Abstract
Background: Patient-reported outcome measures (PROMs) are important tools for assessing outcomes following injuries to the hand and wrist. Many commonly used PROMs have no evidence of reliability, validity, and responsiveness in a hand and wrist trauma population. This systematic review examines the PROMs used in the assessment of hand and wrist trauma patients, and the evidence for reliability, validity, and responsiveness of each measure in this population. Methods: A systematic review of Pubmed, Medline, and CINAHL searching for randomized controlled trials of patients with traumatic injuries to the hand and wrist was carried out to identify the PROMs. For each identified PROM, evidence of reliability, validity, and responsiveness was identified using a further systematic review of the Pubmed, Medline, CINAHL, and reverse citation trail audit procedure. Results: The PROM used most often was the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire; the Patient-Rated Wrist Evaluation (PRWE), Gartland and Werley score, Michigan Hand Outcomes score, Mayo Wrist Score, and Short Form 36 were also commonly used. Only the DASH and PRWE have evidence of reliability, validity, and responsiveness in patients with traumatic injuries to the hand and wrist; other measures either have incomplete evidence or evidence gathered in a nontraumatic population. Conclusions: The DASH and PRWE both have evidence of reliability, validity, and responsiveness in a hand and wrist trauma population. Other PROMs used to assess hand and wrist trauma patients do not. This should be considered when selecting a PROM for patients with traumatic hand and wrist pathology.
Keywords: patient-reported outcomes measures, hand/wrist trauma, reliability, validity, responsiveness
Introduction
The focus of health care delivery in the 21st century is increasingly shifting, by necessity, toward achieving optimal patient outcomes at reasonable cost. This has led health care professionals, including surgeons, to consider the quality and efficacy of the interventions available to them, and how best to maximize benefit for their patients while using resources responsibly.
To accurately evaluate the efficacy of any intervention, it is vital to use appropriate outcome measures. Traditionally, hand and wrist surgeons have used objective clinical assessments, such as grip strength, range of motion, and radiographic measurements.9 These provide useful objective information about a given patient’s outcome, but do not consider the patient’s functional abilities, ability to resume normal activities of daily living or return to work, or persistent pain. “Appropriate, reliable and validated outcome measures are required that take into account all aspects of patient life that may be affected” if the outcome of hand surgery is to be fully evaluated.22
This led to a shift in the focus of outcome analysis toward patient-reported outcome measures (PROMs), which can be a valuable tool for gathering quantitative information about the everyday experience of a patient with a given condition.55 Longitudinal use of PROMs over multiple assessment points allows a surgeon to evaluate the progress of patient cohorts over time, as well as facilitating comparison between groups in clinical trials.35 Aside from use in research, or individual surgeons critically auditing their own performance, PROMs are set to play a key role in quality measurement and resource allocation in the future. Health care purchasers are increasingly moving away from buying a procedure or service, and are moving toward paying for a patient outcome. PROMs will have a key role to play in this practice.
A wide variety of outcome assessments have been proposed for the evaluation of patients with hand and wrist pathology, including generic measurements of health status, measurements specific to the upper limb, and measurements that are specific to the hand and wrist.
Generic instruments such as the Short Form 36 (SF-36)53 assess the impact of musculoskeletal conditions on the overall health and well-being of a patient, and were designed for use in a broad range of conditions.9 They have favorable measurement properties, and can be useful for drawing comparisons about patient-reported health states across groups with varying clinical conditions.35 However, the use of generic tools, such as the SF-36, in the outcome assessment of musculoskeletal conditions and interventions is of limited value because they fail to examine for condition-specific functional outcomes.
Region-specific PROMs, such as the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire,22 claim to assess both symptoms and functional status in patient groups with upper limb musculoskeletal pathology. The DASH has been shown by multiple studies to have an excellent reliability, validity, and responsiveness profile, and it is widely used in the assessment of the upper limb. However, the DASH conceptualizes the upper extremity as a single functional unit, so it is questionable whether it is as useful an assessment tool for hand and wrist pathology as an anatomical site-specific questionnaire.
Anatomical site, or condition-specific, assessment tools include questions on aspects of health affected by the specific body region.55 They have great potential to evaluate domains of physical function and health-related quality of life commonly affected by the specified anatomical site.38 The Patient-Rated Wrist Evaluation (PRWE)29 score and Michigan Hand Outcomes score10 are both examples of PROMs that are commonly used to assess outcome following hand and wrist surgery.
There are now a large number of available PROMs, even within the relatively narrow field of hand and wrist surgery. It is a natural assumption that most of the commonly used outcome assessments had their reliability, validity, and responsiveness assessed before being widely used in clinical practice. Close scrutiny of the measurement properties of these tools, however, is a relatively recent phenomenon, and many of the historical scoring systems have not undergone rigorous assessment. In addition, the characteristics of a patient undergoing elective hand and wrist surgery are likely to be very different to those who experience traumatic hand and wrist pathology. When undertaking an elective procedure for a chronic condition, a patient’s function deteriorates gradually over time causing him or her to adjust one’s functional requirements accordingly; in an acute traumatic event, this is not the case so a patient’s ability to assess changes in function against baseline will be different. Thus, the reliability, validity, and responsiveness of an instrument cannot be assumed to be equal across each patient group.
The aims of this article are to identify which PROMs are being used in randomized controlled trials involving patients who have suffered traumatic injuries to the hand and wrist, to investigate the reported reliability, validity, and responsiveness of each PROM in a trauma population and to identify potential areas for future research.
Methods
Design
This was a systematic review of the PROMs used in randomized controlled trials to assess outcomes for hand and wrist trauma patients.
Search Strategy
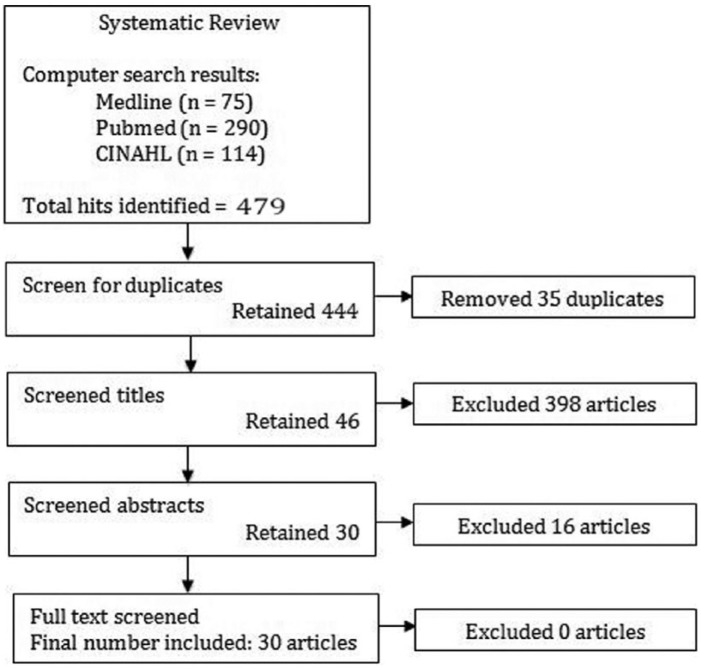
Searches were performed using Medline, Pubmed, and CINAHL from the earliest records available up to the search date April 2013. The search terms used were described in Figure 1.
Figure 1.
Keyword search terms used for primary literature search.
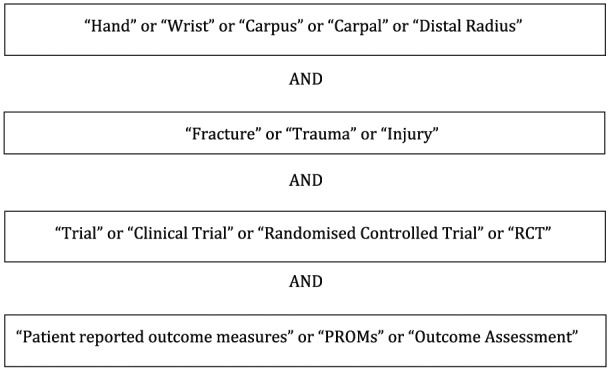
The lead author carried out a conventional 4-stage screening process to identify studies meeting the inclusion criteria. The senior author was available for consultation when there was doubt over the suitability of a study for inclusion. Stage 1 of the screening process removed any studies which were duplicated, stage 2 involved screening of titles, stage 3 screened abstracts, and stage 4 examined the papers in full to check they met the inclusion and exclusion criteria (Figure 2).
Figure 2.
Summary of the 4-stage screening process and the number of papers identified/removed at each stage.
Study Selection
Only randomized controlled trials examining the efficacy of interventions (surgical or otherwise) in a patient group who had suffered traumatic injuries to their hand or wrist were selected. Each was required to have used a PROM as part of their outcome assessment. For the purposes of this study, PROMs were defined as any outcome assessment tool that included a patient-reported component. For example the Gartland and Werley score, which is largely a surgeon-reported tool, was included on the basis of the patient-reported pain element. Studies were excluded if the patient group had suffered upper limb injuries that did not involve the hand or wrist, and if the patient group had undergone elective surgical interventions for chronic conditions. No exclusions were based on type of intervention type, length of follow-up, or numbers lost to follow-up, as these were not relevant to the article.
Data Extraction
The 30 papers accepted for inclusion in the study are documented in Table 1. For each paper, the author, year, clinical intervention, PROM, and any other outcome measure used were summarized (Table 1). The PROMs identified are shown in Table 2.
Table 1.
Details of the Papers Included in the Review.
| Author | Clinical population | Intervention | Patient-reported outcome measures | Other outcome assessments |
|---|---|---|---|---|
| Magnus et al31 | 39 females older than 50 years with a distal radius fracture | Contralateral strength training | PRWE | Grip strength, ROM |
| Rostami et al41 | 30 adults with hand injuries | Mirror therapy | DASH | Total active motion |
| Rhee et al40 | 105 adults with metacarpal fractures | Retrograde fixation using IM Kirschner wire | DASH | ROM |
| Schønnemann et al46 | 61 adults with distal radius fracture | External versus internal fixation | DASH, PRWE | Grip strength, radiographic assessment |
| Wilcke et al56 | 63 adults with distal radius fractures | Locked volar plate versus external fixation | DASH, PRWE | Radiographic assessment |
| Boutis et al7 | 100 children with distal radius fractures | Cast versus splint | Activities Scale for Kids | |
| Belloti et al6 | 100 adults with distal radius fractures | Percutaneous pinning versus external fixation | DASH | Pain score, ROM, grip strength, and radiographic assessment |
| Gruber et al19 | 54 adults with distal radius fracture | Volar plate internal fixation | DASH, SF-36, Gartland and Werley | Casting score |
| Belloti et al6 | 100 adults with distal radius fracture | Percutaneous pinning versus bridging external fixation | DASH | Pain score, ROM, grip strength |
| Pike et al39 | 87 adults with acute mallet finger | Volar versus dorsal versus custom thermoplastic splinting | Michigan Hand Outcomes Questionnaire | Radiographic assessment |
| Rozental et al42 | 45 adults with distal radius fracture | Open reduction internal fixation versus closed reduction and percutaneous fixation | DASH | ROM, grip strength |
| Wei et al54 | 46 adults with distal radius fractures | External fixation versus radial column plate versus volar plate | DASH | Grip strength, pinch strength, ROM, radiographic assessment |
| Sammer et al43 | 99 adults with distal radius fractures | Fragment specific versus volar plate fixation | Michigan Hand Outcomes Questionnaire | ROM, radiographic assessment |
| Hofmeister et al20 | 81 patients with 5th metacarpal neck fractures | Variations of the casting technique | DASH | Grip strength, range of motion and radiographic assessment |
| Varitimidis et al51 | 40 adults with intra-articular distal radius fractures | Fluoroscopic versus arthroscopic reduction | DASH, Mayo Wrist Score | |
| Lozano-Calderon et al26,29 | 60 patients with distal radius fracture | Early versus late mobilization | DASH, Gartland and Werley score, Mayo Wrist Score | Grip strength, ROM, radiographic assessment |
| Vinnars et al52 | 83 patients with acute scaphoid fracture | Nonoperative versus operative treatment | DASH, PRWE | |
| Földhazy et al16 | 87 adults with distal radius fractures | No intervention | Green and O’Brien score | Grip strength, ROM, radiographic assessment |
| Cognet et al11 | 67 adults with distal radius fractures | Open reduction internal fixation | Green and O’Brien score, DASH, PRWE | Radiographic assessment |
| Schneiders et al45 | 344 patients with distal radius fractures | No intervention | Gartland and Werley score | Radiographic assessment |
| Atroshi et al3 | 38 adults with distal radius fractures | Wrist bridging versus nonbridging external fixation | DASH | Grip strength, ROM |
| Müller et al36 | 68 patients with acute scaphoid fractures | Open reduction internal fixation | DASH, Krimmer wrist score | Pain score, radiographic assessment, grip strength |
| Maciel et al30 | 41 patients with distal radius fractures | Activity focused physiotherapy versus exercise and advice | PRWE | ROM, pain score, grip strength |
| Cassidy et al8 | 323 patients with distal radius fractures | Use of Norian SRS cement | SF-36 | Pain score, ROM |
| O’Connor et al37 | 68 adults with distal radius fractures | Plaster cast versus splint | Gartland and Werley score | Radiological assessment, ROM |
| Konrath23 | 25 patients with distal radius fractures | Trimed fragment-specific fixation | DASH, PRWE | ROM, radiographic assessment |
| Arora et al2 | 130 adults, over 70 years, with distal radius fractures | Nonoperative treatment versus volar locking plate | DASH, PRWE, Green and O’Brien score | Pain score, radiographic assessment |
| Egol et al15 | 280 patients with distal radius fractures | Bridging external fixation with K-wire versus volar plate | DASH | |
| Krukhaug et al24 | 75 patients with distal radius fractures | Comparison of two external fixators | DASH | Visual analog score for pain |
| Abramo et al1 | 50 patients with unstable distal radius fractures | Open reduction and internal fixation versus external fixation | DASH | Radiographic assessment |
Note. PRWE, Patient-Rated Wrist Evaluation; ROM, range of motion; DASH, Disabilities of the Arm, Shoulder and Hand; SF-36, Short Form 36.
Table 2.
The PROMs Identified.
| PROM | Studies using the PROM | Anatomical region | Assesses | No. of items |
|---|---|---|---|---|
| DASH | 20 | Shoulder, arm, hand | Symptoms, function | 30 |
| PRWE | 8 | Wrist/hand | Symptoms, function | 15 |
| Gartland and Werley score | 4 | Wrist/hand | Symptoms, function, deformity | 4 |
| Green and O’Brien score | 3 | Wrist/hand | Symptoms, function, X-ray | 5 |
| SF-36 | 2 | Generic | Physical and mental health | 36 |
| Michigan Hand Outcomes Questionnaire | 2 | Hand | Symptoms, function, satisfaction | 37 |
| Mayo Wrist Score | 2 | Wrist | Symptoms, function | 4 |
| Krimmer wrist score | 1 | Wrist | Symptoms, function | 4 |
| Activities Scale for Kids | 1 | General activity | Function | 30 |
Note. PROM, patient-reported outcome measure; DASH, Disabilities of the Arm, Shoulder and Hand; PRWE, Patient-Rated Wrist Evaluation; SF-36, Short Form 36.
Once the relevant PROMs had been identified, a separate literature search was performed for each to investigate whether there was evidence of reliability, validity (construct and content), and responsiveness in a hand and wrist trauma population. The search terms used for the process were “(name of patient-reported outcome measure)” AND “trauma OR injury OR fracture” AND “reliability OR validity OR responsiveness.”
All the studies identified with these searches were studied to assess whether the PROMs’ reliability, validity (construct and criterion), and responsiveness had been demonstrated in a hand and wrist trauma population. Any work examining the reliability, validity and responsiveness of the PROM in question in a hand and wrist trauma population was then thoroughly examined. If there was positive evidence of a given measurement property in a hand and wrist trauma population, this was demonstrated with +, if there was negative evidence of a given measurement property, this was demonstrated with a −, and in the event that no evidence existed on the measurement properties of a given PROM, this was represented with a 0. In the event that was evidence of the measurement properties of a given PROM that had been gathered in a population not including hand and wrist trauma population, this was reported in brackets.
Results
Search Results
The search of Medline, Pubmed, and CINAHL followed by the described 4-stage screening process returned a total of 30 results (see Figure 2).
Patient-Reported Outcome Measures
Nine PROMs were used in these 30 studies. The DASH score was used most frequently, appearing in 20 of the 30 studies. The PRWE was used in eight of the studies, with other measures (Gartland and Werley score, Green and O’Brien score, Michigan Hand Outcomes Questionnaire, Mayo Wrist Score and SF-36) each used on 2 or 3 occasions. The Activities Scale for Kids (ASK) and the Krimmer wrist score were each used on one occasion (Table 2).
Reliability, Validity, and Responsiveness
When assessing reliability, it is important to consider both internal consistency and reproducibility. Internal consistency is a measure of the correlation of different items in the PROMs that measure a similar parameter. It is generally expressed through examining the correlation of each item with other similar outcome measures to generate a value for Cronbach’s alpha. Reproducibility refers to the test-retest properties of a measurement and examines how consistently the same test administrator achieves results for a given test on the same participant in a stable disease state.
Construct validity refers to the degree to which a test measures what it reports to measure, and whether the individual scales behave as expected. Therefore, good construct validity is vital if meaningful clinical conclusions are to be made on the results of a given test. Criterion validity assesses how well a given measurement performs when compared with a “gold-standard” measurement. Responsiveness is the ability of a test to detect important changes in a clinical condition; it is expressed as the standardized response mean (SRM).
A summary of the reliability, validity, and responsiveness findings of the identified PROMs in a hand and wrist trauma population is presented in Table 3. The DASH, PRWE, Michigan Hand Outcomes Questionnaire, SF-36, and ASK had good evidence of reliability, but this evidence was not gathered in a hand and wrist trauma population for 2 of the measures (SF-36 and ASK). This was also true for validity as the same 5 measures had good evidence of validity, but this had not been assessed in a hand and wrist trauma population for the Michigan Hand Outcomes Questionnaire and ASK. Four measures showed good evidence of responsiveness, with 3 in a hand and wrist trauma population (DASH, PRWE, Michigan Hand Outcomes Questionnaire).
Table 3.
Summary of Reliability, Validity, and Responsiveness Evidence in Hand and Wrist Trauma Patients.
| Reliability |
||||
|---|---|---|---|---|
| Internal consistency | Reproducibility | Validity (construct) | Responsiveness | |
| DASH | + | + | + | + |
| PRWE | + | + | + | + |
| Gartland and Werley | 0 | 0 | 0 | 0 |
| Green and O’Brien score | 0 | 0 | 0 | 0 |
| Michigan Hand Outcomes Questionnaire | + (Not trauma) | + (Not trauma) | + (Not trauma) | + |
| Mayo Wrist Score | 0 | 0 | 0 | 0 |
| SF-36 | + (Not trauma) | + (Not trauma) | + | − |
| Activities Scale for Kids | + (Not trauma) | + (Not trauma) | + (Not trauma) | + (Not trauma) |
| Krimmer wrist score | 0 | 0 | 0 | 0 |
Note. + = positive evidence identified; − = negative evidence identified; 0 = no evidence available; (Not trauma) = this addendum was added when the evidence identified had not been reported in a hand and wrist trauma population; DASH, Disabilities of the Arm, Shoulder and Hand; PRWE, Patient-Rated Wrist Evaluation; SF-36, Short Form 36.
Discussion
The PROM used most often was the DASH questionnaire; the PRWE, Gartland and Werley score, Michigan Hand Outcomes score, Mayo Wrist Score, and SF-36 were also used. Other PROMs such as the Krimmer wrist score and ASK were used just once.
Of the PROMs identified, only the DASH and PRWE have evidence of reliability, validity, and responsiveness in patients with traumatic injuries to the hand and wrist; other measures either have incomplete evidence or evidence gathered in a nontraumatic population.
Disabilities of the Arm, Shoulder and Hand Questionnaire
The DASH questionnaire was developed in 1996, as a joint venture by the American Academy of Orthopaedic Surgeons, the Council of Musculoskeletal Specialty Societies, and the Institute for Work and Health. The aim was to produce a tool capable of evaluating single or multiple disorders specific to the upper limb.22 A 3-stage process with initial item generation by a group of clinical experts and methodologists was used to develop the scale. They subsequently underwent item reduction and field testing.22
The DASH is a self-administered questionnaire that consists of 30 core questions with an optional 8 further questions, which assess specific work and sport activities.48 Each item is scored on a 5-point Likert scale with lower scores indicating with minimal impairment.48 Several papers have demonstrated that the DASH is a reliable, valid, and responsive instrument for the assessment of disability and function in patients with upper limb pathology. Beaton et al examined the use of the DASH in 200 patients with a combination of shoulder and wrist pathology and reported good test-retest reliability, validity, and responsiveness in this population.4
Lovgren et al looked specifically at the reliability of the DASH in a hand and wrist trauma population and found it to have good internal consistency, with Cronbach’s alpha values 0.96 in the Disability subscale and 0.94 in the Optional scale.25 Test-retest reliability was reported as excellent with intraclass correlation coefficient (ICC) of .92. The study also showed construct validity similar to that of the PRWE.25 Dias et al evaluated the validity of the DASH in a population that included trauma patients, finding it to have poor construct validity for nerve disorders but reasonable validity for wrist and finger pathology.14 The paper also referred to the DASH’s “troubling” correlation with established measures, but the comparison was with the Gartland and Werley score for wrist pathology, an outcome measure that has no evidence of reliability, validity, or responsiveness and relies mainly on objective and radiographic measurements.14 The DASH shows good responsiveness in a hand and wrist trauma population, with a SRM of 2.07 in a population of 59 distal radius patients.28 All of the quoted evidence for the reliability, validity, and responsiveness of the DASH was carried out by teams independent from the designers of the score.
The DASH is well established and was by far the most commonly used PROM found in this study. It has consistently demonstrated good reliability, validity, and responsiveness in several psychometric studies. However, recent work has questioned the validity of the measure in a hand and wrist population.
Patient-Rated Wrist Evaluation
The PRWE was developed in 1998 by MacDermid et al29 in response to a perceived lack of reliable and valid tools for quantifying wrist pain and disability from a patient’s perspective. The rating tool was developed using a survey of the members of the International Wrist Investigators Workshop (n = 151). This asked the International Wrist Investigators to define current practice and to take opinions on appropriate content with respect to outcome measurement after wrist injury. A 66% response rate was achieved and the PRWE was developed on the basis of this survey of surgeons. It was subsequently tested for reliability in a population of hand and wrist trauma patients (64 distal radius fractures and 35 scaphoid fractures); validity was assessed in 101 patients with distal radius fractures.29
Initial reliability testing of the PRWE was undertaken in 3 separate groups. Group 1 had distal radius fractures, group 2 were patients with healed fractures who had undergone physiotherapy, and group 3 were patients 6 years post treatment for scaphoid nonunion.29 This revealed excellent test-retest reliability in all groups with reliability coefficients (ICC) of >.9.29 This was reproduced by Lovgren et al, independent from the designers of the test, in 32 patients with distal radius fractures. They reported an ICC > .9, which is considered to be excellent.25 They also examined the internal consistency of this PROM with Cronbach’s alpha, and this was also high (0.89-0.95).25
MacDermid et al felt that the manner in which the PRWE was designed, using expert surgical opinion, gave it automatic content, or face, validity despite the lack of patient input. Thus, they focused on construct and criterion validity when assessing its validity. Construct validity was demonstrated as statistically significant differences were found in the PRWE over time (P < .001) in 101 distal radius fracture patients, which was mirrored by improvement in the SF-36. The amount of improvement was 74% as measured by the PRWE compared with 16% for the SF-36. Criterion validity was measured against the SF-36 and a statistically significant correlation was shown in all domains. This supports the validity of the PRWE in measuring pain and disability in a distal radius fracture population.29 Lovgren et al also examined the validity of the PRWE and reported good convergent validity. They concluded that it was a useful measure in both the acute and rehabilitation phase of distal radius fracture.25
MacDermid et al later demonstrated the responsiveness of the PRWE in 59 distal radius fracture patients, finding that the PRWE, with a SRM of 2.27, was comparable with the DASH (SRM, 2.01). Both the PRWE and the DASH considerably outperformed the SF-36 (SRM, 0.92).27 No data were found on the responsiveness of the PRWE, which was independent of the designers of the score.
Of all the PROMs for the assessment of hand and wrist trauma, the PRWE has by far the best demonstrated reliability and validity in a wrist trauma population. It is the most responsive measure for a distal radius fracture population. It must, however, be remembered that the measure is specific to the wrist and is of little use in assessing a patient with hand injuries.
Gartland and Werley Score
The Gartland and Werley score,17 originally described in 1951, and subsequently modified by Sarmiento et al in 1975,44 is an outcome measure for wrist pathology that combines both subjective and objective factors, recorded by the observer. Demerit points are awarded for pain, stiffness and disability, range of motion, and distal radio-ulna joint pain with further points relating to complication profile, including radiographic evidence of posttraumatic osteoarthritis.50 Sarmiento’s modification added points for pronation and grip strength.44 The final score is a value between 0 and 52 with low scores corresponding with the best outcome.50 Some authors have criticized the scoring system as confusing, because surgeon interpretation can play a significant role, and suggested that using a later modification of the test, by Stewart et al in 1986, would be an improvement.13
The measure has been in use since 1951, and in its modified form since 1975, but our study found no evidence to demonstrate its reliability, validity, or responsiveness. Despite the extensive use of this measure in clinical practice, there have been no reliability, validity, or responsiveness studies published to date.
Michigan Hand Outcomes Questionnaire
The Michigan Hand Outcomes Questionnaire, introduced in 1998 by Chung et al, was developed at the Section of Plastic and Reconstructive Surgery at the University of Michigan Medical Centre.10 The aim was to produce an assessment tool capable of measuring outcomes for patients with all types of hand disorder. After the identification of the key domains for investigation, an initial pool of 100 questions was reduced through pilot testing on 20 patients and follow-up testing on 200 hand surgery patients to a 37-item questionnaire.10
A 2013 review into the use of the Michigan Hand Outcomes Questionnaire found that it had been used in 58 clinical research studies and 18 studies had investigated the measurement properties of the assessment tool.47 Chung et al initially reported the measure to have excellent test-retest reliability with 5 of the 6 scales having an ICC of >.85.10 This has been reproduced in subsequent studies, which found an ICC of .95 in patients with rheumatoid arthritis by a group independent to the Chung’s team.32 Chung et al also reported excellent internal consistency with Cronbach’s alpha values of 0.84 to 0.93 across the 6 domains.10 No work has been done to assess these indices in a purely hand and wrist trauma patient group, but Dias et al reported similar internal consistency values of 0.82 to 0.96 in 200 patients that included trauma patients, again independently from the Chung’s original design team.
The validity of the Michigan Hand Outcomes Questionnaire was reported by Chung et al who found that construct validity was demonstrated by significant correlation between scales in a predictable pattern. Chung felt that criterion validity was not assessable, given the lack of a gold standard, but the measure compared favorably with the generic Short Form 12 questionnaire.10 Dias et al also investigated the validity of the DASH, concluding that there was questionable criterion validity based on poor correlation with the Levine score and Gartland and Werley score; however, it must be remembered that neither of their chosen “gold-standard” outcome measures has proven measurement properties.14 Responsiveness of the Michigan Hand Outcomes Questionnaire in a sample of 105 patients with hand injuries reported a SRM of 1.05, which was higher than the DASH, but it is not clear whether this has clinical significance.21
The Michigan Hand Outcomes Questionnaire has undergone extensive psychometric testing since its introduction in 1998 and has been shown to be a reliable, valid, and responsive tool for outcome assessment in patients with hand injuries. At present, the reliability and validity findings have not been reproduced specifically in a hand trauma population.
Green and O’Brien Score
The Green and O’Brien score, introduced in 1978, is a demerit scoring system assessing pain, disability, range of movement, strength, and radiographic features.18 The score is primarily evaluated by a doctor but does require a subjective evaluation of pain, which is patient reported.
Despite being one of the first assessment tools available for the assessment of hand and wrist function following injury, its reliability, validity, or responsiveness have never been assessed.
Mayo Wrist Score
Cooney et al modified the Green and O’Brien score in 1987 by changing the demerit items and removing radiographic indices. The resulting outcome measure was referred to as the Mayo Wrist Score.12 This assesses 4 domains: pain, grip strength, range of motion, and return to employment. Each domain is scored out of 25 points to produce a total score out of 100 points. High scores correlate with good function: Scores of 90 to 100 points denote “excellent” function and a score of less than 65 is considered “poor.”
Despite being used by several papers assessing wrist function, no work has been done on the reliability, validity, or responsiveness of the measure.
Short Form 36
The SF-36 is a patient-reported health survey consisting of 8 scaled scores from which final mental and physical scores, each out of 100, are produced. The score was developed as a result of the Medical Outcomes Study undertaken by the Rand Corporation in 1992.53 It is a generic measure of health status and not specific to a particular anatomical region.
The SF-36 has been subject to rigorous psychometric evaluation since its introduction, initially by Ware et al, who reported a reproducibility ICC of >.8 for each of the subscales, and >.9 for the Physical and Mental Component subscales.33,34 The same authors also reported content, construct, and criterion validity in 4 patient groups, which included patients with a combination of medical and psychiatric illnesses.
Our search found little evidence on the reliability of the SF-36 specifically in a hand and wrist trauma patient group. Soohoo et al examined the construct validity and criterion validity of the SF-36 when comparing it with the DASH. They reported a Pearson correlation coefficient of −.36 to −.62, and noted that the DASH had fewer floor and ceiling scores than the subscales of the SF-36.49 MacDermid et al compared the responsiveness of the SF-36 with the DASH and PRWE in a population of distal radius fracture patients and reported that the SF-36 had significantly impaired responsiveness (SRM 0.92) compared with the DASH (SRM 2.01) and PRWE (SRM 2.27).
The SF-36 is a widely used health outcome measure, and has been independently shown to be reliable, valid, and responsive in a generic population. There is limited evidence available regarding its use in a hand and wrist trauma population, and there is evidence to suggest that it is a less valid and responsive measure than other region-specific scoring systems.
Activities Scale for Kids
The ASK is a self-reported questionnaire designed to assess physical function in children. It is not suitable for adults. The scale contains 30 items, in 7 subdomains. These are aggregated into one overall summary score. It is aimed at children aged 5 to 15 years who are suffering from limitation in their physical ability due to musculoskeletal conditions. The scale has been shown to be reliable, valid, and responsive in children with a variety of conditions, including cerebral palsy, juvenile arthritis, and bone tumors. No studies have investigated whether the ASK is reliable, valid, or responsive in a hand and wrist trauma population.
Krimmer Wrist Score
The Krimmer wrist score is a 4-point scoring system. It has been used in the assessment of outcome after wrist fusion, intercarpal fusion, scaphoid nonunion surgery, and other wrist procedures. It assesses power, range of motion, pain, and function to produce a maximum score of 100 points. It is rarely used in the assessment of trauma patients. No evidence of its reliability, validity, or responsiveness for patients with hand or wrist trauma was found.
In conclusion, clinical trials investigating hand and wrist trauma patients have most frequently used the DASH score, which has specific evidence of reliability, validity, and responsiveness in this population. The DASH is, however, less responsive than the PRWE for patients with distal radius fractures. The PRWE is more site specific than the DASH and also has evidence of reliability, validity, and responsiveness in a hand and wrist trauma population. Despite its excellent psychometric properties, the PRWE is specifically designed for the assessment of wrist pathology, and therefore its use in patients with hand injuries requires further investigation.
The Michigan Hand Outcomes Questionnaire is a widely used and thoroughly investigated assessment tool with evidence of responsiveness in a hand and wrist trauma population, and reliability and validity in a nontrauma population. As suggested in the title, the Michigan Hand Outcomes Questionnaire is specific to the hand and therefore is not intended for use in assessing patients with wrist injuries. Its use in assessing patients with traumatic injuries to the wrist requires further investigation.
The SF-36 and ASK are both generic measures of health status. They both have evidence of reliability, validity, and responsiveness but not in a hand and wrist trauma population. The SF-36 has been shown to be less valid than the DASH, and less responsive than DASH and PRWE in a hand and wrist trauma population.
The Gartland and Werley score, Green and O’Brien score, Mayo Wrist Score, and Krimmer wrist score are well-known assessment tools and are still occasionally used in research. None of these assessment tools has any evidence of reliability, validity, or responsiveness in a hand and wrist trauma population.
Excluding the DASH, and the PRWE, many of the most frequently used PROMs for reporting outcomes in patients with traumatic injuries to the hand and wrist do not have complete evidence of reliability, validity, and responsiveness in a hand and wrist trauma population. This is clearly identifies an area where further research is required if these PROMs are to be used in the future to assess patient outcomes following injury and to measure the efficacy of different interventions. It is also worth noting that future validity research into hand and wrist PROMs should be undertaken by comparing the PROM in question, against “gold-standard” measures that have proven measurement properties.
Footnotes
Ethical Approval: Ethical approval for this study was waived by our institutional review board who did not consider it necessary to give approval for a systematic review of the literature on this subject.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This study involves no human participants, so informed consent was not sought or required.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Abramo A, Kopylov P, Geijer M, Tägil M. Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop. 2009;80(4):478-485. doi: 10.3109/17453670903171875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23(4):237-242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 3. Atroshi I, Brogren E, Larsson G-U, Kloow J, Hofer M, Berggren A-M. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77(3):445-453. doi: 10.1080/17453670610046389. [DOI] [PubMed] [Google Scholar]
- 4. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146. [PubMed] [Google Scholar]
- 5. Belloti JC, Moraes VY, Albers MB, Faloppa F, Santos Dos JBG. Does an ulnar styloid fracture interfere with the results of a distal radius fracture? J Orthop Sci. 2010;15(2):216-222. doi: 10.1007/s00776-009-1443-7. [DOI] [PubMed] [Google Scholar]
- 6. Belloti JC, Tamaoki MJS, Atallah AN, Albertoni WM, Santos dos JBG, Faloppa F. Treatment of reducible unstable fractures of the distal radius in adults: a randomised controlled trial of De Palma percutaneous pinning versus bridging external fixation. BMC Musculoskelet Disord. 2010;11:137. doi: 10.1186/1471-2474-11-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boutis K, Willan A, Babyn P, Goeree R. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ. 2010;182(14):1507-1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cassidy C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003;85-A(11):2127-2137. [DOI] [PubMed] [Google Scholar]
- 9. Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand—which one to choose? Int Orthop. 2007;32(1):1-6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. YJHSU. 1998;23(4):575-587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 11. Cognet JM, Geanah A, Marsal C, Kadoch V, Gouzou S, Simon P. [Plate fixation with locking screw for distal fractures of the radius]. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(7):663-672. [DOI] [PubMed] [Google Scholar]
- 12. Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136-147. [PubMed] [Google Scholar]
- 13. Davis TR. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1987;69(5):791. [PubMed] [Google Scholar]
- 14. Dias JJ, Rajan RA, Thompson JR. Which questionnaire is best? the reliability, validity and ease of use of the patient evaluation measure, the Disabilities of the Arm, Shoulder and Hand and the hand and the Michigan Hand Outcome Questionnaire. J Hand Surg Eur Vol. 2008;33(1):9-17. [DOI] [PubMed] [Google Scholar]
- 15. Egol K, Walsh M, Tejwani N, McLaurin T, Wynn C, Paksima N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90(9):1214-1221. doi: 10.1302/0301-620X.90B9.20521. [DOI] [PubMed] [Google Scholar]
- 16. Földhazy Z, Törnkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L. Long-term outcome of nonsurgically treated distal radius fractures. YJHSU. 2007;32(9):1374-1384. doi: 10.1016/j.jhsa.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 17. Gartland JJ, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33-A(4):895-907. [PubMed] [Google Scholar]
- 18. Green DP, O’Brien ET. Open reduction of carpal dislocations: indications and operative techniques. YJHSU. 1978;3(3):250-265. [DOI] [PubMed] [Google Scholar]
- 19. Gruber G, Zacherl M, Giessauf C, et al. Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am. 2010;92(5):1170-1178. doi: 10.2106/JBJS.I.00737. [DOI] [PubMed] [Google Scholar]
- 20. Hofmeister EP, Kim J, Shin AY. Comparison of 2 methods of immobilization of fifth metacarpal neck fractures: a prospective randomized study. J Hand Surg Am. 2008;33(8):1362-1368. doi: 10.1016/j.jhsa.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 21. Horng Y-S, Lin M-C, Feng C-T, Huang C-H, Wu H-C, Wang J-D. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder, and Hand questionnaire in patients with hand injury. J Hand Surg Am. 2010;35(3):430-436. doi: 10.1016/j.jhsa.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 22. Hudak PL, Amadio PC, Bombardier C, et al. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602-608. doi: [DOI] [PubMed] [Google Scholar]
- 23. Konrath GA, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the trimed fixation system. J Orthop Trauma. 2002;16(8):578-585. [DOI] [PubMed] [Google Scholar]
- 24. Krukhaug Y, Ugland S, Lie SA, Hove LM. External fixation of fractures of the distal radius: a randomized comparison of the Hoffman compact II non-bridging fixator and the Dynawrist fixator in 75 patients followed for 1 year. Acta Orthop. 2009;80(1):104-108. doi: 10.1080/17453670902807433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lövgren A, Hellström K. Reliability and validity of measurement and associations between disability and behavioural factors in patients with Colles’ fracture. Physiother Theory Pract. 2012;28(3):188-197. [DOI] [PubMed] [Google Scholar]
- 26. Lozano-Calderón SA, Souer S, Mudgal C. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008;90(6):1297-1304. [DOI] [PubMed] [Google Scholar]
- 27. MacDermid JC, Richards RS, Donner A, Bellamy N, Roth JH. Responsiveness of the Short Form-36, Disability of the Arm, Shoulder, and Hand Questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg Am. 2000;25(2):330-340. doi: 10.1053/jhsu.2000.jhsu25a0330. [DOI] [PubMed] [Google Scholar]
- 28. MacDermid JC, Tottenham V. Responsiveness of the Disability of the Arm, Shoulder, and Hand (DASH) and Patient-Rated Wrist/Hand Evaluation (PRWHE) in evaluating change after hand therapy. J Hand Ther. 2004;17(1):18-23. [DOI] [PubMed] [Google Scholar]
- 29. MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577-586. [DOI] [PubMed] [Google Scholar]
- 30. Maciel JS, Taylor NF, McIlveen C. A randomised clinical trial of activity-focussed physiotherapy on patients with distal radius fractures. Arch Orthop Trauma Surg. 2005;125(8):515-520. doi: 10.1007/s00402-005-0037-x. [DOI] [PubMed] [Google Scholar]
- 31. Magnus CRA, Arnold CM, Johnston G, et al. Cross-education for improving strength and mobility after distal radius fractures: a randomized controlled trial. Arch Phys Med Rehabil. 2013;94(7):1247-1255. doi: 10.1016/j.apmr.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 32. Massy-Westropp N, Krishnan J, Ahern M. Comparing the AUSCAN Osteoarthritis Hand Index, Michigan Hand Outcomes Questionnaire, and sequential occupational dexterity assessment for patients with rheumatoid arthritis. J Rheumatol. 2004;31(10):1996-2001. [PubMed] [Google Scholar]
- 33. McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). Med Care. 1994 Jan;32(1):40-66. [DOI] [PubMed] [Google Scholar]
- 34. McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247-263. [DOI] [PubMed] [Google Scholar]
- 35. McPhail SM, Bagraith KS, Schippers M, Wells PJ, Hatton A. Use of condition-specific patient-reported outcome measures in clinical trials among patients with wrist osteoarthritis: a systematic review. Adv Orthop. 2012;2012(2):1-10. doi: 10.1186/1471-2474-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Müller M, Chen ZB, Al Morshidy A, Germann G, Sauerbier M. [Postoperative CT-controlled results of renewed osteosynthesis using screw fixation for acute scaphoid fractures]. Unfallchirurg. 2006;109(3):185-192. doi: 10.1007/s00113-005-1023-z. [DOI] [PubMed] [Google Scholar]
- 37. O’Connor D, Mullett H, Doyle M, Mofidi A, Kutty S, O’Sullivan M. Minimally displaced Colles’ fractures: a prospective randomized trial of treatment with a wrist splint or a plaster cast. J Hand Surg Br. 2003;28(1):50-53. [DOI] [PubMed] [Google Scholar]
- 38. Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27(3):S217-S232. [DOI] [PubMed] [Google Scholar]
- 39. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010;35(4):580-588. doi: 10.1016/j.jhsa.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 40. Rhee SH, Lee SK, Lee SL, Kim J, Baek GH, Lee YH. Prospective multicenter trial of modified retrograde percutaneous intramedullary Kirschner wire fixation for displaced metacarpal neck and shaft fractures. Plast Reconstr Surg. 2012;129(3):694-703. doi: 10.1097/PRS.0b013e3182402e6a. [DOI] [PubMed] [Google Scholar]
- 41. Rostami HR, Arefi A, Tabatabaei S. Effect of mirror therapy on hand function in patients with hand orthopaedic injuries: a randomized controlled trial. Disabil Rehabil. 2013;35(19):1647-1651. doi: 10.3109/09638288.2012.751132. [DOI] [PubMed] [Google Scholar]
- 42. Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation: a prospective randomized trial. J Bone Joint Surg Am. 2009;91(8):1837-1846. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 43. Sammer DM, Fuller DS, Kim HM, Chung KC. A comparative study of fragment-specific versus volar plate fixation of distal radius fractures. Plast Reconstr Surg. 2008;122(5):1441-1450. doi: 10.1097/PRS.0b013e3181891677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sarmiento A, Pratt GW, Berry NC. Colles’ fractures. Functional bracing in supination. J Bone Joint Surg Am. 1975;57(3):311-317. [PubMed] [Google Scholar]
- 45. Schneiders W, Biewener A, Rammelt S, Rein S, Zwipp H, Amlang M. [Distal radius fracture. Correlation between radiological and functional results]. Unfallchirurg. 2006;109(10):837-844. doi: 10.1007/s00113-006-1156-8. [DOI] [PubMed] [Google Scholar]
- 46. Schønnemann JO, Hansen TB, Søballe K. Randomised study of non-bridging external fixation compared with intramedullary fixation of unstable distal radial fractures. J Plast Surg Hand Surg. 2011;45(4-5):232-237. doi: 10.3109/2000656X.2011.613243. [DOI] [PubMed] [Google Scholar]
- 47. Shauver MJ, Chung KC. The Michigan Hand Outcomes Questionnaire after 15 years of field trial. Plast Reconstr Surg. 2013;131(5):779e-787e. doi: 10.1097/PRS.0b013e3182865d83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Smith MV. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277-285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. SooHoo NF, McDonald AP, Seiler JG, McGillivary GR. Evaluation of the construct validity of the DASH questionnaire by correlation to the SF-36. YJHSU. 2002;27(3):537-541. [DOI] [PubMed] [Google Scholar]
- 50. Souer J-S, Lozano-Calderon SA, Ring D. Predictors of wrist function and health status after operative treatment of fractures of the distal radius. YJHSU. 2008;33(2):157-163. doi: 10.1016/j.jhsa.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 51. Varitimidis SE, Basdekis GK. Treatment of intra-articular fractures of the distal radius fluoroscopic or arthroscopic reduction? J Bone Joint Surg Br. 2008;90(6):778-785. [DOI] [PubMed] [Google Scholar]
- 52. Vinnars B, Pietreanu M, Bodestedt A, Ekenstam FA, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176-1185. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 53. Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483. [PubMed] [Google Scholar]
- 54. Wei DH, Raizman NM, Bottino CJ, Jobin CM. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate: a prospective randomized trial. J Bone Joint Surg Am. 2009;91(7):1568-1577. [DOI] [PubMed] [Google Scholar]
- 55. Wells GA, Russell AS, Haraoui B, Bissonnette R, Ware CF. Validity of quality of life measurement tools—from generic to disease-specific. J Rheumatol Suppl. 2011;88:2-6. doi: 10.3899/jrheum.110906. [DOI] [PubMed] [Google Scholar]
- 56. Wilcke MKT, Abbaszadegan H, Adolphson PY. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop. 2011;82(1):76-81. doi: 10.3109/17453674.2011.552781. [DOI] [PMC free article] [PubMed] [Google Scholar]