Abstract
Background: A thumb interphalangeal (IP) joint arthrodesis is typically performed in 0° to 30° of flexion; most daily activities involve increased flexion at the IP joint to facilitate pinch and grip. This study evaluates the preferred thumb IP joint position with certain tasks of daily living to determine a more satisfactory angle. Methods: Twenty-eight healthy volunteers were splinted at various degrees (0°, 15°, 30°, 45°, bilaterally) with thumb orthotics, leaving the tip free, to mimic various angles of IP fusion. Participants underwent power tasks (pouring from a gallon jug, opening/closing a tight jar, lifting a heavy glass, and opening a door), timed precision tasks (writing, buttoning/unbuttoning a shirt, translating coins, zipping/unzipping a jacket, and opening/closing Velcro), as well as pinch and grip strength testing. All tasks were performed both at baseline (without any splinting) and with the thumb splinted in each angle. Participants used a 10-point Visual Analogue Scale (VAS) to rate the ease of each task as well as their overall satisfaction at baseline and at each of the various angles for their dominant and nondominant hand. Wilcoxon signed rank tests were conducted for outcomes, with P < .05 denoting statistical significance. Results: Power tasks were best accomplished at 0° for the nondominant hand and 0° to 30° for the dominant hand. Precision tasks were preferred at 15° for both dominant and nondominant hand. Grip strength was best at 15° and 0° for the nondominant and dominant hand, respectively. Pinch was equivocal between 0° and 30° for the nondominant hand and from 15° to 30° for the dominant hand. VAS ratings were most similar to baseline at a fusion angle of 15° followed by 30° for the dominant thumb and 30° followed by 15° for the nondominant thumb. Conclusions: A thumb IP fusion angle of 15° to 30° is a functional and preferred angle of thumb IP joint positioning for various activities of daily living.
Keywords: arthrodesis, interphalangeal joint, thumb
Background
Thumb interphalangeal (IP) joint arthrodesis is a recognized and accepted treatment option for certain thumb IP joint disorders, including rheumatoid arthritis, posttraumatic arthritis, instability, and osteoarthritis. Traditionally, the joint is fused at an angle somewhere between 0° and 30°.1,3,6-9 Most of the descriptions of angles are based on case series and personal experience. Differentiation of fusion angle based on job and function has been grossly described as 5° to 10° in individuals requiring large grip and 20° to 30° for smaller grip function.8
Yao et al has described the position of the thumb IP joint for usage of a smartphone for current technology.9 They tested healthy volunteers’ time to type certain sentences with their dominant thumbs splinted at 0°, 10°, and 30° of flexion at the IP joint and noticed no difference between 10° and 30°. Their conclusion was that the traditional fusion angle of 0° to 15° is an appropriate angle for activities related to smartphone use. While this study justifies the continuing use of the traditional angle range, the authors did not investigate other activities of daily living that might be affected by a fusion angle of 0° to 15°. The effect of pronation has also been evaluated.5 In 88 healthy participants, the thumbs were splinted at 40° of flexion, and photographs were taken of various activities. The thumbs ranged in pronation from 0° to 12°; however, there was no statistical difference depending on job type.
Functional data, describing the typical angle of the thumb IP joint for activities of daily living, power tasks, and precision tasks, are still lacking. Despite this deficiency, the accepted degree of fusion remains between 0° and 30°. We have noticed, through our personal observations, that thumb positioning for functionality, strength, and precision tasks appears to be performed naturally at an angle between 15° and 30° of flexion. The purpose of this study is to determine the optimal angle of the thumb IP joint during power and precision tasks of daily living. We hypothesized that an angle between 15° and 30° is a more appropriate fusion angle of the thumb IP joint.
Methods and Materials
After obtaining institutional review board (IRB) approval, 30 healthy volunteers were recruited for a prospective study. Patients were excluded if they were under 18 years of age, had previous surgery on the metacarpophalangeal or IP joint of the thumb, or were unable to read, write, or understand English. Informed consent was then obtained from all participants. Two people did not complete the tasks, 1 was called to a family emergency and 1 was called to work. Both occurred during early testing and did not return. Twenty-eight patients completed the study in its entirety in one sitting. The study group consisted of 11 males and 17 females with an average age of 33.5 years (range = 23-72). Twenty-five patients were right hand dominant and 3 were left hand dominant.
An intake sheet, which determined age, sex, and hand dominance, was filled out and recorded. Each participant was then measured and fit to a specific sized thumb splint (small, medium, or large), which had previously been made for each of the various fusion angles (0°, 15°, 30°, 45°). Splints were custom-made orthoplast thumb orthotics and placed dorsally leaving the tip free for sensibility (Figures 1a and 1b). This method was meant to mimic the various degrees of IP fusion angles.
Figure 1.
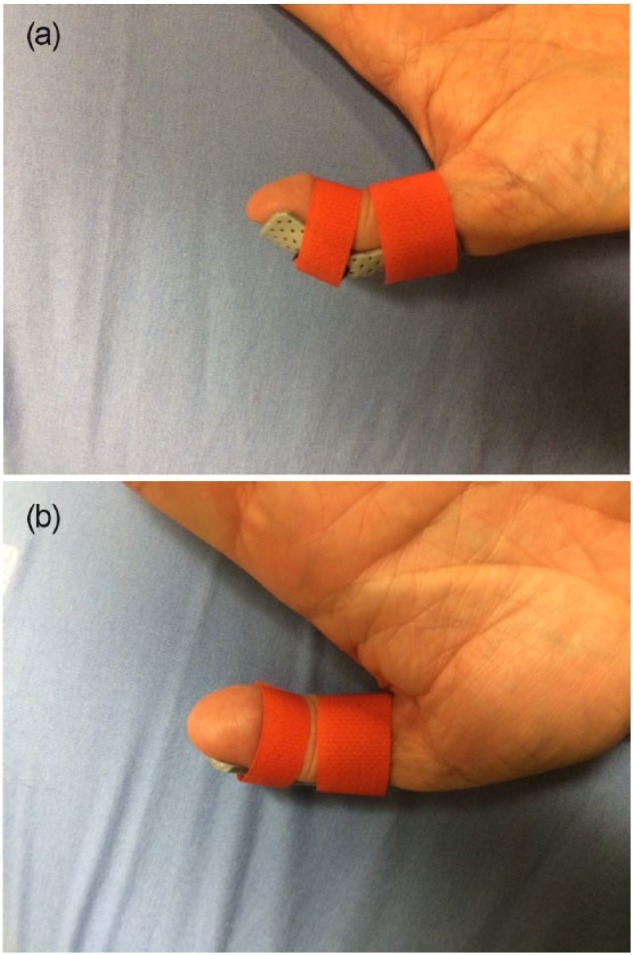
Photograph of a thumb splint that was utilized to secure the thumbs for the study. (a) lateral view and (b) anterior view.
The participants then performed a series of tasks, first at baseline without any splint applied, and then these tasks were repeated with the thumb splinted at each of the 4 positions. The splint was only applied to one hand at a time. The testing was then repeated utilizing the contralateral limb. Therefore, 9 trials were obtained (1 with the dominant hand unsplinted, 1 with the nondominant hand unsplinted, 4 with the dominant hand splinted, and 4 with the nondominant hand splinted). The tasks included 4 power tasks (opening/closing a tight jar, lifting a heavy glass, opening a door, and pouring from a gallon jug), and 6 timed precision tasks (zipping/unzipping a jacket, opening/closing Velcro, tying shoelaces into a bow know, writing, buttoning/unbuttoning a shirt, and translating coins from one hand to the other). Grip strength (Jamar Dynamometer, Lafayette Instruments, Lafayette, Indiana) and key pinch (Lafayette Instruments, Lafayette, Indiana) testing were also obtained for each hand and thumb position. The participants were instructed to proceed through these 10 tasks as quickly and accurately as they would do in normal daily life. All precision tasks were timed by an assistant and recorded as the average of 2 separate measurements per task. After completing each individual task, the participants were asked to rate the ease of completing the task on a 10-point Visual Analogue Scale (VAS). They also rated their overall satisfaction with their thumb at each position after the completion of all 10 tasks for each angle. Of note, writing was the only task completed with the dominant hand only (5 trials).
Separate Wilcoxon signed rank tests were conducted for selected outcomes, with P < .05 denoting statistical significance. Individual analysis between right and left hand dominant individuals was not completed due to the small sample size of left hand dominant participants. Therefore, handedness was combined into a dominant and nondominant category for data analysis.
Results
There were no significant difficulties with any one particular activity. Power tasks were most preferred with an angle of 0° with the nondominant hand and 0° to 30° with the dominant hand. Precision tasks were preferred with an angle of 15° with both the nondominant and dominant hand. Among the different activities performed, the lowest average scores were seen for the button activity and picking up coins, both of which require high precision movements of the thumb (Table 1).
Table 1.
Median Grip and Pinch Strength (kg) by Thumb Position and Hand Dominance.
| Measurement | Grip strength | Pinch strength |
|---|---|---|
| Baseline ND | 86 | 17 |
| (47-127) | (6-24) | |
| 0° ND | 75 | 15 |
| (35-137) | (5-24) | |
| 15° ND | 80 | 15 |
| (35-135) | (4-27) | |
| 30° ND | 75 | 15 |
| (40-132) | (5-26) | |
| 45° ND | 79 | 14 |
| (35-120) | (4-28) | |
| Baseline Dom | 80 | 16 |
| (49-150) | (4-26) | |
| 0° Dom | 80 | 15 |
| (37-135) | (6-24) | |
| 15° Dom | 78 | 16 |
| (47-148) | (7-25) | |
| 30° Dom | 73 | 16 |
| (35-139) | (6-26) | |
| 45° Dom | 73 | 15 |
| (46-150) | (5-29) |
Note. Significant values (P < .05) are indicated by bolded and italicized numbers. Values in parentheses are ranges. ND, nondominant; Dom, dominant.
Precision task timing also changed based on the thumb position. The quickest average time for all tasks was noted at 15° in the nondominant hand. The dominant hand had no clear angular position that was superior, with various tasks performing just as well, or sometimes better than at baseline, with multiple positions of the thumb (Table 2). Most of the times were not significantly different compared to baseline with the exception of translation of coins from one hand to the other, which was increased at all static thumb positions.
Table 2.
Time (in Seconds) for Precision Tasks Separated by Thumb Position and Hand Dominance.
| Measurement | Zipper time | Velcro time | Knot time | Writing timea | Buttons time | Coins time |
|---|---|---|---|---|---|---|
| Baseline ND | 6.2 | 4.6 | 8.0 | NT | 25.8 | 13.9 |
| (3.1-15.8) | (1.1-15) | (4.4-19.9) | (20.1-55.8) | (9.8-19.9) | ||
| 0° ND | 6.8 | 4.4 | 8.7 | NT | 27.5 | 22.0 |
| (3.2-28.9) | (1.5-18.7) | (4-20.2) | (17.1-107) | (11.8-32.4) | ||
| 15° ND | 5.7 | 4.0 | 8.2 | NT | 26.5 | 17.9 |
| (2.4-12.8) | (1.8-15.7) | (4.2-17.6) | (15-57.8) | (14.4-29.6) | ||
| 30° ND | 6.4 | 4.1 | 8.4 | NT | 28.2 | 19.5 |
| (3.2-38.5) | (1.1-18.4) | (3.6-19.4) | (16.7-70) | (14.2-31.6) | ||
| 45° ND | 7.1 | 3.9 | 9.4 | NT | 28.9 | 19.5 |
| (3-10.9) | (1-15.7) | (4.7-20.8) | (16.6-68) | (13.4-31.5) | ||
| Baseline Dom | 7.4 | 4.8 | 8.1 | 9.5 | 29.2 | 14.5 |
| (4.1-23.8) | (1.2-17.5) | (5.1-19.2) | (7.3-23.3) | (20-55.8) | (5.9-19.8) | |
| 0° Dom | 7.8 | 4.6 | 8.7 | 10.1 | 31.4 | 20.5 |
| (2.9-11.8) | (1.5-18.5) | (4.9-19.7) | (7.9-16.2) | (18.1-58.3) | (13.1-34.7) | |
| 15° Dom | 7.5 | 3.8 | 8.3 | 9.2 | 27.9 | 18.5 |
| (2.9-18.2) | (1.1-14) | (4.1-23.8) | (7.3-26.5) | (1-63) | (13.5-32.4) | |
| 30° Dom | 7.3 | 4.4 | 8.5 | 9.0 | 27.9 | 18.8 |
| (2.3-15.3) | (1.1-14.2) | (4.5-22.3) | (6.8-24.3) | (17.4-63) | (12.8-37.2) | |
| 45° Dom | 6.5 | 4.3 | 8.2 | 9.6 | 29.1 | 18.1 |
| (2.3-19.2) | (1.1-12.7) | (4.6-19.9) | (6.3-23.7) | (17.2-65) | (13.5-27.1) |
Note. Significant values (P < .05) are indicated by bolded and italicized numbers. Values in parentheses are ranges. ND, nondominant; NT, not tested; Dom, dominant.
Tested with dominant hand only.
Grip strength of the nondominant hand resembled the baseline value at 15° (P > .05) followed by 45° (P < .05). Grip strength of the dominant hand resembled the baseline value 0° (P > .05) followed by 15° (P > .05). Key pinch was equivalent from 0° to 30° measuring slightly less than baseline (P > .05) with the nondominant hand. Dominant handed key pinch was best at 15° and 30°, which equaled the baseline value (P > .05; Table 3).
Table 3.
Visual Analogue Scores of the Ease of Task Completion by Position and Hand Dominance With Ranges.
| Measurement | Open jar | Lift glass | Door | Pour | Zipper | Velcro | Knot | Writinga | Buttons | Coins |
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline ND | 10 | 10 | 10 | 10 | 10 | 10 | 10 | NT | 10.0 | 10.0 |
| (7-10) | (9-10) | (9-10) | (9-10) | (9-10) | (8-10) | (9-10) | (9-10) | (7-10) | ||
| 0° ND | 9.9 | 9.75 | 9.9 | 9.9 | 9.6 | 9.7 | 9.4 | NT | 8.8 | 7.4 |
| (8-10) | (8-10) | (8-10) | (9-10) | (7-10) | (5-10) | (6-10) | (3-10) | (3-10) | ||
| 15° ND | 9.7 | 9.8 | 9.8 | 9.8 | 9.7 | 9.8 | 9.5 | NT | 8.9 | 8.2 |
| (8-10) | (7-10) | (8-10) | (8-10) | (4-10) | (5-10) | (4-10) | (4-10) | (3-10) | ||
| 30° ND | 9.8 | 9.8 | 9.9 | 9.9 | 9.6 | 9.8 | 9.4 | NT | 9 | 7.8 |
| (5-10) | (4-10) | (7-10) | (7-10) | (3-10) | (2-10) | (4-10) | (3-10) | (2-10) | ||
| 45° ND | 9.75 | 9.7 | 9.9 | 9.8 | 9.6 | 9.7 | 8.7 | NT | 7.8 | 6.5 |
| (6-10) | (4-10) | (7-10) | (7-10) | (5-10) | (2-10) | (2-10) | (3-10) | (1-10) | ||
| Baseline Dom | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| (6-10) | (9-10) | (9-10) | (9-10) | (6-10) | (8-10) | (9-10) | (9-10) | (9-10) | (9-10) | |
| 0° Dom | 9.8 | 9.8 | 9.9 | 9.9 | 9.5 | 9.8 | 9.1 | 9 | 8.1 | 6.8 |
| (9-10) | (8-10) | (8-10) | (9-10) | (7-10) | (5-10) | (5-10) | (6-10) | (4-10) | (3-10) | |
| 15° Dom | 9.8 | 9.8 | 9.8 | 9.9 | 9.7 | 9.8 | 9.4 | 9.6 | 9 | 8.8 |
| (7-10) | (7-10) | (7-10) | (8-10) | (8-10) | (7-10) | (3-10) | (7-10) | (7-10) | (4-10) | |
| 30° Dom | 9.75 | 9.8 | 9.8 | 9.8 | 9.5 | 9.8 | 9.1 | 9.5 | 9.2 | 8.6 |
| (8-10) | (5-10) | (8-10) | (8-10) | (6-10) | (2-10) | (6-10) | (6-10) | (4-10) | (2-10) | |
| 45° Dom | 9.7 | 9.7 | 9.7 | 9.8 | 9.5 | 9.7 | 9.3 | 9.6 | 8.6 | 7.7 |
| (7-10) | (4-10) | (5-10) | (5-10) | (4-10) | (3-10) | (3-10) | (6-10) | (2-10) | (2-10) |
Note. Significant values (P < .05) are indicated by bolded and italicized numbers. Values in parentheses are ranges. ND, nondominant; NT, not tested; Dom, dominant.
Tested with dominant hand only.
Subjective measurement for the total satisfaction of a particular thumb IP joint position with VAS scores differed depending on hand dominance. The dominant thumb had the highest satisfaction rate at 30° followed by 15°. Similarly, a fusion angle of 15° followed by 30° was preferred in the nondominant thumb (Table 4).
Table 4.
Median Overall Satisfaction by VAS Separated by Thumb Position and Hand Dominance.
| Measurements | Overall |
|---|---|
| Baseline ND | 10 |
| (7.4-10) | |
| 0° ND | 7.6 |
| (2.3-10) | |
| 15° ND | 9 |
| (3.3-10) | |
| 30° ND | 7.9 |
| (2.2-10) | |
| 45° ND | 7.2 |
| (0.8-9.8) | |
| Baseline Dom | 10 |
| (9-10) | |
| 0° Dom | 8.2 |
| (3.2-10) | |
| 15° Dom | 9.0 |
| (2.8-10) | |
| 30° Dom | 8.8 |
| (2.7-10) | |
| 45° Dom | 7.6 |
| (1-10) |
Note. Significant values (P < .05) are indicated by bolded and italicized numbers. Values in parentheses are ranges. VAS, Visual Analogue Scale; ND, nondominant; Dom, dominant.
Discussion
Thumb IP joint fusion is a treatment option for patients with IP joint pathology due to posttraumatic, degenerative, or unstable conditions. The functional effects of an arthrodesis procedure are dictated by the positioning of the thumb IP joint during the surgical procedure, and considering the many ways the thumb is utilized, this positioning may affect the overall satisfaction rate. Currently, the most frequently used angle for thumb IP fusion is established between 0° and 30° through previous works. There is little objective data with regard to the positional effect on function of activities of daily living. Our goal was to determine the angle of thumb IP joint fusion that provides patients the most function and satisfaction.
The patients’ thumbs were splinted with orthoplast splints on the dorsal surface of the thumb. In this method, the palmar pad of the thumb was left free for sensibility and tactile feedback to try to prevent influence on task completion. Splinting of the digital joints for evaluation is not a new concept and has been used successfully in the past for determination of outcomes.2,9 The question of the effect of splinting on overall strength of the participant has also been determined by Goetz et al.4 While their article specifically discussed the contribution of the flexor pollicis longus (FPL) to pinch strength, their participants utilized thumb IP splinting. To determine the effect of the splint, the thumbs were tested for grip strength in a splinted and unsplinted position prior to blockade of the FPL. No statistical difference was noted in the strength of a normal thumb with the splint applied.
Determining the position of the thumb depending on employment and gross usage has been evaluated previously. Large grip and the strength required for these tasks are better served in the 5° to 10° position compared with small gripping activities which utilized a more flexed thumb IP angle of 20° to 30° according to Sieber and Segmuller.8 However, activities of daily living are more varied and can exist from the fine motor skill required for buttoning buttons or translating coins to the more strength-driven activities of lifting, carrying, or squeezing.
The increased usage of the thumb for today’s technological advances, such as smartphone usage, has also been evaluated.9 The thumbs of patients were splinted, and the effects of positioning were observed with finer motor skills required for this type of phone activity. A fusion angle of between 10° and 30° was shown to neither help nor hinder the participants’ usage of the device. This study provides important information by showing that finer motor usage can occur without hindrance at a variety of fusion angles, but only evaluated smartphone usage and not other fine motor activities.
Our data demonstrate that activities of daily living can be influenced by the position of the thumb, in both their efficiency and the participants’ evaluation of ease. Overall, positioning with precision tasks seems more important than with power tasks. Precision task positioning was preferred at 15° for both the dominant and nondominant hand. Tasks were generally performed most efficiently with the thumb at 15° for the nondominant hand and no real preference was noted for the dominant hand. We feel this mimics activities in general when the nondominant hand is typically held in one position as an assist hand. The dominant hand requires increased manipulation for certain activities. The tasks such as unbuttoning buttons and coin manipulation were shown to be more difficult with the thumb IP joint fused, likely due to the dexterity required for these activities. The 15° and 30° angle was the closest to baseline measurements for these specific tasks.
Power tasks were best completed at an angle of 0° with the nondominant hand and anywhere from 0° to 30° for the dominant hand. Grip was best at 15° for the nondominant and 0° to 15° for the dominant, while pinch was best at 0° to 30° for the nondominant hand and 15° to 30° for the dominant hand. With gripping and strength, the thumb is typically in a more flexed posture, likely to engage the extrinsic FPL and increase total muscular involvement.
Overall, the position that was best preferred was 30° followed by 15° for the dominant hand and the opposite 15° followed by 30° for the nondominant hand. This position allows slight flexion at the thumb, engaging the FPL, and places the tip of the thumb over the index finger in a more natural pinch. A 0° flexion angle was favored third, and while this angle is a more traditionally accepted angle for thumb arthrodesis, our study demonstrates this position is an isolated preference in nondominant hand power tasks. The flexed angle of 45° is the least favorable with the worst performance in power tasks, precision tasks, grip, pinch, and overall preference. This position should be avoided.
Our study has multiple strengths. First, it is prospective in nature and therefore not limited by recall bias that may limit a retrospective study. It compares different fusion angles for multiple tasks, most of which are utilized daily in life, and represent a variety of ways in which the thumb is used. The participants were able to directly compare differing angles in one sitting and evaluate them subjectively, while objective measurements helped to validate the angles efficiency and effectiveness at completing the tasks. Previous studies examined subjective satisfaction and objective grip and pinch measurements with only the one arthrodesed position. Last, the methods for immobilization were utilized previously and found to have no effect on strength of the thumb.2,4,9
Our study had some weaknesses. Two participants left during the early testing phases of the study and did not return. The data were incomplete for both and did not extend beyond the first baseline unsplinted measurements. Therefore, it was excluded to prevent skewing the data or statistics. We chose to exclude patients with previous surgeries to the thumb as we felt it may influence the manner in which the thumb is utilized for pinch and activities. The angular positions referenced in this article cannot be accurately extended into this postsurgical population without further evaluation, as the authors are unsure if the data would be the same. In addition, there was no ability to determine any difference between left and right hand dominant individuals given the low sample size of left hand dominant participants. The dominant hand data were placed together in one group to allow comparison with nondominant hand tasks, but a difference in thumb positioning preference may exist between left and right hand dominant participants. Our group had no ambidextrous participants, and therefore, while it did not bias the data of the nondominant hand, the results may not be accurate to this population. Finally, our patient population, on average, was younger; therefore, other comorbid conditions, such as carpometacarpal (CMC) arthritis, sesamoid arthritis, metacarpophalangeal joint laxity, or metacarpophalangeal joint arthritis, in elderly patients may alter the optimal position, and future studies within this older population would be beneficial.
We recommend a fusion angle of between 15° and 30° when performing a thumb IP joint arthrodesis for increased patient satisfaction and function. Differentiating between these angles can be done depending on handedness of the patients if desired. Fusing outside of this range should consider the more extended 0° position rather than the more flexed 45° position.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: K.S.M. has received consulting fees from DePuy Synthes.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Carroll RE, Hill NA. Small joint arthrodesis in hand reconstruction. J Bone Joint Surg Am. 1969;51(6):1219-1221. [PubMed] [Google Scholar]
- 2. Domalain M, Evans PJ, Seitz WH, Jr, Li ZM. Influence of index finger proximal interphalangeal joint arthrodesis on precision pinch kinematics. J Hand Surg Am. 2011;36(12):1944-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ferlic DC, Turner BD, Clayton ML. Compression arthrodesis of the thumb. J Hand Surg Am. 1983;8(2):207-210. [DOI] [PubMed] [Google Scholar]
- 4. Goetz TJ, Costa JA, Slobogean G, Patel S, Mulpuri K, Travlos A. Contribution of flexor pollicis longus to pinch strength: an in vivo study. J Hand Surg Am. 2012;37(11):2304-2309. [DOI] [PubMed] [Google Scholar]
- 5. Jemec B, Verjee LS, Jain A, Sandford F. Rotation in the interphalangeal thumb joint in vivo. J Hand Surg Am. 2010;35(3):425-429. [DOI] [PubMed] [Google Scholar]
- 6. Rizzo M. Thumb arthrodesis. Tech Hand Up Extrem Surg. 2006;10(1):43-46. [DOI] [PubMed] [Google Scholar]
- 7. Shin EK, Osterman AL. Treatment of thumb metacarpophalangeal and interphalangeal joint arthritis. Hand Clin. 2008;24(3):239-250, v. [DOI] [PubMed] [Google Scholar]
- 8. Sieber HP, Segmuller G. [Arthrodesis of the interphalangeal joint of the thumb: indication, technic, results]. Handchir Mikrochir Plast Chir. 1983;15(1):11-16. [PubMed] [Google Scholar]
- 9. Yao J, Park MJ, Davis D, Chang J. Ideal position for thumb interphalangeal arthrodesis in the era of smartphones and text communication. Orthopedics. 2012;35(11):955-957. [DOI] [PubMed] [Google Scholar]


