Abstract
Background: In the treatment of basal joint arthritis of the thumb, recent studies suggest equivalent outcomes with regard to long-term pain, mobility, and strength, in patients undergoing either trapeziectomy alone or trapeziectomy with ligament reconstruction and tendon interposition (LRTI). The goal of this study was to investigate risk factors for complications in carpometacarpal (CMC) arthroplasty. Methods: We conducted a retrospective chart review of 5 surgeons at a single institution performing CMC arthroplasties from November 2006 to November 2012. A total of 200 thumbs in 179 patients underwent simple trapeziectomy with or without LRTI and with or without Kirschner wire stabilization, or a Weilby procedure. The average follow-up was 11.6 months (range = 1-69 months). Data collection included sex, age, history of smoking or diabetes, and any other surgeries performed on the hand at the time of arthroplasty. Furthermore, we collected outcomes involving any adverse events, paying attention to those necessitating reoperation, antibiotics, or those who developed complex regional pain syndrome. Results: Seventy hands had a postoperative complication. Ten of these complications were considered major, defined as requiring antibiotics, reoperation, or other aggressive interventions. On multivariate analysis, risk of total complications was significantly greater only in patients undergoing either trapeziectomy with LRTI or Weilby procedure in comparison with trapeziectomy with K-wire stabilization (odds ratio = 4.30 and 6.73, respectively). Conclusions: Patients undergoing trapeziectomy with LRTI or Weilby had a greater incidence of reported complications when compared with trapeziectomy alone. These results suggest an advantage of simple trapeziectomy; however, further study is warranted.
Keywords: carpometacarpal (CMC), arthritis, thumb, trapeziectomy
Arthritis of the trapeziometacarpal (carpometacarpal [CMC]) joint represents a common manifestation of osteoarthritis with some estimates reporting an incidence as high as 15% in the general population.7 In 1949, Gervis described treatment for this process as a simple trapeziectomy to provide pain relief. Since then, a number of variations have been described in an attempt to improve thumb pinch strength and decrease rates of recurrent pain. These operations included various materials for interposition in the vacant space following trapeziectomy as well as ways to reconstruct the volar beak ligament.1,16 Although synthetic materials trialed as a biomechanically sound treatment, they were met with unacceptable complications.3,8,11-13 Many other modalities include some sort of Kirschner wire (K-wire or pins) fixation, which can leave patients open to complications such as pin site infection and pin migration.4,9,10 Recent level I2,5,17 and level III15 evidence suggests that long-term pain relief and functionality can be achieved with equivalent success among common variations of the procedure including simple trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition.2,4,5,15,17 The aim of this study is to evaluate our experience with CMC arthroplasty and identify factors associated with postoperative complications in the treatment of basal joint arthritis.
Materials and Methods
After receiving Institutional Board approval, we conducted a retrospective chart review of 5 surgeons at a single institution who performed CMC arthroplasties from November 2006 to November 2012.
Operations performed were trapeziectomy alone or trapeziectomy and ligament reconstruction tendon interposition (LRTI) with or without K-wire stabilization, or a Weilby procedure. The Weilby procedure involved partial harvest of flexor carpi radialis (FCR) which was then weaved between abductor pollicis longus (APL) and remaining FCR to suspend the metacarpal in abduction. The harvested tendon also courses allowing it to serve as an interposition.18 K-wire was not used. In cases of LRTI, FCR tendon was used as a complete tendon or a partially harvested tendon, depending on surgeon. Our postoperative course and operation choice varied per surgeon. Two authors preferred trapeziectomy with LRTI and K-wire through a dorsal incision. Postoperatively, these authors kept patients in 4 weeks of K-wire distraction. One of these authors, who used a partial harvest of FCR tendon, began patients on hand therapy immediately following pin removal; the other surgeon, who used full FCR tendon, began therapy 2 weeks post removal. Two other authors preferred trapeziectomy with K-wire, one through a dorsal incision, the other through a radial/volar incision. Postoperatively, patients were kept in distraction for 4 weeks and then allowed full motion when removed. One of these authors also performed trapeziectomy without the use of K-wire and kept these patients in a thumb spica splint for 4 week followed by full motion. One author performed a Weilby procedure through a radial/volar incision. The patient would begin hand therapy starting 2 weeks post surgery. The choice of operation was determined by surgeon preference and not by disease or patient characteristics.
Data collection included patient age, sex, operation type, diabetes, smoking, and outcomes involving any adverse events, paying attention to those necessitating reoperation, antibiotics, or those who developed complex regional pain syndrome (CRPS). We divided complications into major, defined as requiring antibiotics, reoperation, or CRPS, and minor. Minor complications included swelling, stiffness, paresthesias, symptomatic subsidence, and symptomatic tendonitis.
Results
Overall, we identified 200 operations in 179 patients; 40 of the patients were male and 139 were female. The mean age of the patients was 59.4 years old. Of the 200 operations, 102 were on the right thumb and 98 on the left thumb (Table 1). The average follow-up was 11.6 months (range was 1-69 months).
Table 1.
Patient Demographics Data.
| Patient characteristics | Number of patients |
|---|---|
| Male | 40 |
| Female | 139 |
| Age, mean (years) | 59.4 (range = 21.9-80.2) |
| Right thumb | 102 |
| Left thumb | 98 |
Of the 200 operations, the majority underwent trapeziectomy with LRTI with the use of K-wire. Trapeziectomy with the use of K-wire was second most common, followed by Weilby procedure, and trapeziectomy without the use of K-wire (Figure 1).
Figure 1.
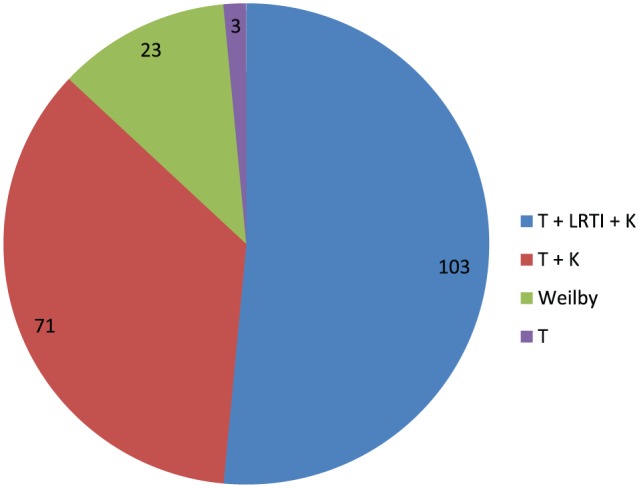
Distribution of operative techniques.
Note. Number of cases listed within each section of the pie chart. T, trapeziectomy; LRTI, ligament reconstruction with tendon interposition; K, use of Kirschner wire.
Seventy hands had a postoperative complication. Ten of these complications were major and 36 of the complications were minor as further illustrated in Table 2. Number of complications per surgery type is also included in Table 3.
Table 2.
Complications Divided Into Subgroups: Major and Minor.
| Major complications (10) | Minor complications (36) |
|---|---|
| Infection requiring antibiotics (6) | Paresthesias (8) |
| Reoperation/procedural Intervention (5) | Wound/scar related issues (10) |
| Complex regional pain syndrome (1) | Symptomatic subsidence (18) |
| Prolonged swelling (3) |
Table 3.
Complications by Each Procedure Type.
| Procedure | Total number (n) | Major complications (n) | Minor complications (n) | Total complications (n) |
|---|---|---|---|---|
| Trapeziectomy | 3 | 1 | 0 | 1 |
| Trapeziectomy + K-wire | 71 | 2 | 7 | 9 |
| Trapeziectomy + LRTI | 103 | 6 | 22 | 28 |
| Weilby | 23 | 1 | 7 | 8 |
Note. LRTI, ligament reconstruction and tendon interposition.
We performed a multivariate analysis comparing trapeziectomy with K-wire with trapeziectomy plus LRTI and the Weilby procedure. We removed patients who had undergone trapeziectomy in the absence of K-wire (n = 3) during this analysis due to the low number of these patients. When controlling for age, sex, history of smoking or diabetes, and the performance of a concomitant operation on the same hand, patients had an increased rate of complications in trapeziectomy with LRTI group (odds ratio = 4.30, P = .005) and Weilby procedure group (odds ratio = 6.73, P = .006; Table 4). Furthermore, we found an increase in minor complications in these 2 groups, but not in major complications (Table 5).
Table 4.
Multivariate Analysis Comparing Trapeziectomy Plus K-Wire With Trapeziectomy Plus LRTI and Weilby Procedure With Regard to Total Complications.
| OR | P value | CI | |
|---|---|---|---|
| Trapeziectomy + K-wire | 1.00 | — | — |
| Trapeziectomy + LRTI | 4.30 | .005* | 1.54-12.03 |
| Weilby | 6.73 | .006* | 1.75-25.96 |
| Age > 65 | 1.92 | .175 | 0.75-4.96 |
| Sex (male) | 0.82 | .671 | 0.32-2.06 |
| Diabetes | 0.68 | .499 | 0.22-2.08 |
| Smoking | 1.11 | .817 | 0.47-2.59 |
| Concomitant surgery | 0.59 | .258 | 0.24-1.47 |
Note. Lower portion of the chart demonstrating control for age, sex, diabetes, smoking, and the performance of other procedures on the same hand at the time of surgery. LRTI, ligament reconstruction and tendon interposition; OR, odds ratio; CI, confidence interval.
Indicates statistical significance with P < .05.
Table 5.
Analysis Comparing Trapeziectomy Plus K-Wire With Trapeziectomy Plus LRTI and Weilby Procedure With Regard to Major and Minor Complications.
| OR | P value | CI | |
|---|---|---|---|
| Major | |||
| Trapeziectomy + K-wire | 1.00 | — | — |
| Trapeziectomy + LRTI | 4.66 | 1.40 | 0.54-39.9 |
| Weilby | 3.47 | .86 | 0.20-58.8 |
| Minor | |||
| Trapeziectomy + K-wire | 1.00 | — | — |
| Trapeziectomy + LRTI | 2.91 | .05* | 1.00-8.49 |
| Weilby | 5.76 | .01* | 1.47-22.6 |
Note. LRTI, ligament reconstruction and tendon interposition; OR, odds ratio; CI, confidence interval.
*Indicates statistical significance with P < .05.
Five cases required operative or procedural intervention that deferred from the surgeon’s predetermined protocol (Table 6). One case of pin cellulitis required incision and drainage and early pin removal. One case of pin irritation also required early pin removal. One case of severe joint space infection required incision and drainage 8 weeks after arthroplasty. The patient required admission and IV antibiotics and was noted to be non-methicillin resistant Staphylococcus aureus (MRSA). This patient had undergone trapeziectomy plus LRTI with the use of K-wire. There was also 1 case of FCR tendonitis requiring operative exploration, FCR tenotomy, and debridement of the scaphoid tubercle. One case of persistent pain required revision arthroplasty that had originally been performed in LRTI fashion. In this case, a small amount of boney material had been identified in the CMC joint that was cleared. All of these patients went on to do well with regard to their arthroplasties.
Table 6.
Cases Requiring Reoperation (n = 5).
| Pin irritation |
| Pin cellulitis |
| FCR tendonitis |
| Joint space infection |
| Persistent pain requiring revision arthroplasty |
Note. FCR, flexor carpi radialis.
Discussion
In the treatment of basal joint arthritis, surgeon preference often leads to choice of operation. Recent evidence suggests that outcomes from these procedures are similar with regard to pain relief, pinch strength, and grip strength.2,4,5,15,17 Our study suggests that there is an association between reported adverse events in patients undergoing trapeziectomy with ligament reconstruction and tendon interposition in comparison with trapeziectomy alone. These results are consistent with the results of others as summarized in a Cochrane review of treatment for CMC arthritis in 2009.17 In that review, 5 studies identified adverse events in their respective series. Complications cited in these series included complications similar to our own such as sensory changes in superficial radial sensory nerve or palmar cutaneous branch distribution, scar tenderness, tendon adhesions, CRPS, and wound infections. It was concluded that there was an increased risk of adverse events with LRTI compared with trapeziectomy alone.17 Here, we present our single-institution experience, with a multivariate analysis controlling for confounding variables that also includes a comparison with the Weilby procedure.
Although not statistically significant, we did identify 9 complications specifically related to the use of K-wire. Some of these have been severe requiring antibiotics or even operative intervention. Others have reported complications specific to K-wire usage in their series, including pin migration and pin infection.6,9,10 In addition, it has been subject to debate whether maintenance of trapezial space height correlated with any improvement in the clinical outcome.4,10,19 Salem and Davis demonstrated no advantage with LRTI plus K-wire in comparison with trapeziectomy alone with a period of 3 weeks with bulky bandage with a follow-up of 6 years.14
Performing concomitant surgeries on the same hand does not appear to influence risk of complications related to the arthroplasty. Patient-specific risk factors including smoking, diabetes, and age were also not found to be significantly associated with complications.
Our data are retrospective and is therefore open to reporter bias. Unfortunately, no meaningful data could be collected regarding pinch or grip strength due to the variability in documentation among surgeons. Operations were performed based on surgeon preference, and these operations were surgeon specific, with 1 surgeon performing the same operation for every patient with little or no variation; this reduced selection bias in study. Initially, we included pain in our criteria for minor complications. We found this to be the most common minor complication, affecting 38 patients. During statistical analysis, we were able to identify LRTI as being associated with an increase in reported adverse events, both when pain was and was not included as a minor complication. We also found that when we included pain as a minor complication, we found 1 surgeon to have statistically fewer adverse events compared with the other surgeons. Excluding pain as a minor complication resulted in the loss of this statistical significance. These findings could be explained as either evidence of reporter bias regarding documentation of pain specifically or evidence that this surgeon’s procedure of choice, trapeziectomy with the use of K-wire, is associated with fewer reports of pain.
Due to the retrospective nature of our study, pinch and grip strength, as well as objective measures of pain preoperation and postoperation could not be collected consistently. Previous studies, including randomized controlled trials providing level I2,5,17 and level III15 evidence, have highlighted objective outcomes regarding these measures and have demonstrated similar outcomes specifically when comparing trapeziectomy alone with trapeziectomy plus LRTI.2,5,15,17
Our data in combination with already published literature lead us to recommend surgeons to carefully evaluate their choice of procedure in the treatment of CMC arthritis. As surgery has evolved for the treatment of this condition from simple trapeziectomy, to interposition with biologic and synthetic materials, to ligament reconstruction, it is of interest to note that more elaborate operations may not result in any significant gain in patient outcome.
Acknowledgments
We would like to formally thank Heather Strom for her assistance in facilitating Institutional Review Board approval for this study. Furthermore, we would like to thank Natasha Dolgin for her invaluable assistance in our statistical analysis.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: Informed consent was not obtained as part of this study. The study is a retrospective review with no identifying information collected for publication and was therefore exempt from requiring informed consent by the Institutional Review Board of University of Massachusetts Medical School.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Barron AOC, Louis W. Thumb basal joint arthritis. In: Wolfe SW, ed. Green’s Operative Hand Surgery. Vol. 1 6th ed. Philadelphia, PA: Elsevier; 2011:407-426. [Google Scholar]
- 2. Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Br. 2000;25(4):350-356. [DOI] [PubMed] [Google Scholar]
- 3. Clarke S, Hagberg W, Kaufmann RA, Grand A, Wollstein R. Complications with the use of Artelon in thumb CMC joint arthritis. Hand. 2011;6(3):282-286. doi: 10.1007/s11552-011-9332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Downing ND, Davis TR. Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am. 2001;26(5):862-868. [DOI] [PubMed] [Google Scholar]
- 5. Gangopadhyay S, McKenna H, Burke FD, Davis TR. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37(3):411-417. doi: 10.1016/j.jhsa.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 6. Gray KV, Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am. 2007;32(1):23-29. [DOI] [PubMed] [Google Scholar]
- 7. Haara MM, Heliovaara M, Kroger H, et al. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86-A(7):1452-1457. [DOI] [PubMed] [Google Scholar]
- 8. Jorheim M, Isaxon I, Flondell M, Kalen P, Atroshi I. Short-term outcomes of trapeziometacarpal Artelon implant compared with tendon suspension interposition arthroplasty for osteoarthritis: a matched cohort study. J Hand Surg Am. 2009;34(8):1381-1387. doi: 10.1016/j.jhsa.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 9. Kuhns CA, Emerson ET, Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: a prospective, single-surgeon study including outcomes measures. J Hand Surg Am. 2003;28(3):381-389. [DOI] [PubMed] [Google Scholar]
- 10. Lins RE, Gelberman RH, McKeown L, Katz JN, Kadiyala RK. Basal joint arthritis: trapeziectomy with ligament reconstruction and tendon interposition arthroplasty. J Hand Surg Am. 1996;21(2):202-209. [DOI] [PubMed] [Google Scholar]
- 11. Luria S, Waitayawinyu T, Nemechek N, Huber P, Tencer AF, Trumble TE. Biomechanic analysis of trapeziectomy, ligament reconstruction with tendon interposition, and tie-in trapezium implant arthroplasty for thumb carpometacarpal arthritis: a cadaver study. J Hand Surg Am. 2007;32(5):697-706. [DOI] [PubMed] [Google Scholar]
- 12. Nilsson A, Liljensten E, Bergstrom C, Sollerman C. Results from a degradable TMC joint Spacer (Artelon) compared with tendon arthroplasty. J Hand Surg Am. 2005;30(2):380-389. [DOI] [PubMed] [Google Scholar]
- 13. Nilsson A, Wiig M, Alnehill H, et al. The Artelon CMC spacer compared with tendon interposition arthroplasty. Acta Orthop. 2010;81(2):237-244. doi: 10.3109/17453671003635835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Salem H, Davis TR. Six year outcome excision of the trapezium for trapeziometacarpal joint osteoarthritis: is it improved by ligament reconstruction and temporary Kirschner wire insertion? J Hand Surg Eur Vol. 2012;37(3):211-219. doi: 10.1177/1753193411414516. [DOI] [PubMed] [Google Scholar]
- 15. Sandvall BK, Cameron TE, Netscher DT, Epstein MJ, Staines KG, Petersen NJ. Basal joint osteoarthritis of the thumb: ligament reconstruction and tendon interposition versus hematoma distraction arthroplasty. J Hand Surg Am. 2010;35(12):1968-1975. doi: 10.1016/j.jhsa.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 16. Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(1):157-169. doi:110.1016/j.jhsa.2010.1010.1028. [DOI] [PubMed] [Google Scholar]
- 17. Wajon A, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2009(4):CD004631. doi: 10.1002/14651858.CD004631.pub3. [DOI] [PubMed] [Google Scholar]
- 18. Weilby A. Surgical treatment of osteoarthritis of the carpo-metacarpal joint of the thumb. Indications for arthrodesis, excision of the trapezium, and alloplasty. Scand J Plast Reconstr Surg. 1971;5(2):136-141. [DOI] [PubMed] [Google Scholar]
- 19. Yang SS, Weiland AJ. First metacarpal subsidence during pinch after ligament reconstruction and tendon interposition basal joint arthroplasty of the thumb. J Hand Surg Am. 1998;23(5):879-883. [DOI] [PubMed] [Google Scholar]


