Abstract
Background: Despite the frequent occurrence of these injuries, we know little about the natural history of Salter-Harris II (SH II) distal radius fractures. We conducted a systematic review of studies examining the radiographic and clinical outcomes of nonoperatively managed SH II distal radius fractures. Methods: Systematic searches of the MEDLINE and Cochrane computerized literature databases and manual searches of bibliographies were performed. We reviewed both descriptive and quantitative data. Results: Seven studies including 434 SH II fractures were reviewed. Two studies reported clinical outcomes based on patient age, but neither study described a statistical correlation between patient age and outcome. Two studies discussed the effect of age on radiographic outcome and reported higher rates of anatomic remodeling in children 10 years or younger. Two studies with long-term (average follow-up greater than 8 years) clinical results reported complication rates of 5%. Long-term follow-up of radiographic outcomes appeared in 4 studies with variable results. Five studies reported the frequency of premature physeal arrest after SH II fractures, with results ranging from 0% to 4.3%. Conclusions: Based on this review, no recommendations can be made as to what defines an acceptable reduction or which fractures would benefit from surgical intervention. Angular deformity seems to correct to an acceptable alignment in patients less than 10 years of age, but these younger patients seem to be at higher risk for symptomatic shortening if a growth arrest occurs. Redisplacement after reduction is fairly common, and other more severe complications such as pain, loss of motion, and nerve injury can occur.
Keywords: distal radius, growth plate radius, Salter-Harris, physeal arrest, physeal fracture
Introduction
The reported incidence of pediatric distal radius fractures (DRFs) ranges from approximately 279 to 373 per 100 000 person-years, and 15% of these fractures involve the physis.5,12 Salter-Harris II (SH II) fractures comprise the majority of physeal injuries.9
Despite the common occurrence of these injuries, we know little about the natural history of SH II DRFs. The distal radius physis contributes 75% of the longitudinal growth of the radius, which allows for substantial remodeling in younger children. In fact, Nietosvaara et al11 reported an average improvement in angulation of 1° to 2° per month. However, SH II DRFs frequently occur in children nearing skeletal maturity. The peak DRF incidence occurs at age 11.5 to 12.5 years for girls and at age 13.5 to 14.5 years for boys.1 Despite the substantial growth potential of the distal radius physis, advanced patient age may not allow for complete correction of angulation.
No clearly defined treatment guidelines for SH II DRFs exist, and author opinions vary substantially. Although most authors recommend nonsurgical interventions,7 others propose operative treatment for children close to skeletal maturity, cases with significant initial fracture displacement, or inability to achieve an anatomic closed reduction.11 In 1967, Blount reported a series of pediatric forearm fractures and noted that with physeal fractures, “there is usually no complication.”2 Others describe complications including early physeal arrest, redisplacement after closed reduction, malunion, acute carpal tunnel syndrome, and compartment syndrome.4,10,11
We conducted a systematic review of the literature to better understand the clinical and radiographic outcomes of SH II DRFs. We sought to describe the radiographic and clinical outcomes of nonoperatively managed SH II DRFs, examine whether these outcomes vary based on patient age, and present the incidence of complications including physeal arrest (radiographic outcomes included malunion defined by radial shortening or dorsal angulation).
Materials and Methods
Search Strategy and Article Selection
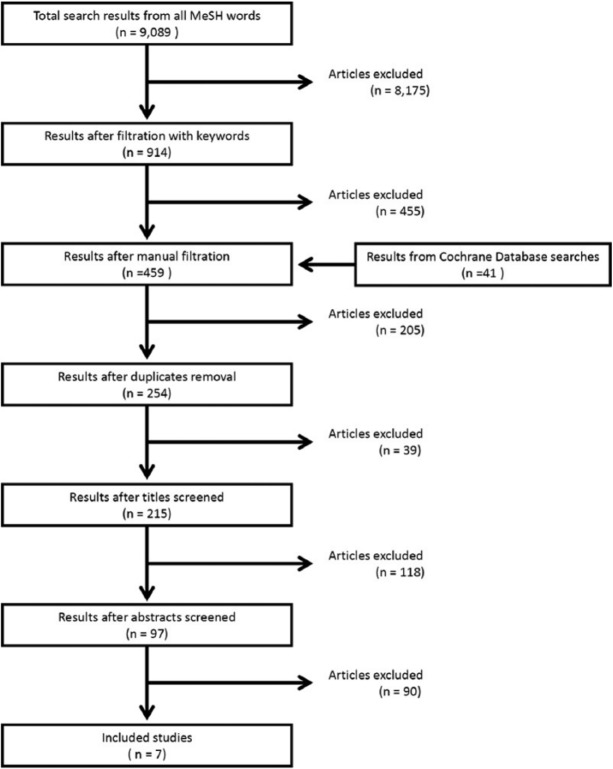
To be eligible for inclusion, published studies had to be case series, randomized controlled trials, prospective studies, or retrospective studies of operative or nonoperative treatment of SH II DRFs. We performed a systematic MEDLINE search of studies published between 1965 and November 2013 using PubMed (Appendix Table A1) and the Cochrane Database of Systematic Reviews and the Central Register of Controlled Trials (Appendix Table A2) using 9 keywords/phrases: distal radius, growth plate radius, Salter-Harris, forearm fracture, physeal arrest, percutaneous pinning, closed reduction radius, physeal fracture, and distal radius complications. Each term was searched independently of the other 8 (Appendix Table A1). We discarded any articles in which the title did not contain at least 2 additional keywords or 1 keyword and publication in a pediatric journal (Figure 1). One author (AR) then manually reviewed all titles for relevance and included articles for further review when the title indicated a focus on pediatric forearm or wrist fractures. After eliminating all duplicate results, 3 authors (ML, KB, CW) reviewed the remaining titles for relevance and selected abstracts for further review. These authors examined the abstracts and chose studies for full-text review. For articles without available abstracts, authors reviewed the full text. Following the independent review of full articles by each reviewer, all authors agreed upon the final studies for inclusion.
Figure 1.
Flow diagram of study selection process.
A flow diagram of the study selection process is shown in Figure 1, which is based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The authors independently evaluated the full text of 97 articles for quality and relevance. Three authors (ML, KB, CW) unanimously agreed on inclusion of 7 studies.
Results
The 7 selected studies were all retrospective (Table 1) and included a total of 434 fractures. The majority of the 90 eliminated studies made no distinction between different types of DRF or excluded physeal fractures. Many studies combined all “physeal fractures” or “distal third forearm fractures” and provided no analysis of outcomes based on fracture type.
Table 1.
Study Characteristics.
| First author, year | Level of evidence | No. of patients (No. of fractures) | No. of SH II fractures | Age range of physeal fracture, y; Type | Intervention | Mean follow-up (range) |
|---|---|---|---|---|---|---|
| Davis, 19764 | IV, case series | 547 | 63 | 7-16; SH II | CR and casting | NR |
| (547) | ||||||
| Cannata, 20033 | IV, case series | 157(163) | 139 | 5-17; SH I and II | Casting, CR, and casting | 25.5 y (14-46 y) |
| Houshian, 20045 | IV, case series | 85(85) | 85 | 4-15; SH II | Casting, CR, and casting | 8.5 y (2.5-15 y) |
| Nietosvaara, 200511 | IV, case series | 109(109) | 96 | 5-16; SH I and II | CR and casting, CRPP | 6 wk (1 wk-2 y) |
| Hove, 20086 | IV, case series | 88(88) | 7 | 8-15; SH I, II, IV | CR and casting | 7 y (select pts) |
| Luscombe, 20108 | IV, case series | 108(112) | 22 | 15-16; All fracturesa | CR and casting, CRPP | 1.1 y (10 wk-2 y) |
| McQuinn, 201210 | IV, case series | 155 | 22 | 0-15; All fracturesa | CR and casting | 5-10 d |
| (155) |
Note. SH, Salter-Harris; CR, closed reduction; CRPP, closed reduction and percutaneous pinning; NR, not reported; pts, patients.
Physeal and nonphyseal fractures of distal radius.
Operative Versus Nonoperative Treatment
No study directly compared the clinical or radiographic outcomes of operatively versus nonoperatively treated SH II DRF. The majority of patients underwent closed reduction and casting, but 1 study described 5 SH II DRFs treated with supplemental Kirschner wire (K-wire) fixation in addition to closed reduction and immobilization.11 Luscombe et al8 evaluated their practice of selective closed reduction and K-wire fixation for displaced DRFs (including SH II and other fracture patterns) to minimize fracture redisplacement. However, each of the 22 SH II physeal fractures included in the study was anatomically reduced without the use of K-wires, and no displacement occurred during the healing period. The review of 109 patients with SH I and II DRFs by Nietosvaara et al11 included 5 patients who underwent percutaneous pinning due to difficulty maintaining reduction, neurovascular concern, or an ipsilateral supracondylar humerus fracture.
Long-term Clinical Results
Two studies reported medium- to long-term follow-up of clinical outcomes of nonoperatively treated SH II DRF, and these 2 studies also reported the age at the time of injury of their patients. No studies utilized validated outcome questionnaires such as the Pediatric Outcomes Data Collection Instrument (PODCI), and no study specifically reported range of motion or grip strength. Clinical sequelae occurred in up to 5% of patients. In the study by Cannata et al,3 7 of 139 (5%) SH II DRFs followed for an average of 25.5 years presented with wrist complaints: 7 patients showed decreased wrist motion, 5 had visible deformity, 2 had wrist pain, 3 exhibited wrist snapping, and 4 demonstrated decreased grip strength. All 7 of these patients exhibited radial shortening greater than 1 cm, and 6 of the 7 patients were 12 years or younger at the time of their injury. Three underwent additional surgery for wrist problems (Darrach procedure, 2 patients; ulnar shortening, 1 patient). These patients ranged from 5 to 14 years old when injured. The child with the greatest number of complaints (visible deformity, pain, decreased motion, and grip strength) was the youngest (5 years 6 months) at the time of injury; this fracture also resulted in the most radial shortening (6.5 cm).
After a mean follow-up of 8.5 years (range, 2.5-15 years), 4 of 85 (4.7%) patients reviewed by Houshian et al5 complained of “slight” or “moderate” nonspecific wrist pain with sports or extensive work. Houshian et al5 grouped their patients in three 5-year age categories (1-5 years, 6-10 years, 11-15 years) and reported “normal” grip strength and wrist and forearm motion in all groups, although the authors provided no objective grip strength or motion data. The 4 symptomatic patients were between the ages of 6 and 15 years at the time of injury.
Long-term Radiographic Outcomes
Long-term follow-up of radiographic outcomes of nonoperatively treated SH II DRFs appeared in 4 studies with variable results. Nietosvaara et al11 stated that 48% of SH I and II DRFs healed in malunion, “which was usually mild,” but did not provide specific radiographic criteria for mild malunion. Thirteen percent of these cases healed with greater than 20% displacement and 14% healed with at least 10° angulation. In the subset of 20 (of 109) patients followed long term, 2 of 20 healed with greater than 10° apex volar angulation.11 Houshian et al5 reported that the median angulation at time of healing was 10° (range, 2°-22°) in the 63 patients (74%) who underwent an initial closed reduction. The remaining 26% of patients treated with cast immobilization alone healed with 9° (range, 2°-20°) angulation. Houshian et al5 provided no information about criteria for casting alone versus closed reduction and casting. At final follow-up, 86% of fractures in this study had completely remodeled.
Using comparison films of the uninjured wrist, Cannata et al found 39 of 157 (25%) patients had a radioulnar length discrepancy at an average follow-up of 25.5 years. All 7 patients with radial shortening that were greater than 1 cm displayed deficits in wrist function (see above). An additional 33 SH II DRFs healed with a length discrepancy of 2 to 9 mm compared with the uninjured side. In 27 cases, the affected radius was shorter and in 6 it was longer.3
Effect of Age on Radiographic Outcome
Two studies discussed the effect of patient age on radiographic outcomes. Houshian et al5 found that patient age influenced remodeling of volar tilt. In their study, 73 of 85 (86%) children demonstrated complete remodeling of both volar tilt and radial inclination of the distal radius after an average of 8.5 years. Of those patients aged 10 years or younger, 33 of 34 (97%) anatomically remodeled their volar inclination, compared with 41 of 51 (80%) of children older than 10 years at the time of injury. Thirty-three of 34 (97%) patients aged 10 years or younger and 47 of 51 (92%) of children older than 10 years completely remodeled radial inclination. Based on this, Houshian et al5 concluded that although some remodeling occurred in all ages, complete remodeling could occur in children below age 10. Nietosvaara et al reported that 2 of 20 patients selected for long-term follow-up exhibited more than 10° dorsal angulation. Injury occurred less than 6 months from skeletal maturity in both patients, and both patients reported persistent “wrist symptoms,” although the nature of those symptoms was not described.11
Physeal Arrest and Other Complications
Five studies reported that premature physeal arrest after SH II DRF from 0% to 4.3%.3-6,11 Houshian et al5 and Hove and Brudvik6 identified no physeal arrests in 85 children and 7 children, respectively, although neither author described the time to final follow-up radiographs. Davis and Green4 reported premature physeal arrest in 1 of 63 (1.6%) fractures. Of 109 SH I and II injuries, Nietosvaara et al11 reported 3 (2.5%) premature physeal closures. One child developed a growth arrest after late open reduction at 3 weeks, but this particular patient was not followed long term. Although Cannata et al did not specifically comment on physeal arrest, distal radius shortening greater than 1 cm (6 patients) most likely resulted from early physeal arrest3. The additional 27 fractures with length discrepancy of 2 to 9 mm in the Cannata study suggest radial growth disturbance as well.
Several other complications occurred after SH II DRF, including fracture displacement, acute carpal tunnel syndrome, compartment syndrome, and other neurovascular findings. These findings are summarized in Table 2.
Table 2.
SH II Patient Complications.
| First author, year | No. of SH II fractures | Redisplacement (%) | Repeat reduction (%) | Wrist deformity (%) | Growth arrest (%) | Restricted wrist ROM (%) | Paresthesia (%) | Pain (%) | Decreased grip strength (%) |
|---|---|---|---|---|---|---|---|---|---|
| Davis, 19764 | 63 | 4/53 (7.5) | — | — | 1 (1.6) | — | 2 (3.8) | — | — |
| Cannata, 20033 | 139 | 12/139 (8.6) | 7 (5) | 5 (3.6) | 2 (1.4) | 7 (5) | — | 2 (1.4) | 4 (2.9) |
| Houshian, 20045 | 85 | 7/63 (11.1) | — | — | 0 (0) | 0 (0) | — | 4 (4.7) | 0 (0) |
| Nietosvaara, 200511 | 96 | — | — | — | 3 (2.5) | — | — | 10 (10) | — |
| Hove, 20086 | 7 | — | — | — | 0 (0) | — | — | — | — |
| Luscombe, 20108 | 22 | 0/22 (0) | 0 (0) | — | 0 (0) | — | — | — | — |
| McQuinn, 201210 | 22 | 5/22 (22.7) | — | — | — | — | — | — | — |
Note. SH II, Salter-Harris II; %, percent of total SH II fractures; ROM, range of motion; “—”, not recorded.
Discussion
Only 7 articles contained enough information to warrant inclusion in this review of radiographic and clinical outcomes of SH II DRF in children. Very few studies included long-term radiographic follow-up, and no studies utilized validated clinical outcome measures or objective physical exam measurements. The heterogeneity of outcome variables and study design across these articles made any consensus difficult.
We assume younger patients have greater remodeling potential, which allows orthopedists to “accept” larger deformity at the time of fracture healing. However, SH II DRFs tend to occur in children closer to skeletal maturity, leaving patients with little time to remodel any malunion. In the reviewed studies, the peak incidence occurred around 11 to 12 years of age, with 1 study reporting 70% of their cohort older than 12 years of age.4 Due to symptomatic angular malunion in their patients injured near skeletal maturity, Nietosvaara et al11 recommended an anatomic reduction with possible pinning in children with greater than 50% displacement and less than 1 year of growth remaining. Houshian et al5 found that 95% to 97% aged 10 years or less completely remodeled their angular deformity versus 80% to 92% corrected after age 10 years. Based on the data available, we cannot make any specific recommendation about treatment of SH II DRF based on patient age. With this very limited information, age greater than 10 years may be helpful to use as a cutoff when counseling patients and families about their child’s ability to completely remodel angular deformity.
Patients with closing physes and little remaining growth potential may have a higher risk of residual angulation due to the lack of remodeling but less risk of symptomatic shortening of the radius. Cannata et al3 highlight the problem with growth arrest in younger patients. Of the 7 patients in their study with long-term clinical symptoms, 6 were 12 years old or younger at the time of injury, and all patients with clinical symptoms demonstrated radial shortening of greater than 1.0 cm, with a range of 1.0 to 6.5 cm. When fractures result in growth arrest, patients may be at a higher risk of long-term wrist dysfunction, but no studies have analyzed what patient or injury factors are associated with physeal arrest. No studies examined whether the natural history of a patient’s growth arrest could be altered with any intervention at the time of injury.
Close analysis of the study by Cannata et al3 reveals an additional 25% of patients with a length discrepancy between the radius and ulna less than 1 cm, quite likely due to some physeal disruption. This study had the longest follow-up and evaluated growth by comparing injured and contralateral limbs using bilateral radiographs. The methodology of other studies was less stringent, possibly accounting for the lower percentage of reported growth disturbance. The data suggest that growth disturbance is common with these injuries but may not be clinically relevant unless complete physeal arrest results in shortening greater than 1 cm.
SH II fractures can lead to complications other than growth disturbance. The reviewed studies reported a redisplacement rate of up to 22%,5 compartment syndrome, median nerve neuropraxia, as well as pain and functional problems. Two studies showed that 5% of patients reported wrist symptoms after fracture healing, including loss of wrist motion, visible deformity, wrist pain, and decreased grip strength. In the included studies, these sequelae occurred in patients who also had residual angular or length deformity of the radius. Theoretically, improved distal radius anatomic alignment at fracture healing in patients nearing skeletal maturity may help prevent some of these long-term issues.
The greatest limitation of this study is the lack of data in the literature. The heterogeneity of the study design of the selected studies made pooling of data difficult. All the studies are retrospective in nature and do not have any direct prospective comparisons of different treatments. Based on this review, no recommendations can be made as to what defines an acceptable reduction or which fractures would benefit from surgical intervention.
This topic would greatly benefit from prospective collection of clinical and radiographic outcomes utilizing a validated wrist outcome tool such as the PODCI. In light of the current deficiencies in the literature, a retrospective review that provides detailed analysis of injury characteristics, including degree of displacement and patient age at the time of injury, could help identify patients with increased risk of poor radiographic or clinical outcomes.
Appendix
Table A1.
MEDLINE Search Results.
| MeSH termsa | No. of results | Selected results | After further filtration | After duplicate removal |
|---|---|---|---|---|
| distal radius | 4117 | 252 | 145 | 254 |
| growth plate radius | 233 | 69 | 30 | |
| physeal fracture | 317 | 63 | 16 | |
| Salter-Harris | 185 | 65 | 11 | |
| forearm fracture | 2179 | 169 | 124 | |
| physeal arrest | 142 | 28 | 7 | |
| percutaneous pinning | 374 | 67 | 10 | |
| closed reduction radius | 350 | 117 | 69 | |
| distal radius complications | 1192 | 84 | 47 |
Filters used for all MeSH terms included (1) Humans, (2) Full text available, (3) English.
Inclusion words (Must contain at least 2 inclusion words in title to be flagged or contain 1 inclusion word and be in a pediatric journal).
Forearm
Distal radius fracture
Growth plate
Physeal/physis; metaphyseal; epiphysis; epiphyseal plate
Adolescent(s), child(ren), pediatric, paediatric,
Pediatric journal
Wrist
Table A2.
Cochrane Database Systematic Reviews and Central Register of Controlled Trials Search.
| Keyword(s)/phrasea | No. of results | Selected results | After further filtration | After duplicate removal |
|---|---|---|---|---|
| distal radius | 556 | 34 | 9 | 41 |
| growth plate radius | 921 | 49 | 7 | |
| physeal fracture | 1626 | 53 | 15 | |
| Salter-Harris | 172 | 13 | 3 | |
| forearm fracture | 1752 | 28 | 8 | |
| physeal arrest | 92 | 9 | 2 | |
| percutaneous pinning | 175 | 21 | 5 | |
| closed reduction radius | 3436 | 62 | 7 | |
| distal radius complications | 4446 | 93 | 29 |
See below for filters used for the Cochrane Database of Systematic Reviews and the Central Register of Controlled Trials.
Filters Used
Search mode: Find any of my search terms
Published date: Anytime-November 2013
Year of publication: 0-2013
Cochrane Database of Systematic Reviews
Document Type: All
Year of Publication—Protocols: Anytime-2013
Year of Publication—Reviews: Anytime-2013
Date Last Assessed: Anytime-2013
- Cochrane Library Source
- Cochrane Database of Systematic Reviews
- About the Cochrane Collaboration
- Records by Review Group
- Cochrane Bone, Joint and Muscle Trauma Group
- Cochrane Injuries Group
- Cochrane Musculoskeletal Group
Special Limiters for Cochrane Center Register of Controlled Trials
MEDLINE Publication Type: All
Language: English
- Review Groups & Registers
- Cochrane Bone, Joint and Muscle Trauma Group
- Cochrane Injuries Group
- Cochrane Musculoskeletal Group
MEDLINE/EMBASE Records: All
Inclusion words (Must contain at least 2 inclusion words in title to be flagged or contain 1 inclusion word and be in a pediatric journal)
Forearm
Distal radius fracture
Growth plate
Physeal/physis; metaphyseal; epiphysis; epiphyseal plate
Adolescent(s), child(ren), pediatric, paediatric,
Pediatric journal
Wrist
Footnotes
Ethical Approval: Institutional review board approval was not required because this study was a systematic review, examining the reported data from past studies regarding the subject of interest. At no point in this study were live patients, or protected health information, examined. No animals participated in this study.
Statement of Human and Animal Rights: Procedures performed in this study were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Statement of Informed Consent: Informed consent was not required because this study was a systematic review, examining the reported data from past studies regarding the subject of interest. At no point in this study were live patients, or protected health information, examined. No animals participated in this study.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71:1225-1231. [PubMed] [Google Scholar]
- 2. Blount WP. Forearm fractures in children. Clin Orthop Relat Res. 1967;51:93-107. [PubMed] [Google Scholar]
- 3. Cannata G, De Maio F, Mancini F, Ippolito E. Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma. 2003;17:172-179; discussion 179-180. [DOI] [PubMed] [Google Scholar]
- 4. Davis DR, Green DP. Forearm fractures in children: pitfalls and complications. Clin Orthop Relat Res. 1976;(120):172-183. [PubMed] [Google Scholar]
- 5. Houshian S, Holst AK, Larsen MS, Torfing T. Remodeling of Salter-Harris type II epiphyseal plate injury of the distal radius. J Pediatr Orthop. 2004;24:472-476. [DOI] [PubMed] [Google Scholar]
- 6. Hove LM, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg. 2008;128:55-60. [DOI] [PubMed] [Google Scholar]
- 7. Lee BS, Esterhai JL, Jr, Das M. Fracture of the distal radial epiphysis: characteristics and surgical treatment of premature, post-traumatic epiphyseal closure. Clin Orthop Relat Res. 1984;(185):90-96. [PubMed] [Google Scholar]
- 8. Luscombe KL, Chaudhry S, Dwyer JS, Shanmugam C, Maffulli N. Selective Kirschner wiring for displaced distal radial fractures in children. Acta Orthop Traumatol Turc. 2010;44:117-123. [DOI] [PubMed] [Google Scholar]
- 9. Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop. 1990;10:713-716. [DOI] [PubMed] [Google Scholar]
- 10. McQuinn AG, Jaarsma RL. Risk factors for redisplacement of pediatric distal forearm and distal radius fractures. J Pediatr Orthop. 2012;32:687-692. [DOI] [PubMed] [Google Scholar]
- 11. Nietosvaara Y, Hasler C, Helenius I, Cundy P. Marked initial displacement predicts complications in physeal fractures of the distal radius: an analysis of fracture characteristics, primary treatment and complications in 109 patients. Acta Orthop. 2005;76:873-877. [DOI] [PubMed] [Google Scholar]
- 12. Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma. 1972;12:275-281. [DOI] [PubMed] [Google Scholar]