Abstract
Attachment theory is useful for understanding how couples cope with stress across the lifespan. This study used the the Actor Partner Interdependence Model to examine the extent to which attachment related to one’s own (actor effect) and one’s partner’s (partner effect) depressive symptoms and marital satisfaction among older, married couples with a musculoskeletal condition. Pain and support were also examined as mediators. A group of 77 couples completed self-report measures as part of a larger study in which support was manipulated. Results revealed that, when one or both partners were insecurely attached, both partners reported greater depressive symptoms and lower satisfaction; however, pain and support were not significant mediators. Findings have implications for targeted, dyadic interventions to improve psychological health of couples coping with pain.
Keywords: musculoskeletal conditions, attachment, psychological health, late-life marriage, pain
Musculoskeletal conditions such as osteoarthritis and lower back pain are commonly experienced by older adults and can result in varying levels of pain (NIAMS, 2010). Not only can this be stressful for individuals with musculoskeletal conditions themselves (Hawker et al., 2011), but also for their spouses and their marriage (Badr, Laurenceau, Schart, Basen-Engquist, & Turk, 2010; Monin & Schulz, 2009; Schwartz, Slater, Birchler, & Atkinson, 1991). Examining factors that make couples dealing with musculoskeletal conditions more resilient or place them at heightened risk for depressive symptoms and lower marital satisfaction is important. We propose that one such factor is the interplay between couple members’ attachment orientations. Attachment orientations guide interpersonal stress regulation, or the interaction between the propensity to seek support from others in times of threat, such as when a person experiences pain (Meredith, Ownsworth, & Strong, 2008), and to care for others who are suffering (Mikulincer et al., 2001).
This study examined, in the context of older married couples dealing with a musculoskeletal condition, the extent to which both partners’ attachment orientations were associated with the respective partner’s reports of individual and relational aspects of psychological health (depressive symptoms and marital satisfaction). We also examined two potential mechanisms for hypothesized links between the partners’ attachment orientations and psychological health-perceptions of pain and spousal support.
Attachment Theory
According to attachment theory (Bowlby, 1969), humans have an evolutionary-based system designed to ensure proximity to caregivers during times of threat throughout the life-span. On the basis of interactions with primary caregivers in early life, people develop enduring cognitive schemas (attachment orientations) that continue into adulthood and guide their behavior and expectations in other relationships. Responsiveness from primary caregivers results in the development of comfort with interpersonal closeness and willingness to depend on others. This is referred to as secure attachment. In contrast, insecure attachment develops in response to inconsistent or unresponsive caregiving and can involve a tendency to be anxious regarding possible rejection, discomfort with close relationships, or both.
There are two fundamental dimensions with regard to attachment orientation (Brennan, Clark, & Shaver, 1998). The anxiety dimension assesses the degree to which the self is perceived to be unworthy of love and the degree to which the individual is worried about being rejected by others. The avoidance dimension assesses the degree to which individuals are uncomfortable with intimacy and dependence on others (Brennan et al., 1998). People are considered to be securely attached when they score low on both the anxiety and avoidance dimensions. There are other conceptualizations of attachment orientation; however, we used this approach as it is common in the close relationships literature.
Studies using attachment theory as a framework have mainly focused on young children and adults, although Bowlby theorized that attachment characterized experiences from “the cradle to the grave.” Despite there being a growing literature on attachment in the context of late life (Bradley & Cafferty, 2001; Consedine & Magai, 2003), the majority of this work has examined individuals rather than couples. The present study is unique in examining attachment dynamics in older marriages in which one person has a musculoskeletal condition causing pain, focusing on associations among each partner’s attachment orientation and each partner’s individual and relational psychological health.
Attachment Theory and Pain Conditions
Because affect regulation has been widely implicated in chronic pain conditions (Laganà & Hassija, 2012; Meredith, Strong, & Feeney, 2007; Monsen, Monsen, Svartberg, & Havik, 2002) and attachment theory is a theory of affect regulation (e.g., Mikulincer, Shaver, & Pereg, 2003), increasing attention has been paid to how attachment orientations relate to individuals’ chronic pain experiences (Meredith et al., 2008). Most of the studies on attachment and pain show that people who are more anxiously attached catastrophize their pain and experience with more depressive symptoms due to their condition, whereas avoidant attachment seems to be unrelated to well-being unless the person is also high in anxious attachment (e.g., Ciechanowski, Sullivan, Jensen, Romano, & Summers, 2003; Meredith et al., 2007). Less is known about how older couples cope, as reflected by their report of depressive symptoms and relationship satisfaction, when one partner has chronic pain and how this relates to each partner’s attachment orientations.
Each Spouse’s Attachment Orientations and Their Own Psychological Health
In general, attachment orientations have important consequences for older individuals’ psychological health. Secure attachment tends to be related to greater psychological well-being (e.g., Bradley & Cafferty, 2001; Merz & Consedine, 2009; Wensauer & Grossmann, 1995), whereas insecure attachment (both anxious and avoidant attachment) is negatively related to well-being (Kafetsios & Sideridis, 2006). More specifically, in the context of chronic pain, it has been shown that securely attached individuals report greater well-being (e.g., Andersen, 2012; Meredith et al., 2007). In contrast, insecurely attached individuals with pain tend to report more depressive symptoms and mal-adaptive coping strategies (e.g., Andersen, 2012; Ciechanowski et al., 2003; Mikulincer & Florian, 1998).
It is theorized that the attachment orientations of individuals facing stressors such aschronic pain have important consequences for their psychological health because attachment orientations are associated with differences in the ability to regulate distress (Meredith et al., 2008; Wei, Vogel, Ku, & Zakalik, 2005) and utilize social support (e.g., Kafetsios & Sideridis, 2006; Karantzas & Cole, 2011). Research shows that people with high anxious attachment tend to overreact to their negative feelings in order to elicit support from others and to ensure others’ availability, an emotion regulation strategy called hyperactivation (e.g., Cassidy & Kobak, 1988). In contrast, people high in avoidant attachment tend to suppress their negative feelings and maximize their distance from others in order to avoid distress caused by others unavailability, a strategy referred to as deactivation (e.g., Cassidy, 2000; Cassidy & Kobak, 1988). These affect-regulation strategies are thought to have short-term adaptive value by reducing uncomfortable feelings toward others who have been insensitive or rejecting (Cassidy, 2000). However, the rigid use of these affect strategies tend to contribute to depressive symptoms and anxiety (Lopez, Mauricio, Gormley, Simko,& Berger, 2001) and physical symptoms (Sadava, Busseri, Molnar, Perrier, & DeCourville, 2009).
When an individual with pain is married, not only is their pain a stressor for themselves, but also for their spouses. Spouses are faced with regulating negative affect in response to their partner’s pain (Monin & Schulz, 2009), making spouses’ attachment orientations relevant as well (Monin & Schulz, 2010). However, no studies to our knowledge have examined how the attachment orientation of a spouse of a person with pain relates to the spouse’s own psychological health. One exception is a study by McWilliams and Holmberg (2010), which asked people about pain catastrophizing with regard to their significant other’s pain. They found that anxiously attached individuals reported feeling helpless and distressed, whereas avoidant individuals were less likely to ruminate about their partner’s pain and were also less likely to feel helpless. There have also been studies of spouses of individuals with cancer. For example, a study of early-stage lung-cancer patients and their spouses showed that more avoidantly attached spouses reported significantly higher levels of depressed mood than less avoidant spouses. Also, spouses high in attachment anxiety reported higher anxious mood than spouses low in attachment anxiety (Porter et al., 2012). These related studies suggest that the attachment style of spouses has implications for how spouses cope with their partner’s pain experience.
In the study of couples it is also important to understand relational aspects of each spouse’s psychological health. No research has examined how each partner’s attachment orientation relates to each partner’s own relationship satisfaction in the context of chronic pain. However, there have been some studies in the cancer caregiving literature showing that secure attachment is associated with greater self-reported marital satisfaction for both husbands and wives (Shields, Travis, & Rousseau, 2000). The latter research suggests that, when couples are coping with health-related stressors, attachment orientation may be an important factor in predicting marital satisfaction.
Attachment Orientation and Partner’s Psychological Health
Attachment theory emphasizes the importance of dyadic processes in which one partner’s outcomes are linked to the other partner’s needs, goals, and behavioral tendencies (Kane et al., 2007). Despite this theoretical emphasis on interpersonal processes, most empirical studies on attachment and relationships have taken an intrapersonal perspective in which one partner’s attachment orientation is linked to his or her own outcomes. In the chronic pain literature this has also been the case. One exception is a laboratory study of young women who completed a pain-eliciting tourniquet task while accompanied by their romantic partners. In this study it was found that insecurely attached women who were accompanied by an anxiously attached romantic partner responded most negatively to pain (Wilson & Ruben, 2011).
One can also draw from other health-related stress contexts with which older couples are faced, such as cancer and dementia, in predicting how older spouses with pain may be affected by their partner’s attachment orientation. For example, in their study of lung-cancer patients and spouses, Porter and colleagues (2012) found that spouse avoidant attachment was significantly associated with patient reports of increased pain and poorer functional well-being, and that spouse anxious attachment was associated with poorer martial quality. They also found that dyads in which both partners were insecurely attached had significantly poorer adjustment compared to dyads in which both partners reported secure attachment. Similarly, the study of couples with cancer by Shields and colleagues (2000) also showed partner effects of attachment on marital satisfaction, such that the secure attachment of wives was related to greater marital satisfaction as reported by husbands. In addition, husbands and wives generally had lower marital satisfaction when their partner was high in avoidant attachment. In the context of dementia, Monin, Schulz and Kershaw (2013) found that anxiously attached individuals with Alzheimer’s disease reported more psychological and physical symptoms of suffering when their spousal caregivers were also anxiously attached. These past studies suggest that each partner’s attachment orientation is likely to be related to each partner’s psychological health, both in terms of depressive symptoms and marital satisfaction.
Perceptions of Pain and Spousal Support as Potential Mediators of Attachment and Psychological Health
First, perceived pain may be a mechanism through which attachment orientation affects one’s own and one’s partner’s psychological health. For example, as already described, anxiously attached individuals tend to catastrophize their pain leading to depressive symptoms in the self and close partners (Ciechanowski et al., 2003; McWilliams & Asmundson, 2007). In contrast, avoidant individuals may suppress their pain, which tends to be a maladaptive coping strategy for the self (e.g., Masedo & Esteve, 2007). Lack of expression may also be distressing for the spouse, as it may be seen as a sign of less intimacy or comfort with support-seeking (Monin, Martire, Schulz, & Clark, 2009).
Second, spouses’ perceptions of the pain of the individual with the chronic condition may also be a pathway through which attachment relates to both partner’s well-being. Attachment orientations guide not only support-seeking behavior, but also caregiving behavior, which often involves being attuned to others’ signs of distress (Bowlby, 1969). Indeed, attachment security in young adults is associated with more empathic reactions to others’ distress (Mikulicer et al., 2001), and anxious attachment is associated with more personal distress reactions to others’ distress, including older adults with osteoarthritis (Monin, Feeney, & Schulz, 2012; Monin, Schulz, Feeney, & Cook, 2010).
In addition, perceptions of spouse support may account for the associations between attachment orientation and psychological health among individuals with pain. For instance, Collins and Feeney (2004) showed that individuals are predisposed to appraise support experiences in ways consistent with their chronic working models. Specifically, insecure individuals tend to view ambiguous behaviors from their partners as unsupportive, whereas secure individuals tend to interpret the same behaviors as more supportive. Among older adults, specifically, it has also been shown that avoidant attachment is related to lower levels of perceived support and that this is a mechanism for poorer mental health outcomes (Kafetsios & Sideridis, 2006). Taken together, it is possible that self-reported pain, the spouse’s perceptions of pain, and perceived support from the spouse could account for associations between partners’ attachment orientations and psychological health.
Current Study
Past research on couples dealing with health-related stressors (e.g., cancer, dementia, pain) suggests that an individual’s attachment orientation is related to his or her own psychological health (an actor effect), and that an individual’s attachment orientation is related to his or her partner’s psychological health (a partner effect). In the present study we take this a step further positing that, among older couples coping with a musculoskeletal condition, the attachment orientation of both partners will have an interactive effect on both partners’ individual and relational psychological health. Specifically, we hypothesize that, when one or both partners are high in attachment insecurity (either anxious or avoidant attachment), both partners will report more depressive symptoms (Hypothesis 1) and lower marital satisfaction (Hypothesis 2) than when one or both partners are low in attachment insecurity. In doing so we also explore whether these associations apply to both partners, only the partner with pain, or only the spouse.
Next, we hypothesize that perceived pain and spousal support will mediate the associations between partners’ attachment orientations and psychological health. We predict that insecure attachment in one or both partners will be related to greater perceptions of pain, and greater perceived pain will be related to lower psychological health (Hypothesis 3). We also hypothesize that more secure attachment in one or both partners will be associated with more responsive support, and more responsive support will be associated with greater psychological health (Hypothesis 4).
Method
Participants
A total of 77 individuals with a self-reported musculoskeletal condition (IMCs, i.e., osteoarthritis, lower back pain) and their spouses were recruited from newspaper advertisements and community bulletins. In order to be eligible to participate, 1) the IMCs had to be over 50 years old; 2) the couple had to be married or in a marriage-like relationship and have lived together for at least 6 months; 3) the spouse could not have a musculoskeletal condition; and 4) if the spouse had another chronic condition that caused pain, the spouse had to have less pain on average than the IMC.1 Participants also completed the Short Portable Mental Status Questionnaire – Mini-Mental State Examination (SPMSQ; Pfeiffer, 1975) to evaluate their cognitive functioning. Those who correctly answered at least 7 out of 10 items were considered to be eligible for the study. Spouses who were taking beta-blockers, a class of drug affecting heart rate, were excluded because of the aims of the parent study.
The mean age of the IMCs was 65.90 (SD = 7.88) and the mean age of spouses was 64.81 (SD = 8.41). The IMCs reported that they had been experiencing chronic pain from a musculoskeletal condition for 123.77 months on average (SD = 129.79, range = 0–636). Sixty-seven (87.01%) IMCs reported that they had osteoarthritis in at least one location. The remaining participants reported lower back pain unrelated to arthritis. Fifty (64.90%) IMCs reported arthritis in a second location. Twenty-nine (38%) IMCs reported their primary site of pain to be knees, 12 (18%) back, 10 (13%) feet or ankles, 7 (10.4%) hips, 7 (10.4%) hands/fingers, and 2 (3%) shoulders. The remaining participants did not report a primary location. See Table 1 for more details of participant characteristics.
Table 1.
Participant demographics
| Sample characteristic | Spouse (N = 77) |
IMC (N = 77) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Children* | ||||
| Yes | 59 | (77.6) | 59 | (77.6) |
| No | 17 | (22.4) | 17 | (22.4) |
| Gender | ||||
| Male | 45 | (58.4) | 32 | (41.6) |
| Female | 32 | (41.6) | 45 | (58.4) |
| Education | ||||
| Did not complete high school | 5 | (6.5) | 4 | (5.2) |
| Completed high school | 24 | (31.2) | 22 | (28.6) |
| Postsecondary education/training | 48 | (62.3) | 51 | (66.2) |
| Employment | ||||
| Employed | 30 | (39.5) | 27 | (35.1) |
| Homemaker | 3 | (3.9) | 2 | (2.6) |
| Unemployed/retired | 43 | (56.6) | 48 | (62.3) |
| Race | ||||
| White | 72 | (93.5) | 75 | (97.4) |
| African American | 1 | (1.3) | 1 | (1.3) |
| Other | 4 | (5.2) | 1 | (1.3) |
| Family income*** | ||||
| Less than $50,000 | 35 | (47.95) | – | – |
| $50,000-$99,999 | 31 | (42.47) | – | – |
| $100,000 or more | 7 | (9.6) | – | – |
Notes. One spouse did not report information on children.
One spouse did not report on employment status.
Four spouses did not report income.
Procedure
After signing informed consent, both partners participated in an experiment manipulating the spouse’s exposure to IMC pain, the spouse’s support provision, and IMC feedback concerning the support. The primary aim of the parent study was to examine older adults’ cardiovascular reactivity to witnessing a partner’s pain and to determine whether providing support and receiving appreciative feedback from the partner attenuates reactivity. Because the experiment had the potential to influence participants’ responses to the self-report questionnaires in the present study, we explain the parent study procedures in detail.
In the experiment, the spouse watched on a video screen in an adjacent room the IMC complete a simulated household task in which he/she loaded canned goods into two grocery bags (5 lbs each), carried the bags across an 8 ft space, unloaded the bags, and repeated the process for 3 min. This task was similar to those used in previous research with participants with musculoskeletal conditions to elicit pain expression (Martire et al., 2006; Monin et al., 2010; Romano et al., 1991). The IMC was instructed to freely express pain verbally and nonverbally as experienced, to act as naturally as possible, and to pretend to be doing the task at home. Participants were told they could stop at any time.
Spouses were assigned to one of three conditions. In the control condition (n = 26 couples), spouses were asked to watch the IMC perform the grocery task and to say to him/herself, “It has been 1 minute,” at the 1-minute mark, “It has been 2 minutes,” at the 2-minute mark, and “It has been 3 minutes,” at the 3-minute mark. The door was closed in this condition. In the other two conditions (the support conditions), spouses were instructed to watch the IMC perform the task and to say through the open door, “It has been 1 minute. Great job [spouse’s name],” “It has been 2 minutes. You are doing great!” and “It has been 3 minutes. You did a good job!” Before the task, IMCs were instructed not to respond to the spouse’s comments.
After the task was completed, the IMCs reported their pain and the spouse reported their perception of the IMC’s pain during the task. On a scale from 1 (no pain at all) to 10 (extreme pain), the mean pain reported by IMCs was 2.33 (SD = 1.72) and the mean perceived pain of the IMCs reported by spouses was 2.80 (SD = 1.87). A paired t-test showed that partners’ ratings of the IMC’s pain were not significantly different, t(74) = −1.89, p = .06.
Then the spouse received a note written in the IMC’s handwriting. In the control condition and in one of the support conditions (the support only condition; n = 25 couples), the note said the task was challenging. In the other support condition, the note said the task was challenging, and that the IMC appreciated the spouse’s support (the support plus appreciation condition; n = 26 couples).
Next there was a resting period of 10 minutes for spouses, and they provided two verbal accounts of instances in which they felt their partner with the musculoskeletal condition had experienced suffering. After each partner had completed their appropriate tasks, a background questionnaire was given to each partner in separate rooms.
Measures
Attachment Orientation
Both couple members rated their feelings about their relationship with their current romantic partner, using a modified 26-item version of the Experiences in Close Relationships Scale (Brennan et al., 1998; Feeney, 2007). This measure assesses two dimensions of adult attachment: attachment anxiety (i.e., “I worry a lot about my relationship with my partner.”) and attachment avoidance (i.e., “I am nervous when my partner gets too close to me.”). Participants responded using a 7-point scale for each item (i.e., 1 = disagree strongly; 7 = agree strongly). Relationship-specific attachment was measured, which has been reported to be more accessible than trait attachment during interactions with romantic relationship partners (Baldwin, Keelan, Fehr, Enns, & Koh-Rangarajoo, 1996). For spouses, the Cronbach’s α for attachment avoidance was 0.77 (M = 2.36, SD = 1.03), and for attachment anxiety it was 0.79 (M = 2.46, SD = 0.96). For IMCs, the Cronbach’s α for attachment avoidance was 0.61 (M = 2.34, SD = 1.03), and for attachment anxiety it was 0.82 (M = 2.33, SD = 1.02). The means and the standard deviations for female IMCs and spouses’ attachment avoidance were 2.34 (SD = 1.00) and 2.33 (SD = 0.95), respectively; for attachment anxiety they were 2.15 (SD = 0.90) and 2.62 (SD = 0.87), respectively. The means for male IMCs and spouses’ attachment avoidance were 2.34 (SD = 1.02) and 2.38 (SD = 1.09), respectively; for attachment anxiety they were 2.60 (SD = 1.12) and 2.35 (SD = 1.01), respectively. These means are lower than attachment dimension (anxiety and avoidance) norms for both younger and older age groups as reported by Fraley (2012).
Depressive Symptoms
We used the 20-item version of the Center for Epidemiological Studies–Depression scale (CES-D) to measure both partners’ depressive symptoms during the past week (Radloff, 1977). Examples of items included “I was bothered by things that don’t usually bother me” and “I felt depressed.” Participants indicated how often they felt this way using a scale from 0 (rarely or none of the time) to 3 (most or all of the time). For spouses, the Cronbach’s α was 0.84 with a mean score of 9.60 (SD = 7.94); for IMCs, the Cronbach’s α was 0.76 with a mean score of 7.72 (SD = 6.07).
Marital Satisfaction
The self-reported marital satisfaction of both partners was assessed using the 16-item Locke and Wallace Marital Adjustment Test (MAT; Locke & Wallace, 1959). Several aspects of their relationship quality were measured: 1) their general level of marital happiness, using a scale from 0 (very unhappy) to 6 (perfectly happy); 2) agreement on items (i.e., handling family finances, matters of recreation, friends, sex relations, etc.), using a scale from 0 (always disagree) to 5 (always agree); and 3) questions on whether or not they give in when disagreements arise, their engagement in outside interests, and their views to current partner. Scores range from 28 to 119. The higher the MAT score, the higher level of marital satisfaction. For spouses, the mean was 95.69 (SD = 19.35). For IMCs, the mean was 96.36 (SD = 15.99). The Cronbach’s αs were 0.74 for IMCs and 0.80 for spouses.
IMC Perceived Support
IMCs were asked to think about whether they could count on their spouse for help and comfort when they were feeling distressed, and they were asked to indicate how much they agreed or disagreed on scale from 1 (disagree strongly) to 5 (agree strongly) with 10 statements (e.g., “My spouse is always there for me whenever I need him/her”; “When I’m feeling distressed about something, I know I can turn to my spouse for comfort and assistance”; “When I am feeling worried or distressed about something, it only makes things worse to tell my spouse about it.”) This was a measure developed by Feeney to assess responsiveness to need or home base security (Feeney, 2004, 2007). The Cronbach’s α was 0.91, and the mean was 2.33 (SD = .92, range = 1–5.29).
Covariates
Average Pain and Pain Medication Use in Daily Life
To measure average pain, IMCs were asked the following: “In the past 7 days, on the average, how intense was your pain rated on a 0–10 scale where 0 is no pain and 10 is pain as bad as could be.” The mean rated average pain was 3.65 (SD = 2.49, range = 0–10). IMCs were also asked whether they took medication for pain, and if so what medication. Out of the 77 IMCs, 23 were regularly taking NSAIDs, 8 took opioids, 7 took Tylenol, and 3 took other medications to treat pain specifically (i.e., Elavil, Gabapentin, and Cymbalta).
Comorbidity/Physical Conditions
The physical condition index (PCI) was used to evaluate the physical health of both partners (Katz, Chang, Sangha, Fossel, & Bates, 1996). This variable was measured as a potential covariate. This allowed us to account for both partner’s physical health in general. This was especially important for spouses who may also have been burdened by chronic conditions other than musculoskeletal conditions that caused psychological stress. The PCI is a self-report survey with 24 items. Questions include respondents’ current conditions related to cardiovascular, respiratory, digestive problems, surgery, and cancer among other physical health issues. Scores range from 0 to 24. For spouse’s physical conditions, the mean score was 2.91 (SD = 1.95). For IMCs, the mean score was 3.69 (SD = 2.47).
Analysis Plan
First, we examined correlations among all study variables. Next, we examined whether there were differences in study variables between experimental conditions to help rule out potential moderating effects of the support manipulation on the self-report measures in the present study. If there were differences among conditions, we planned to control for experimental condition by entering dichotomous variables for support provision (0 = no, 1 = yes) and support feedback (0 = no, 1 = yes) in our main models.
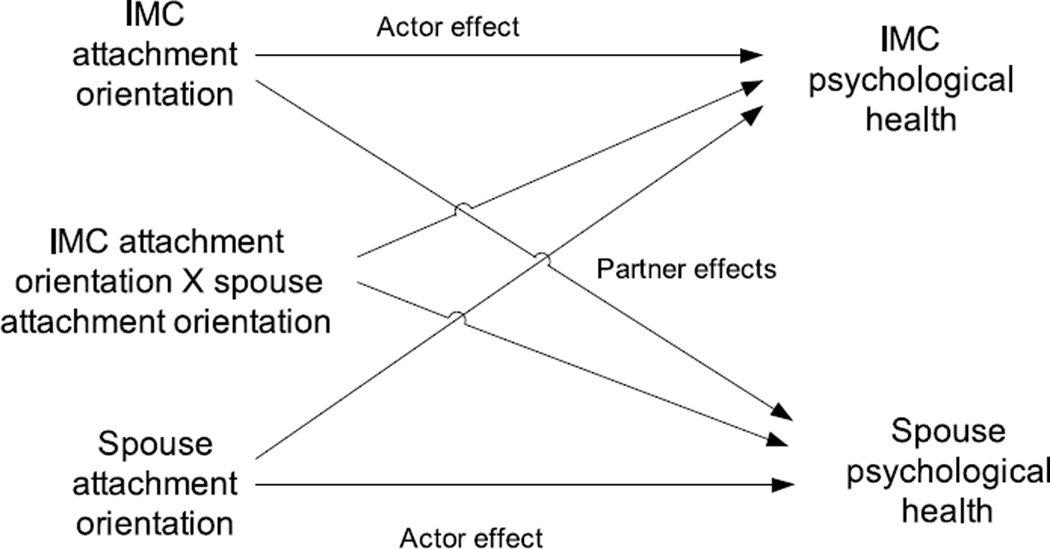
To test models that included both partners’ attachment variables predicting both partners’ depressive symptoms and marital satisfaction (Hypothesis 1 and 2), we used a dyadic data analytic technique. Specifically, we used the actor-partner interdependence model (APIM; Kenny, Kashy, & Cook, 2006) with the mixed procedure in SPSS to deal with the nonindependence of the data and address questions on mutual influence. APIM is a dual-intercept model ensuring to calculate two effects: “actor effects” and “partner effects” (see Figure 1).
Figure 1.
Proposed, simplified actor partner interdependence model.
Actor effect represents the influence that an individual’s score on a predictor variable has on his/her own score on a dependent variable (e.g., the association of the attachment anxiety of the IMC to the depression of the IMC). A partner effect represents the influence that an individual’s score on a predictor variable has on his/her partner’s score on a dependent variable (e.g., the association of the attachment avoidance of the IMC on the spouse’s marital satisfaction). To explore whether or not each effect was specific to the outcome of the IMC or the spouse, we tested for interactions with a “role” variable, where spouses were coded as 1 and IMC were coded as −1. In a second set of models, we also entered interactions between actor and partner variables to examine the multiplicative effects of both partners’ attachment dimensions on both partner’s physical health outcomes. In our analyses, we centered all independent variables (attachment dimensions) on the grand mean.
To test whether perceived pain (Hypothesis 3) and support (Hypothesis 4) mediated the associations between attachment and each indicator of psychological health (depressive symptoms and marital satisfaction), we first examined the correlations between the attachment variables and the potential mediators and between the mediators and the psychological health variables. We did this before pursuing more formal mediation models.
Finally, in follow-up analyses, to determine whether the experiment had a significant effect on psychological health variables depending on each partner’s attachment, we ran the mixed models again entering interactions between the attachment variables and the experimental dummy coded variables. There were no significant interactions with the experimental variables that remained significant in the simplified models. For the sake of parsimony we do not report the models with these nonsignificant interaction terms.
Results
Preliminary Analyses
As shown in Table 2, the correlation analysis showed that anxious and avoidant attachment were positively related for both IMCs and spouses; IMCs with older spouses had less attachment anxiety; and avoidant spouses had more chronic conditions. With regard to pain measures, IMCs’ average pain was associated with their task pain; spouses’ perceptions of the IMCs task pain were positively related to IMCs’ self-reports; and men reported greater perceived task pain than women. In terms of psychological health, IMCs’ marital satisfaction and depressive symptoms were significantly negatively associated, and IMC’s and spouses’ marital satisfaction were significantly positively associated.
Table 2.
Intercorrelations among independent variables and potential covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IMC | ||||||||||||||||||||
| 1. Age | −.09 | −.12 | .01 | −.04 | −.10 | .16 | .07 | .18 | −.15 | .49** | −.08 | .12 | .11 | −.07 | .14 | −.15 | .29* | .03 | .18 | |
| 2. Edu | −.07 | .12 | −.09 | .14 | .05 | −.16 | −.17 | .04 | .07 | .48** | −.06 | .01 | −.12 | −.12 | .25* | .05 | −.08 | −.07 | ||
| 3. Anx | .36** | −.12 | .01 | .04 | .09 | −.41** | .41** | −.26* | −.05 | .14 | .19 | −.05 | −.17 | −.22 | .12 | −.43** | −.04 | |||
| 4. Avoid | −.05 | −.03 | −.02 | −.19 | −.53** | .17 | −.16 | −.04 | .28* | .17 | −.09 | −.21 | .00 | −.04 | −.30** | −.10 | ||||
| 5. Av pain | .39** | .21# | .19# | −.07 | .02 | −.05 | −.02 | −.04 | −.05 | .19 | −.07 | −.10 | −.22 | −.03 | −.07 | |||||
| 6. Task pain | .01 | .18 | −.03 | .14 | .02 | .12 | −.02 | .07 | .37** | .14 | .23* | −.02 | −.06 | .14 | ||||||
| 7. Chronic cond | .03 | −.14 | .08 | .01 | −.16 | .11 | .21 | −.03 | .09 | −.04 | .09 | −.03 | .01 | |||||||
| 8. Perc supp | −.01 | .15 | .21# | .00 | .05 | −.01 | −.05 | .09 | −.06 | .04 | .16 | −.05 | ||||||||
| 9. Marital sat | −.49** | .20# | .00 | −.11 | −.24* | .10 | .08 | .14 | .00 | .47** | −06 | |||||||||
| 10. Depress | −.12 | .05 | .05 | .30* | .03 | .13 | −.03 | .16 | −.28* | .14 | ||||||||||
| Spouse | ||||||||||||||||||||
| 11. Age | .10 | −.04 | .05 | −.17 | .21# | .28* | .42** | .31** | −.13 | |||||||||||
| 12. Edu | −.05 | .01 | −.16 | −.02 | −.02 | .12 | −.08 | −.15 | ||||||||||||
| 13. Anx | .33** | −.03 | .05 | −.14 | −.23# | −.25* | .18 | |||||||||||||
| 14. Avoid | −.11 | .29* | .03 | −.07 | −.57** | .30** | ||||||||||||||
| 15. Perc task pain | .06 | .08 | −.18 | .03 | .15 | |||||||||||||||
| 16. Chronic cond | .15 | .04 | .11 | .28* | ||||||||||||||||
| 17. Gender | .09 | .23* | −.08 | |||||||||||||||||
| 18. Mar length | .13 | −.18 | ||||||||||||||||||
| 19. Marital sat | −.22# | |||||||||||||||||||
| 20. Depress | ||||||||||||||||||||
Note. IMC = individual with a musculoskeletal condition. Edu = education, Anx = attachment anxiety, Avoid = attachment avoidance, Av pain = average pain in daily life, Chronic cond = chronic conditions, Marital sat = marital satisfaction, Depress = depressive symptoms, Perc task pain = perceived task pain, Mar length = marriage length.
p < .00,
p < .05,
p < .10.
Gender: 1 = male, ø = female.
According to the ANOVAs, there were significant differences in spouses’ avoidant attachment (F(2, 73) = 3.40, p = .04) and depressive symptoms (F(2, 74) = 3.35, p = .04) among the experimental conditions. Spouses reported significantly greater avoidant attachment and depressive symptoms in the support plus neutral feedback condition (avoidant attachment: M = 2.72; depressive symptoms: M = 12.76) compared to the support plus appreciation feedback condition (avoidant attachment: M = 1.98, Tukey’s HSD mean difference = −.73, SE = .28, p = .03; depressive symptoms: M = 7.50, Tukey’s HSD mean difference = 5.26, SE = 2.16, p = .045). There were no other significant differences between conditions. IMC perceived support did not significantly differ by condition (F(2, 73) = .56, p = .58).
Based on these preliminary analyses, we controlled for each partners’ age and sex as well as experimental condition in the mixed models examining each of the main hypotheses. We limit to these covariates that were associated with both the hypothesized predictors and outcomes in the proposed models.
Hypothesis 1: Do Both Partners’ Attachment Orientations Relate to Both Partners’ Depressive Symptoms?
As shown in Table 3, there was an actor effect of anxious attachment such that both IMCs and spouses who were anxiously attached reported greater depressive symptoms. Second, there was a significant interaction between role and partner avoidance. Simple slopes analysis showed that IMCs’ depressive symptoms were positively related to spouse’s avoidant attachment (B = 2.34, SE = .71, t(65.13) = 3.29, p = .002); whereas, spouses’ depressive symptoms were high regardless of whether or not the IMC was high or low in avoidant attachment (B = −.47, SE = 1.15, t(68.50) = −.41, p = .68).
Table 3.
Model 1: Simplified SPSS mixed model testing actor, partner, and role effects
| Depressive symptoms | Marital satisfaction | |||
|---|---|---|---|---|
| B | SE | B | SE | |
| Intercept | 8.73** | 0.96 | 94.16** | 2.04 |
| Role | 0.58 | 0.49 | 0.34 | 0.93 |
| Support | 1.15 | 1.39 | 3.61 | 2.94 |
| Feedback | −2.40 | 1.45 | −0.33 | 3.06 |
| Actor age | − .19** | 0.07 | 0.49** | 0.14 |
| Partner age | 0.11 | 0.07 | −0.07 | 0.14 |
| Actor anxiety | 2.01** | 0.58 | −1.48 | 1.20 |
| Partner anxiety | − .36 | 0.58 | −1.28 | 1.20 |
| Actor avoidance | 0.96 | 0.55 | −7.91** | 1.14 |
| Partner avoidance | −0.13 | 0.57 | −2.22 | 1.14 |
| Role * partner anxiety | − | − | −2.20* | 1.05 |
| Role * partner avoidance | −1.19* | 0.51 | − | − |
Note. All independent variables were centered on the mean and simultaneously entered into the models.
p < .01,
p < .05.
The explained variance was 13.9% for depressive symptoms and 30.8% for marital satisfaction.
As shown in Table 4, for both partners there was a significant interaction between actor anxious attachment and partner avoidant attachment, such that people reported the least depressive symptoms when they were low in anxiety and their partners were low in avoidance. When actor anxiety was low, partner avoidance was marginally positively associated with actor depressive symptoms (B = 2.29, SE = 1.18, t(91.01) = 1.94, p = .055). When actor anxiety was high, partner avoidance was not significantly associated with actor depressive symptoms (B = −.42, SE = .70, t(118.29) = −.60, p = .55).
Table 4.
Model 2: Simplified SPSS mixed model with actor, partner, and role interaction predicting depressive symptoms
| B | SE | |
|---|---|---|
| Intercept | 9.95** | 0.99 |
| Role | 0.86 | 0.47 |
| Support | 1.01 | 1.35 |
| Feedback | −2.57 | 1.45 |
| Actor age | − .20 | 0.07 |
| Partner age | 0.13 | 0.07 |
| Actor anxiety | 1.03 | 0.68 |
| Partner anxiety | −0.44 | 0.67 |
| Actor avoidance | 2.14** | 0.66 |
| Partner avoidance | 1.16 | 0.66 |
| Role * actor anxiety | −0.67 | 0.61 |
| Role * partner anxiety | −0.41 | 0.59 |
| Role * actor avoidance | 0.75 | 0.58 |
| Role * partner avoidance | −1.12 | 0.58 |
| Actor anxiety * partner anxiety | 0.95 | 0.83 |
| Actor avoidance * partner avoidance | 1.22 | 0.90 |
| Partner anxiety * partner avoidance | −1.70** | 0.57 |
| Actor anxiety * actor avoidance | − .68 | 0.58 |
| Actor anxiety * partner avoidance | −1.70 | 0.59 |
| Partner anxiety * actor avoidance | −0.73 | 0.62 |
| Role * actor anxiety * partner anxiety | −1.37* | 0.62 |
Note. All independent variables were centered on the mean and simultaneously entered into the models. There were no significant actor X partner interactions predicting marital satisfaction.
p < .01,
p < .05.
The explained variance for depressive symptoms was 16.1%.
Also shown in Table 4, there was a significant interaction among role, actor anxiety, and partner anxiety predicting depressive symptoms. IMCs in particular reported the most depressive symptoms when they were high in anxious attachment and their spouses were high in anxious attachment. Simple slopes analysis showed that when IMCs were high in attachment anxiety, spouses attachment anxiety was not significantly associated with IMCs depressive symptoms (B = 2.16, SE = 1.39, t(63.42) = 1.55, p = .13), whereas when IMCs were low in attachment anxiety, spouses attachment anxiety was significantly negatively associated with IMCs depressive symptoms (B = −2.41, SE = 1.00, t(65.84) = −2.42, p = .02). The interaction between each partners’ attachment anxiety scores predicting spouses’ depressive symptoms was not significant (B = −.78, SE = 1.30, t(70.05) = −.60, p = .55).
Hypothesis 2: Do Both Partners’ Attachment Orientations Relate to Both Partners’ Marital Satisfaction?
As shown in Table 3, there was a significant actor effect of avoidant attachment on marital satisfaction, such that both partners reported lower marital satisfaction when they were high in attachment avoidance. Also, there was a significant interaction between role and partner anxious attachment, such that spouses reported marginally significantly lower marital satisfaction when the IMC was high in attachment anxiety (B = −3.25, SE = 1.92, t(68.16) = −1.69, p = .10), whereas IMC reported marginally significantly higher marital satisfaction when the spouse was high in anxious attachment (B = 3.31, SE = 2.00, t(66.15) = 1.65, p = .10).
Hypotheses 3 and 4: Does IMC Pain or Perceived Support Mediate the Associations Between Attachment and Depressive Symptoms and Attachment and Marital Satisfaction?
As shown in Table 2, IMC pain and perceived support were not significantly associated with either partner’s attachment dimensions, marital satisfaction, or depressive symptoms, thus not satisfying criteria for mediation.
Discussion
Past research shows that attachment security has important implications for psychological health in couples coping with health-related stressors (e.g., dementia, cancer). The present study extends past research by examining the interplay between partners’ attachment orientations and indicators of individual and relational psychological health among older couples coping with a musculoskeletal condition. In addition to showing that attachment is related to one’s own and one’s partners’ psychological health, our study shows interactive associations between partners’ attachment and psychological health. Here we discuss our findings in terms of their support for theoretical processes related to attachment anxiety and avoidance.
Attachment Anxiety
We found that one’s own attachment anxiety was associated with greater depressive symptoms for both individuals with musculoskeletal conditions and their spouses. This is consistent with a large literature showing that anxiously attached individuals generally report more depressive symptoms and maladaptive coping strategies in the face of chronic stress (e.g., Andersen, 2012; Ciechanowski et al., 2003; Mikulincer & Florian, 1998). Attachment theory suggests that this is because of anxiously attached individuals’ hyperactivated attachment system, which causes them to be especially sensitive to negative emotion and to display signs of distress to elicit social support (Cassidy & Kobak, 1988; McWilliams & Asmundson, 2007). Our study shows that this sensitivity may be in reaction to either one’s own health condition or to one’s spouses’ health condition, as previous work with spousal caregivers of osteo-arthritis patients also shows (Monin et al., 2012).
Importantly, we also found that when both partners were high in anxious attachment, the person with the musculoskeletal condition reported the greatest depressive symptoms. The fact that the person with the chronic condition was particularly affected by both partners’ attachment insecurity also fits with prior findings. For example, in a study of individuals with dementia and their spouses, individuals with dementia reported the greatest physical symptoms when both partners were high in attachment anxiety (Monin et al., 2013). It has been suggested that insecure “care-recipients” may be particularly likely to suffer when their spouses are unable to provide a secure caregiving environment (Solomon & George, 1996) and when both spouses are experiencing heightened negative affect (Monin & Schulz, 2009; Wei et al., 2005). In other words, attachment anxiety is likely to hinder both the support-seeking and caregiving processes for the couple, which may be especially harmful to the person who needs more support.
We also found that attachment anxiety was related to marital satisfaction. Specifically, spouses reported lower marital satisfaction when their partner with the musculoskeletal condition was high in anxious attachment. As individuals high in anxious attachment are more likely to catastrophize their pain (Ciechanowski et al., 2003) and seek support (Kafetsios & Sideridis, 2006) than individuals low in anxious attachment, it may be emotionally and/or physically demanding for their spouses. Instead of spouses experiencing depressive symptoms that are more self-oriented when their partner is anxious, spouses may feel other negative emotions toward their partner, such as frustration or guilt, manifesting as low marital satisfaction. This finding highlights the importance of examining both individual and relational aspects of psychological health when examining how couples cope with a partner’s chronic condition.
Attachment Avoidance
Avoidant attachment was also related to both partners’ psychological health. Specifically, high avoidant attachment was associated with lower marital satisfaction for both partners, a finding consistent with numerous studies of healthy and unhealthy and younger and older populations (e.g., Feeney, 1994). Because individuals who are high in avoidant attachment report being uncomfortable with intimacy and receiving and providing support (Brennan et al., 1998), it is likely that their close interpersonal relationships suffer. This may be especially the case when one partner in the relationship is experiencing physical symptoms and requires caregiving. Avoidant individuals with the musculoskeletal condition may feel uncomfortable asking for support (Collins & Feeney, 2000) and avoidant spouses may feel uncomfortable providing support (Feeney & Collins, 2001), potentially leading to a breakdown in communication that is central to marital satisfaction. Also consistent with this, we found that the individuals with the musculoskeletal condition reported more depressive symptoms when their spouses were high in avoidant attachment perhaps indicating that they may not have received adequate support. Taken together, the fact that both partners’ avoidant attachment had implications for both partners’ psychological health suggests that avoidant attachment may also impede both the support-seeking and caregiving processes for the couple trying to cope with the musculoskeletal condition.
On the other hand, we found that being low in attachment anxiety and having a partner low in avoidant attachment was associated with lower depressive symptoms for both the individual with the musculoskeletal condition and the spouse. Thus, not only does being high in attachment insecurity have potential risks for poor psychological health, we also showed that security in both partners may have a synergistic effect on the well-being of the couple. More specifically, being less anxious may aid in regulating one’s own stress and having a partner low in avoidance may be linked with receiving better support.
Although theory and past research would suggest that perceptions of pain and support at least partially explain why attachment is linked with psychological health, we did not find evidence for this in our study. Our null results may have been stemmed from the fact that our sample experienced low levels of pain during the experiment and in daily life. Also, our measure of support only tapped emotional support and did not refer to a specific situation. It may be that avoidant attachment, for example, hindered other types of caregiving such as tangible support that individuals with chronic pain may desire.
Finally, it is interesting to note that age was associated with lower depressive symptoms and greater marital satisfaction, providing further evidence for research showing that people tend to experience more harmonious relationships with close others as they age (Carstensen, Gottman, & Levenson, 1995). Also, length of marriage was not significantly related to relationship satisfaction or attachment security. This may reflect that some older couples were remarried and also experienced high levels of marital satisfaction as newlyweds.
Strengths, Limitations, and Future Directions
First, although attachment theory has stimulated an enormous body of empirical research focused on infancy, childhood, and early adulthood, research on late-life relationships using this perspective has been relatively limited (for exceptions see Consedine, Fiori, Tuck, & Merz, 2013; Consedine & Magai, 2003). Furthermore, research on attachment and older adults has mainly been conducted with individuals rather than dyads. A strength of this study is that it examined the interactive effects of partner’s attachment orientations on both partners psychological health in a sample of older adults. Second, this study examined how attachment related to relational dynamics in a specific health-related context. Very little research has used attachment theory to understand how couples cope with one person having chronic pain (Monin & Schulz, 2010). Third, both individual and relational aspects of psychological health were considered. No research to our knowledge has examined how attachment relates to marital satisfaction in the context of couples coping with chronic pain conditions despite that there is a substantial literature on marital satisfaction and pain.
The findings of this study should be interpreted with the following limitations in mind. First, we did not have ratings of attachment and psychological health prior to the support manipulation. Thus, in examining how the support manipulation related to attachment and psychological health, we can only examine associations rather than establish causal effects in terms of change in these variables. In a similar vein we cannot determine whether we were tapping more stable or momentary aspects of a person’s attachment orientation. That being said, because we used the ECR (instead of other state measures; Gillath, Hart, Noftle, & Stockdale, 2009), it is likely that we were capturing more stable attachment orientations (Xu & Shrout, 2013). Also, because we assessed attachment only after the experimental manipulation, one could argue that our main findings concerning the associations between attachment and psychological health are less generalizable. That said, we did control for experimental conditions in the dyadic analysis, and findings were robust regardless of whether they engaged in a support interaction or not. The self-report measures were also given about 30 minutes after the experiment. In addition, we explicitly tested differences by experimental condition to help provide a more accurate picture about how attachment orientations relate to well-being in a particular social context. We did not find that attachment was associated with psychological health depending on the experimental condition. However, this may be due to the fact that our sample size was small, and there was not adequate power to detect significant interaction effects. This may have also been why we did not find significant interactions with gender predicting psychological health. Finally, because we tested multiple models, there is an increased chance of incidental findings.
Our findings should be considered preliminary evidence for the dyadic effects of attachment on older couples’ psychological health in the face of chronic health stressors. It will be important for future research to examine the causal mechanisms through which each partner’s attachment influences each partner’s psychological health in real-time support interactions. For example, an ideal study would be to simulate a support interaction in the laboratory, manipulate older couples’ attachment security, and examine each partner’s perceptions of distress, support, and psychological health directly before, during, and after the support interaction. Focusing on an actual encounter in real time may reveal richer information about how attachment insecurity hinders the support-seeking and caregiving processes for older couples coping with pain. This type of design would also allow for both observational and self-report measures of support-seeking and caregiving behavior.
Implications
Findings from this study have implications for dyadic interventions for older adults coping with chronic conditions that cause pain. For example, issues of attachment should be paid particular attention in marital therapy, such as assessing insecurity and helping to change negative attachment models of partners (Shi, 2003). Such marital therapy may be an effective treatment for depression especially when there is marital distress (Whiffen, 2001). Also, taking an attachment theoretical perspective can help health care providers establish counseling for insecurely attached couples, who are less likely to seek social support than securely attached couples (Karantzas et al., 2010). One of the empirically based interventions is EFT (Emotionally Focused Couple Therapy), which is suggested to be helpful in enhancing marital satisfaction for older couples coping with a chronic condition (Monin et al., 2012; Johnson, 2003). More specifically, findings from this study suggest that couples in which one or both partners are insecurely attached may particularly benefit from support interventions. It may be that avoidant individuals are lacking the necessary skills to adequately provide support and that anxiously attached individuals are particularly demanding when seeking support. Identifying these couples early may decrease risk for poor psychological outcomes down the road.
Acknowledgments
This study was funded in part by a Research Career Development Award from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (NIA P30AG21342) and a K01 career development award from the NIA (K01 AG042450-01A1) to Dr. Monin.
Footnotes
Three of the spouses indicated at the lab session that they had osteoarthritis or lower back pain. Excluding them from analysis did not change the results.
Declaration of Conflicts of Interest
The authors declare that no conflicts of interest exist.
References
- Andersen TE. Does attachment insecurity affect the outcomes of a multidisciplinary pain management program? The association between attachment insecurity, pain, disability, distress, and the use of opioids. Social Science & Medicine. 2012;74:1461–1468. doi: 10.1016/j.socscimed.2012.01.009. [DOI] [PubMed] [Google Scholar]
- Badr H, Laurenceau J, Schart L, Basen-Engquist K, Turk D. The daily impact of pain from metastatic breast cancer on spousal relationships: A dyadic electronic diary study. Pain. 2010;151:644–54. doi: 10.1016/j.pain.2010.08.022. [DOI] [PubMed] [Google Scholar]
- Baldwin MW, Keelan JPR, Fehr B, Enns V, Koh-Rangarajoo E. Social cognitive conceptualization of attachment styles: Availability and accessibility effects. Journal of Personality and Social Psychology. 1996;71:94–109. [Google Scholar]
- Bowlby J. Attachment and loss, Volume I: Attachment. New York: Basic Books; 1969. [Google Scholar]
- Bradley MJ, Cafferty TP. Attachment among older adults: Current issues and directions for future research. Attachment & human development. 2001;3:200–221. doi: 10.1080/14616730126485. [DOI] [PubMed] [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: an integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. New York: Guilford; 1998. pp. 46–76. [Google Scholar]
- Carstensen LL, Gottman JM, Levenson RW. Emotional behavior in long-term marriage. Psychology and Aging. 1995;10:140–149. doi: 10.1037//0882-7974.10.1.140. [DOI] [PubMed] [Google Scholar]
- Cassidy J. Adult romantic attachments: A developmental perspective on individual differences. Review of General Psychology. 2000;4:111–131. [Google Scholar]
- Cassidy J, Kobak RR. Avoidance and its relation to other defensive processes. In: Belsky J, Nezworski T, editors. Clinical implications of attachment. Hillsdale, NJ: Erlbaum; 1988. pp. 300–323. [Google Scholar]
- Ciechanowski P, Sullivan M, Jensen M, Romano J, Summers H. The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain. 2003;104:627–637. doi: 10.1016/S0304-3959(03)00120-9. [DOI] [PubMed] [Google Scholar]
- Collins NL, Feeney BC. A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. Journal of Personality and Social Psychology. 2000;78:1053–1073. doi: 10.1037//0022-3514.78.6.1053. [DOI] [PubMed] [Google Scholar]
- Collins NL, Feeney BC. Working models of attachment shape perceptions of social support: evidence from experimental and observational studies. Journal of Personality and Social Psychology. 2004;87:363–383. doi: 10.1037/0022-3514.87.3.363. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Fiori KL, Tuck NL, Merz EM. Attachment, activity limitation, and health symptoms in later life: The mediating roles of negative (and positive) affect. Journal of Aging and Health. 2013;25:56–79. doi: 10.1177/0898264312466260. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Magai C. Attachment and emotion experience in later life: The view from emotions theory. Attachment & Human Development. 2003;5:165–187. doi: 10.1080/1461673031000108496. [DOI] [PubMed] [Google Scholar]
- Feeney BC. A secure base: Responsive support of goal strivings and exploration in adult intimate relationships. Journal of Personality and Social Psychology. 2004;87:631–648. doi: 10.1037/0022-3514.87.5.631. [DOI] [PubMed] [Google Scholar]
- Feeney BC. The dependency paradox in close relationships: Accepting dependence promotes independence. Journal of Personality and Social Psychology. 2007;92:268–285. doi: 10.1037/0022-3514.92.2.268. [DOI] [PubMed] [Google Scholar]
- Feeney BC, Collins N. Predictors of caregiving in adult intimate relationships: An attachment theoretical perspective. Journal of Personality and Social Psychology. 2001;80:972–994. [PubMed] [Google Scholar]
- Feeney JA. Attachment style, communication patterns, and satisfaction across the life cycle of marriage. Personal Relationships. 1994;1:333–348. [Google Scholar]
- Fraley RC. Information on the Experiences in Close Relationships – Revised (ECR-R) Adult Attachment Questionnaire. 2012 Retrieved from http://internal.psychology.illi-nois.edu/~rcfraley/measures/ecrr.htm.
- Gillath O, Hart J, Noftle EE, Stockdale GD. Development and validation of a state adult attachment measure (SAAM) Journal of Research in Personality. 2009;43:362–373. [Google Scholar]
- Hawker GA, Gignac MA, Badley E, Davis AM, French MR, Li Y, Lou W. A longitudinal study to explain the pain-depression link in older adults with osteoar-thritis. Arthritis Care & Research. 2011;63:1382–1390. doi: 10.1002/acr.20298. [DOI] [PubMed] [Google Scholar]
- Johnson SM. Emotionally focused couples therapy: Empiricism and art. In: Sexton TL, Weeks GR, Robbins MS, editors. Handbook of family therapy: The science and practice of working with families and couples. New York: Brunner-Routledge; 2003. pp. 263–280. [Google Scholar]
- Kafetsios K, Sideridis GD. Attachment, social support and well-being in young and older adults. Journal of Health Psychology. 2006;11:863–875. doi: 10.1177/1359105306069084. [DOI] [PubMed] [Google Scholar]
- Kane HS, Jaremka LM, Guichard AC, Ford MB, Collins NL, Feeney BC. Feeling supported and feeling satisfied: How one partner’s attachment style predicts the other partner’s relationship experiences. Journal of Social and Personal Relationships. 2007;24:535–555. [Google Scholar]
- Karantzas GC, Cole SF. Arthritis and support seeking tendencies: The role of attachment. Journal of Social and Clinical Psychology. 2011;30:404–440. [Google Scholar]
- Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford; 2006. [Google Scholar]
- Laganà L, Hassija CM. Bodily pain and coping styles among four geriatric age groups of women. Journal of Health Psychology. 2012;17:545–555. doi: 10.1177/1359105311421045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke HJ, Wallace KM. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage & Family Living. 1959;21:251–255. [Google Scholar]
- Lopez FG, Mauricio AM, Gormley B, Simko T, Berger E. Adult attachment orientations and college student distress: The mediating role of problem coping styles. Journal of Counseling & Development. 2001;79:459–464. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, Starz TW. Older spouses’ perceptions of partners’ chronic arthritis pain: implications for spousal responses, support provision, and caregiving experiences. Psychology and Aging. 2006;21:222–230. doi: 10.1037/0882-7974.21.2.222. [DOI] [PubMed] [Google Scholar]
- Masedo AI, Esteve RM. Effects of suppression, acceptance and spontaneous coping on pain tolerance, pain intensity and distress. Behavior Research and Therapy. 2007;45:199–209. doi: 10.1016/j.brat.2006.02.006. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Asmundson GJ. The relationship of adult attachment dimensions to pain-related fear, hypervigilance, and catastrophizing. Pain. 2007;127:27–34. doi: 10.1016/j.pain.2006.07.020. [DOI] [PubMed] [Google Scholar]
- McWilliams L, Holmberg D. Adult attachment and pain catastrophizing for self and significant other. Pain. 2010;149:278–283. doi: 10.1016/j.pain.2010.02.019. [DOI] [PubMed] [Google Scholar]
- Meredith PJ, Strong J, Feeney JA. Adult attachment variables predict depression before and after treatment for chronic pain. European Journal of Pain. 2007;11:164–170. doi: 10.1016/j.ejpain.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Meredith P, Ownsworth T, Strong J. A review of the evidence linking adult attachment theory and chronic pain: Presenting a conceptual model. Clinical psychology review. 2008;28:407–429. doi: 10.1016/j.cpr.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Merz EM, Consedine NS. The association of family support and well-being in later life depends on adult attachment style. Attachment & human development. 2009;11:203–221. doi: 10.1080/14616730802625185. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Gillath O, Halevy V, Avihou N, Avidan S, Eshkoli N. Attachment theory and reactions to others’ needs: Evidence that activation of the sense of attachment security promotes empathic responses. Journal of personality and social psychology. 2001;81:1205–1224. [PubMed] [Google Scholar]
- Mikulincer M, Florian V. The relationship between adult attachment styles and emotional and cognitive reactions to stressful events. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. New York: Guilford; 1998. pp. 143–165. [Google Scholar]
- Mikulincer M, Shaver PR, Pereg D. Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment-related strategies. Motivation and Emotion. 2003;27:77–102. [Google Scholar]
- Monin JK, Feeney BC, Schulz R. Attachment orientation and reactions to anxiety expression in close relationships. Personal Relationships. 2012;19:535–550. [Google Scholar]
- Monin JK, Martire LM, Schulz R, Clark MS. Willingness to express emotions to caregiving spouses. Emotion. 2009;9:101–106. doi: 10.1037/a0013732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging. 2009;24:681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R. The effects of suffering in chronically ill older adults on the health and well-being of family members involved in their care: The role of emotion-related processes. GeroPsych. 2010;23:207–213. doi: 10.1024/1662-9647/a000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Feeney BC, Cook TB. Attachment insecurity and perceived partner suffering as predictors of personal distress. Journal of Experimental Social Psychology. 2010;46:1143–1147. doi: 10.1016/j.jesp.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, Greenberg MS. Spouses’ cardiovascular reactivity to their partners’ suffering. Journals of Gerontology: Psychological Sciences. 2010;65B:195–201. doi: 10.1093/geronb/gbp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Kershaw TS. Caregiving spouses’ attachment orientations and the physical and psychological health of individuals with Alzheimer’s disease. Aging & Mental Health. 2013;17:508–516. doi: 10.1080/13607863.2012.747080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsen K, Monsen JT, Svartberg M, Havik OE. Chronic pain patients: Patterns of change in interpersonal problems, pain intensity, and depression-anxiety. Psychotherapy Research. 2002;12:339–354. [Google Scholar]
- NIAMS. What is osteoarthritis? Fast facts: An easy-to-read series of publications for the public. 2010 Retrieved from http://www.niams.nih.gov/health_info/Osteoarthritis/osteoarthritis_ff.asp.
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Davis D, Rumble M, Scipio C, Garst J. Attachment styles in patients with lung cancer and their spouses: associations with patient and spouse adjustment. Supportive Care in Cancer. 2012;20:2459–2466. doi: 10.1007/s00520-011-1367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Romano JM, Turner JA, Jensen MP, Friedman LS, Bul-croft RA, Hops H, Wright SF. Chronic pain patient-spouse behavioral interactions predict patient disability. Pain. 1995;63:353–360. doi: 10.1016/0304-3959(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Sadava SW, Busseri MA, Molnar DS, Perrier CPK, DeCourville N. Investigating a four-pathway model of adult attachment orientation and health. Journal of Social and Personal Relationships. 2009;26:604–633. [Google Scholar]
- Schwartz L, Slater MA, Birchler GR, Atkinson JH. Depression in spouses of chronic pain patients: the role of patient pain and anger, and marital satisfaction. Pain. 1991;44:61–67. doi: 10.1016/0304-3959(91)90148-Q. [DOI] [PubMed] [Google Scholar]
- Shi L. The association between adult attachment styles and conflict resolution in romantic relationships. American Journal of Family Therapy. 2003;31:143–157. [Google Scholar]
- Shields CG, Travis LA, Rousseau SL. Marital attachment and adjustment in older couples coping with cancer. Aging & Mental Health. 2000;4:223–233. [Google Scholar]
- Solomon J, George C. Defining the caregiving system: Toward a theory of caregiving. Infant Mental Health Journal. 1996;17:183–197. [Google Scholar]
- Wei M, Vogel DL, Ku T, Zakalik RA. Adult attachment, affect regulation, negative mood, and interpersonal problems, the mediating roles of emotional reactivity and emotional cutoff. Journal of Counseling Psychology. 2005;52:14–24. [Google Scholar]
- Wensauer M, Grossman KE. Quality of attachment representations, social integration, and use of network resources in old age. Zeitschrift für Gerontologie und Geriatrie. 1995;28:444–456. [PubMed] [Google Scholar]
- Whiffen EV, Kallos-Lilly VA, MacDonald JB. Depression and Attachment in Couples. Cognitive Therapy and Research. 2001;25:577–590. [Google Scholar]
- Wilson CL, Ruben MA. A pain in her arm: Romantic attachment orientations and the tourniquet task. Personal Relationships. 2011;18:242–265. [Google Scholar]
- Xu JH, Shrout PE. Assessing the reliability of change: A comparison of two measures of adult attachment. Journal of Research in Personality. 2013;47:202–208. [Google Scholar]