76%, n=110), and the other pesticide most commonly was glyphosate (n=53), fluazifop (n=28) and/or dicamba (n=24). Most cases were male (paraquat=60%, diquat=63%). Two percent (n=4) and 10% (n=14) of paraquat and diquat cases, respectively, were under the age of 15 years, all of whom had non-occupational exposures.
Of the ingestion cases involving paraquat (n=43) and diquat (n=25), most were due to unintentional ingestion (58% and 50%, respectively) (Table 1). Unintentional paraquat ingestion was commonly due to improper storage of the pesticide in beverage containers (48%; n=12). Other less common unintentional ingestion cases included unintentionally ingesting while applying paraquat or diquat at work (n=6; paraquat=5, diquat=1), swallowing paraquat while attempting to siphon it (n=3), and not washing hands after diquat application and then using chewing tobacco (n=1). In this study, intentional (i.e. suicidal) ingestion occurred in 5% (n=15) and 8% (n=12) of all paraquat and diquat-related illness cases, respectively. Ingestion (seven from unintentional ingestion and two from intentional ingestion) was responsible for 47% (n=9) of the 19 high severity, acute paraquat-related illnesses; and ingestion was responsible for 79% (n=19, seven from unintentional ingestion and 12 from intentional ingestion) of the 24 paraquat-related deaths.
Although most cases of acute paraquat-related illness were of low (41%) or moderate (44%) severity, death occurred in a total of 8% (n=24) illnesses, and all but one of these deaths were non-work-related. A total of 50% of the deaths (n=12), involved unintentional paraquat exposure: seven of these deaths involved unintentional paraquat ingestion from improper storage, including a 15-month old and 8-year old; two deaths involved exposure to paraquat from off-target drift; and, in three unintentional deaths, the exact mechanism of exposure could not be determined. Among the five acute diquat-related deaths identified by SENSOR/PISP/IDS, one occurred due to unintentional ingestion (non-occupational), and the other four involved intentional ingestions.
Although paraquat accounts for only 6% of all acute herbicide-related illnesses in the SENSOR-Pesticides database (n=2313), it accounts for 15% of high severity cases of acute herbicide-related illnesses (this comparison is not possible for PISP and IDS because severity was not determined for cases poisoned by non-dipyridyl pesticides). Diquat accounts for 5% of all acute herbicide-related illnesses in the SENSOR-Pesticides database but 9% of high severity of acute herbicide-related illnesses. Furthermore, the vast majority (85%) of all herbicide-related deaths in the SENSOR-Pesticides and PISP databases were caused by either paraquat or diquat. Of the four herbicide-related deaths captured by SENSOR-Pesticides, paraquat and diquat were involved in 75% and 25%, respectively; in PISP, of the nine herbicide-related deaths, three were caused by paraquat, four involved diquat, one involved glyphosate, and one MSMA.
For cases with known application location, the vast majority of paraquat-related illnesses were related to agricultural applications while non-agricultural applications accounted for the vast majority of diquat-related illnesses (Table 2). The majority of paraquat and diquat illness cases occurred in pesticide handlers (53% and 54%, respectively).
Table 2.
Acute paraquat- and diquat-related illness cases by exposure and occupational characteristics: SENSOR, PISP, and IDS data, 1998–2011.
| Paraquat
|
Diquat
|
|||||
|---|---|---|---|---|---|---|
| All cases | Non-work-related cases | Work-related cases | All cases | Non-work-related cases | Work-related cases | |
|
| ||||||
| Variable | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| Total | 300 | 63(21) | 203(68) | 144 | 81(56) | 42(29) |
| Application site | ||||||
| Agriculturala | 153(51) | 13(21) | 140(69) | 12(8) | 1(1) | 11(26) |
| Non-agricultural | 35(12) | 24(38) | 10(5) | 127(88) | 72(89) | 27(64) |
| Unknown | 112(37) | 26(41) | 53(26) | 5(3) | 8(10) | 4(10) |
| Activity during exposure | ||||||
| Handlersb | 159(53) | 4(6) | 152(75) | 78(54) | 32(40) | 34(81) |
| Routine indoor/outdoor living activities not involved with pesticide application | 34(11) | 21(33) | 0 | 33(23) | 29(36) | 0 |
| Routine work activities not involved with pesticide application | 31(10) | 1(2) | 30(15) | 6(4) | 0 | 5(12) |
| Other | 6(2) | 5(8) | 0 | 10(7) | 9(11) | 1(2) |
| Unknown | 70(23) | 31(49) | 21(10) | 17(12) | 11(14) | 2(5) |
| Routes of exposurec | ||||||
| Dermal | 128(43) | 12(19) | 102(50) | 63(44) | 32(40) | 23(55) |
| Ocular | 70(23) | 4(6) | 61(30) | 37(26) | 17(21) | 11(26) |
| Inhalation | 74(25) | 18(29) | 51(25) | 35(24) | 24(30) | 6(14) |
| Ingestion | 43(14) | 28(44) | 9(4) | 25(17) | 22(27) | 3(7) |
| Unintentional ingestiond | 25(58) | 14(50) | 9(100) | 13(50) | 10(45) | 3(100) |
| Intentional ingestion(i.e. suicide or attempted suicide)d | 15(35) | 13(46) | 0 | 12(46) | 12(55) | 0 |
| Ingestion of unknown intentd | 3(7) | 1(4) | 0 | 1(41) | 0 | 1(2) |
| Unknown | 12(4) | 6(10) | 6(3) | 3(2) | 1(1) | 1(2) |
| Type of exposurec, e | ||||||
| Directly sprayed with herbicide | 60(34) | 3(8) | 55(41) | 46(32) | 23(28) | 9(21) |
| Leak/spill | 37(21) | 2(6) | 35(26) | 29(20) | 8(10) | 18(43) |
| Drift | 25(14) | 16(44) | 9(7) | 15(10) | 11(14) | 2(5) |
| Contact with treated surface | 9(5) | 1(3) | 8(6) | 7(5) | 4(5) | 1(2) |
| Other | 15(9) | 9(25) | 6(4) | 20(14) | 15(19) | 5(12) |
| Unknown | 30(17) | 6(17) | 22(16) | 28(19) | 20(25) | 7(17) |
| Toxicityf, e | ||||||
| I-Danger | 114(65) | 18(50) | 91(67) | 0 | 0 | 0 |
| II-Warning | 0 | 0 | 0 | 32(22) | 14(17) | 16(38) |
| III-Caution | 0 | 0 | 0 | 75(52) | 51(63) | 9(21) |
| Unknown | 62(35) | 18(50) | 42(31) | 37(26) | 16(20) | 17(40) |
| Application targete | ||||||
| Undesired plants | 53(30) | 5(14) | 48(36) | 24(17) | 14(17) | 8(19) |
| Fruit crops | 22(13) | 1(3) | 21(16) | 3(2) | 1(1) | 2(5) |
| Grain/fiber/grass crops | 16(9) | 9(25) | 7(5) | 8(6) | 7(9) | 1(2) |
| Other (e.g., miscellaneous crops, soil) | 15(9) | 6(17) | 9(7) | 5(3) | 2(2) | 1(2) |
| Landscape/forest | 3(2) | 2(6) | 1(1) | 24(17) | 16(20) | 8(19) |
| Aquatic (excluding pools) | 0 | 0 | 0 | 14(10) | 9(11) | 5(12) |
| Unknown | 67(38) | 9(25) | 49(36) | 66(46) | 32(40) | 17(40) |
| Application equipmente | ||||||
| Low-pressure ground sprayer | 46(26) | 2(6) | 44(33) | 2(1) | 1(1) | 1(2) |
| Spray Line, handheld | 17(10) | 4(11) | 13(10) | 21(15) | 16(20) | 2(5) |
| Sprayer, backpack | 17(10) | 1(3) | 16(12) | 14(10) | 5(6) | 9(21) |
| Aerial applicator | 12(7) | 10(28) | 2(1) | 1(1) | 1(1) | 0 |
| Other | 12(7) | 2(6) | 10(7) | 7(5) | 4(5) | 1(2) |
| Trigger Pump | 3(2) | 1(3) | 2(1) | 19(13) | 15(19) | 4(10) |
| Manual placement | 6(3) | 3(8) | 3(2) | 1(1) | 0 | 0 |
| Pressurized can | 0 | 0 | 0 | 4(3) | 4(5) | 0 |
| Unknown | 63(36) | 13(36) | 45(33) | 74(51) | 32(40) | 25(60) |
‘Agricultural’ includes: farm, nursery, forest, livestock and animal specialty production, greenhouse, and other non-production agricultural processing.
‘Handlers’ includes: pesticide applicators, mixers/loaders, transporters/disposers, repair/maintenance of pesticide application equipment.
Sum of some variables will exceed 100% because in some instances cases had more than one type of exposure.
Denominator is total cases of ingestion for corresponding category.
IDS data (N=124; Non-work: n=27; Work: n=68) excluded from analysis due to substantial missing information.
USEPA toxicity categories ranging from toxicity I (the most toxic) to IV (the least toxic) are assigned to each product (USEPA, 2014).
Health effects among the paraquat-related illness cases predominantly included dermal symptoms (42%), such as skin pain, and rash (Table 3). Ocular (34%), neurological (27%), and respiratory (24%) symptoms were also observed. For diquat cases, the most commonly observed health effects involved the skin (42%), eye (31%), neurological (30%) (e.g. headache), and respiratory systems (28%) (e.g. upper respiratory irritation).
Table 3.
Signs and symptoms of acute paraquat- and diquat-related illness: SENSOR, PISP, and IDS data, 1998–2011.
| Body part/system affecteda | Paraquat, n (%) | Diquat, n (%) |
|---|---|---|
| Total | 300 | 144 |
| Dermal | 125(42) | 61(42) |
| Skin pain | 55(18) | 33(23) |
| Erythema | 51(17) | 35(24) |
| Rash | 36(12) | 14(10) |
| Edema | 28(9) | 10(7) |
| Skin burn | 27(9) | 10(7) |
| Pruritis | 24(8) | 14(10) |
| Bullae | 23(7) | 8(6) |
| Contact dermatitis | 7(2) | 4(3) |
| Hives | 2(1) | 3(2) |
| Otherb | 7(2) | 4(3) |
| Eye | 103(34) | 45(31) |
| Eye pain/irritation/inflammation | 95(32) | 38(26) |
| Lacrimation | 30(10) | 13(9) |
| Conjunctivitis | 25(8) | 16(11) |
| Corneal abrasion | 19(6) | 6(4) |
| Eye burns | 18(6) | 5(3) |
| Otherb | 13(4) | 3(2) |
| Neurologic | 82(27) | 43(30) |
| Headache | 41(14) | 14(10) |
| Dizziness | 22(7) | 10(7) |
| Blurred vision | 17(6) | 1(1) |
| Paresthesias | 9(3) | 3(2) |
| Muscle weakness | 10(3) | 5(3) |
| Muscle pain | 5(2) | 2(1) |
| Hyperactivity/anxiety/irritability | 4(1) | 5(3) |
| Confusion | 3(1) | 4(3) |
| Otherb | 24(8) | 15(10) |
| Respiratory | 73(24) | 40(28) |
| Dyspnea | 34(11) | 14(10) |
| Upper respiratory pain | 27(9) | 20(14) |
| Cough | 17(6) | 10(7) |
| Respiratory depression | 5(2) | 2(1) |
| Wheezing | 5(2) | 2(1) |
| Pleuritic chest pain | 4(1) | 2(1) |
| Lower respiratory irritation | 4(1) | 6(4) |
| Otherb | 33(11) | 13(9) |
| Gastrointestinal | 68(23) | 31(22) |
| Nausea | 36(12) | 18(13) |
| Vomiting | 35(12) | 20(14) |
| Abdominal pain/cramping | 12(4) | 8(6) |
| Diarrhea | 9(3) | 6(4) |
| Otherb | 8(3) | 4(3) |
| Cardiovascular | 40(13) | 19(13) |
| Hypertension | 12(4) | 2(1) |
| Tachycardia | 10(3) | 7(5) |
| Chest Pain | 16(5) | 6(4) |
| Bradycardia | 0 | 4(3) |
| Other | 10(3) | 8(6) |
| Miscellaneous | 49(16) | 26(18) |
| Renalc | 22(7) | 8(6) |
| Fatigue/malaise | 12(4) | 10(7) |
| Acidosis | 5(2) | 4(3) |
| Hyperthermia/fever | 4(1) | 4(3) |
Each person may have more than one body part/system affected and may have multiple signs or symptoms per body part/system.
Other includes: For paraquat: Dermal-flaky skin/nail (n=4), skin peeling (n=3); Eye-blurred vision (n=8), eye blisters (n=2), mucous (n=3 Neurological-peripheral neuropathy (n=1), fasciculations (n=1), muscle rigidity (n=1), slurred speech (n=2), diaphoresis (n=1), fainting (n=1), salivation (n=4), altered taste (n=4), ataxia (n=2), loss of consciousness (n=2), tremors/twitching (n=2), giddiness (n=1), sleeplessness (n=1); Respiratory-hyperventilation/tachypnea (n=3), cyanosis (n=1), pulmonary edema (n=1), sore throat (n=1), burning nasal passages (n=3), respiratory failure/dysfunction (n=7), nosebleed (n=3), respiratory distress (n=2), pulmonary fibrosis (n=4), respiratory irritation (n=3), broncho-constriction (n=1); Gastrointestinal-loss of appetite (n=2), bloody stool/vomit (n=2), epigastric pain (n=2), gastrointestinal bleeding/dysfunction (n=2);Cardiovascular-hypotension (n=2), cardiac arrest (n=3), cardiac conduction disturbance (n=1). For Diquat: Dermal-white oral patches (n=2); Eye-blurred vision (n=3); Neurological-peripheral neuropathy (n=1), diaphoresis (n=4), fainting (n=1), salivation (n=1), altered taste (n=5), ataxia (n=1), drowsiness (n=2); Respiratory-hyperventilation/tachypnea (n=1), asthma (n=1), sore throat (n=3), nasal irritation (n=3), mucous (n=2); Gastrointestinal-hyperactive bowel sounds (n=2); Cardiovascular-hypotension (n=4), palpitations (n=1), cardiac arrest (n=1), chest tightness (n=2).
Includes: for Paraquat: reduced/absent urination (n=2), blood in urine (n=1), blue urine (n=1), proteinuria (n=2), elevated creatinine (n=1), renal failure (n=15). For diquat: elevated creatinine (n=1), reduced/absent urination (n=1), frequent urination (n=1), Renal failure (n=5).
For paraquat-related illnesses, the most common root cause was failure to wear adequate personal protective equipment (33%), especially eye protection (19%) (Table 4). Other common root causes were off-target pesticide drift from the application site (14%), inadvertent spill/splash (not involving application equipment failure) (14%), and application equipment failure (e.g., hose leaks and improper equipment assembly) (12%). Many paraquat-related illnesses involving off-target drift were due to aerial applications that drifted from the application site to individuals who were engaged in their routine living activities (e.g. sitting or working in their yard)(41%). Common root causes for acute diquat-related illnesses were application equipment failure (17%), and inadvertent spill/splash of liquid (16%). Of the 23 acute diquat-related illnesses caused by spill/splash, 20 occurred at the time of spill/splash, 2 occurred during clean-up, and one case lacked detail to determine if the exposure occurred during or after the spill/splash.
Table 4.
Root causes for acute paraquat- and diquat-related illness: SENSOR, PISP, and IDS data, 1998–2011.
| Paraquat | Diquat | |
|---|---|---|
|
| ||
| (n=300) | (n=144) | |
|
| ||
| Root causea | n (%) | n (%) |
| One or more root causes identified | 258(86) | 129(90) |
| Required PPE not worn:b | 100(33) | 10(7) |
| Required eye protection not worn or inadequate | 56(19) | 6(4) |
| Required respirator not worn or inadequate | 28(9) | 1(1) |
| Required gloves not worn or inadequate | 27(9) | 3(2) |
| Other required PPE not worn or inadequate | 23(8) | 2(1) |
| Drift from application site | 43(14) | 12(8) |
| Spill/splash of liquid or dust | 42(14) | 23(16) |
| Application equipment failure | 36(12) | 25(17) |
| Label violations not otherwise specified | 20(7) | 10(7) |
| Decontamination not adequate or timely | 19(6) | 3(2) |
| Intentional harm | 15(5) | 13(9) |
| Improper storage | 12(4) | 13(9) |
| Applicator not properly trained or supervised | 8(3) | 0 |
| No label violation identified but person still ill | 7(2) | 8(6) |
| People were in the treated area during application | 3(1) | 2(1) |
| Notification/posting lacking or ineffective | 1(<1) | 3(2) |
| Early re-entry into treated area | 1(<1) | 2(1) |
| Excessive application of pesticide | 0 | 1(1) |
| Mixture of incompatible products | 0 | 2(1) |
| Unknown | 42(14) | 15(10) |
PPE=personal protective equipment.
Cases can have more than one root cause.
Row represents individual cases that did not wear one or more of the required PPE.
3.3. Case reports
The following five cases presented in chronological order, illustrate different patterns of exposure to paraquat and diquat products.
Case 1
In April 2003, a 41-year-old man working on a water-melon farm in California developed nausea, vomiting, difficulty breathing, and sleeplessness after inhaling a whiff of paraquat (Gramoxone Max Herbicide, EPA Registration Number (Reg#) 100-1074, active ingredient (AI): 43.8% paraquat) while he hand-poured it into a 300-gallon mix tank. He failed to use the required closed system. He continued working for several hours before informing his supervisor. It is unknown whether he lost time from work or leisure activities, but he was not hospitalized. His illness was classified as “probable” and of low severity.
Case 2
In July 2008, an 8-year-old child in North Carolina drank an unknown amount of paraquat (Gramoxone Inteon, Reg# 100-1217, AI: 30.1% paraquat), from a soda bottle stored in the garage. The child developed ataxia, confusion, respiratory depression, lethargy, vomiting, acidosis, mediastinitis, pneumothorax, and kidney failure. The child died after an 8 day hospitalization. His illness was classified as a “definite” case.
Case 3
In November 2008, a 38-year-old severely autistic man in California, with a history of pica, drank an unknown amount of diquat (Roundup Weed & Grass Killer Concentrate Plus, Reg# 71995-29, AI: 0.73% Diquat and 18% glyphosate) that his caretaker said he might have mistaken for juice. He sought care at the emergency department and developed hypoxia and hypothermia. He died the next day. This case was classified as “definite”.
Case 4
In July 2011, a 17-year-old male in the Southeastern region of the US accidentally sprayed diquat (Reg# 9688-208, AI: 0.18% Diquat dibromide, 0.06% fluazifop, and 0.04% dicamba) on his face, eyes and chest, and unintentionally ingested some of the product. An hour later, he developed eye pain, irritation, and inflammation. He also developed abdominal pain/cramping, conjunctivitis, tachycardia, and confusion. He received treatment at the Emergency Department. It is unknown whether he lost time from his regular activities. His illness was classified as a “probable” case with moderate severity.
Case 5
In September 2011, a 57-year-old female school principal in Washington drenched her hand with diquat (Reg# 9688-208, AI: 0.18% Diquat dibromide, 0.06% fluazifop-p-butyl, and 0.04% dicamba) after the spray nozzle broke while spraying for weed control on school property. She developed skin redness, upper respiratory pain, headache, dizziness, paresthesia, and a metallic taste in her mouth 20 min after exposure. She sought advice from the local PCC. She did not lose any time from work or her regular leisure activities. Her illness was classified as “probable” and low severity.
4. Discussion
Using surveillance data from 1998 to 2011 compiled by SENSOR/PISP/IDS, 300 paraquat- and 144 diquat-related illnesses were identified. For the years 1998–2003 and 2006–2013, NPDS identified 693 and 2128 illnesses related to paraquat and diquat, respectively. These numbers suggest that the magnitude of acute paraquat and diquat-related illnesses is relatively low. Although paraquat is highly toxic, most cases of acute paraquat-related illness were of low (41%) or moderate (44%) severity. However, the proportions of acute paraquat-related illness identified by SENSOR/PISP/IDS involving high severity illness and death were relatively high (14%), compared to illnesses identified in SENSOR-Pesticides involving all other non-dipyridal pesticides (2%). The vast majority (85%) of all herbicide-related deaths in the SENSOR-Pesticides and PISP databases involved either paraquat or diquat. Among cases with available information, most acute paraquat-related illnesses arose from agricultural applications (81%) and were work-related (77%), while diquat cases were primarily non-work-related (66%), and non-agricultural (91%). As expected, there were fewer non-work-related paraquat-related illnesses compared to diquat because paraquat is a restricted-use pesticide that is unavailable to consumers.
Many of the illnesses caused by paraquat occurred because the paraquat label instructions, which are legally enforceable, were not strictly followed. For example, the most common root cause of paraquat-related illness was failure to comply with PPE requirements (n=100, 33%). Paraquat handlers are required to wear extensive PPE, including: air-purifying respirator with cartridges; chemical resistant gloves; protective eyewear; and, long clothing (USEPA, 1997). The most common PPE root cause for paraquat-related illness was lack of eye protection (19%). A 1995 unpublished study performed by a paraquat registrant found that among 17 paraquat handlers who were told to comply with label requirements but whose practices were otherwise not interfered with, only three (18%) wore the required eye protection (USEPA, 1997). Factors influencing a worker’s decision to wear protective eyewear include knowledge that eye protection is required, eye-wear design (e.g. comfort, fit, fogging-resistant), availability (e.g. employer-provided at no cost), and eyewear stylishness (Lombardi et al. 2009). Eye protection compliance may be increased by enhancing awareness of eyewear requirements and potential consequences of non-usage, ensuring proper fit, offering attractive styles, and making them readily available. Similar measures could be employed to enhance use of the other PPE required when using paraquat.
Unintentional paraquat ingestion was commonly due to another label violation, i.e., improper storage of paraquat. Paraquat labels forbid decanting paraquat into alternate containers (e.g. beverage containers), prohibit storing paraquat in the home, and outlaw the giving/selling of paraquat to non-certified applicators. Greater efforts to train certified applicators and to enforce these prohibitions are needed.
Ingestion was responsible for a substantial proportion of high severity and fatal paraquat-related illnesses. In addition to para-quat being a restricted use pesticide and the need for compliance with label requirements, mitigation strategies to address ingestion risks have primarily involved product reformulation, such as adding alerting agents (e.g. pigments, stenching agents, and emetic agents), gelling agents (i.e. alginates to reduce stomach absorption), and/or reformulating to lower concentrations. Since 1988, a blue pigment, stenching compound, and emetic were added to paraquat products (USEPA, 1997). However, there is little evidence supporting the effectiveness of these alerting agents in reducing paraquat-related mortality (Onyon and Volans, 1987). Gastric acid-triggered “gelling” agents, introduced in 2005, are designed to reduce paraquat absorption following ingestion (Heylings et al., 2007), and have been found to reduce mortality (Wilks et al., 2008). In contrast to the US where only formulations with paraquat concentrations between 30% and 43% are sold, in 1986 paraquat was reformulated in Japan from a 24% solution down to a 5% solution that included the addition of a 5–7% diquat solution. Patients ingesting the 5% paraquat solution had non-significantly higher survival rates compared to those who ingested a 24% solution (Nagami et al., 2007). Most deaths were from suicide, but at least one death involved accidental ingestion of 40 ml of the 5% paraquat solution.
A complete ban on paraquat sales appears to be an effective strategy to prevent paraquat-related illness, and this approach was adopted by the European Union and at least seven other countries. The bans led to reductions in paraquat-related illnesses in the United Kingdom (Perry et al., 2014) and France (Kervegant et al., 2013).
Most cases of acute diquat-related illness were low severity (81%), principally affecting the skin and eyes. Products containing diquat are available in concentrations ranging from 0.2% to 41%. Products with concentrations below 1% require the handler to wear long-sleeved shirts and pants, shoes, and socks only. Even products with concentrations above 1% do not always require use of chemical-resistant gloves and eye protection. Equipment failure and inadvertent spills and splashes were the most common contributing factors for diquat exposure (17% and 16%, respectively). Labels for all diquat products could be revised to require use of chemical-resistant gloves and protective eyewear during use and when cleaning spills; however, these PPE would not protect the five individuals exposed by mouth or nose. Some diquat-containing products require use of an air-purifying respirator, thereby protecting mouth and nose.
The findings in this report are subject to several limitations. First, because rates are not provided, caution is needed when comparing case counts from different geographic regions. NPDS data are more national in scope and are more likely to reflect the true geographic distribution of cases, compared to SENSOR/PISP/IDS. Second, acute illnesses due to paraquat and diquat exposures are likely under-reported, and our data represent minimum estimates of their true magnitude. For example, cases who did not seek medical care or advice from a PCC would not be identified. Additionally, low severity cases of acute paraquat-related illness identified by the IDS data system were not included because no details were available on these cases. This likely contributed to an over-representation of paraquat-related illnesses with moderate severity or higher in SENSOR/PISP/IDS, compared to NPDS. Also, intentional exposures are under-reported because some SENSOR-Pesticides states do not capture intentional exposures and they were not available in the 2006–2013 NPDS data. Third, information was incomplete for some reported cases because investigations did not always occur or insufficient details were obtained. For example, IDS cases typically did not have information on many characteristics (e.g. application target, equipment, and work-relatedness). Fourth, some individuals may have been incorrectly diagnosed with acute paraquat- or diquat-related illness. This is because symptoms for these acute illnesses are often nonspecific and laboratory diagnostic tests are rarely performed due to their lack of availability. Additionally, most of the cases included in our analyses were classified as “possible” (83%) meaning they were based on subjective data, without objective verification of health effects and exposure. Furthermore, 16% of paraquat cases and 76% of diquat cases were exposed to pesticide mixtures, and these cases may have had their symptoms erroneously attributed to paraquat or diquat. Finally, root causes for most SENSOR-Pesticides cases were coded retrospectively, so misclassification was possible.
5. Conclusion
In conclusion, to our knowledge this is the first summary of the magnitude and characteristics of acute paraquat- and diquat-related illness in the US, using four different systems. Although the magnitude of acute paraquat- and diquat-related illness was relatively low, and most cases were of low severity, SENSOR/PISP/IDS identified 29 deaths (24 from paraquat and 5 from diquat), and 26 high severity illnesses (19 from paraquat and 7 from diquat) during a 14-year time period (1998–2011). The proportions of acute paraquat- and diquat-related illness involving high severity illness and death were relatively high (14% and 8%, respectively). Furthermore, data from NPDS found that the counts of diquat-related illnesses exceeded those of paraquat-related illnesses. All of these cases were preventable, many through stricter compliance with label instructions. For example, unintentional paraquat ingestion, often due to improper storage of the pesticide in beverage containers, was responsible for at least seven deaths. As paraquat labels forbid decanting paraquat into alternate containers, greater efforts are needed to train certified applicators and to enforce these prohibitions. Requiring additional PPE such as chemical-resistant gloves and protective eyewear when using diquat and using a closed system when mixing and loading paraquat should also be considered. Users of paraquat may also limit their exposure by considering less harmful weed control alternatives (e.g. glufosinate).
Acknowledgments
Funding sources
Funding was provided by the National Institute for Occupational Safety and Health, United States, the United States Environmental Protection Agency (EPA Interagency Agreement identification number DW-75-95840001-2), and the participating state agencies that provided data.
Footnotes
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health, the United States Environmental Protection Agency, or each author’s state agency.
Disclosure
The authors declare they have no actual or potential competing financial interests.
Human subjects review
Because all personal identifiers were removed from the data prior to NIOSH submission, this study was exempt from consideration by the federal Institutional Review Board.
References
- Bronstein AC, Spyker DA, Cantilena LR, Rumack BH, Dart RC. 2011 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th annual report. Clin Toxicol. 2012;50:911–1164. doi: 10.3109/15563650.2012.746424. [DOI] [PubMed] [Google Scholar]
- California Department of Pesticide Regulation. [accessed 25.09.15];Pesticide Illness Surveillance Program (PISP) Database User Documentation/Dictionary. 2015 Available: < http://www.cdpr.ca.gov/docs/whs/pisp/data_dictionary.pdf>.
- Calvert GM, Mehler LN, Alsop J, De Vries AL, Besbelli N. Surveillance of pesticide-related illness and injury in humans. In: Krieger RI, editor. Hayes’ Handbook of Pesticide Toxicology. 3. Elsevier; New York: 2010. pp. 1313–1369. [Google Scholar]
- Calvert GM, Karnik J, Mehler L, Beckman J, Morrissey B, Sievert J, et al. Acute pesticide poisoning among agricultural workers in the United States, 1998–2005. Am J Ind Med. 2008;51(12):883–898. doi: 10.1002/ajim.20623. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Pesticide-Related Illness and Injury Surveillance: A how-to Guide for State Based Programs. US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; Cincinnati, OH: 2005. [accessed 25.09.15]. http://www.cdc.gov/niosh/docs/2006-102/ [Google Scholar]
- Centers for Disease Control and Prevention. Case Definition for Acute Pesticide-Related Illness and Injury Cases Reportable to the National Public Health Surveillance System. US Department of Health and Human Services, CDC, National Institute for Occupational Safety and Health; Cincinnati, OH: 2012. [accessed 25.09.15]. http://www.cdc.gov/niosh/topics/pesticides/pdfs/casedef.pdf. [Google Scholar]
- Heylings JR, Farnworth MJ, Swain CM, Clapp MJ, Elliot BM. Identification of an alginate-based formulation of paraquat to reduce the exposure of the herbicide following oral ingestion. Toxicology. 2007;241:1–10. doi: 10.1016/j.tox.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Jones GM, Vale JA. Mechanisms of toxicity, clinical features, and management of diquat poisoning: a review. Clin Toxicol. 2000;38(2):123–128. doi: 10.1081/clt-100100926. [DOI] [PubMed] [Google Scholar]
- Kervegant M, Merigot L, Glaizal M, Schmitt C, Tichadou L, de Haro L. Paraquat poisonings in France during the European ban: experience of the poison control center in Marseille. J Med Toxicol. 2013;9:144–147. doi: 10.1007/s13181-012-0283-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi DA, Verma SK, Brennan MJ, Perry MJ. Factors influencing worker use of personal protective eyewear. Accid Anal Prev. 2009;41:755–762. doi: 10.1016/j.aap.2009.03.017. [DOI] [PubMed] [Google Scholar]
- Mowry JB, Spyker LR, Cantilena LR, Mcmillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol. 2014;52:1032–1283. doi: 10.3109/15563650.2014.987397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagami H, Nishigaki Y, Matsushima S, Yajima N. Paraquat poisoning in Japan: a hospital-based survey. J Rural Med. 2007;2:85–92. [Google Scholar]
- Onyon LJ, Volans GN. The epidemiology and prevention of paraquat poisoning. Hum Toxicol. 1987;6:19–29. doi: 10.1177/096032718700600104. [DOI] [PubMed] [Google Scholar]
- Paraquat Information Center. [accessed 25.09.15];Use. 2014 Available: < http://paraquat.com/use>.
- Perry L, Adams RD, Bennett AR, Lupton DJ, Jackson G, Good AM, Thomas SHL, Vale JA, Thompson JP, Bateman DN, Eddleston M. National toxicovilgilance for pesticide exposures resulting in health care contact – an example from the UK’s National Poisons Information Service. Clin Toxicol. 2014;52:549–555. doi: 10.3109/15563650.2014.908203. http://dx.doi.org/10.3109/15563650.2014.908203. [DOI] [PubMed] [Google Scholar]
- Roberts JR, Reigart JR. Recognition and Management of Pesticide Poisonings. 6. US Environmental Protection Agency; Washington, D.C: 2013. [accessed 25.09.15]. pp. 110–117. http://www2.epa.gov/sites/production/files/2015-01/documents/rmpp_6thed_final_lowresopt.pdf. [Google Scholar]
- Rose MS, Smith LL. Tissue uptake of paraquat and diquat. Gen Pharmacol. 1977;8:173–176. doi: 10.1016/0306-3623(77)90045-3. [DOI] [PubMed] [Google Scholar]
- The Court of First Instance Annuls. The Directive Authorising Paraquat As An Active Plant Protection Substance. Court of First Instance of the European Communities; 2007. [accessed 25.09.15]. Available: < http://curia.europa.eu/en/actu/communiques/cp07/aff/cp070045en.pdf>. [Google Scholar]
- US Environmental Protection Agency. Reregistration Eligibility Decision: Diquat Dibromide. US Environmental Protection Agency; Washington DC: 1995. [Google Scholar]
- US Environmental Protection Agency. OPP Report on Incident Information: the Baseline. US Environmental Protection Agency; Washington DC: 2007. [Google Scholar]
- US Environmental Protection Agency. Reregistration Eligibility Decision: Paraquat Dichloride. US Environmental Protection Agency; Washington DC: 1997. [accessed 25.09.15]. Available: < http://www.epa.gov/pesticides/reregistration/REDs/0262red.pdf>. [Google Scholar]
- US Environmental Protection Agency. Label Review Manual. [accessed 25.09.15];Pre-cautionary statements. 2014 Chapter 7 Available: < http://www2.epa.gov/sites/production/files/2014-07/documents/chapter7_revised_final_0714.pdf>. [Google Scholar]
- Vale JA, Meredith TJ, Buckley BM. Paraquat poisoning: clinical features and immediate general management. Hum Toxicol. 1987;6:41–47. doi: 10.1177/096032718700600107. [DOI] [PubMed] [Google Scholar]
- Vanholder R, Colardyn F, De Reuck J, Praet M, Lameire N, Ringoir S. Diquat intoxication: report of two cases and review of the literature. Am J Med. 1981;70:1267–1271. doi: 10.1016/0002-9343(81)90836-6. [DOI] [PubMed] [Google Scholar]
- Watts M. Paraquat. [accessed 25.09.15];Penang, Malaysia: Pesticide Action Network Asia and the Pacific. 2011 Available: < http://wssroc.agron.ntu.edu.tw/note/Paraquat.pdf>.
- Wilks MF, Fernando R, Ariyananda PL, Eddleston M, Berry DJ, Tomenson JA, Buckley NA, Jayamanne S, Gunnell D, Dawson A. Improvement in survival after paraquat ingestion following introduction of a new formulation in Sri Lanka. PLoS Med. 2008;5(2):e49. doi: 10.1371/journal.pmed.0050049. http://dx.doi.org/10.1371/journal.pmed.0050049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2004. International Programme on Chemical Safety; 2005. [accessed 25.09.15]. Available: < http://www.who.int/ipcs/publications/pesticides_hazard_rev_3.pdf>. [Google Scholar]