Abstract
Introduction
Arthroplasty is commonplace in orthopaedic practice, and post operative pain has been shown to substantially hinder recovery and discharge from hospital.
Objectives
The current study assessed a multidisciplinary, multimodal Orthopaedic ERP in terms of its effect on patient perceived post operative pain in hip and knee arthroplasty. Secondary outcome was in the form of a cost analysis.
Methods
A prospective study was performed on consecutive arthroplasty patients across a 6 week period in a district orthopaedic unit. A multidisciplinary approach to devising an ERP was undertaken between anaesthetists, surgeons and physiotherapists. Domains included optimising pre-operative nutrition, anaesthetic pre-meds, standardised anaesthetic technique, standardised intra-operative technique and use of locally infiltrated anaesthetic (LIA), as well as a post operative pain regimen. The multidisciplinary team (MDT) involved physiotherapy for the patient on day 0. Demographic data, day 1 and day 2 post operative subjective pain scores using an analogue scale were recorded. Data was collated and analysed using appropriate statistical methods. A p-value of <0.05 was considered significant.
Results
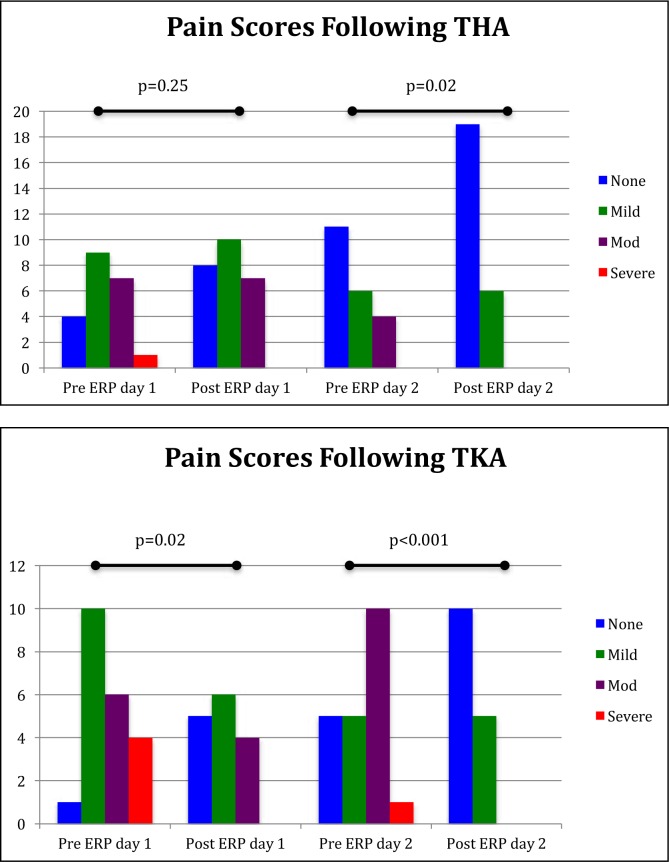
A total of 40 patients (25 total hip replacements and 15 total knee replacements) were included. All conformed to the ERP. Reductions in patient reported pain scores were observed. Specifically, in total hip arthroplasty (THA), day 1 scores were not significantly improved (p=0.25), however day 2 scores improved significantly (p=0.02). For total knee arthroplasty (TKA), both day 1 and day 2 scores improved significantly (p=0.02 & p<0.001, respectively) Analgesic requirements were not significantly different between hip and knee replacements. Early mobilization occurred in 95% of patients. Length of stay was reduced significantly in hip (1.8 days, p=0.003) and knee (1.9 days(p<0.001) replacements following ERP. Cost analysis demonstrated a potential annual saving of approximately £200,000 for the study unit if ERP was applied to all elective hip and knee arthroplasty procedures.
Conclusions
The study demonstrates that a tailored, MDT orientated ERP can be beneficial in elective hip and knee arthroplasty. Reductions in pain scores, early ambulation and facilitated early discharge are beneficial to the patient, and cost effective for the unit. The implementation across the region may result in further cost savings.
Keywords: Arthroplasty, Hip, Knee, Enhanced Recovery Protocol
INTRODUCTION
Orthopaedic arthroplasty procedures are amongst the most painful operations reported by patients, with over 40% noting moderate to severe pain in the initial 48 hour post-opeative period. 1 This can substantially hinder recovery and delay discharge from hospital, incurring potentially avoidable costs.2 A Danish study identified multiple factors that impact upon length of stay following hip and knee arthroplasty.3 Post-operative pain management was a key issue. The concept of enhanced recovery protocols (ERPs) have been successfully applied in general surgical practice, especially in colorectal surgery.4 Literature regarding the use of similar protocols in orthopaedic practice have demonstrated pain reduction through the use of locally infiltrated anaesthetic (LIA) to the surgical area in hip and knee arthroplasty.5–7 Similarly, other studies have demonstrated significant analgesic benefits and reduced length of stay following the use of LIA in hip arthroplasty. 8–10
It is well recognized that the use of intrathecal diamorphine is associated with significant postoperative nausea and vomiting, and it is felt that the use of LIA can avoid this undesirable side affect.11 We describe how a local perioperative enhanced recovery protocol (ERP) for total hip (THA) and total knee (TKA) arthroplasty has produced significant clinical, and cost benefits, in a DGH unit, that may be applicable to a larger regional scale.
PATIENTS AND METHODS
Hospital management and the acute pain team were able to provide data regarding the length of stay and pain scores postoperatively on day 1 and 2, prior to the introduction of ERP. The average lengths of stay for both total hip arthroplasty (THA), and total knee arthroplasty (TKA), were 6.3 and 6.1 days respectively in keeping with national length of stay.12 Following the apparent success of ERPs across the published literature 5–10, a tailored ERP for the unit was devised using a multidisciplinary team (MDT) approach.
A prospective, consecutive cohort of patients admitted for primary elective total hip or total knee arthroplasty were recruited over a 6 week period. An established multidisciplinary perioperative ERP, detailed in Table 1, was followed for each patient. All patients received carbohydrate drinks pre-operatively in order to achieve optimal nutritional status and reduce preoperative fasting times. This included 4 Nutricia PreOp© (Nutricia, UK) drinks the night before surgery. For afternoon cases, a further 2 drinks could be taken the morning of surgery. An oral analgesic pre-med was given to all patients 2 hours prior to surgery. This consisted of 1g Paracetamol, 10mg Oxycontin M/R (Longtec®, reduced to 5mg for age>75 years of age), and either 300mg Gabapentin or 100mg if >75 years of age.
TABLE 1.
Aspects of the multimodal enhanced recovery programme utilized by department
| Preoperative | Intraoperative | Postoperative |
|---|---|---|
| Carbohydrate drinks | Spinal anaesthetic | Early oral hydration |
| Continue regular analgesia | Capsular LIA by operating surgeon | Thromboprophylaxis |
| Analgesic Premed on day of surgery(paracetamol 1g/Longtec 10mg§/Gabapentin 300mg*) | No urinary catheter | Physiotherapy on day of surgery to mobilise |
| Preoperative warming | Tranexamic acid 1g | Regular oral analgesia |
Longtec dose reduced to 5mg for patients aged >75 years
Gabapentin dose reduced to 100mg for patients aged >75 years
The use of urinary catheters was restricted to patients deemed by the anaesthetic team to be at risk for acute kidney injury or postoperative urinary retention.
At the time of surgery, a spinal anaesthetic (3ml 0.5% Chirocaine for THA or 2.3-2.5mls heavy Marcaine with 0.1-0.2mg morphine for TKA) was administered to patients. In the cases of failed spinal, a general anesthetic using Propofol with IV morphine was provided.
All TKA procedures were performed under the use of an electronic, calibrated lower limb tourniquet at a pressure of 300mmHg.
A dose of 1g Tranexamic acid was provided to all patients at the time of skin incision in THA, or 30 minutes before release of the tourniquet in TKA (unless contra-indicated).
Intraoperative LIA was administered by the surgical team at the time of surgery in all patients. This consisted of three 50ml boluses of 0.2% Ropivicaine. Two of these syringes had an added 0.25mls of 1:1000 adrenaline added. The third bolus consisted of Ropivicaine only.
For THA, one bolus of ropivicaine with adrenaline was administered to the hip short rotators and capsule. The second bolus of LIA was injected around the ilio-tibial band. The bolus of plain ropivicaine was administered subcutaneously at the time of skin closure.
For TKA, the adrenaline infused boluses were administered firstly to the posterior capsule after the femoral and tibial cuts were performed. The second adrenaline infused LIA was administered to the anterior capsule, collateral ligaments and quadriceps muscle anteriorly after insertion of the TKA components. Again, the ropivicaine only bolus was administered subcutaneously at the time of skin closure.
Post operatively, on days 0-2, all patients received regular paracetamol 1g IV QDS for 24 hours before reducing to oral paracetamol 1g QDS. IV Parecoxib was administered for the initial 48 hours post operatively if no contra-indications were present. In addition to this, regular Oxycontin® (Longtec) 10-15mg PO BD (5mg BD if >75 years) and Gabapentin 300mg PO BD (100mg if >75 years) was provided. Additional breakthrough analgesia in the form of Oxynorm® 5-10mg PO 2-4 hourly was provided on a PRN basis. On day 3 post operatively, patient analgesia was stepped down to Cocodamol 15/500, with two tablets administered QDS, and Oxynorm® 5-10mg PRN breakthrough analgesia available as above.
Post operative mobilisation was recorded by the physiotherapists as part of the multidisciplinary approach to the multimodal ERP. All morning cases were mobilised early; were to at least stand on day of surgery, while all afternoon cases being mobilised on the morning of day 1 postoperatively.
Post operatively, oral fluids were provided in the recovery room to ensure early oral rehydration. Routine thromboprophylaxis was provided to all patients in accordance with NICE guidelines.
Primary aims were to study:
Effect of ERP on length of hospital stay
Post operative pain scores (recorded as none, mild, moderate, severe)
Secondary aim of the study was a cost analysis following ERP implementation to assess its financial feasibility.
Statistical analysis was performed using two way ANOVA for non parametric data, and independent samples T-testing where appropriate, using SPSS V21. A p value <0.05 was considered statistically significant.
RESULTS
A total of 40 consecutive primary arthroplasty patients were recruited to the study, 25 THA and 15 TKA surgeries. Patient demographics are demonstrated in Table 2. All patients conformed to the ERP protocol.
TABLE 2.
Patient demographics
| THR | TKR | |
|---|---|---|
| N | 25 | 15 |
| Female : male | 14:11 | 9:6 |
| Average age in years (SD) | 66 (15.9) | 76 (6.1) |
| Age Range | 30-89 | 62-89 |
| ASA Grade | ||
| 1 | 4 | 2 |
| 2 | 13 | 8 |
| 3 | 8 | 4 |
| 4 | 0 | 0 |
Spinal anaesthetic was successfully performed in all cases except for 2 patients undergoing TKRs, who received a general anaesthetic, one due to patient preference and the other following failed spinal.
Tranexamic acid was withheld in 3 patients (7.5%), all of whom had a contraindication precluding its use.
LIA was administered in each of the cases as outlined in the method above. No adverse events as a result of the Ropivicaine with or without adrenaline was noted intraoperatively, or postoperatively.
Postoperative
Postoperative pain scores were assessed on days one and two post operatively by the pain team. Following THA, day 1 pain scores were not significantly different pre and post introduction of the ERP (p=0.25). However, day 2 scores were significantly improved (p=0.02). For TKA, both day 1 and day 2 post operative scores improved with the implementation of the ERP (p=0.02 and p<0.001 respectively). Table 3 and Figure 1 summarise the pain score data.
TABLE 3.
Patient reported pain scores on Days 1 and 2 postoperatively after THA and TKA before and after the introduction of the ERP
| Patient Reported Pain Score | |||||
|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | p Value | |
| THA | |||||
| Day 1 | |||||
| Pre ERP (n=21) | 4 | 9 | 7 | 1 | 0.25 |
| Post ERP (n=25) | 8 | 10 | 7 | 0 | |
| Day 2 | |||||
| Pre ERP (n=21) | 11 | 6 | 4 | 0 | 0.02 |
| Post ERP (n=25) | 19 | 6 | 0 | 0 | |
| TKA | |||||
| Day 1 | |||||
| Pre ERP (n=21) | 1 | 10 | 6 | 4 | 0.02 |
| Post ERP (n=15) | 5 | 6 | 4 | 0 | |
| Day 2 | |||||
| Pre ERP (n=21) | 5 | 5 | 10 | 1 | <0.001 |
| Post ERP (n=15) | 10 | 5 | 0 | 0 | |
Fig 1a and b.
Trends in postoperative patient reported pain scores on days 1 and 2 following TKA and THA
Post-operative analgesic requirements were analysed by oxycodone requirements in the forms of Oxycontin and Oxynorm. Average Oxycontin requirements for THA and TKA were not statistically significant (Oxycontin: 60.8±45.4mg Vs 58.7±23.9mg; p=0.21, Oxynorm: 48.4±55.3mg Vs 68.7±47.0mg; p=0.74 respectively).
Early mobilisation on day of surgery occurred in 100% of morning cases. None of the PM cases returned to the ward early enough to receive physiotherapy input within normal working hours. On day 1 postoperatively 38/40 (95%) of patients were mobilised (one was hypotensive and unsuitable for mobilization, one was a planned admission to ICU for 24 hours post operatively). On day 2 postoperatively, all patients had been mobilised with physiotherapy input.
Length of stay and cost analysis
Pre-ERP length of stay for THA and TKA was 6.3 and 6.1 days respectively. Our multimodal approach resulted in a statistically significant reduced length of stay following THA to 4.5 days (p=0.003) and following TKA to 4.2 days (p<0.001).
A cost analysis was undertaken looking at novel aspects of the ERP. All other costs such as regular analgesia, cost of daily nursing etc were assumed to be part of standard care in order to specifically look at the ERP intervention. Urinary catheters were used in approximately 20% of the study population. The ERP aims to reduce unnecessary catheterization if possible, and so this figure was used for the purposes of a cost analysis. Pharmaceutical costings were obtained from the hospital pharmacy department regarding the cost per patient of LIA versus previous practice of intrathecal diamorphine. Average spend on Oxycodone per patient for THA and TKA was calculated from the study data and extrapolated. Similarly reference costs for the cost of a bed day per patient were taken from the Department of Health Reference Costs manuscript. Table 4 outlines the cost analysis calculation based on the study results for a single year based on our annual unit throughput. Overall, we calculated a potential saving of £203,524.80 per annum based on current unit throughput.
TABLE 4.
Breakdown of costs analysis for study unit ERP. Parameters such as nursing care and regular analgesia which are considered “standard” for inpatient arthroplasty were not considered as these are necessary costs regardless of the use of ERP
| Unit price | Cases Annually | Comments | Cost Per Annum | |
|---|---|---|---|---|
| Savings | ||||
| Catheter | £20 | 480 | 20% incidence | £1,920.00 |
| Reduction Length of Stay | £264/Day | 300 hips | mean -1.8 days | |
| 180 knee | mean -1.9 days | |||
| Total bed days | 882 bed days p/a | £232,848.00 | ||
| Costs | ||||
| LIA added cost | £61.15 | 480 | All cases | £29,352.00 |
| Postop analgesia | ||||
| Hip | £3.70 | 300 | £1,110.00 | |
| Knee | £4.34 | 180 | £781.20 | |
| Average total p/a | £1,891.20 | |||
| Overall cost analysis net saving per annum | £203,524.80 | |||
DISCUSSION
ERP's core principles are to improve patient outcomes and speed up recovery following surgery. It focuses on optimising multiple aspects of patient care, and promotes active participation from the patient in order to fast-track recovery.
ERP has successfully been utilized in colorectal surgery and has been extensively reported in the literature.4 This has spawned interest in its possible adaptation and application for THA and TKA with a view to reducing pain, improving patient outcomes and shortening inpatient stay.13
Husted et al demonstrated that logistical and clinical aspects could be addressed in individual units with shorter length of stay, better patient satisfaction and thus recommended an introduction of ERPs at a national lavel.3 A paucity of data exists for ERPs in orthopaedics as a whole, but recent studies have shown multiple benefits and a reduced mortality rate following the introduction of ERPs for lower limb arthroplasty.14, 15
One of the key variables in lower limb arthroplasty is patient reported pain postoperatively, with over 40% of patients reporting moderate to severe pain in the first 48 hours.1 Pain spikes have been reported following upper and lower limb arthroplasty, with subsequent prolongation of inpatient stay. We did not observe any spikes in pain perception in our population however.16, 17 Reduced patient reported pain and analgesia use, with subsequent improvement in patient mobilisation and reduced length of hospital stay, have been reported for patients receiving intraoperative injections of local anaesthetic as part of an ERP utilizing multimodal analgesic techniques. Whilst the exact LIA preparation varies between individual studies, it has consistently shown improvements, especially for TKA.6, 18–21
Our study, whilst it utilizes individually tailored ERP design, has demonstrated a similar trend reported throughout the literature with regards to THA and TKA.14–24 We have shown a significant reduction in pain scores in the immediate 48 hours after THA and TKA which is in keeping with other ERP designs.
We report significant cost savings associated with reduced length of stay by using ERP in our trust. To our knowledge, we are the only unit in the region to be utilizing an established ERP for THA and TKA. We have reported significant benefits for both patients and the unit, which are applicable on a regional scale. If ERPs were widely adopted, additional regional savings could be made.
A major limitation of our study is the relatively small sample size compared with other studies. Despite this, we have shown a significant reduction in our unit length of stay even at this small scale, as well as significant patient reported benefits through streamlining our management for primary THA and TKA using a multidisciplinary ERP. We also admit that variability in individual ERP designs limit the ability to assess where the exact benefits in terms of improved pain scores and reduced length of stay actually result from. A follow up telephone survey may have clarified if post-operative pain management remains effective after the inpatient perioperative stay. It is however clear that a multidisciplinary approach to an ERP does result in significant improvements in patient care, and convey significant potential annual savings for hospital trusts.
Despite the limitations, we have shown a potential saving of approximately £200,000 in a single unit utilizing our ERP methodology. In Northern Ireland in 2013, a total of 2404 primary THA and 1806 primary TKAs were performed. No other arthroplasty units currently utilise an ERP programme. Extrapolation of our figures to the 2013 data equates to a net saving of approx £1,750,000 per annum. This conveys a significant cost saving during times of financial austerity in an area of practice whose burden on NHS resources will continue to increase
CONCLUSION
Successful ERP programmes have been reported in the literature for both THA and TKA, despite variability amongst individual unit ERP designs. ERP is an effective means of reducing pain, reducing length of inpatient hospital stay and reducing costs associated with THA and TKA, as demonstrated in our study. Whilst the principles of ERP are not new, adoption in orthopaedics has been slow, but with over 160,000 THA and TKA procedures per annum in England and Wales alone25 the application of ERPs could have huge potential savings for the NHS if adopted on a larger, regional or national scale.
REFERENCES
- 1.Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Surgery of postoperative analgesia following ambulatory surgery. Acta Anaesthesiol Scand. 1997;41(8):1017–22. doi: 10.1111/j.1399-6576.1997.tb04829.x. [DOI] [PubMed] [Google Scholar]
- 2.Dahl JB, Moiniche S. Relief of postoperative pain by local anesthetic infiltration: efficacy for major abdominal and orthopedic surgery. Pain. 2009;143(1-2):7–11. doi: 10.1016/j.pain.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 3.Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, et al. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg. 2010;130(2):263–8. doi: 10.1007/s00402-009-0940-7. [DOI] [PubMed] [Google Scholar]
- 4.Lassen K, Soop M, Nygren J, Cox PB, Hendry PO. Consensus review of optimal care in colorectal surgery. Enhanced recovery after surgery. (ERAS) Group recommendation. Arch Surg. 2009;144(10):961–9. doi: 10.1001/archsurg.2009.170. [DOI] [PubMed] [Google Scholar]
- 5.Busch C, Shore B, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006;88(5):959–63. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
- 6.Vendittoli P, Makinen P, Drolet P, Lavigne M, Fallaha M, Guestin MC, et al. A multimodal analgesia protocol for total knee arthroplasty. A randomized control study. J Bone Joint Surg Am. 2006;88(2):282–9. doi: 10.2106/JBJS.E.00173. [DOI] [PubMed] [Google Scholar]
- 7.Reilly KA, Beard DJ, Barker KL, Dodd CA, Price AJ, Murray DW. Efficacy of accelerated recovery protocol for Oxford unicompartmental knee arthroplasty - a randomised controlled trial. Knee. 2005;12(5):351–7. doi: 10.1016/j.knee.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Andersen KV, Peiffer-Jensen M, Haraldsted V, Soballe K. Reduced hospital stay and narcotic comsumption, and improved mobilization with local and intraarticular infiltration after hip arhtroplasty. A randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop. 2007;78(2):180–6. doi: 10.1080/17453670710013654. [DOI] [PubMed] [Google Scholar]
- 9.Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty. A randomized, double blinded, placebo controlled study on peroperative and postoperative ropivicaine, ketorolac and adrenaline wound infiltration. Acta Orthop. 2007;78(2):187–92. doi: 10.1080/17453670710013663. [DOI] [PubMed] [Google Scholar]
- 10.Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of postoperative pain following knee and hip surgery. Acta Orthop. 2008;79(2):174–83. doi: 10.1080/17453670710014950. [DOI] [PubMed] [Google Scholar]
- 11.Grant CR, Checketts MR. Analgesia for primary hip and knee arthroplasty: the role of regional anaesthesia. Contin Educ Anaesth Crit Care Pain. 2008;8(2):56–61. [Google Scholar]
- 12.Hospital Episodes Statistics. Admitted patient care, England, 2014-15. Table 6: Procedures and diagnoses. Leeds: Health and Social Care Information Centre [HSCIC] 2015. Available at http://www.hscic.gov.uk/catalogue/PUB19124/hosp-epis-stat-admi-summ-rep-2014-15-rep.pdf.
- 13.Wainwright T, Middleton R. An orthopaedic enhanced recovery pathway. Curr Anaesth Crit Care. 2010;21(3):114–20. [Google Scholar]
- 14.Malviya A, Martin K, Harper I, Muller SD, Emmerson KP, Partington PF, et al. Enhanced recovery program for hip and knee replacement reduces death rate: A study of 4,500 consecutive primary hip and knee replacements. Acta Orthop. 2011;82(5):577–81. doi: 10.3109/17453674.2011.618911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDonald DA, Siegmeth R, Deakin AH, Kinninmonth AW, Scott NB. An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom – follow up at one year. Knee. 2012;19(5):525–9. doi: 10.1016/j.knee.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Ilfeld BM, Mariano ER, Girard PJ, Loland VJ, Meyer RS, Donoan JF, et al. A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards. Pain. 2010;150(3):477–84. doi: 10.1016/j.pain.2010.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilfeld BM, Vanderborne K, Duncan PW, Sessler DI, Enneking FK, Shuster JJ, et al. Ambulatory continuous interscalene nerve blocks decrease the time to discharge-readiness after total shoulder arthroplasty: a randomized, triple-masked, placebo-controlled study. Anesthesiol. 2006;105(5):999–1007. doi: 10.1097/00000542-200611000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Anderson LO, Husted H, Otte KS, Kristensen BB, Kehlet H. High volume infiltration analgesia in total knee arthroplasty: a randomized, double-blind, placebo controlled trial. Acta Anaesthesiol Scand. 2008;52(10):1331–5. doi: 10.1111/j.1399-6576.2008.01777.x. [DOI] [PubMed] [Google Scholar]
- 19.Bianconi M, Ferraro L, Traina GC, Zanoli G, Antonelli T, Gubert A, et al. Pharmacokinetics and efficacy of ropivicaine continuous wound instillation after joint replacement surgery. Br J Anaesth. 2003;91(6):830–5. doi: 10.1093/bja/aeg277. [DOI] [PubMed] [Google Scholar]
- 20.Essving P, Axelsson K, Kjellberg J, Wallgren D, Gupta A, Lundin A, et al. Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty. Acta Orthop. 2010;81(3):354–60. doi: 10.3109/17453674.2010.487241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toftdahl K, Nikolajsen L, Haraldsted V, Madsen F, Tonnesen LK, Soballe K. Comparison of peri- and intra-articular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. Acta Orthop. 2007;78(2):172–9. doi: 10.1080/17453670710013645. [DOI] [PubMed] [Google Scholar]
- 22.Busch CA, Whitehouse MR, Shore BJ, MadDonald SJ, McCalder RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res. 2010;468(8):2152–9. doi: 10.1007/s11999-009-1198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007;22(6 Suppl 2):33–8. doi: 10.1016/j.arth.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 24.Lee KJ, Min BW, Bae KC, Cho Ch, Kwon DH. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg. 2009;1(3):155–60. doi: 10.4055/cios.2009.1.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Joint Registry. Patients. Joint replacement statistics. Hemel Hempsted, UK: Healthcare Quality Improvement Partnership; 2015. Available from: http://www.njrcentre.org.uk/njrcentre/Patients/Jointreplacementstatistics/tabid/99/Default.aspx. Last accessed Feb 2016. [Google Scholar]